Escolar Documentos
Profissional Documentos
Cultura Documentos
Anti Vegf Drugs in The Prevention of Blindness
Enviado por
Indra PermanaTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Anti Vegf Drugs in The Prevention of Blindness
Enviado por
Indra PermanaDireitos autorais:
Formatos disponíveis
DRUGS
Anti-VEGF drugs in the
prevention of blindness
David Yorston
Consultant Ophthalmologist: Tennent
Institute of Ophthalmology, Gartnavel
Hospital, Glasgow, UK.
dbyorston@btinternet.com
Disorders of the blood vessels in the
retina are responsible for some of the
most common causes of blindness in the
world. These include:
retinopathy of prematurity (an important
cause of blindness in children in middleincome countries)
diabetic retinopathy (the most common
cause of blindness in the working-age
population of industrialised countries)
age-related macular degeneration (the
third most common cause of blindness
in the world).
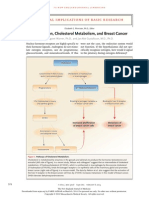
All of these conditions are caused partly
by over-production of a protein called
vascular endothelial growth factor
(VEGF). This protein was discovered in
the 1980s and is important in the growth
and development of blood vessels. VEGF
production is increased by hypoxia (a lack
of oxygen). So, if a tissue is not getting
enough oxygen, it will produce more
VEGF, which will stimulate the growth of
additional blood vessels to provide more
oxygen. This is beneficial in the heart
muscle, or in a growing baby; however, in
the eye it can be harmful.
The effects of VEGF may be summarised as:
Increased permeability of existing blood
vessels, causing them to leak.
Growth of new blood vessels, which may
bleed or leak fluid and proteins.
In the eye, both can lead to retinal
damage.
Normal retinal capillaries (very fine
blood vessels in the retina) are sealed
thanks to tight junctions between the
cells making up the capillary walls. This
means that large molecules, such as
proteins and lipids, cannot leak out of
these retinal capillaries into the retina. In
the presence of excessive VEGF, however,
the capillaries start to leak and large
molecules form exudates and escape into
the retina, causing oedema in the
surrounding tissues. If this affects the
macula, then the central vision will be
reduced. This is what causes diabetic
macular oedema.
Excessive VEGF also causes the growth
of new, abnormal retinal blood vessels
and capillaries. These do not grow within
the retina, where they might be useful.
44
Instead, the abnormal capillaries grow out
from the retina onto the surface of the
vitreous, where the vitreous touches the
retina. This happens in proliferative
diabetic retinopathy and retinopathy of
prematurity. The new vessels are fragile
and prone to tearing. When a new vessel
is torn, it bleeds, causing vitreous
haemorrhage. As the vitreous contracts,
the new vessels pull on the retina,
causing a traction retinal detachment. If
the detachment includes the macula,
vision will be impaired.
In the presence of excessive VEGF, new
vessels can also grow out from the choroid
(the layer immediately under the retina).
These new vessels grow into the space
between the retina and the choroid,
usually just under the retinal pigment
epithelium. The newvessels leak exudates
formed of fluid or blood, causing oedema;
eventually a fibrous scar is formed that
destroys the photoreceptor cells at the
centre of the macula. This is what
happens in exudative (or wet) age-related
macular degeneration (AMD).
Because of these very damaging
effects in the eye, researchers have been
working for years to find a way to block the
activity of VEGF in the eye.
Anti-VEGF drugs
VEGF has many beneficial effects in the
rest of the body. Therefore, any
anti-VEGF drug has to be given by a route
that gives the maximum effect in the eye,
but little or no effect elsewhere. In
practice, this means it must be injected
into the eye (intraocular injection). This
carries a number of risks, and it is
thought that about 1 in every 1,000
injections has a serious complication
such as cataract, vitreous haemorrhage,
retinal detachment, or infection. Each
injection must be handled with appropriate sterilisation and aseptic technique
(see page 47).
The two most widely used drugs at
present are Lucentis (ranibizumab) and
Avastin (bevacizumab). Both drugs are
monoclonal antibodies that bind to all
three forms of VEGF. They are very similar
drugs (see page 48), but Lucentis is a
smaller molecule and is believed to bind
VEGF in the eye with greater affinity.
Lucentis is intended purely for intraocular
injection, and each vial can only be used
for one patient. Avastin was intended to
be given intravenously as an anti-cancer
drug, and comes in vials of 100 mg.
As the dose required for intravitreal
COMMUNITY EYE HEALTH JOURNAL | VOLUME 27 ISSUE 87 | 2014
injection is only 2.5mg, one vial of 100 mg
of Avastin can be used to treat 40
patients, provided that you have the
necessary skills and facilities to prepare
sterile injections for intraocular injection.
In the United Kingdom, the British
National Formulary gives a net price of
242* for a 100 mg vial of Avastin,
(containing 40 doses). The British
National Formulary gives a net price of
742* for a single 2.5 mg dose of
Lucentis. This means that a single dose of
Avastin can work out to be over 100 times
cheaper than a single dose of Lucentis
(provided that you have the skills and
facilities, as stated above). [*Note: The
actual prices of drugs vary considerably
due to local purchasing arrangements,
and may be very different from the net
prices quoted above. These are taken
from the British National Formulary, and
only give an indication of the relative costs
of the drugs.]
The most recently approved drug is
aflibercept (also known as Eylea). This is
an artificial protein that contains the VEGF
receptor molecules that are normally
attached to cell membranes. The VEGF
binds to these receptors and is trapped
and rendered harmless. Aflibercept
seems to be as effective as Avastin and
Lucentis, but may be given less frequently.
In the British National Formulary, a single
dose has a net price of 816.
Side-effects
VEGF is important for the growth of new
blood vessels. Although the dose of
anti-VEGF needed to treat eye diseases is
very small, it has been shown to reduce
the level of VEGF in the bloodstream. This
means that there is a theoretical risk that,
in adults, anti-VEGF drugs may increase
the risk of cardiovascular disease,
including heart attacks and strokes.
However, clinical trials have not shown
conclusive evidence of an increased risk
of cardiovascular disease in patients
treated with anti-VEGF drugs compared to
those given sham injections.
In babies and young children, VEGF is
essential for the growth of blood vessels
and normal growth and development of
many other organs including the lungs,
kidney and brain. This is one of the
reasons why anti-VEGF drugs are
absolutely contra-indicated in pregnancy.
Women of childbearing age should have a
pregnancy test prior to starting treatment,
and must avoid pregnancy during
treatment. Although Avastin has been
Treatment regimes in adults
Regardless of the treatment indication,
there are essentially two regimes for
administering anti-VEGF drugs:
continuous and intermittent/as
required (or pro re nata, PRN for short).
Most of the initial trials were done as
a continuous regime, with regular
monthly injections over the course of 2
years, i.e. patients would have 24 injections in total. These trials showed that
treatment delivered in this way was
effective, but it is also expensive and
inconvenient for both the patient and the
health care provider.
A number of other trials have examined
PRN regimes. These are all fairly similar
and consist of three injections given over
3 months, followed by review. At this point
the patient may:
be much better, in which case no
additional treatment is needed
have no improvement at all, in which
case further treatment is futile
have some improvement, which would
justify further injections.
Even among those patients who do very
well, and do not require more than three
injections initially, many will relapse and
require further injections in the future.
This means they must be regularly
reviewed in the clinic, i.e. every 12
months, which involves testing of visual
acuity and/or retinal thickness. If patients
visual acuity is lower by one or more lines,
or if they develop worsening macular
oedema, they need a further injection of
anti-VEGF.
Trials of this dosing regime for AMD and
diabetic macular oedema have shown
that an average of seven injections are
required in the first year of treatment and
that outcomes are as good as for regular
monthly injections. The trials used as their
indication for re-treatment with anti-VEGF
either a reduction in visual acuity or an
increase in retinal thickness (measured
using optical coherence tomography
[OCT]); both were assessed at each visit.
While visual acuity is easily measured,
retinal thickness can only be measured
accurately by OCT. These machines are
costly and will only be available in major
Continues overleaf
FROM THE FIELD
Use of anti-VEGF drugs at the Instituto de
la Visin de Montemorelos
Pedro A Gomez Bastar
CBM Medical Adviser and Chairman, Instituto de la Vision, Universidad de
Montemorelos, Mexico pgomez07@gmail.com
1 Which antiVEGF agents
do we use?
Pedro A. Gomez Bastar
used in the management of retinopathy of
prematurity, its use is controversial,
because of the potential for serious
adverse effects when used in young
babies (see panel on page 46).
In practice, the major adverse effects
of these drugs appear to be associated
with the intraocular injection rather than
the active drug.
We use bevazucimab
(Avastin) the dose
used is 2.5 mg (0.1 ml).
This anti-VEGF agent is
used because of its:
proven efficacy and
effectiveness (CATT &
IVAN studies)
low cost, making it
affordable for our
patients.
Anti-VEGF injections are given in a clean room
5 What are the outcomes?
2 What are the
indications?
Vitreous haemorrhage secondary to
proliferative diabetic retinopathy
particularly when there has been no
previous laser.
Prior to vitrectomy for proliferative
diabetic retinopathy.
Clinically significant macular oedema
due to diabetic retinopathy.
Macular oedema secondary to branch
or central retinal vein occlusion.
Exudative age-related macular
degeneration.
Neovascular glaucoma.
3 Who gives the
injections?
Intra-vitreal injections are always given
by an ophthalmologist, for example:
retina specialists
retina subspecialty trainees
ophthalmology residents in the retinal
service.
4 Are anti-VEGF agents
used without OCT?
Anti VEGF agents are used without OCT
in selected cases:
vitreous haemorrhage secondary to
proliferative diabetic retinopathy
particularly when there has been no
previous laser
prior to vitrectomy for proliferative
diabetic retinopathy
clinically significant macular oedema
due to diabetic retinopathy
neovascular glaucoma.
Clinical experience has been very
positive and we believe this is a costeffective treatment for our patients.
Vitreous haemorrhage secondary
to proliferative diabetic retinopathy:
We have been pleased with our results.
Anti-angiogenic therapy reduces the
vitreous haemorrhage in many
patients with diabetic retinopathy,
allowing us to apply laser and avoid
vitrectomy surgery.
Prior to vitrectomy for proliferative
diabetic retinopathy: Application
35 days before surgery reduces the
risk of intra-operative and postoperative bleeding.
Neovascular glaucoma: In these
patients, we are careful to avoid further
increases in the IOP. When the rubeosis
regresses we apply pan-retinal laser,
giving us more control of the iris
neovascularisation.
Clinically significant macular
oedema: In clinically significant macular
oedema due to diabetic retinopathy, we
normally apply three doses of Avastin
with 1-month intervals between injections. After the last injection, a macular
OCT is requested and, if the oedema
has decreased, we apply focal laser.
Age-related macular degeneration
(AMD): In patients with exudative AMD,
an injection is given every month for
several months to improve visual acuity
and to control the disease, following the
treat and extend protocol.
Continues overleaf
COMMUNITY EYE HEALTH JOURNAL | VOLUME 27 ISSUE 87 | 2014 45
DRUGS Continued
cities in low- and middle income countries.
We dont yet know how effective PRN
treatment might be when retreatment is
guided by visual acuity alone, as both
visual acuity and retinal thickness were
measured at each visit in these trials.
Although intermittent regimes reduce
the number of injections, patients still
have to be reviewed every 12 months,
which leads to very busy clinics; this is
also a significant burden for the patients
and for their families.
Which diseases can be
treated?
Age-related macular degeneration
Lucentis, Avastin and Eyelea are equally
effective in exudative AMD. There
appears to be little difference between
monthly and PRN dosing. The average
(mean) improvement in vision is about
12 lines, and about one-third of
patients will improve by three or more
lines. With a PRN regime, an average of
seven injections will be required in the
first year. Most of these trials excluded
eyes with a vision of less than 6/96
(4/60), and treatment is unlikely to be
effective in advanced exudative AMD with
sub-macular scarring or a vision of
counting fingers or hand movement.
Unfortunately, exudative AMD often
co-exists with atrophic (dry) AMD, and
the anti-VEGF drugs only treat the
exudative component. With longer
follow-up (over 2 years), atrophic AMD
may cause a gradual loss of vision
despite effective anti-VEGF treatment.
Diabetic macular oedema
Once again, there seems to be little
difference between the different
anti-VEGF drugs. All three are effective at
treating diabetic macular oedema, and
the average improvement in vision is
about 1.5 lines. Roughly 25% of patients
will have their visual acuity improve by
three or more lines and 50% by two or
more lines. An average of seven injections
will be required in the first year of
treatment with a PRN regime.
Not all patients with diabetic macular
oedema need to be treated with
anti-VEGF. Laser treatment still has an
important role: macular oedema which
does not involve the fovea is best treated
with laser. These patients will normally
have good vision, and the laser will help to
preserve it. Moreover, laser is usually
effective with a single treatment, which is
much easier for the patient than repeated
monthly injections.
If new vessels are present, they should
be given pan-retinal laser treatment first,
before any macular oedema is treated
using anti-VEGF. This is because
anti-VEGF makes the new vessels regress
very quickly. As the treated vessels
become fibrotic, they contract, which can
cause a retinal detachment.
Retinal vein occlusion
There is good evidence from clinical trials
that all three anti-VEGF drugs will reduce
the risk of loss of vision following central
retinal vein occlusion. About 50% of
patients will gain three or more lines, with
a mean improvement of about two lines.
There is also a reduced risk of rubeosis
and secondary glaucoma with anti-VEGF
treatment.
Lucentis has been shown to improve
outcomes after branch retinal vein
occlusion as well. However, as many of
these patients will improve spontaneously,
this evidence is not quite as strong.
In summary, anti-VEGF drugs are probably
the most significant advance in ophthalmology in the last decade. They have
enabled us to treat what were previously
untreatable conditions. They are not a
perfect solution, however.
They do not cure the underlying
problem, so repeated treatment is
necessary and most patients will require
a lifetime of regular monitoring.
The drugs are expensive, and even highincome countries have struggled with the
costs and logistics of delivering thousands
of intraocular injections every year.
Although anti-VEGF drugs are the most
effective treatment for many retinal
diseases, the visual improvement is
modest, averaging about two lines of
vision. Relatively few patients will regain
normal vision.
Patients who present late, with very
advanced disease and a visual acuity of
less than 3/60, may not benefit from
treatment.
Most PRN treatment regimes rely on
OCT imaging, which is rarely available in
low and middle income countries. We
have little information on the use of
anti-VEGF in this setting, and we cannot
be sure that the good results achieved
in Europe and North America will be
replicated in Africa, India, or China.
Despite these reservations, anti-VEGF
drugs are going to play an increasing role
in the prevention of blindness worldwide.
As the global population ages, and
becomes more overweight, both AMD
and diabetic retinopathy will become
more common. The drugs will become
cheaper, and we may find better ways of
monitoring treatment so that expensive
OCT is no longer essential.
Anti-VEGF treatment for acute ROP not yet recommended!
Clare Gilbert
Co-director: International Centre for
Eye Health, Disability Group, London
School of Hygiene and Tropical
Medicine, London, UK.
There are several reasons why anti-VEGF
agents are not recommended for acute,
severe retinopathy of prematurity (ROP).
There has only been one randomised
trial, which compared laser with
Avastin (bevacizumab) for Type 1 ROP.
It was only more effective in preventing
early recurrence of severe disease in
Zone 1 (posterior), but the recurrence
rate in the laser arm was worse than
would be expected based on other
studies. More babies died in the
anti-VEGF arm of the trial, but the
46
difference was not statistically
significant.
There are major concerns about the
short- and long-term impact of
anti-VEGF agents on the lung, kidneys
and brain of a baby.
Follow-up studies, using fluorescein
angiography, indicate that normal
retinal vascularisation may not take
place after administration of
bevacizumab, with extensive areas of
non-perfusion months after treatment.
There are an increasing number of
case reports which show that, although
Avastin can lead to regression of ROP
in the short term, the ROP can recur
months later. This means that an acute
disease with a known natural history
has the potential to become a chronic
COMMUNITY EYE HEALTH JOURNAL | VOLUME 27 ISSUE 87 | 2014
disease with an unknown and
unpredictable natural history.
Some surgeons use Avastin for Stage
4a or 4b ROP prior to surgery. This can
make the surgery easier, but there is
still the risk of systemic complications.
The leaking capillaries present in eyes
with retinopathy increase the risk of large
molecules (e.g. anti-VEGF drugs injected
into the eye) entering the systemic circulation, and so the systemic safety of
these drugs is important, particularly in
preterm infants. If anti-VEGF drugs seem
to be the only option to preserve sight
when extensive laser has failed, or the
infant is too sick for laser, this treatment
can be offered, but only after parents
have been fully informed of the possible
consequences.
The author/s and Community Eye Health Journal 2014. This is an Open Access
article distributed under the Creative Commons Attribution Non-Commercial License.
Você também pode gostar
- Avastin Injection ConsentDocumento4 páginasAvastin Injection ConsentSaumya SanyalAinda não há avaliações
- 933 001abedi2013Documento7 páginas933 001abedi20136jprsrbhkcAinda não há avaliações
- Bevacizumab 21 A AdDocumento11 páginasBevacizumab 21 A Adbangun baniAinda não há avaliações
- Anti VEGFDocumento43 páginasAnti VEGFanantkumar85Ainda não há avaliações
- Review Article: Intravitreal Therapy For Diabetic Macular Edema: An UpdateDocumento23 páginasReview Article: Intravitreal Therapy For Diabetic Macular Edema: An UpdateRuth WibowoAinda não há avaliações
- Comparison of Intravitreal Bevacizumab (Avastin) With Triamcinolone For Treatment of Diffused Diabetic Macular Edema: A Prospective Randomized StudyDocumento9 páginasComparison of Intravitreal Bevacizumab (Avastin) With Triamcinolone For Treatment of Diffused Diabetic Macular Edema: A Prospective Randomized StudyBaru Chandrasekhar RaoAinda não há avaliações
- Uveitis Definition: C. Stephen Foster, M.DDocumento2 páginasUveitis Definition: C. Stephen Foster, M.DMasha AllahAinda não há avaliações
- Compounded BevacizumabDocumento6 páginasCompounded BevacizumabHenrique AquinoAinda não há avaliações
- A Collaborative Retrospective Study On The Efficacy and Safety of Intravitreal Dexamethasone Implant (Ozurdex) in Patients With Diabetic Macular EdemaDocumento17 páginasA Collaborative Retrospective Study On The Efficacy and Safety of Intravitreal Dexamethasone Implant (Ozurdex) in Patients With Diabetic Macular EdemaJosé Díaz OficialAinda não há avaliações
- Jurnal 4Documento8 páginasJurnal 4Putri kartiniAinda não há avaliações
- Local Therapies For Inflammatory Eye Disease in Translation Past, Present and Future 2013Documento8 páginasLocal Therapies For Inflammatory Eye Disease in Translation Past, Present and Future 2013Igor VainerAinda não há avaliações
- Ma 2021 Uveitis 101Documento5 páginasMa 2021 Uveitis 101Jenny MaAinda não há avaliações
- Dexamethasone Intravitreal Implant in TheDocumento15 páginasDexamethasone Intravitreal Implant in TheMadalena AlmeidaAinda não há avaliações
- Choroidal NeovascularizationNo EverandChoroidal NeovascularizationJay ChhablaniAinda não há avaliações
- AVASTINDocumento10 páginasAVASTINFitri ShabrinaAinda não há avaliações
- HelmDocumento22 páginasHelmEga Gumilang SugiartoAinda não há avaliações
- Advances in The Treatment of Age-Related Macular Degeneration (AMD)Documento22 páginasAdvances in The Treatment of Age-Related Macular Degeneration (AMD)Ega Gumilang SugiartoAinda não há avaliações
- Glaucoma 9Documento13 páginasGlaucoma 9Sheila Kussler TalgattiAinda não há avaliações
- Brolucizumab PDFDocumento6 páginasBrolucizumab PDFCl WongAinda não há avaliações
- Intophthalmolclin2006462141 64Documento24 páginasIntophthalmolclin2006462141 64Laura BortolinAinda não há avaliações
- International Journal of Case Reports (ISSN:2572-8776) Loading Doses of Bevacizumab in Branch Retinal Vein Occlusion (BRVO) : A Case ReportDocumento5 páginasInternational Journal of Case Reports (ISSN:2572-8776) Loading Doses of Bevacizumab in Branch Retinal Vein Occlusion (BRVO) : A Case ReportPeony PinkAinda não há avaliações
- 2017 Article 1861Documento12 páginas2017 Article 1861nanaAinda não há avaliações
- Retinal Vein Occlusion (RVO)Documento5 páginasRetinal Vein Occlusion (RVO)Rana PandaAinda não há avaliações
- Steps For A Safe Intravitreal Injection Technique - A ReviewDocumento6 páginasSteps For A Safe Intravitreal Injection Technique - A ReviewriveliAinda não há avaliações
- Pio y AntivegfDocumento14 páginasPio y AntivegfBernardo RomeroAinda não há avaliações
- Related ReadingsDocumento5 páginasRelated Readingscassandra cosAinda não há avaliações
- GP Factsheet - Steroids and The EyeDocumento6 páginasGP Factsheet - Steroids and The EyeBima RizkiAinda não há avaliações
- Porto Biomedical JournalDocumento7 páginasPorto Biomedical JournalzzakieAinda não há avaliações
- Ni Hms 707256Documento11 páginasNi Hms 707256iqbalAinda não há avaliações
- Vernal Keratoconjunctivitis: Why Is Allergic Eye Disease A Problem For Eye Workers?Documento3 páginasVernal Keratoconjunctivitis: Why Is Allergic Eye Disease A Problem For Eye Workers?darendraabimayuAinda não há avaliações
- Chronic EpididymitisDocumento4 páginasChronic EpididymitisAhamed RockAinda não há avaliações
- Difluprednato EC U S JOPT 2010 26 5 475 FosterDocumento11 páginasDifluprednato EC U S JOPT 2010 26 5 475 FosterMartin MauadAinda não há avaliações
- Case Vignette Macular DegenerationDocumento6 páginasCase Vignette Macular DegenerationJosh BlasAinda não há avaliações
- Uveitis PDFDocumento3 páginasUveitis PDFTri BasukiAinda não há avaliações
- What Do We Do About Diabetes?: See P 397Documento2 páginasWhat Do We Do About Diabetes?: See P 397Ika PuspitaAinda não há avaliações
- Anti VEGF Intravitreal InjectionDocumento26 páginasAnti VEGF Intravitreal InjectionAyesya KamilahAinda não há avaliações
- IncidenceDocumento11 páginasIncidenceNenad ProdanovicAinda não há avaliações
- Ret 1115 IDocumento24 páginasRet 1115 IeyheghedgeAinda não há avaliações
- Recent Advances Glaucoma ImplantsDocumento5 páginasRecent Advances Glaucoma ImplantsAnumeha JindalAinda não há avaliações
- 1 s2.0 S1091853116304438 MainDocumento6 páginas1 s2.0 S1091853116304438 MainMarcella PolittonAinda não há avaliações
- Intravitreal Bevacizumab (Avastin) Therapy For Persistent Diffuse Diabetic Macular EdemaDocumento7 páginasIntravitreal Bevacizumab (Avastin) Therapy For Persistent Diffuse Diabetic Macular EdemaJose Antonio Fuentes VegaAinda não há avaliações
- Intravitreal Injection of Bevacizumab: Review of Our Previous ExperienceDocumento6 páginasIntravitreal Injection of Bevacizumab: Review of Our Previous ExperienceShintya DewiAinda não há avaliações
- Neovascularization & EdemaDocumento3 páginasNeovascularization & EdemaKweku Grant-AcquahAinda não há avaliações
- Retinal Reperfusion in Diabetic Retinopathy Following Treatment With anti-VEGF Intravitreal InjectionsDocumento10 páginasRetinal Reperfusion in Diabetic Retinopathy Following Treatment With anti-VEGF Intravitreal InjectionsAzizan HakimAinda não há avaliações
- MataDocumento16 páginasMataIslah NadilaAinda não há avaliações
- Journal Pone 0131770 PDFDocumento23 páginasJournal Pone 0131770 PDFKarina Mega WAinda não há avaliações
- Case Vignette in NCM 116B (E/E-Age Related Macular Degeneration)Documento4 páginasCase Vignette in NCM 116B (E/E-Age Related Macular Degeneration)faye kimAinda não há avaliações
- 2020 - 10.1007 - s00347 020 01250 yDocumento10 páginas2020 - 10.1007 - s00347 020 01250 yEko NoviantiAinda não há avaliações
- Retinopathy of Prematurity: GGW Adams Moorfields Eye Hospital, LondonDocumento29 páginasRetinopathy of Prematurity: GGW Adams Moorfields Eye Hospital, LondonJuan R. AntunezAinda não há avaliações
- Cyclosporine Cationic Emulsion Pediatric VKDocumento11 páginasCyclosporine Cationic Emulsion Pediatric VKDinda Ajeng AninditaAinda não há avaliações
- Retina Clinica Trials Update - 0813 - Supp2Documento16 páginasRetina Clinica Trials Update - 0813 - Supp2cmirceaAinda não há avaliações
- Anti-VEGF Agents and Their Clinical Applications: Dr. Sriniwas Atal MD. Resident OphthalmologyDocumento67 páginasAnti-VEGF Agents and Their Clinical Applications: Dr. Sriniwas Atal MD. Resident OphthalmologySriniwasAinda não há avaliações
- Original Investigation: JamaDocumento13 páginasOriginal Investigation: JamaGema Akbar WakhidanaAinda não há avaliações
- Opth 9 367Documento5 páginasOpth 9 367titisAinda não há avaliações
- Herpes Zoster Ophthalmicus - EyeWikiDocumento1 páginaHerpes Zoster Ophthalmicus - EyeWikiStephanie AureliaAinda não há avaliações
- Recovery Following The TransplantDocumento10 páginasRecovery Following The TransplantAci Indah KusumawardaniAinda não há avaliações
- Branch Retinal Vein Occlusion (BRVO) : How Does BRVO Occur?Documento3 páginasBranch Retinal Vein Occlusion (BRVO) : How Does BRVO Occur?merizAinda não há avaliações
- Clinical Management Review 2023-2024: Volume 2: USMLE Step 3 and COMLEX-USA Level 3No EverandClinical Management Review 2023-2024: Volume 2: USMLE Step 3 and COMLEX-USA Level 3Ainda não há avaliações
- tmp5D2D TMPDocumento4 páginastmp5D2D TMPFrontiersAinda não há avaliações
- Uveitis: Signs and SymptomsDocumento4 páginasUveitis: Signs and SymptomsMoses Karanja Jr.Ainda não há avaliações
- KP LamafIS Sin1Documento1 páginaKP LamafIS Sin1Indra PermanaAinda não há avaliações
- Mata36a PDFDocumento10 páginasMata36a PDFIndra PermanaAinda não há avaliações
- Jurnal Mata PonkoppDocumento7 páginasJurnal Mata PonkoppIndra PermanaAinda não há avaliações
- Eye Journal PonkopDocumento7 páginasEye Journal PonkopIndra PermanaAinda não há avaliações
- Jurnal ObgynDocumento10 páginasJurnal ObgynIndra PermanaAinda não há avaliações
- Initial Resus TableDocumento3 páginasInitial Resus TableParama AdhikresnaAinda não há avaliações
- Journal LL LL PediatriDocumento4 páginasJournal LL LL PediatriIndra PermanaAinda não há avaliações
- CholesterolDocumento2 páginasCholesterolIndra PermanaAinda não há avaliações
- Metodologi Penelitian Kedokteran Dan Kesehatan Kedokteran Dan KesehatanDocumento16 páginasMetodologi Penelitian Kedokteran Dan Kesehatan Kedokteran Dan KesehatanGhisqy Arsy MulkiAinda não há avaliações
- Daftar PusTaka SNHDocumento7 páginasDaftar PusTaka SNHIndra PermanaAinda não há avaliações
- Cover Kel. A19 Respi FixxDocumento1 páginaCover Kel. A19 Respi FixxIndra PermanaAinda não há avaliações
- Penggunaan Berbagai Cut-Off Indeks Massa Tubuh Sebagai Indikator Obesitas Terkait Penyakit Degeneratif Di IndonesiaDocumento14 páginasPenggunaan Berbagai Cut-Off Indeks Massa Tubuh Sebagai Indikator Obesitas Terkait Penyakit Degeneratif Di IndonesiaLutfi RensiansiAinda não há avaliações
- Abnormal Breath SoundsDocumento3 páginasAbnormal Breath SoundsIndra PermanaAinda não há avaliações
- Abnormal Breath SoundsDocumento3 páginasAbnormal Breath SoundsIndra PermanaAinda não há avaliações
- Ministry of Truth Big Brother Watch 290123Documento106 páginasMinistry of Truth Big Brother Watch 290123Valentin ChirilaAinda não há avaliações
- E 18 - 02 - Rte4ltay PDFDocumento16 páginasE 18 - 02 - Rte4ltay PDFvinoth kumar SanthanamAinda não há avaliações
- WWW - Ib.academy: Study GuideDocumento122 páginasWWW - Ib.academy: Study GuideHendrikEspinozaLoyola100% (2)
- Unsaturated Polyester Resins: Influence of The Styrene Concentration On The Miscibility and Mechanical PropertiesDocumento5 páginasUnsaturated Polyester Resins: Influence of The Styrene Concentration On The Miscibility and Mechanical PropertiesMamoon ShahidAinda não há avaliações
- Improving Self-Esteem - 08 - Developing Balanced Core BeliefsDocumento12 páginasImproving Self-Esteem - 08 - Developing Balanced Core BeliefsJag KaleyAinda não há avaliações
- Water On Mars PDFDocumento35 páginasWater On Mars PDFAlonso GarcíaAinda não há avaliações
- CV AmosDocumento4 páginasCV Amoscharity busoloAinda não há avaliações
- Unit 2-ED (Theory)Documento13 páginasUnit 2-ED (Theory)chakramuAinda não há avaliações
- Strategi Pencegahan Kecelakaan Di PT VALE Indonesia Presentation To FPP Workshop - APKPI - 12102019Documento35 páginasStrategi Pencegahan Kecelakaan Di PT VALE Indonesia Presentation To FPP Workshop - APKPI - 12102019Eko Maulia MahardikaAinda não há avaliações
- Direct Filter Synthesis Rhea PreviewDocumento25 páginasDirect Filter Synthesis Rhea Previewoprakash9291Ainda não há avaliações
- Quarter 2-Module 7 Social and Political Stratification: Department of Education Republic of The PhilippinesDocumento21 páginasQuarter 2-Module 7 Social and Political Stratification: Department of Education Republic of The Philippinestricia100% (5)
- Class NotesDocumento16 páginasClass NotesAdam AnwarAinda não há avaliações
- AS 1 Pretest TOS S.Y. 2018-2019Documento2 páginasAS 1 Pretest TOS S.Y. 2018-2019Whilmark Tican MucaAinda não há avaliações
- Rizal ExaminationDocumento3 páginasRizal ExaminationBea ChristineAinda não há avaliações
- (Durt, - Christoph - Fuchs, - Thomas - Tewes, - Christian) Embodiment, Enaction, and Culture PDFDocumento451 páginas(Durt, - Christoph - Fuchs, - Thomas - Tewes, - Christian) Embodiment, Enaction, and Culture PDFnlf2205100% (3)
- Mathematics - Grade 9 - First QuarterDocumento9 páginasMathematics - Grade 9 - First QuarterSanty Enril Belardo Jr.Ainda não há avaliações
- Commercial CrimesDocumento3 páginasCommercial CrimesHo Wen HuiAinda não há avaliações
- Aìgas of Bhakti. at The End of The Last Chapter Uddhava Inquired AboutDocumento28 páginasAìgas of Bhakti. at The End of The Last Chapter Uddhava Inquired AboutDāmodar DasAinda não há avaliações
- 38 Page 2046 2159 PDFDocumento114 páginas38 Page 2046 2159 PDFAkansha SharmaAinda não há avaliações
- Tool Stack Template 2013Documento15 páginasTool Stack Template 2013strganeshkumarAinda não há avaliações
- Creating Literacy Instruction For All Students ResourceDocumento25 páginasCreating Literacy Instruction For All Students ResourceNicole RickettsAinda não há avaliações
- Biblehub Com Commentaries Matthew 3 17 HTMDocumento21 páginasBiblehub Com Commentaries Matthew 3 17 HTMSorin TrimbitasAinda não há avaliações
- TLS FinalDocumento69 páginasTLS FinalGrace Arthur100% (1)
- Introduction To Sociology ProjectDocumento2 páginasIntroduction To Sociology Projectapi-590915498Ainda não há avaliações
- Elementary SurveyingDocumento19 páginasElementary SurveyingJefferson EscobidoAinda não há avaliações
- Stroke Practice GuidelineDocumento274 páginasStroke Practice GuidelineCamila HernandezAinda não há avaliações
- Software Project Management PDFDocumento125 páginasSoftware Project Management PDFUmirAinda não há avaliações
- Aroma TherapyDocumento89 páginasAroma TherapyHemanth Kumar G0% (1)
- Financial Crisis Among UTHM StudentsDocumento7 páginasFinancial Crisis Among UTHM StudentsPravin PeriasamyAinda não há avaliações
- Gothic Revival ArchitectureDocumento19 páginasGothic Revival ArchitectureAlexandra Maria NeaguAinda não há avaliações