Escolar Documentos
Profissional Documentos
Cultura Documentos
Ulcerative Conditons
Enviado por
Victoria GoDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Ulcerative Conditons
Enviado por
Victoria GoDireitos autorais:
Formatos disponíveis
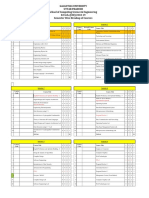
ULCERATIVE CONDITONS
By NAVARRA, NICOLAS, OCLIASO, OLMEDO,
ONG, PABLO
Transmitted most often through sexual
contact with an infected person
Other transmission is through body
fluids and childbirth
Reactive Lesions
Traumatic Ulcerations
Most common kind of ulcer in the
mouth
Break in the mucosa with a shallow
base and non-raised margins
May be diffuse or localized
Aspirin: the most common drug that
can cause ulceration
Sloughing is usually due to chemical
burns
Remove the cause for the treatment
Clean the area with sterile saline
solution
The "clap" or "drip
Symptoms
1. Greenish yellow or whitish
discharge from the vagina
2. Lower abdominal or pelvic pain
3. Burning when urinating
4. Conjunctivitis (red, itchy eyes)
5. Bleeding between periods
6. Spotting after intercourse
7. Swelling of the vulva (vulvitis)
8. Burning in the throat (due to oral
sex)
9. Swollen glands in the throat (due to
oral sex)
Tuverculosis
Caused by aerobic, nonspore-forming
bacillus
A. M. tuberculosis: air-borne
droplets
Bacterial Infections
B. M. bovis: transmitted via
infected milk of cows
Syphilis
Treponema pallidum.
C. M. avium
Stages of syphilis
D. M. intracellulare
1. Primary: presence of sores which
are hard and painless; occurs in
genitals or around the mouth after
10-90 days exposure; the sore will
heal after 6 weeks
2. Secondary: duration is 1-3 months
that begins within 6 months after
exposure; usually with a rosy
copper penny rash on palms and
sole also moist warts, white
patches and weight loss.
3. Latent: the infection is dormant
4. Tertiary: affects the heart, brain
and nerves.
Gonorrhea
Neisseria gonorrhoeae
Ability to resist degradation by
macrophages and to the development
of a type Iv hypersensitivity reaction
(Mantoux and tine skin test)
Reacts to Ziehl-Neelsen and Fite
technique (acid-fast bacilli)
Implantation of organisms found in
sputum or hematogenous deposition
Indurated, chronic, nonhealing ulcers
that are usually painful; bony
involvement (tuberculous
osteomyelitits)
Granulomtous inflammation showing
caseous necross
Leprosy
Severe, disfiguring skin sores and
nerve damage in the arms and legs.
Aka. Cancrum oris/gangrenous
stomatitis
Mycobacterium leprae; Hansen's
disease
Affects malnourished children (noma
neonatorum: low birth-weight infants)
Fusobacterium necrophorum
The skin sores and pales.
Main symptoms: skin sore, lumps or
bumps
Painful gingival ulcerations (gingival,
buccal), denudation of bone,
exfoliaton of loose teeth, fetid necrotic
lesions
Types
Fluids, electrolytes, general nutrition,
antibiotics
1. Tuberculoid: mild leprosy; one or
a few patches of flat, pale-colored
skin (paucibacillary leprosy);
affected area may feel numb
because of nerve damage; less
contagious than other forms
2. Lepromatous: severe form of the
disease with widespread skin
bumps and rashes (multibacillary
leprosy); numbness, and muscle
weakness; the nose, kidneys,
and male reproductive organs may
also be affected; more contagious
3. Borderline: have symptoms of
both the tuberculoid and
lepromatous forms.
Actinomycosis
Actionomyces israelii, part of the
normal flora in the nose and throat.
Usually triggered by DENTAL ABSCESS
or ORAL SURGERY also by IUD
Lumpy jaw
Symptoms
1. Draining sores in the skin,
especially on the chest wall from
lung infection with Actinomyces
2. Fever
3. Minimal or no pain
4. Swelling or a hard, red to reddishpurple lump on the face or upper
neck
5. Weight loss
Noma
Antibiotics and surgical drainage and
removal of the IUD.
Fungal Infections
Deep Fungal Diseases
Indurated, nonhealing, frequently
painful, chronic ulcer
Usually following implantation of
organism from the lungs
Cause:
1. Histoplasma capsulatum
2. Coccidioidesi immites
Treatment: antifungal drugs
Subcutaneous Fungal Infection:
Sporotrichosis
Sporothrix schenkii
Inoculation of the skin/mucosa by
contaminated soil or thorny plants
Nonspecific chronic ulcers
Granulomatous central abscess,
pseydoepitheliomatous hyperplasia
Solution of potassium iodide,
ketoconazole
Opportunistic Fungal Infection
Infection caused by pathogens,
particularly opportunistic pathogens.
Those that take advantage of certain
situationssuch as bacterial, viral,
fungal or protozoan infections that
usually do not cause disease in a
healthy host, one with a healthy
immune system.
Occurs in compromised host
Necrotic, nonhealing ulcers
Cause:
1. Mucormycosis
2. Rhizopus
Treatment: depends on the type of
opportunistic infection, but usually
involves different antibiotics.
Immunologic Diseases
Behcets Syndrome
Unknown etiology; can be due to
immunodysfunction and genetic
predisposition (prominence of HLAB51)
Ulcers identical to that of aphthous
stomatitis
Magic syndrome <mouth and genital
ulcers with inflamed cartilage>
(Behcets stigmata + recurrent
polychondritis), recurrent arthritis
Prominent T-lymphocytes, PMN
infiltrate in the vessel walls
Immunosuppressive drugs
(chlorambucil, azathioprine)
Aphthous Ulcers
Aka Canker Sores
Recurrent, painful ulcers found on
nonkeratinized oral mucosa (tongue,
vestibular mucosa, floor of the mouth
and facial pillars.)
They are not found on skin, vermillion,
attached gingiva or hard palate.
Usually round or oval
Etiology:
1. May probably an immune defect
mediated by T-cells
2. Precipitated by emotional stress
3. Trauma on oral tissues
4. Diet
5. Hormones
Reiters Syndrome
A triad of nonspecific urethritis,
conjunctivitis, and arthritis
Follows bacterial dysentery or
exposure to a sexually transmissible
disease
Male with HLA-B27 has a 20% risk for
Reiter's disease after an episode of
Shigella dysentery
Acute onset
Occurs predominantly in white men in
their third decade
Oral Manifestations
3 types:
1. Minor:
Most common type
Usually solitary
<0.5 cm in diameter
May heal 1-2 weeks
2. Major:
Very painful; severe
>0.5 cm in diameter
May take several weeks to heal
3. Herpetiform:
Multiple
Recurrent crops of ulcers
Treatment:
1. Tetracycline
2. Corticosteroids
1. Painless aphthous-type ulcers
2. Seen anywhere in the mouth
3. Tongue lesions resemble
geographic tongue
Duration varies from weeks to months,
and recurrences are not uncommon
NSAIDS are generally used as a
treatment
Drug Reactions
Pathogenesis may be related to either
immunologic or nonimmunologic
mechanisms
Allergy
Non-immunologic
Overdose, toxicity, side
effects
Patch testing and history taking may
be helpful for diagnosis.
Biopsy findings may be confirmatory.
Not AB dependent
Treatment:
Clinical Features
1. Elimination of offending
material
2. Topical steroids may hasten the
healing process
Erythema Multiforme
Oral Manifestations
1. Erythematous, vesicular, or
ulcerative
2. Lichenoid drug reactions mimic
erosive lichen planus
Treatment: identification and
withdrawal of the causative agent
Contact with foreign antigen
Toothpaste
Cinnamon
Mouthwash
Denture base material
1. Changes appear rapidly
2. Urticaria, maculopapular rash,
erythema, vesicles, ulcers
3. Acquired angioedema IgEmediated allergic reactions caused
by drugs or foods like nuts and
shellfish
4. Hereditary angioedema rare
autosomal dominant trait with the
deficiency of the first component of
complement C1 esterease
5. Appears as soft, diffuse, painless
swelling (lips, face, neck)
Etiology:
1.
2.
3.
4.
5.
Immunologic
Antihistamines and
corticosteroids for the
management of oral and
cutaneous eruptions
Contact Allergy
Lesions due to direct contact with
foreign antigen.
Erythema, vesicles and ulcers may be
seen
Primarily affects the attached gingiva
as bright red in color
Self-limiting
o
Minor form: HSV trigger (HSV
type I and II), TB,
Histoplasmosis
Major severe form: caused by
systemic drugs (barbiturates,
sulfonamides, carbamazepine,
phenytoin)
A few aphthous-type lesions to
multiple superficial widespread ulcers
in EM major
Stevens-Johnson syndrome: crusting
of lips, superficial ulceration preceded
by bullae
Epithelial hyperplasia and spongiosis,
parabasal apoptotic keratinocytes
Differential diagnosis: Primary HSV
infection, aphthous ulcers, pemphigus
vulgaris, mucous membrane
pemphigoid, erosive lichen planus
Topical corticosteroids with
antifungals, acyclovic (HSV-triggered
disease)
Wegeners Granulomatosis
A rare, serious, systemic,
inflammatory condition of an unknown
etiology
May be inherited or acquired
Oral ulcers with periodicity
Involvement of upper respiratory tract,
lung, and kidney
Infections
Intraoral lesions consist of red,
hyperplastic, granular lesions on the
attached gingiva
1. Adenopathy
2. Periodontal disease
Cause: mutations in neutrophil
elastase gene
Treatment: no ideal therapy for
neutropenia, but recombinant G-CSF
(granulocyte-colony stimulating factor)
such as filgrastim (Neupogen) can be
effective in chemotherapy patients.
Midline Granuloma
A diagnosis made by exclusion of
other granulomatous and necrotizing
midfacial lesions
Unifocal destructive process
Seen in the midline of the oronasal
region
Aggressive necrotic ulcers, progressive
and nonhealing
May extend to soft tissue, cartilage,
and bone
May be treated with local radiation
Chronic Granulomatous Disease
Rare sytemic (X-linked or autosomal
recessive) disease
Defects in the nicotinamide adenine
dinucleotide phosphate (NADPH)
oxidase complex which alters
neutrophils and macrophages function
Manifestations seen during childhood,
more prevalent in males
May affect many organs
Oral lesions are seen in the form of
multiple ulcers that are recurrent or
persistent
Cyclic Neutropenia
Rare blood disorder characterized by
recurrent episodes of abnormally low
levels of neutrophils in the body.
Neoplasms
Maxillary Sinus Carcinoma
Uncommon
Exposure to wood dust
People working in nickel and chrome
industries are more prone; people
working in leather industries
Symptoms of sinusitis or referred pain
to teeth
May cause malocclusion or mobile
teeth
May appear as ulcerative mass in
palate or alveolus.
Treatment:
1.
2.
3.
4.
Surgery
Radiotherapy
Chemotherapy
Combined management
modality
Squamous Cell Carcinoma
Etiology:
1. Tobacco smoking
2. Reverse smoking habit in
India and South American
countries
3. Alcohol adds to risk of oral
cancer
4. Candida albicans carcinogen
N-nitrosobenzylmethylamine
5. UV light
6. Chronic irritation, poor oral
hygiene
Loss of cell cycle control
through increased proliferation
and reduced apoptosis
Increased tumor cell motility
Carcinoma of the Lips
Carcinoma of the Tongue
Most common intraoral
malignancy, 25-40%
Common in men in their 6th, 7th
and 8th decades
Lingual carcinoma
1. Asymptomatic
2. later stages: pain and/or
dysphagia
Presents in one of four ways:
1. Indurated, nonhealing
ulcer
2. Red lesion
3. White lesion
4. Red and white lesion
May be endophytic or exophytic
Posterior-lateral border most
common location; 45% of all
tongue lesions
Posterior 1/3 or base of tongue
25% of lesions
Carcinoma of the Floor of the Mouth
Second most common intraoral
location; 15-20% of all cases
Painless, nonhealing, indurated
ulcer
White or red patch
Infiltrates floor of mouth,
causing decreased tongue
mobility
Metastasis to submandibular
lymph nodes
Pathogenesis: 2 stages
More common in lower lip than
upper lip
Account for 25-30% of all oral
cancers
50-70 years of age; affect men
more often than women
Arise on the vermillion as a
chronic, nonhealing lesion that
is verrucous in nature
Metastasis to submental or
submandibular lymph nodes
with larger lesions
Metastatic deposits are usually
found in the lymph nodes of the
neck, ipsilateral side
Carcinoma of the Buccal Mucosa and
Gingiva
Account for 10% of oral
squamous cell carcinomas
Varies from a white patch to a
nonhealing ulcer to an
exophytic lesion
Verrucous carcinoma broadbased, wart-like mass
Rarely metastasizes
Carcinoma of the Palate
Common occurrence at the soft
palate (10-20%), rare at the
hard palate
Asymptomatic red or white
plaques
Ulcerated keratotic mass
Histopathology
o Spindle-cell carcinoma
(sarcomatoid carcinoma)
o Appears as proliferation
of spindle cells mistaken
as sarcoma
o Verrucous carcinoma
Well-differentiated
epithelial cells that
appear more
hyperplastic than
neoplastic
Key feature:
invasive nature of
the lesion in the
form of broad,
pushing margins
Basaloid-squamous
carcinoma
Basaloid pattern of
tumor cells is seen
adjacent to tumor
cells that exhibit
squamous
differentiation
Has a predilection
for the base of the
tongue and the
pharynx
Treatment
1. Simple excision
2. Curettage and
electrodessication
3. Radiation therapy
4. Cryosurgery
5. For advanced cancer:
A. lymph node dissection
B. Systemic chemotherapy
Você também pode gostar
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Derivational and Inflectional Morpheme in English LanguageDocumento11 páginasDerivational and Inflectional Morpheme in English LanguageEdificator BroAinda não há avaliações
- Philodendron Plants CareDocumento4 páginasPhilodendron Plants CareSabre FortAinda não há avaliações
- 10 1108 - TQM 03 2020 0066 PDFDocumento23 páginas10 1108 - TQM 03 2020 0066 PDFLejandra MAinda não há avaliações
- Combined South Dakota Motions To Reconsider in ICWA CaseDocumento53 páginasCombined South Dakota Motions To Reconsider in ICWA CaseLee StranahanAinda não há avaliações
- Analysis of Rates (Nh-15 Barmer - Sanchor)Documento118 páginasAnalysis of Rates (Nh-15 Barmer - Sanchor)rahulchauhan7869Ainda não há avaliações
- Literature Review Template DownloadDocumento4 páginasLiterature Review Template Downloadaflsigfek100% (1)
- Galgotias University Uttar Pradesh School of Computing Science & Engineering B.Tech. (CSE) 2018-19 Semester Wise Breakup of CoursesDocumento2 páginasGalgotias University Uttar Pradesh School of Computing Science & Engineering B.Tech. (CSE) 2018-19 Semester Wise Breakup of CoursesRohit Singh BhatiAinda não há avaliações
- Evidence Prove DiscriminationDocumento5 páginasEvidence Prove DiscriminationRenzo JimenezAinda não há avaliações
- SP-Chapter 14 PresentationDocumento83 páginasSP-Chapter 14 PresentationLoiDa FloresAinda não há avaliações
- Bcom (HNRS) Project Final Year University of Calcutta (2018)Documento50 páginasBcom (HNRS) Project Final Year University of Calcutta (2018)Balaji100% (1)
- Perdarahan Uterus AbnormalDocumento15 páginasPerdarahan Uterus Abnormalarfiah100% (1)
- CG Photo Editing2Documento3 páginasCG Photo Editing2Mylene55% (11)
- 9400 Series - Catalogue - AccessoriesDocumento86 páginas9400 Series - Catalogue - AccessoriesSaulo Leonardo Fabelo FontesAinda não há avaliações
- Genuine Fakes: How Phony Things Teach Us About Real StuffDocumento2 páginasGenuine Fakes: How Phony Things Teach Us About Real StuffGail LeondarWrightAinda não há avaliações
- Industrial ExperienceDocumento30 páginasIndustrial ExperienceThe GridLockAinda não há avaliações
- Unit 1 Module 3 Rep in PlantsDocumento26 páginasUnit 1 Module 3 Rep in Plantstamesh jodhanAinda não há avaliações
- MFE Module 1 .Documento15 páginasMFE Module 1 .Adarsh KAinda não há avaliações
- Best Mutual Funds For 2023 & BeyondDocumento17 páginasBest Mutual Funds For 2023 & BeyondPrateekAinda não há avaliações
- D25KS Sanvick PDFDocumento4 páginasD25KS Sanvick PDFJiménez Manuel100% (1)
- Very Narrow Aisle MTC Turret TruckDocumento6 páginasVery Narrow Aisle MTC Turret Truckfirdaushalam96Ainda não há avaliações
- AIIMS 2015 Solved PaperDocumento436 páginasAIIMS 2015 Solved PaperSurya TejaAinda não há avaliações
- Nikos MIDI Pack - Chord Progression GuideDocumento5 páginasNikos MIDI Pack - Chord Progression GuideSamuel ThompsonAinda não há avaliações
- Fuzzy Gain Scheduled Pi Controller For ADocumento5 páginasFuzzy Gain Scheduled Pi Controller For AOumayAinda não há avaliações
- CURRICULUM PharmasubDocumento10 páginasCURRICULUM PharmasubZE Mart DanmarkAinda não há avaliações
- ABARI-Volunteer Guide BookDocumento10 páginasABARI-Volunteer Guide BookEla Mercado0% (1)
- China Training WCDMA 06-06Documento128 páginasChina Training WCDMA 06-06ryanz2009Ainda não há avaliações
- Universal Ultrasonic Generator For Welding: W. Kardy, A. Milewski, P. Kogut and P. KlukDocumento3 páginasUniversal Ultrasonic Generator For Welding: W. Kardy, A. Milewski, P. Kogut and P. KlukPhilip EgyAinda não há avaliações
- Registration ListDocumento5 páginasRegistration ListGnanesh Shetty BharathipuraAinda não há avaliações
- Jul - Dec 09Documento8 páginasJul - Dec 09dmaizulAinda não há avaliações
- Lodge at The Ancient City Information Kit / Great ZimbabweDocumento37 páginasLodge at The Ancient City Information Kit / Great ZimbabwecitysolutionsAinda não há avaliações