Escolar Documentos
Profissional Documentos
Cultura Documentos
Cases Illustrating Problems With Intensive Insulin Therapy For Diabetes Mellitus
Enviado por
luisecmeTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Cases Illustrating Problems With Intensive Insulin Therapy For Diabetes Mellitus
Enviado por
luisecmeDireitos autorais:
Formatos disponíveis
6/6/2014
Cases illustrating problems with intensive insulin therapy for diabetes mellitus
Official reprint from UpToDate
www.uptodate.com 2014 UpToDate
Cases illustrating problems with intensive insulin therapy for diabetes mellitus
Author
David K McCulloch, MD
Section Editor
David M Nathan, MD
Deputy Editor
Jean E Mulder, MD
All topics are updated as new evidence becomes available and our peer review process is complete.
Literature review current through: May 2014. | This topic last updated: Dec 13, 2013.
INTRODUCTION The following cases illustrate some of the common problems that may arise during intensive
insulin therapy in patients with type 1 diabetes mellitus. (See "Insulin therapy in adults with type 1 diabetes
mellitus".)
LACK OF CONTROL DUE TO DIET A 57-year-old hospital administrator who has had type 1 diabetes for 15
years is trying very hard to maintain strict glycemic control. She keeps fit with exercise, and adjusts not only her
insulin dose but also her food intake and exercise pattern in response to her blood glucose concentrations.
Her usual insulin doses are:
Before breakfast 6 units regular insulin and 26 units NPH insulin
Before lunch 4 units regular insulin
Before evening meal 4 units regular insulin
Before bedtime 26 units NPH insulin
She is frustrated at the unpredictability of her blood glucose values, as shown below (in mg/dL and, in parentheses,
mmol/L).
Day
Before
breakfast
Before
lunch
Before
evening meal
Before
bedtime
1
2
3
195 (10.8)
61 (3.4)
287 (15.9)
52 (2.9)
46 (2.6)
222 (12.3)
126 (7.0)
210 (11.7)
161 (8.9)
88 (4.9)
197 (10.9)
72 (4.0)
Interpretation and approach This patient is probably trying too hard. If a person continually adjusts insulin
doses, food intake, and exercise, it is often impossible to identify patterns that can be corrected. In this woman,
keeping a three-day food record can determine if there are major problems with dietary inconsistency (figure 1). As
can be seen, the woman's total carbohydrate intake and its distribution are markedly different each day. This
variability prevents the attainment of strict glycemic control with an intensive insulin regimen.
You can attempt to correct the dietary inconsistency by advising her to consult a nutritionist or to attend a diet
workshop, which can be set up for 6 to 10 patients at a time [1]. At these workshops, approximately 10 to 12
meals are laid out, including breakfasts, fast food lunches, fancy evening meals, and snacks. Patients are asked to
estimate how many grams of carbohydrate are in each meal. Their (and clinicians') estimates are often remarkably
inaccurate, but can improve with training. Once this has been achieved, it is then possible to develop a Consistent
Carbohydrate Profile for each patient. The patient can quote this profile to you at every clinic visit and, more
importantly, it becomes part of their conscious behavior at meal times. Rather than forcing a patient to eat the
same amount of carbohydrate at the same meal every day with a fixed dose of insulin, some patients can be taught
to calculate a carbohydrate:insulin ratio. As an example, this patient may need 1 unit of regular insulin to cover 15
http://www.uptodate.com/contents/cases-illustrating-problems-with-intensive-insulin-therapy-for-diabetes-mellitus?topicKey=ENDO%2F1797&elapsedTimeMs
1/14
6/6/2014
Cases illustrating problems with intensive insulin therapy for diabetes mellitus
g of carbohydrate. Although she typically eats 90 g of carbohydrate for breakfast (and so takes 6 units of regular
insulin), if she ate only 30 g on one morning, she would reduce her regular insulin dose to 2 units. She might then
use an insulin algorithm to adjust this basic dose based on her blood glucose concentration (see below).
BEDTIME HYPERGLYCEMIA A 27-year-old woman with type 1 diabetes is treated with the following regimen:
Before breakfast 8 units insulin aspart and 20 units insulin detemir
Before evening meal 4 units aspart
Before bedtime 12 units detemir
Her blood glucose values (in mg/dL and, in parentheses, mmol/L) are as follows:
Day
Before
breakfast
1
2
3
86 (4.8)
146 (8.1)
111 (6.2)
Before
lunch
Before
evening meal
104 (5.8)
123 (6.8)
97 (5.4)
96 (5.3)
105 (5.8)
92 (5.1)
Before
bedtime
320 (17.8)
296 (16.4)
341 (18.9)
Interpretation and approach The main problem with her current level of glycemic control is hyperglycemia
before bedtime. This can probably be improved by increasing the dose of insulin aspart before her evening meal. It
is also prudent to consider some other aspects of her lifestyle. As an example, she may be eating her evening
meal very late, so that there is not much time between the meal and her bedtime test. Furthermore, the evening
meal may be her biggest meal of the day. It would therefore be helpful to review her food record to see how she
distributes her food and what type of food she is eating.
MORNING HYPERGLYCEMIA A 24-year-old insurance salesman with type 1 diabetes for two years feels
stressed and tired at work and has early morning headaches. His hemoglobin A1C (A1C) value is 9.6 percent. Until
fairly recently, he thought that his diabetes was well controlled. His current regimen is:
Before breakfast 6 units regular insulin and 28 units NPH insulin
Before evening meal 4 units regular insulin and 16 units NPH insulin
Blood glucose values (in mg/dL and, in parentheses, mmol/L) are:
Day
Before
breakfast
(8 AM)
1
2
3
282 (15.7)
321 (17.8)
280 (15.6)
Before
lunch
(12 PM)
140 (7.8)
163 (9.1)
153 (8.5)
Before
snack
(1:30 PM)
261 (14.5)
294 (16.3)
310 (17.2)
Before
evening meal
(5 PM)
Before
bedtime
(11 PM)
82 (4.6)
96 (5.3)
107 (5.9)
130 (7.3)
123 (6.8)
144 (8.0)
Interpretation and approach The increasing difficulty in maintaining glycemic control in this patient with
recent-onset diabetes is probably due in part to a progressive decline in endogenous insulin secretion. In addition,
his insulin regimen is not ideal: he is taking too little regular insulin and too much NPH insulin. As an example, his
high blood glucose values at 1:30 PM suggest that he needs to take regular insulin before lunch.
On the other hand, the triad of reasonable blood glucose values before bedtime, very high fasting values before
breakfast, and a history of tiredness and early morning headache suggest a problem with the NPH insulin dose that
he is taking before his evening meal. The action of the NPH insulin may be maximal in the late evening and middle
of the night (causing both normoglycemia at bedtime and nocturnal hypoglycemia) and then dissipating in the
early morning (causing hyperglycemia before breakfast) [2].
The hypothesis that nocturnal hypoglycemia leads to fatigue and decreased well-being was tested in a study of 10
http://www.uptodate.com/contents/cases-illustrating-problems-with-intensive-insulin-therapy-for-diabetes-mellitus?topicKey=ENDO%2F1797&elapsedTimeMs
2/14
6/6/2014
Cases illustrating problems with intensive insulin therapy for diabetes mellitus
patients with type 1 diabetes who were evaluated on the morning after experimentally-induced nocturnal
hypoglycemia (for one hour at 41 mg/dL [2.3 mM]) and on a control night when hypoglycemia was avoided [3].
Symptoms of well-being and fatigue were significantly worse after the night of hypoglycemia, although higher
cerebral function was unchanged.
The presence of nocturnal hypoglycemia followed by early morning hyperglycemia can be confirmed by measuring
blood glucose at 3 AM. One solution is to move his evening dose of NPH insulin from before the evening meal to
before bedtime. Another approach might be to switch from NPH insulin to an insulin with a longer, flatter profile
(such as insulin glargine or detemir). In addition, other aspects of his lifestyle should also be evaluated:
He may not be eating enough carbohydrate in his evening meal or late night snack.
Alternatively, the type of food he is eating may be inadequate to maintain his blood glucose concentration
through the night. A bedtime snack that is low in protein, fat, and fiber may be entirely digested and absorbed
within two or three hours.
A review of his exercise patterns in the evening may also be helpful. Vigorous exercise at that time makes it
more likely that his blood glucose concentration will fall to low values during the night.
The following changes in his insulin regimen lead to marked improvement in his glycemic control:
8 units insulin glulisine and 30 units insulin glargine before breakfast
6 units glulisine before lunch
8 units glulisine before the evening meal
Three months later his blood glucose values (in mg/dL and, in parentheses, mmol/L) are:
Day
Before
Before
breakfast lunch
Before
snack
Before
Before
evening meal bedtime
1
2
3
141 (7.7)
121 (6.7)
150 (8.3)
161 (8.9)
134 (7.4)
110 (6.2)
82 (4.6)
96 (5.3)
107 (5.9)
110 (6.2)
163 (9.1)
153 (8.5)
3 AM
140 (7.8) 92 (5.1)
93 (5.2)
144 (8.0) 104 (5.9)
His A1C value is now 7.8 percent. He has more energy, the headaches are gone, he is eating and exercising
consistently, and has just been promoted because of his improved productivity. To reduce his A1C value to below
7.0 percent, he will probably require a pre-meal insulin algorithm. (See "Blood glucose self-monitoring in
management of adults with diabetes mellitus".)
INSULIN ALGORITHM A 43-year-old factory worker is striving for strict glycemic control with three injections of
insulin per day. Her blood glucose concentrations are somewhat variable due to alterations in her food intake and
exercise program. She is interested in using an insulin algorithm. Her current regimen consists of:
Before breakfast 8 units regular insulin and 15 units NPH insulin
Before dinner 7 units regular insulin
Before bedtime 8 units NPH insulin
Her blood glucose values (in mg/dL and, in parentheses, mmol/L) are as follows:
Day
Before
breakfast
1
2
3
159 (8.8)
117 (6.5)
102 (5.7)
Before
lunch
134 (7.4)
164 (9.1)
122 (6.8)
Before
evening meal
186 (10.3)
210 (11.7)
261 (14.5)
Before
bedtime
84 (4.7)
97 (5.4)
79 (4.4)
http://www.uptodate.com/contents/cases-illustrating-problems-with-intensive-insulin-therapy-for-diabetes-mellitus?topicKey=ENDO%2F1797&elapsedTimeMs
3/14
6/6/2014
Cases illustrating problems with intensive insulin therapy for diabetes mellitus
Interpretation and approach Her blood glucose concentrations vary before breakfast, lunch, and her evening
meal (dinner). She should therefore adjust her doses of regular insulin according to an insulin algorithm (table 1).
The algorithm is designed specifically for each patient. Different patients vary in how much the insulin doses need
to be changed and what blood glucose values will be used to guide the changes. Some patients, as an example,
need much smaller adjustments than others (see 'Late morning hyperglycemia' below).
She should not take extra insulin before bedtime, and should not adjust her doses of NPH insulin.
If this algorithm were applied to her current insulin regimen, then the alterations in her dose of regular insulin on day
1 according to the blood glucose concentration would be:
Day 1:
Before breakfast 159 mg/dL (8.8 mmol/L); add 1 unit regular insulin to total dose of 9 units
Before lunch 134 mg/dL (7.4 mmol/L); no insulin dose
Before dinner 186 mg/dL (10.3 mmol/L); add 2U regular insulin to total dose of 9 units
Before bedtime 84 mg/dL (4.7 mmol/L); no change
Similar adjustments would be made on subsequent days until glycemic control is attained. She could also consider
using a carbohydrate:insulin ratio to allow her to take less food and less insulin at certain meals.
VARIABLE GLYCEMIC CONTROL A 32-year-old executive has a busy office job that is unpredictable in terms
of physical activity, time of meals, or the length of the workday. Her current insulin regimen is:
Before breakfast 4 units regular insulin and 10 units NPH insulin
Before evening meal 8 units regular insulin and 14 units NPH insulin
Her blood glucose records (in mg/dL or, in parentheses, in mmol/L) for one week are as follows. The asterisk refers
to hypoglycemic episodes and A refers to average values during the week.
Day
1
2
3
4
5
6
7
A
Before
breakfast
156 (8.7)
147 (8.2)
182 (10.1)
191 (10.6)
165 (9.3)
246 (13.7)
178 (9.9)
181 (10.1)
Before
lunch
Before
evening meal
111 (6.2)
98 (5.4)
124 (7.9)
115 (6.4)
108 (6.0)
89 (4.9)
97 (5.4)
106 (5.9)
97 (5.4)
59* (3.3)
86 (4.8)
46* (2.6)
101 (5.6)
92 (5.1)
67 (3.7)
78 (4.3)
Before
bedtime
63 (3.5)
301 (16.7)
87 (4.7)
62 (3.4)
235 (13.1)
57 (3.3)
164 (9.1)
138 (7.7)
3 AM
91 (5.1)
78 (4.3)
She played racquetball for one hour at 8 PM on day 4 and had a late night pizza at 11 PM on day 5.
Interpretation and approach Evaluation of this patient's records can be best approached by considering each
time period separately:
Before breakfast Her average blood glucose value before breakfast is too high at 181 mg/dL (10.1 mmol/L).
The individual values are also fairly consistent (from 147 to 191 mg/dL [8.2 to 10.6 mmol/L]) apart from one
high value (246 mg/dL [13.7 mmol/L]) on day 5, which can probably be explained by her late-night pizza the
preceding day [4].
This patient should benefit from increasing her NPH insulin dose before the evening meal, since this is the
insulin that is working during the night. However, her two 3 AM values are in the ideal range. There is therefore
http://www.uptodate.com/contents/cases-illustrating-problems-with-intensive-insulin-therapy-for-diabetes-mellitus?topicKey=ENDO%2F1797&elapsedTimeMs
4/14
6/6/2014
Cases illustrating problems with intensive insulin therapy for diabetes mellitus
a risk that increasing her evening NPH insulin dose will induce nocturnal hypoglycemia. This risk can be
minimized by increasing her evening NPH insulin in small increments and continuing to measure blood
glucose both at 3 AM and before breakfast. Another approach is to have her take her evening dose of NPH
insulin at bedtime, instead of before the evening meal. She could also be switched to insulin detemir or insulin
glargine.
Before lunch Her before-lunch blood glucose values are consistent and average 106 mg/dL (5.9 mmol/L).
This is very good control, suggesting that her morning dose of regular insulin and her breakfast and midmorning snacks are appropriate and consistent from day to day and that her exercise and work schedule for
the morning are relatively constant. However, she may be in danger of hypoglycemia before lunch once her
before breakfast glucose values are lowered as recommended above. It might therefore be wise to slightly
decrease her morning regular insulin dose as the evening NPH insulin dose is increased.
Before evening meal Her before evening meal blood glucose values are too low, with an average value of 78
mg/dL (4.3 mmol/L) and two hypoglycemic episodes during the week. These findings suggest that she may
be taking too much NPH insulin before breakfast, since this is the insulin that is acting during the afternoon.
Another possible explanation might be that her lunch is too early or too light, or that she doesn't eat an
adequate mid-afternoon snack. There is inadequate information to identify the primary problem.
Before bedtime Her before bedtime blood glucose values average 138 mg/dL (7.7 mmol/L). While this
average is close to ideal, the individual values vary widely from 57 to 301 mg/dL (3.2 to 16.7 mmol/L). This
suggests that some variable aspect of her lifestyle is creating the fluctuations in the bedtime glucose values.
Possible problems include variation in the time or content of her evening meal or in evening exercise. As an
example, the blood glucose value of 301 mg/dL (16.7 mmol/L) before bedtime on day 2 may have resulted
from dietary overcompensation for her hypoglycemic episode before the evening meal.
In summary, this patient's record keeping is better than most. Nevertheless, it is not sufficient to permit
assessment of her problems before the evening meal and before bedtime. It would be helpful to know the exact
times when her blood glucose was measured and exactly when she eats and the content of each meal.
LATE AFTERNOON HYPOGLYCEMIA A 42-year-old garage mechanic is treated with the following insulin
regimen:
Before breakfast 8 units insulin lispro and 16 units insulin glargine
Before lunch 4 units lispro
Before evening meal 10 units lispro and 22 units glargine
He uses an algorithm (table 2) to adjust pre-meal doses of lispro insulin.
Blood glucose values (in mg/dL or, in parentheses, mmol/L) for one week are shown below. The doses of lispro (LP)
and glargine (G) insulin are also noted. The asterisks on days 2 and 4 reflect hypoglycemic episodes.
Day
Before
breakfast
Before
lunch
Before
evening meal
Before
bedtime
100 (5.6)
8 LP, 16 G
205 (11.4)
8 LP
116 (6.4)
115 (6.4)
10 LP, 22 G
118 (6.6)
8 LP, 16 G
172 (9.6)
7 LP
47* (2.6)
124 (6.9)
8 LP, 22 G
77 (4.3)
6 LP, 16 G
145 (8.1)
4 LP
85 (4.7)
108 (6.0)
10 LP, 22 G
113 (6.3)
136 (7.6)
54* (3.0)
3 AM
92 (5.1)
111 (6.2)
http://www.uptodate.com/contents/cases-illustrating-problems-with-intensive-insulin-therapy-for-diabetes-mellitus?topicKey=ENDO%2F1797&elapsedTimeMs
5/14
6/6/2014
Cases illustrating problems with intensive insulin therapy for diabetes mellitus
8 LP, 16 G
5 LP
132 (7.3)
9 LP, 16 G
97 (5.4)
4 LP
98 (5.4)
8 LP, 16 G
122 (6.8)
5 LP
158 (8.8)
109 (6.1)
8 LP, 16 G
4 LP
9:55 AM (late)
114 (6.3)
141 (7.8)
8 LP, 22 G
103 (5.7)
97 (5.4)
10 LP, 22 G
87 (4.8)
82 (4.6)
102 (5.7)
10 LP, 22 G
93 (5.2)
89 (4.9)
10 LP, 22 G
83 (4.6)
107 (5.9)
Interpretation and approach This patient's record is quite complete, but there is no information about the
quantity of food eaten and periods of exercise. He is consistent about the timing of blood glucose testing and meals
and has adjusted his insulin doses correctly using the algorithm. He made only one "mistake." His blood glucose
was measured between 7:05 and 7:15 AM every day except for day seven when he slept late and the test was done
at 9:55 AM. According to the algorithm, he should have increased the dose of lispro insulin by 2U to 10U for a blood
glucose value of 158 mg/dL (8.8 mmol/L). Several other patterns can be detected:
He needed to take extra insulin before lunch on four of the seven days. This suggests that his pre-breakfast
dose of lispro insulin may be too low or that his mid-morning snack is too large or taken too close to lunch.
His average blood glucose value is too low (83 mg/dL [4.6 mmol/L]) before the evening meal, with
hypoglycemia occurring on days two and four. Possible explanations include a morning dose of insulin
glargine or lunchtime dose of lispro insulin that is too high, or an inadequate midafternoon snack.
His blood glucose values before bedtime and at 3 AM are normal.
LATE MORNING HYPERGLYCEMIA A 21-year-old woman is 62 inches (157 cm) tall and weighs 104 lb (47 kg).
She runs 40 miles per week. She is being treated with a continuous subcutaneous insulin infusion (CSII) according
to the following insulin regimen. (See "Insulin therapy in adults with type 1 diabetes mellitus".)
Basal infusion rate 0.4 units/hour
Pre-breakfast bolus dose 3 units
Pre-lunchtime bolus dose 2 units
Pre-evening meal bolus dose 4 units
She adjusts the pre-meal bolus doses according to the following algorithm (table 3).
She has kept a three-day record of her glycemic control, with the doses of regular insulin shown under the blood
glucose values. The time of the pre-meal measurements is roughly constant from day to day.
Day
Before
breakfast
Before
lunch
mg/dL
Before
evening meal
(mmol/L)
Before
bedtime
105 (5.7)
3 units
195 (10.8)
3.5 units
146 (8.1)
5 units
125 (6.9)
112 (6.2)
3 units
122 (6.8)
2.5 units
147 (8.2)
5 units
94 (5.2)
77 (4.3)
2 units
186 (10.3)
3.5 units
165 (9.2)
5.5 units
108 (6.0)
3 AM
89 (4.9)
http://www.uptodate.com/contents/cases-illustrating-problems-with-intensive-insulin-therapy-for-diabetes-mellitus?topicKey=ENDO%2F1797&elapsedTimeMs
6/14
6/6/2014
Cases illustrating problems with intensive insulin therapy for diabetes mellitus
Interpretation and approach This patient's records are complete with regard to time, blood glucose values,
and insulin doses. She is consistent in terms of blood glucose testing and timing of meals, but we do not have
information about the size and number of meals or the timing of exercise. This consistency is reflected in the
relatively constant blood glucose levels at each time of day. She is appropriately increasing her before-lunch and
before-evening meal bolus insulin doses, since her blood glucose values are elevated only at those times. The fact
that she has to add insulin every day before lunch suggests that some adjustment may be needed in her overall
regimen during the morning. She may need a larger pre-breakfast dose of insulin, a smaller breakfast or midmorning snack, or an increase in her basal rate of insulin infusion. She could also consider using a
carbohydrate:insulin ratio to allow her to take less food and less insulin at certain meals. It would also help if she
switched from using regular insulin to insulin aspart in her pump.
EVENING HYPERGLYCEMIA A 34-year-old teacher is striving for excellent glycemic control. He eats a healthy
diet, counts carbohydrates, exercises at a consistent time each day, and has been taking the following regimen:
Before breakfast (6 AM) 4 units insulin aspart and 14 units NPH
Before lunch 4 units insulin aspart
Before evening meal (6 PM) 6 units insulin aspart and 14 units NPH insulin
Doses of insulin aspart are also adjusted using an insulin algorithm.
Because of nocturnal hypoglycemia and unexplained variation in blood glucose concentrations before the evening
meal, NPH insulin was stopped and replaced with a single dose of 28 units insulin glargine taken at 10 PM. Doses
of insulin aspart remained the same. Typical blood glucose concentrations (in mg/dL and, in parentheses, mmol/L)
a few weeks later are:
Day Before breakfast Before lunch Before evening meal Before bed
(6 AM)
1
2
3
107 (5.9)
130 (7.3)
140 (7.8)
(11 AM)
123 (6.8)
111 (6.2)
144 (8.0)
(6 PM)
163 (9.1)
146 (8.1)
178 (9.9)
(10 PM)
296 (16.4)
210 (11.7)
261 (14.5)
Interpretation and approach Blood glucose values are ideal before breakfast and lunch, but are somewhat
high before the evening meal and are much too high before bedtime. Since he has not changed his eating habits or
doses of insulin aspart, it is likely that the effect of the insulin glargine is waning after 20 hours. He could try
increasing the dose of insulin glargine or splitting it into two equal doses taken about 12 hours apart. Alternatively,
he could increase the dose of insulin aspart before the evening meal.
SWITCHING FROM NPH INSULIN TO INSULIN DETEMIR A 33-year-old man with type 1 diabetes is treated
with the following regimen:
Before breakfast 28 units NPH insulin
Before bedtime 12 units NPH insulin
He also administers insulin aspart by sliding scale before each meal.
Despite being extremely consistent from day-to-day in his activity level and in the timing and carbohydrate content
of his meals, he is having unpredictable swings in blood glucose concentrations with occasional episodes of
hypoglycemia in the late morning or early afternoon.
Blood glucose values (in mg/dL and, in parentheses, mmol/L) are:
Day Before breakfast Before lunch Before evening meal Before bed
http://www.uptodate.com/contents/cases-illustrating-problems-with-intensive-insulin-therapy-for-diabetes-mellitus?topicKey=ENDO%2F1797&elapsedTimeMs
7/14
6/6/2014
Cases illustrating problems with intensive insulin therapy for diabetes mellitus
(8 AM)
1
2
3
4
(12 PM)
132 (7.3)
119 (6.6)
141 (7.8)
108 (6.0)
54 (3.0)*
136 (7.6)
108 (6.0)
48 (2.7)*
(5 PM)
206 (11.4)
140 (7.8)
125 (6.9)
196 (10.9)
(11 PM)
118 (6.6)
151 (8.4)
107 (5.9)
140 (7.8)
*Represent episodes of symptomatic hypoglycemia.
In order to change from NPH to insulin detemir his total daily dose of NPH is calculated (28 + 12 = 40), decreased
by 10 percent (4 units), and is given as a single injection of 36U of detemir insulin at bedtime.
One week later his blood glucose values (in mg/dL and, in parentheses, mmol/L) are:
Day Before breakfast Before lunch Before evening meal Before bed
(8 AM)
1
2
3
4
(12 PM)
98 (5.4)
103 (5.7)
217 (12.1)*
92 (5.1)
124 (6.9)*
131 (7.3)
127 (7.0)
119 (6.6)*
(5 PM)
168 (9.3)
171 (9.5)
192 (10.7)
185 (10.3)
(11 PM)
213 (11.8)
232 (12.9)
251 (13.9)
211 (11.7)
*He was awakened with hypoglycemia at 4 AM and took 60 grams of carbohydrate to treat this.
Interpretation and approach His blood glucose values before breakfast on days 1, 2 and 4 are slightly low.
That, along with one episode of hypoglycemia at 4 AM, suggests that 36 units of insulin detemir may be too much
for him. The blood glucose values before lunch are ideal, but they are too high before dinner and even higher before
bedtime. This suggests that insulin detemir is not lasting 24 hours, but that its action wanes after 18 to 20 hours.
After switching to 20 units insulin detemir twice daily (at about 8 AM and 8 PM) his blood glucose values became
stable throughout the day.
While many patients do well with a single dose of insulin detemir at bedtime, this case illustrates two practical
points. Although its peak action is less than that of NPH insulin, it can have a slight peak in some patients which
may result in hypoglycemia during the night [5]. Also, although it lasts for 24 hours in some patients, some
patients require two daily injections (figure 2).
Use of UpToDate is subject to the Subscription and License Agreement.
REFERENCES
1. McCulloch DK, Mitchell RD, Ambler J, Tattersall RB. Influence of imaginative teaching of diet on compliance
and metabolic control in insulin dependent diabetes. Br Med J (Clin Res Ed) 1983; 287:1858.
2. Gale EA, Tattersall RB. Unrecognised nocturnal hypoglycaemia in insulin-treated diabetics. Lancet 1979;
1:1049.
3. King P, Kong MF, Parkin H, et al. Well-being, cerebral function, and physical fatigue after nocturnal
hypoglycemia in IDDM. Diabetes Care 1998; 21:341.
4. Ahern JA, Gatcomb PM, Held NA, et al. Exaggerated hyperglycemia after a pizza meal in well-controlled
diabetes. Diabetes Care 1993; 16:578.
5. Heise T, Nosek L, Rnn BB, et al. Lower within-subject variability of insulin detemir in comparison to NPH
insulin and insulin glargine in people with type 1 diabetes. Diabetes 2004; 53:1614.
Topic 1797 Version 5.0
http://www.uptodate.com/contents/cases-illustrating-problems-with-intensive-insulin-therapy-for-diabetes-mellitus?topicKey=ENDO%2F1797&elapsedTimeMs
8/14
6/6/2014
Cases illustrating problems with intensive insulin therapy for diabetes mellitus
GRAPHICS
Erratic carbohydrate intake prevents glycemic control
Carbohydrate (CHO) profiles from 6 AM to 12 AM on two consecutive days in
a 57 year-old woman with fluctuating blood glucose concentrations (shown,
in mg/dL, by the numbers in the graphs). Each column represents the CHO
intake at a meal or snack. Both the total CHO intake and the distribution of
CHO intake vary markedly, a change that was even more marked on the day
3 when total CHO intake was 267 grams (not shown). The asterisk on day 1
indicates mild hypoglycemic symptoms at that time. To convert blood glucose
values to mmol/L multiply by 0.056.
Graphic 60634 Version 1.0
http://www.uptodate.com/contents/cases-illustrating-problems-with-intensive-insulin-therapy-for-diabetes-mellitus?topicKey=ENDO%2F1797&elapsedTimeMs
9/14
6/6/2014
Cases illustrating problems with intensive insulin therapy for diabetes mellitus
Insulin algorithm: Regular insulin, example 1
Blood glucose values
mg/dL
mmol/L
Change in dose, units
of regular insulin
<70
<3.9
-2R
70 to 140
4.4 to 6.7
0 R
141 to 160
7.8 to 8.9
+1 R
161 to 200
8.9 to 11.1
+2 R
201 to 240
11.4 to 13.3
+3 R
>240
>11.3
+4 R
Graphic 83951 Version 1.0
http://www.uptodate.com/contents/cases-illustrating-problems-with-intensive-insulin-therapy-for-diabetes-mellitus?topicKey=ENDO%2F1797&elapsedTimeM
10/14
6/6/2014
Cases illustrating problems with intensive insulin therapy for diabetes mellitus
Insulin algorithm: Lispro insulin
Blood glucose values
mg/dL
mmol/L
Change in dose, units
of insulin lispro
<80
<4.4
- 2 units
80 to 120
4.4 to 6.7
0 units
121 to 140
6.7 to 7.8
+ 1 units
141 to 160
7.8 to 8.9
+ 2 units
161 to 200
8.9 to 11.1
+ 3 units
>200
>11.1
+ 4 units
Graphic 83953 Version 1.0
http://www.uptodate.com/contents/cases-illustrating-problems-with-intensive-insulin-therapy-for-diabetes-mellitus?topicKey=ENDO%2F1797&elapsedTimeM
11/14
6/6/2014
Cases illustrating problems with intensive insulin therapy for diabetes mellitus
Insulin algorithm: Regular insulin, example 2
Blood glucose values
mg/dL
mmol/L
Change in dose, units
of regular insulin
<80
<4.4
-1R
80 to 120
4.4 to 6.7
0 R
121 to 140
6.7 to 7.8
+ 0.5 R
141 to 160
7.8 to 8.9
+1 R
161 to 200
8.9 to 11.1
+ 1.5 R
>200
>11.1
+2 R
Graphic 83952 Version 1.0
http://www.uptodate.com/contents/cases-illustrating-problems-with-intensive-insulin-therapy-for-diabetes-mellitus?topicKey=ENDO%2F1797&elapsedTimeM
12/14
6/6/2014
Cases illustrating problems with intensive insulin therapy for diabetes mellitus
Variation in pharmacokinetics of insulin detemir
Variation in pharmacokinetics of insulin detemir among six individuals given the
same dose on four separate occasions (note significant peak effect at 8 to 12
hours and duration well short of 24 hours in some patients).
Data from: Heist T, Nosek L, Ronn BB, et al. Lower within-subject variability of insulin
detemir in comparison to NPH insulin and insulin glargine in people with type 1 diabetes.
Diabetes 2004; 53:1614.
Graphic 64125 Version 2.0
http://www.uptodate.com/contents/cases-illustrating-problems-with-intensive-insulin-therapy-for-diabetes-mellitus?topicKey=ENDO%2F1797&elapsedTimeM
13/14
6/6/2014
Cases illustrating problems with intensive insulin therapy for diabetes mellitus
Disclosures
Disclosures: David K McCulloch, MD Nothing to disclose. David M Nathan, MD Nothing to disclose. Jean E Mulder, MD Employee of
UpToDate, Inc.
Contributor disclosures are review ed for conflicts of interest by the editorial group. When found, these are addressed by vetting through
a multi-level review process, and through requirements for references to be provided to support the content. Appropriately referenced
content is required of all authors and must conform to UpToDate standards of evidence.
Conflict of interest policy
http://www.uptodate.com/contents/cases-illustrating-problems-with-intensive-insulin-therapy-for-diabetes-mellitus?topicKey=ENDO%2F1797&elapsedTimeM
14/14
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Hemodialysis Patient's Endorsement FormDocumento1 páginaHemodialysis Patient's Endorsement FormHacienda Galea Resort and Events Place100% (1)
- Appendix 3 Examples of Dilutions of Anaesthetic Mixtures For Small Rodents 2016 Laboratory Animal Anaesthesia Fourth EditionDocumento4 páginasAppendix 3 Examples of Dilutions of Anaesthetic Mixtures For Small Rodents 2016 Laboratory Animal Anaesthesia Fourth EditionAlejandra CárdenasAinda não há avaliações
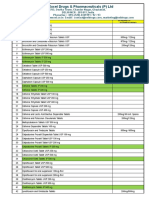
- Generic Medicines PricelistDocumento15 páginasGeneric Medicines PricelistJoseph Michael Vitug100% (1)
- Activity 6 Online Resources RetrievalDocumento4 páginasActivity 6 Online Resources RetrievalHazel Jane AquinoAinda não há avaliações
- Extravasation Management ProtocolDocumento1 páginaExtravasation Management ProtocolThắng NguyễnAinda não há avaliações
- Session 08 EctDocumento23 páginasSession 08 EctMalakatete Mwaipojele-fAinda não há avaliações
- Medisiddh Pharma Private Limited 971A/6, Thirumal Nagar, Near K.R Arts College-Nh7, Kovilpatti-628503 LICENSE NO: 490/25DDocumento2 páginasMedisiddh Pharma Private Limited 971A/6, Thirumal Nagar, Near K.R Arts College-Nh7, Kovilpatti-628503 LICENSE NO: 490/25Dhk_scribdAinda não há avaliações
- TDM of Valproic AcidDocumento43 páginasTDM of Valproic Acidryo_ninukAinda não há avaliações
- Barcode List FinalDocumento6 páginasBarcode List FinalMhammad NaveedAinda não há avaliações
- QRG Morpheus8 BODY February 2021 (TIPS)Documento2 páginasQRG Morpheus8 BODY February 2021 (TIPS)JWAinda não há avaliações
- Care Homes - Good Practice Guidance Expiry Dates For MedicationDocumento1 páginaCare Homes - Good Practice Guidance Expiry Dates For MedicationafrizalsyahyeriAinda não há avaliações
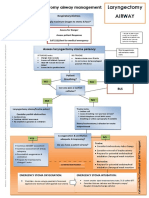
- Laryngectomy Airway: Emergency Tracheostomy Airway ManagementDocumento1 páginaLaryngectomy Airway: Emergency Tracheostomy Airway ManagementDana IlieAinda não há avaliações
- Inform Concent Actemra 1Documento2 páginasInform Concent Actemra 1lukiharjantiAinda não há avaliações
- RJPDocumento38 páginasRJPjoyfullAinda não há avaliações
- Major and Minor TranquilizerDocumento6 páginasMajor and Minor TranquilizerAli IjazAinda não há avaliações
- JunaidDocumento41 páginasJunaidShobhit GoswamiAinda não há avaliações
- Case 11 J&J Again Recalls Thousands of Faulty Hip ImplantsDocumento2 páginasCase 11 J&J Again Recalls Thousands of Faulty Hip ImplantsShiela Mae Catalan AludoAinda não há avaliações
- Flix o Tide InhalerDocumento5 páginasFlix o Tide InhalerEthik MoesAinda não há avaliações
- Campral (Acamprosate Calcium)Documento1 páginaCampral (Acamprosate Calcium)E100% (1)
- Route of Administration PDFDocumento45 páginasRoute of Administration PDFBurhan MubasharAinda não há avaliações
- Before Taking Losartan,: What Special Dietary Instructions Should I Follow?Documento8 páginasBefore Taking Losartan,: What Special Dietary Instructions Should I Follow?Hillary Ann AbuelAinda não há avaliações
- Drug Interaction MonitoringDocumento5 páginasDrug Interaction MonitoringAnonymousAinda não há avaliações
- Routes of Drug AdministrationDocumento34 páginasRoutes of Drug AdministrationNa SyaAinda não há avaliações
- Nacromin Eye DropsDocumento2 páginasNacromin Eye DropsAnamul hossainAinda não há avaliações
- Test Bank For Drug Calculations Ratio and Proportion Problems For Clinical Practice 9th Edition BrownDocumento19 páginasTest Bank For Drug Calculations Ratio and Proportion Problems For Clinical Practice 9th Edition BrownGraceLopezyfmox100% (37)
- Successful Treatment of Amoxapine Induced IntractaDocumento5 páginasSuccessful Treatment of Amoxapine Induced IntractaNatasha Vera100% (1)
- New Checklist Trolley Emergency Icu Revisi 12 Okt 2021Documento4 páginasNew Checklist Trolley Emergency Icu Revisi 12 Okt 2021Laras TriAinda não há avaliações
- Rituximab TrialDocumento9 páginasRituximab TrialsrildaAinda não há avaliações
- A Guide To Calculating Parenteral Nutrition When T-2 - 1Documento2 páginasA Guide To Calculating Parenteral Nutrition When T-2 - 1Steve JacobAinda não há avaliações
- VXL-List of Pharma Products (Domestic and Export)Documento10 páginasVXL-List of Pharma Products (Domestic and Export)Singh PushpanjaliAinda não há avaliações