Escolar Documentos
Profissional Documentos
Cultura Documentos
Nursing Care Plan
Enviado por
Marielle SorianoDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Nursing Care Plan
Enviado por
Marielle SorianoDireitos autorais:
Formatos disponíveis
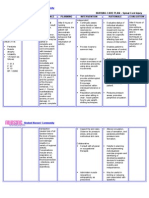
NURSING CARE PLAN
Assessment
S-
Objectives :
RR- 24
Abnormal
breath sounds
use of
accessory
muscles
Dyspnea
Cyanosis
Cough
with sputum
production
Nursing Diagnosis
Planning
Ineffective Airway After 8 hours of Nursing
Clearance related
Intervention the patient
to
will :
Tracheal bronchial
inflammation,
Identify/demonst
decrease energy
rate behaviors to
and fatigue
achieve airway
clearance.
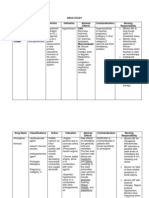
Intervention
Assess
rate/depth
respirations
and
movement.
of
chest
Rationale
Tachypnea, shallow respirations, and
asymmetric chest movement are
frequently present because of
discomfort of moving chest wall
and/or fluid in lung.
Auscultate lung fields, noting
areas of decreased/absent
airflow and adventitious
breath sounds, e.g., crackles,
wheezes.
Elevate head of bed, change
position frequently
Lowers diaphragm, promoting chest
expansion, aeration of lung segments,
mobilization and expectoration of
secretions.
Assist patient with frequent
deep-breathing
exercises.
Demonstrate/help
patient
learn to perform activity, e.g.,
splinting chest and effective
coughing while in upright
position.
Deep breathing facilitates maximum
expansion of the lungs/smaller
airways. Coughing is a natural selfcleaning mechanism, assisting the
cilia to maintain patent airways.
Splinting reduces chest discomfort,
and an upright position favors deeper,
more forceful cough effort.
Suction as indicated (e.g.,
frequent or sustained cough,
adventitious breath sounds,
desaturation related to airway
secretions).
Stimulates cough or mechanically
clears airway in patient who is unable
to do so because of ineffective cough
or decreased level of consciousness.
Display patent
airway with breath
sounds clearing;
absence of dyspnea,
cyanosis.
Decreased airflow occurs in areas
consolidated with fluid. Bronchial
breath sounds (normal over bronchus)
can also occur in consolidated areas.
Crackles, rhonchi, and wheezes are
heard on inspiration and/or expiration
in response to fluid accumulation,
thick
secretions,
and
airway
spasm/obstruction.
Evaluation
Goal partially met.
After 8 hours of Nursing
Intervention the patient :
Identified/demonstrated
behaviors to achieve
airway clearance.
Displayed patent airway
with breath sounds
clearing; absence of
dyspnea, cyanosis.
Force fluids to at least 3000
mL/day
(unless
contraindicated, as in heart
failure). Offer warm, rather
than cold, fluids.
Fluids (especially warm liquids) aid
in mobilization and expectoration of
secretions
Assist with/monitor effects of
nebulizer treatments and
other
respiratory
physiotherapy, e.g., incentive
spirometer, IPPB, percussion,
postural drainage. Perform
treatments between meals and
limit fluids when appropriate.
Facilitates liquefaction and removal
of secretions. Postural drainage may
not be effective in interstitial
pneumonias or those causing alveolar
exudate/destruction. Coordination of
treatments/schedules and oral intake
reduces likelihood of vomiting with
coughing, expectorations.
Administer medications as
indicated:
mucolytics,
expectorants,
bronchodilators, analgesics.
Aids in reduction of bronchospasm
and mobilization of secretions.
Analgesics are given to improve
cough effort by reducing discomfort,
but should be used cautiously because
they
can
decrease
cough
effort/depress respirations.
Provide supplemental fluids,
e.g., IV, humidified oxygen,
and room humidification
Fluids are required to replace losses
(including insensible) and aid in
mobilization of secretions. Note:
Some studies indicate that room
humidification has been found to
provide minimal benefit and is
thought to increase the risk of
transmitting infection.
Monitor serial chest x-rays,
ABGs,
pulse
oximetry
readings.
Follows progress and effects of
disease process/therapeutic regimen,
and facilitates necessary alterations in
therapy.
Você também pode gostar
- Asthma Care PlanDocumento3 páginasAsthma Care PlanSam ParkAinda não há avaliações
- Ineffective Airway Clearance Nursing Care PlanDocumento2 páginasIneffective Airway Clearance Nursing Care Planrois romaAinda não há avaliações
- Assessment Diagnosis Scientific Explanation Objective Interventions Rationale Expected Outcome Short Term: Short TermDocumento4 páginasAssessment Diagnosis Scientific Explanation Objective Interventions Rationale Expected Outcome Short Term: Short TermGensen Cu RoxasAinda não há avaliações
- Ineffective Airway Clearance CareplanDocumento6 páginasIneffective Airway Clearance CareplanderreshaAinda não há avaliações
- ASTHMADocumento9 páginasASTHMAmildred alidonAinda não há avaliações
- Wk2 NCP Edited2012Documento6 páginasWk2 NCP Edited2012Jessely Caling SalasAinda não há avaliações
- PneumoniaDocumento2 páginasPneumoniaPia MedinaAinda não há avaliações
- Angel Therisse B. Ramelb BSN Ii-C Nursing DiagnosisDocumento2 páginasAngel Therisse B. Ramelb BSN Ii-C Nursing DiagnosisSalvaje CaballeroAinda não há avaliações
- NCPDocumento8 páginasNCPryzaimaliaAinda não há avaliações
- NCP PTBDocumento6 páginasNCP PTBJay Dela VegaAinda não há avaliações
- Nursing Care Plans For Activity IntoleranceDocumento4 páginasNursing Care Plans For Activity IntolerancethebigtwirpAinda não há avaliações
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term Goal: IndependentDocumento4 páginasAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term Goal: IndependentNinaAinda não há avaliações
- Cerebral Aneurysm Case Analysis and Concept MapDocumento5 páginasCerebral Aneurysm Case Analysis and Concept Mapate NarsAinda não há avaliações
- NCP BronchopneumoniaDocumento8 páginasNCP BronchopneumoniaCrisantaCasliAinda não há avaliações
- Nursing ManagementDocumento16 páginasNursing ManagementNica Marie LumbaAinda não há avaliações
- NCPDocumento27 páginasNCPcuakialyannaAinda não há avaliações
- Nursing Care PlanDocumento4 páginasNursing Care Planapi-309251523Ainda não há avaliações
- Decreased Cardiac OutputDocumento4 páginasDecreased Cardiac OutputAdnan Khan100% (1)
- Student NurseDocumento2 páginasStudent NurseTAYABAN, KENNETH JAKE, Q.Ainda não há avaliações
- Concept Map - Abby !Documento2 páginasConcept Map - Abby !Abegail Abaygar100% (3)
- Scribd 020922 Case Study-Oncology A&kDocumento2 páginasScribd 020922 Case Study-Oncology A&kKellie DAinda não há avaliações
- Assessment Diagnosis Planning Nursing Intervention Rationale EvaluationDocumento2 páginasAssessment Diagnosis Planning Nursing Intervention Rationale Evaluationjennelyn losantaAinda não há avaliações
- NCP Copd4Documento15 páginasNCP Copd4Alessa Marie Crisostomo Salazar100% (1)
- Course in The WardDocumento1 páginaCourse in The WardGeevee Naganag VentulaAinda não há avaliações
- Nursing Care PlanDocumento26 páginasNursing Care PlanPrincessLienMondejarAinda não há avaliações
- Far Eastern University Nursing Care Plan Nursing Diagnosis Analysis Goals and Objectives Intervention Rationale EvaluationDocumento1 páginaFar Eastern University Nursing Care Plan Nursing Diagnosis Analysis Goals and Objectives Intervention Rationale EvaluationSarah CarreteroAinda não há avaliações
- Nursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveDocumento2 páginasNursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveFreisanChenMandumotanAinda não há avaliações
- NCP #2Documento4 páginasNCP #2Nutz TolentinoAinda não há avaliações
- Planning 3 NCPSDocumento5 páginasPlanning 3 NCPSCuttie Anne GalangAinda não há avaliações
- Acute PainDocumento3 páginasAcute PainJayr ChinAinda não há avaliações
- Nursingcribcom Nursing Care Plan Spinal Cord InjuryDocumento2 páginasNursingcribcom Nursing Care Plan Spinal Cord InjuryJanine Erika Julom Brillantes100% (1)
- NCP PainDocumento2 páginasNCP PainApril_Ivy_Raga_3835Ainda não há avaliações
- Nursing Care Plan FinalDocumento16 páginasNursing Care Plan FinalErickson OcialAinda não há avaliações
- Nursing Care PlanDocumento14 páginasNursing Care PlanVin Landicho100% (1)
- Ineffective Airway ClearanceDocumento1 páginaIneffective Airway ClearanceChristineAlaAinda não há avaliações
- NCP BMDocumento1 páginaNCP BMSourabh MehraAinda não há avaliações
- NCP KoDocumento1 páginaNCP Kojiellianemae100% (1)
- Nursing Care PlanDocumento15 páginasNursing Care PlanZhel Geron MercadoAinda não há avaliações
- NCP ProperDocumento5 páginasNCP ProperRustan FrozenAinda não há avaliações
- Discharge Plan Post SeizureDocumento2 páginasDischarge Plan Post SeizureVecky TolentinoAinda não há avaliações
- Chest Pain Care PlanDocumento2 páginasChest Pain Care Planapi-545292605Ainda não há avaliações
- Nursing Care PlanDocumento5 páginasNursing Care PlanPaola Marie VenusAinda não há avaliações
- NCP For Rapid Shallow BreathingDocumento1 páginaNCP For Rapid Shallow Breathingbamboo2dAinda não há avaliações
- NCP Cad ElectiveDocumento1 páginaNCP Cad ElectivejoegeAinda não há avaliações
- JDM Care PlanDocumento5 páginasJDM Care PlangopscharanAinda não há avaliações
- Deficient Knowledge: Nursing Diagnosis Nursing Care Plans (NCP)Documento3 páginasDeficient Knowledge: Nursing Diagnosis Nursing Care Plans (NCP)Vincent Paul SantosAinda não há avaliações
- Cu 4Documento3 páginasCu 4Paul SahagunAinda não há avaliações
- 1 Ineffective Airway ClearanceDocumento8 páginas1 Ineffective Airway ClearanceEsel Mae DinamlingAinda não há avaliações
- NCP On DyspneaDocumento5 páginasNCP On DyspneaDizzy BualanAinda não há avaliações
- Impaired Gas Exchange NCPDocumento3 páginasImpaired Gas Exchange NCPRomel BaliliAinda não há avaliações
- Nursing Care PlanDocumento1 páginaNursing Care PlanMikki lor PuaganAinda não há avaliações
- Problem: Viii. Planning (Nursing Cre Plan)Documento10 páginasProblem: Viii. Planning (Nursing Cre Plan)Raidis PangilinanAinda não há avaliações
- Impaired Gas Exchange NCPDocumento3 páginasImpaired Gas Exchange NCPRomel BaliliAinda não há avaliações
- Acute Pain SCMCDocumento2 páginasAcute Pain SCMCWik Wik PantuaAinda não há avaliações
- Assessment Explanatio Nofthe Problem Objectives Nursing Intervention Rationale EvaluationDocumento3 páginasAssessment Explanatio Nofthe Problem Objectives Nursing Intervention Rationale EvaluationAziil LiizaAinda não há avaliações
- PneumoniaDocumento17 páginasPneumoniajustin_saneAinda não há avaliações
- Below Are 8 Pneumonia Nursing Care Plans (NCP)Documento16 páginasBelow Are 8 Pneumonia Nursing Care Plans (NCP)Diana CarinoAinda não há avaliações
- Ineffective Airway ClearanceDocumento10 páginasIneffective Airway ClearanceHannah VueltaAinda não há avaliações
- Asthma: 1.) What Are The Nursing Managements For Each Respiratory Disorders?Documento5 páginasAsthma: 1.) What Are The Nursing Managements For Each Respiratory Disorders?Charlyn AustriaAinda não há avaliações
- Name of DrugDocumento1 páginaName of DrugMarielle SorianoAinda não há avaliações
- Case Study Liver CirrhosisDocumento30 páginasCase Study Liver CirrhosisMarielle Soriano100% (3)
- Effectiveness of E-Technology As Innovative Teaching Strategy: "Basis For E-Technology Preparedness"Documento2 páginasEffectiveness of E-Technology As Innovative Teaching Strategy: "Basis For E-Technology Preparedness"Marielle SorianoAinda não há avaliações
- Final G CaseDocumento34 páginasFinal G CaseMarielle SorianoAinda não há avaliações
- BullyDocumento80 páginasBullyMarielle SorianoAinda não há avaliações
- Thesis Chapter 1Documento18 páginasThesis Chapter 1Marielle Soriano60% (10)
- Nursing Care Plan Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationDocumento2 páginasNursing Care Plan Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationMarielle SorianoAinda não há avaliações
- Drug Study Drug Name Classifications Action Indication Adverse Effects Contraindication Nursing Responsibility CnsDocumento4 páginasDrug Study Drug Name Classifications Action Indication Adverse Effects Contraindication Nursing Responsibility CnsMarielle SorianoAinda não há avaliações
- Drug Study Drug Name Classifications Action Indication Adverse Effects Contraindication Nursing Responsibility CnsDocumento4 páginasDrug Study Drug Name Classifications Action Indication Adverse Effects Contraindication Nursing Responsibility CnsMarielle SorianoAinda não há avaliações
- Drugs Action Indicatio N Contraindicatio N Side and Adverse Effect Nursing Responsibilit Y - Hypertensiv e Client and Having A Heart FailureDocumento4 páginasDrugs Action Indicatio N Contraindicatio N Side and Adverse Effect Nursing Responsibilit Y - Hypertensiv e Client and Having A Heart FailureMarielle SorianoAinda não há avaliações
- Stem Cell Therapy: NR-41 Group 3Documento12 páginasStem Cell Therapy: NR-41 Group 3Marielle SorianoAinda não há avaliações
- NCPDocumento4 páginasNCPMarielle SorianoAinda não há avaliações
- Stem Cell TherapyDocumento2 páginasStem Cell TherapyMarielle SorianoAinda não há avaliações
- Muffin 3: Bestfriend BestfriendDocumento2 páginasMuffin 3: Bestfriend BestfriendMarielle SorianoAinda não há avaliações
- Activity Based Teaching StrategiesDocumento9 páginasActivity Based Teaching StrategiesMarielle Soriano100% (1)
- When A Force Does No WorkDocumento2 páginasWhen A Force Does No WorkMarielle SorianoAinda não há avaliações
- Eurolite Led TMH 7 PDFDocumento2 páginasEurolite Led TMH 7 PDFSarahAinda não há avaliações
- Chemical Resistance TableDocumento6 páginasChemical Resistance TableEdgarDavidDiazCamposAinda não há avaliações
- Definition of Logistics ManagementDocumento4 páginasDefinition of Logistics ManagementzamaneAinda não há avaliações
- Company ProfileDocumento36 páginasCompany ProfileShahzad Nasir SayyedAinda não há avaliações
- Salmonella - Methods and Protocols.-springer-Verlag New York (2020)Documento215 páginasSalmonella - Methods and Protocols.-springer-Verlag New York (2020)Yudith ParamitadeviAinda não há avaliações
- Notes StressDocumento4 páginasNotes StressRohitKalraAinda não há avaliações
- An Infallible JusticeDocumento7 páginasAn Infallible JusticeMani Gopal DasAinda não há avaliações
- The Church of Kapnikarea in Athens - N. GkiolesDocumento13 páginasThe Church of Kapnikarea in Athens - N. GkiolesMaronasAinda não há avaliações
- Asutphin Client Assessment Matrix Fitt Pros Unit 8Documento4 páginasAsutphin Client Assessment Matrix Fitt Pros Unit 8api-307235123Ainda não há avaliações
- Donali Lalich Literature ReviewDocumento4 páginasDonali Lalich Literature Reviewapi-519746057Ainda não há avaliações
- 300 20Documento3 páginas300 20Christian JohnsonAinda não há avaliações
- 020 Basketball CourtDocumento4 páginas020 Basketball CourtMohamad TaufiqAinda não há avaliações
- Balmatech Go Ep Tds 2022-03 GBDocumento2 páginasBalmatech Go Ep Tds 2022-03 GBAnalista De CalidadAinda não há avaliações
- A Practical Approach To Classical YogaDocumento39 páginasA Practical Approach To Classical Yogaabhilasha_yadav_1Ainda não há avaliações
- MHT-CET 2021 Question Paper: 25 September 2021Documento3 páginasMHT-CET 2021 Question Paper: 25 September 2021Sank DamAinda não há avaliações
- The Russian Review - 2020 - ROTH EY - Listening Out Listening For Listening in Cold War Radio Broadcasting and The LateDocumento22 páginasThe Russian Review - 2020 - ROTH EY - Listening Out Listening For Listening in Cold War Radio Broadcasting and The LateOkawa TakeshiAinda não há avaliações
- 765 p1+2+3 Guide Limta Mock 2022Documento8 páginas765 p1+2+3 Guide Limta Mock 2022Théophile MbameAinda não há avaliações
- 159 SnackDocumento97 páginas159 SnackGuy PlaterAinda não há avaliações
- Macedonian KavalDocumento1 páginaMacedonian Kavalmikiszekely1362Ainda não há avaliações
- Final Project ReportDocumento83 páginasFinal Project ReportMohit SrivastavaAinda não há avaliações
- Website Catalog MOTORS v2 PDFDocumento8 páginasWebsite Catalog MOTORS v2 PDFИгорь КернякевичAinda não há avaliações
- X Glo LED Strip Lighting For Tunnelling BrochureDocumento6 páginasX Glo LED Strip Lighting For Tunnelling BrochureJOSE HUAMANIAinda não há avaliações
- BFE II ScenariosDocumento25 páginasBFE II Scenarioselmitxel100% (1)
- .... Applicant Versus: Cri. Appln. No. 4353/16 & Anr. 1Documento11 páginas.... Applicant Versus: Cri. Appln. No. 4353/16 & Anr. 1Manashree EngineerAinda não há avaliações
- Backlash SDPDocumento11 páginasBacklash SDPPatrick Cyr GagnéAinda não há avaliações
- Earthing ResistanceDocumento4 páginasEarthing ResistanceNeeraj Purohit100% (1)
- Big Fat Lies - How The Diet Industry Is Making You Sick, Fat & PoorDocumento212 páginasBig Fat Lies - How The Diet Industry Is Making You Sick, Fat & PoorangelobuffaloAinda não há avaliações
- Anatomia Dezvoltarii PancreasuluiDocumento49 páginasAnatomia Dezvoltarii Pancreasuluitarra abuAinda não há avaliações
- Curvature CorrectionDocumento7 páginasCurvature CorrectionE J SAinda não há avaliações
- Manual Elspec SPG 4420Documento303 páginasManual Elspec SPG 4420Bairon Alvira ManiosAinda não há avaliações