Escolar Documentos
Profissional Documentos
Cultura Documentos
Attach Any Wound Tracings Here Attach Any Wound Tracings Here
Enviado por
wiwi handayaniDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Attach Any Wound Tracings Here Attach Any Wound Tracings Here
Enviado por
wiwi handayaniDireitos autorais:
Formatos disponíveis
* F RC0 1 3 2 5 0 *
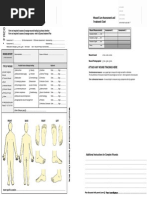
Wound Care Assessment and
Treatment Chart
Wound Care Assessment and
Treatment Chart
Wound Measurements
Form
orm not required to assess & manage wounds healing by primary intention
Form
orm not required to assess & manage eczema - refer to Eczema treatment Plan
Date of Assessment 1........................
Initial Assessment Review Assessment
Date of Assessment 2........................
Medication Allergies: Yes No
WOUND HISTORY:
Nil known
Assessment 2
Greatest Width...........mm
Greatest Length ........mm
Assessed by..........
........................................
Greatest Depth .........mm
Assessed by........................................
by.........................
Skin / Wound Product Sensitivities.........................................
.......................................
Date Admitted..................
Admitted..............................
Assessment 1
Sinus......................... mm
Cause of Wound....................................................
Wound traced
Yes No N/A
Wound Photographed
Yes No N/A
(If initial assessment)
TYPE OF WOUND:
Acute Surgical
Wound
Trauma Wound
Burn
Infected Wound
Chronic Wound
Pressure Injury
Other...................
Possible Factors Delaying Healing
Malnutrition
Obesity
Reduced blood supply Infection
Medication
Chemotherapy
Underlying disease
Maceration
Psychological stress
Lack of sleep
Unrelieved pressure
Immobility
Patient compliance
Radiotherapy
Reduced wound temperature
Inappropriate wound management
IF PRESSURE INJURY
Stage 1 2 3 4
Referrals
Dietitian
Stomal Therapy
Orthotics
Infection Control
Social Work
Mental Health
Burns Coordinator
Dermatology
Plastics
Infectious Diseases
ATTACH ANY WOUND TRACINGS HERE
Date................
Date................Sign.................
Two-dimensional measures use a paper tape to measure the length and width in millimetres.
The circumference
ference of the wound is traced if the wound edges are not even often required for chronic wounds
Date...............
Date...............Sign.................
Date...............
Date...............Sign.................
Three dimensional measures the wound depth is measured using a dampened cotton tip applicator
Date...............
Date................Sign.................
Date................Sign.................
Date................Sign.................
Date..........
Date................Sign.................
Date................Sign.................
Date................Sign.................
Date................Sign.................
FRONT
BACK
RIGHT
LEFT
Wound Care Assessment and Treatment Chart TRIAL
Other (Please specify..........................................................
Additional Instructions for Complex Wounds
.............................................................................................................................
.....................................................................................................................................................................................................
....................................................
....................................................................................................................
......................................................................................................................................................................................................
...................................................
.................................................................................................................................................................................
..................................................................................................................................................
...................................................
.............................................................................................................................
.......................................................................................................................................................................................................
..................................................
.............................................................................................................................
......................................................................................................................................................................................................
...................................................
..................................................................................................................
......................................................................................................................................................................................................
...................................................
.
...............................................................................................................................................................................
.....................................................................................................................................................
..................................................
State Specific Location.............................................................................................................................
.............................................................................................................................
..............................................................................................................................................
Plan discussed with parent/carer
Parent / carer Signature............................................................................................
Assessment 1 Date............................. Print Name & designation.............................................................................................
Step 1 Assessment (minimum weekly or if change noted)
Step 2 Treatment (Do not complete each dressing change)
1. Analgesia required prior to dressing change?
Patients perception of wound pain (please circle)
Yes No N/A
Agreed Arrangements for Dressing Change:
Pre Dressing
(min) 0 1 2 3 4 5 6 7 8 9 10 (max)
2.
During Dressing
(min) 0 1 2 3 4 5 6 7 8 9 10 (max)
Post Dressing
(min) 0 1 2 3 4 5 6 7 8 9 10 (max)
Own Bed
Chair
Distraction techniques
Exudate Amount: Dressing interaction
Dry
Moist
Wet
Saturated
Leaking
Primary dressing is unmarked
Primary dressing may be lightly marked
Primary dressing is extensively marked
Primary dressing is wet & strikethrough is occurring
Dressing are saturated & exudate is escaping from
primary & secondary dressings
Exudate Consistency:
Exudate Odour:
High viscosity (thick,
sometimes sticky)
Low viscosity (thin, runny)
Normal (serous)
Other
Nil
Unpleasant (may
indicate bacterial growth,
infection, necrotic tissue
sinus / fistula
Wound Edge:
Appearance:
Colour:
Pink
Dusky
Raised (chronic wounds)
Rolled (chronic wounds)
Contraction (chronic wounds)
Erythema
Surrounding Skin
Surrounding Skin Appearance
Black/ blue discoloration
Healthy
Fragile
Dry/flaky
Excoriation
Erythema
Oedema
Macerated
Eczematous
Induration
Cellulitis
Wound Bed: (may tick more than one choice)
Granulating (red)
25% 50% 75% 100%
Epithelialising (pink)
25% 50% 75% 100%
Sloughy (yellow)
25% 50% 75% 100%
Necrotic/ Eschar (black)
25% 50% 75% 100%
Hypergrannulation (Raised ) 25% 50% 75% 100%
Other..........................................................................................
Wound Infection (e.g. pyrexia, localised pain, eruthema,
oedema)
Swab attended:
Control Pain
Debridement
Protection
Control exudate
Reduce Bacteria
Encourage Granulation)
Rehydration
3 x week
Weekly
Other..........................................
5. Cleansing Solution:
Other..........................................................................................
Normal
Warm
Cool
Number of staff required.............................................................
3. Treatment objectives (may tick more than one choice)
Daily
2nd Daily
2 x week
Serous (clear, straw coloured)
Haemoserous (pink)
Sanguineous (red)
Purulent (yellow, grey, green)
Temperature
Other.........................................
Time Required............................................................................
Other..........................................................................................
4. Dressing Frequency
Exudate Type:
Treatment Room
Parent/carer present
Yes No N/A
Date of swab
: .........................................
Result (if known)..............................................................................
6. Cleansing Method:
Warmed Saline
Swab
Warmed Sterile Water
Irrigate
Tap Water
Shower
Other......................................................................................
7. Care of surrounding skin: (may tick more than one choice)
Barrier Cream
Zinc Cream
Moisture Cream
Steroid Cream
Olive oil
Vitamin E Cream
Other............................................................................................
8. Primary Dressing:
Synthetic fibre gauze Medicated paste or gel
Island dressing
Semipermeable film dressing
Tulle Gras
Tulle Gras with antiseptic
Foam
Calcium Alginate
Hydrocolloid
Hydrogel
Hydrofibre
Multilayer absorbent dressing
Silicone dressing
Hypertonic saline impregnated
Silver dressing
Odour absorbing dressing
Negative pressure therapy device
Other..........................................................................................
Size................................... No of pieces....................................
9. Secondary dressings:
Semipermeable film dressing
Non-adherent Dressing
Foam
Gauze
Highly Absorbent Pad
Combine
Hydrocolloid
Other..........................
Size............................... No of pieces....................................
10. Tape/ Fixation
Cohesive Bandage
Orthopaedic casting
Adhesive tape eg mefix Paper tape
Tubular Bandage
Crepe Bandage
Polyacrylate fixation sheet
Other......................................................................................
Refer to additional Instructions on back page
Next assessment and review date:..............................
Assessment 2
Date............................. Print Name & designation.............................................................................................
Step 1 Assessment (minimum weekly or if change noted)
Step 2 Treatment (Do not complete each dressing change)
1. Analgesia required prior to dressing change?
Patients perception of wound pain (please circle)
Yes No N/A
Agreed Arrangements for Dressing Change:
Pre Dressing
(min) 0 1 2 3 4 5 6 7 8 9 10 (max)
2.
During Dressing
(min) 0 1 2 3 4 5 6 7 8 9 10 (max)
Post Dressing
(min) 0 1 2 3 4 5 6 7 8 9 10 (max)
Own Bed
Chair
Distraction techniques
Exudate Amount: Dressing interaction
Dry
Moist
Wet
Saturated
Leaking
Primary dressing is unmarked
Primary dressing may be lightly marked
Primary dressing is extensively marked
Primary dressing is wet & strikethrough is occurring
Dressing are saturated & exudate is escaping from
primary & secondary dressings
Exudate Consistency:
Exudate Odour:
High viscosity (thick,
sometimes sticky)
Low viscosity (thin, runny)
Normal (serous)
Other
Nil
Unpleasant (may
indicate bacterial growth,
infection, necrotic tissue
sinus / fistula
Wound Edge:
Appearance:
Colour:
Pink
Dusky
Raised (chronic wounds)
Rolled (chronic wounds)
Contraction (chronic wounds)
Erythema
Surrounding Skin
Surrounding Skin Appearance
Black/ blue discoloration
Healthy
Fragile
Dry/flaky
Excoriation
Erythema
Oedema
Macerated
Eczematous
Induration
Cellulitis
Wound Bed: (may tick more than one choice)
Granulating (red)
25% 50% 75% 100%
Epithelialising (pink)
25% 50% 75% 100%
Sloughy (yellow)
25% 50% 75% 100%
Necrotic/ Eschar (black)
25% 50% 75% 100%
Hypergrannulation (Raised ) 25% 50% 75% 100%
Other..........................................................................................
Wound Infection (e.g. pyrexia, localised pain, eruthema, oedema)
Swab attended:
Control Pain
Debridement
Protection
Control exudate
Reduce Bacteria
Encourage Granulation)
Rehydration
3 x week
Weekly
Other..........................................
5. Cleansing Solution:
Other..........................................................................................
Normal
Warm
Cool
Number of staff required.............................................................
3. Treatment objectives (may tick more than one choice)
Daily
2nd Daily
2 x week
Serous (clear, straw coloured)
Haemoserous (pink)
Sanguineous (red)
Purulent (yellow, grey, green)
Temperature
Other...................................
Time Required..........................................................................
Other..........................................................................................
4. Dressing Frequency
Exudate Type:
Treatment Room
Parent/carer present
Yes No N/A
Date of swab
: .........................................
Result (if known)..............................................................................
6. Cleansing Method:
Warmed Saline
Swab
Warmed Sterile Water
Irrigate
Tap Water
Shower
Other......................................................................................
7. Care of surrounding skin: (may tick more than one choice)
Barrier Cream
Zinc Cream
Moisture Cream
Steroid Cream
Olive oil
Vitamin E Cream
Other............................................................................................
8. Primary Dressing:
Synthetic fibre gauze Medicated paste or gel
Island dressing
Semipermeable film dressing
Tulle Gras
Tulle Gras with antiseptic
Foam
Calcium Alginate
Hydrocolloid
Hydrogel
Hydrofibre
Multilayer absorbent dressing
Silicone dressing
Hypertonic saline impregnated
Silver dressing
Odour absorbing dressing
Negative pressure therapy device
Other..........................................................................................
Size................................... No of pieces....................................
9. Secondary dressings:
Semipermeable film dressing
Non-adherent Dressing
Foam
Gauze
Highly Absorbent Pad
Combine
Hydrocolloid
Other...............................
Size............................... No of pieces....................................
10. Tape/ Fixation
Cohesive Bandage
Orthopaedic casting
Adhesive tape eg mefix Paper tape
Tubular Bandage
Crepe bandage
Polyacrylate fixation sheet
Other......................................................................................
Refer to additional Instructions on back page
Next assessment and review date:..............................
Você também pode gostar
- Wound Assessment Chart PDFDocumento4 páginasWound Assessment Chart PDFFivendra100% (1)
- Wound Assessment ChartDocumento2 páginasWound Assessment ChartAnonymous H3DpmCZX100% (6)
- Wound Assessment ChartDocumento4 páginasWound Assessment ChartSinichi Kudo100% (1)
- NHS Fife Assessment Chart For Wound ManagementDocumento3 páginasNHS Fife Assessment Chart For Wound ManagementImran KhanAinda não há avaliações
- Histopathology Specimens - Clinical, Pathological and Laboratory Aspects (PDFDrive)Documento560 páginasHistopathology Specimens - Clinical, Pathological and Laboratory Aspects (PDFDrive)Xyrelle Navarro100% (2)
- Wound Care Giudeline NHS Bolton HospitalDocumento44 páginasWound Care Giudeline NHS Bolton HospitalJumatun Mona WarahAinda não há avaliações
- Care of Clients With Problems Related To Neurological SystemDocumento44 páginasCare of Clients With Problems Related To Neurological Systemapi-3735995100% (1)
- Assess Patient Pain ThoroughlyDocumento5 páginasAssess Patient Pain Thoroughlyisapatrick8126Ainda não há avaliações
- CL-078 Wound Assessment Guideline 2015Documento35 páginasCL-078 Wound Assessment Guideline 2015JovialAinda não há avaliações
- Perioperative Nursing Core ConceptsDocumento67 páginasPerioperative Nursing Core ConceptsYucef Bahian-AbangAinda não há avaliações
- Wound Assessment and DocumentationDocumento66 páginasWound Assessment and DocumentationRiaReimannAinda não há avaliações
- Validating Wound Care Algorithms For Use by Registered Nurses: Results of A Cross-Sectional StudyDocumento2 páginasValidating Wound Care Algorithms For Use by Registered Nurses: Results of A Cross-Sectional StudyConvaTecWoundAinda não há avaliações
- Arthroplasty CareDocumento3 páginasArthroplasty CareEmjhay Swakida100% (1)
- Med Surg 1Documento21 páginasMed Surg 1Leogalvez BedanoAinda não há avaliações
- Nursing Chapter 48 Skin Integrity and Wound Care FlashcardsDocumento6 páginasNursing Chapter 48 Skin Integrity and Wound Care FlashcardsMark M. AlipioAinda não há avaliações
- Federal Regulations of Pressure Sores (F314Documento3 páginasFederal Regulations of Pressure Sores (F314Jing CruzAinda não há avaliações
- Push 3Documento2 páginasPush 3Sandeep SharmaAinda não há avaliações
- Answers, Rationales, and Test Taking Strategies: The Nursing Care of Adults With Medical and Surgical Health ProblemsDocumento15 páginasAnswers, Rationales, and Test Taking Strategies: The Nursing Care of Adults With Medical and Surgical Health ProblemsNursyNurseAinda não há avaliações
- Z-Tract Method of ImsDocumento1 páginaZ-Tract Method of Imsapi-242267470Ainda não há avaliações
- Malignant Hyperthermia Fact SheetDocumento2 páginasMalignant Hyperthermia Fact Sheetapi-301819201Ainda não há avaliações
- H. OncologyDocumento27 páginasH. OncologyGloryJaneAinda não há avaliações
- AbbreviationDocumento19 páginasAbbreviationJayson NatividadAinda não há avaliações
- Medication Administration: The 5 Rights, Routes, and Proper TechniquesDocumento70 páginasMedication Administration: The 5 Rights, Routes, and Proper Techniquesadni_wgAinda não há avaliações
- Wound Care Handbook: Patient Teaching GuideDocumento26 páginasWound Care Handbook: Patient Teaching GuideRohmatullahAinda não há avaliações
- Physical Examination Health AssessmentDocumento2 páginasPhysical Examination Health AssessmentRosa Willis0% (1)
- Wound Care PDFDocumento100 páginasWound Care PDFVanessaMUeller100% (2)
- Common Surgical PresentationsDocumento49 páginasCommon Surgical PresentationsJeremiah HiiAinda não há avaliações
- Critical Care Skills Checklist: Personal InformationDocumento5 páginasCritical Care Skills Checklist: Personal InformationRin noharaAinda não há avaliações
- Aseptic Wound Dressing Edited 3 Dec 2008Documento11 páginasAseptic Wound Dressing Edited 3 Dec 2008zahisma89Ainda não há avaliações
- Operating Room Preparation: Philipp Acaso Ralph ArcoDocumento158 páginasOperating Room Preparation: Philipp Acaso Ralph ArcoTiffany Luv Adrias100% (1)
- Wound Care MangementDocumento17 páginasWound Care Mangementdian lukman hakimAinda não há avaliações
- Suturing!: Prologue Course Directors Ucsf Department of Surgery Harras Zaid and Derek Ward, MsiisDocumento20 páginasSuturing!: Prologue Course Directors Ucsf Department of Surgery Harras Zaid and Derek Ward, MsiisHarkanAinda não há avaliações
- Central Venous Access Device (CVAD) ManagementDocumento77 páginasCentral Venous Access Device (CVAD) ManagementEvaG2012Ainda não há avaliações
- 3 Wound CareDocumento14 páginas3 Wound Caresechzhen83% (6)
- Notes For Perioperative NursingDocumento5 páginasNotes For Perioperative NursingNey JuneAinda não há avaliações
- CsDocumento7 páginasCsakosiMJcutie100% (1)
- Operating Room NotesDocumento35 páginasOperating Room NotesMagdaraog Gabrielle A.Ainda não há avaliações
- Test Bank For Alexanders Care of The Patient in Surgery 16Th Edition by Rothrock Full File at Https://Testbankdirect - EuDocumento4 páginasTest Bank For Alexanders Care of The Patient in Surgery 16Th Edition by Rothrock Full File at Https://Testbankdirect - EuHumbe OshunAinda não há avaliações
- Preparation-Surgical Area: Have To Operate Without ConsentDocumento5 páginasPreparation-Surgical Area: Have To Operate Without ConsentJane Bautista100% (1)
- Emergency Nursing: By: Keverne Jhay P. ColasDocumento61 páginasEmergency Nursing: By: Keverne Jhay P. ColasGaras AnnaBerniceAinda não há avaliações
- Documentation Guideline: Wound Assessment &treatment Flow Sheet (WATFS) Portrait Version With PSLS#Documento6 páginasDocumentation Guideline: Wound Assessment &treatment Flow Sheet (WATFS) Portrait Version With PSLS#eva arna abrarAinda não há avaliações
- Nursing in EmergenciesDocumento5 páginasNursing in EmergenciesAvisheel KalsiAinda não há avaliações
- Perioperative Nursing UnpDocumento140 páginasPerioperative Nursing Unprnrmmanphd100% (1)
- A Brief History and Definition of Triage in Emergency MedicineDocumento25 páginasA Brief History and Definition of Triage in Emergency MedicineHussein Qunash-JordanAinda não há avaliações
- Medical Triage Codes ExplainedDocumento3 páginasMedical Triage Codes ExplainedAnieaj Buj LevineAinda não há avaliações
- Types and Uses of Surgical NeedlesDocumento12 páginasTypes and Uses of Surgical NeedlesAnuradha RoopchandAinda não há avaliações
- History of The Suture Personal Suture Preference Suture CharacteristicsDocumento33 páginasHistory of The Suture Personal Suture Preference Suture Characteristicsmob3Ainda não há avaliações
- Nursing Guidelines (Draft)Documento221 páginasNursing Guidelines (Draft)Aminath Meesan100% (1)
- Trauma NurseDocumento11 páginasTrauma Nurseapi-247119922Ainda não há avaliações
- RN Job Description PDFDocumento1 páginaRN Job Description PDFvhon100% (1)
- Perioperative Nursing Concept PDFDocumento21 páginasPerioperative Nursing Concept PDFMari Fe100% (1)
- Head to-Toe-Assessment Complete Guide - Nightingale CollegeDocumento1 páginaHead to-Toe-Assessment Complete Guide - Nightingale CollegeDabon RusselAinda não há avaliações
- Whipple SurgeryDocumento22 páginasWhipple SurgeryPrincess Brigitte R. PATE�AAinda não há avaliações
- Medical TerminologyDocumento8 páginasMedical Terminologyiannello100% (1)
- Skin Integrity and Wound CareDocumento47 páginasSkin Integrity and Wound CareCHALIE MEQUAinda não há avaliações
- 40 Items Comprehensive NCLEX ReviewDocumento9 páginas40 Items Comprehensive NCLEX ReviewLj FerolinoAinda não há avaliações
- Assessment SheetDocumento1 páginaAssessment SheetnkuligowskiAinda não há avaliações
- ICU Scoring Systems A Complete Guide - 2020 EditionNo EverandICU Scoring Systems A Complete Guide - 2020 EditionAinda não há avaliações
- NURSING CARE OF ADULTS II: Passbooks Study GuideNo EverandNURSING CARE OF ADULTS II: Passbooks Study GuideAinda não há avaliações
- Cdc-Guideline For Disinfection and Sterilization in Health-Care Facilities-2008Documento158 páginasCdc-Guideline For Disinfection and Sterilization in Health-Care Facilities-2008fuentenatura100% (1)
- Attach Any Wound Tracings Here Attach Any Wound Tracings HereDocumento2 páginasAttach Any Wound Tracings Here Attach Any Wound Tracings Herewiwi handayani100% (1)
- Cdc-Guideline For Disinfection and Sterilization in Health-Care Facilities-2008Documento158 páginasCdc-Guideline For Disinfection and Sterilization in Health-Care Facilities-2008fuentenatura100% (1)
- Sarung Tangan Operasi (Surgical Gloves)Documento23 páginasSarung Tangan Operasi (Surgical Gloves)wiwi handayaniAinda não há avaliações
- Detail of Trainee Particular Topic (1029)Documento145 páginasDetail of Trainee Particular Topic (1029)Muhammad Qasim KhanAinda não há avaliações
- Chest RadiographyDocumento19 páginasChest RadiographyClaraMonet PalomoAinda não há avaliações
- Mammography LeafletDocumento15 páginasMammography LeafletWidya Surya AvantiAinda não há avaliações
- Emetogenic Potential of Antineoplastic Agents PDFDocumento1 páginaEmetogenic Potential of Antineoplastic Agents PDFalfox2000Ainda não há avaliações
- Pott's Disease Night SweatsDocumento22 páginasPott's Disease Night SweatsjesuitkrisAinda não há avaliações
- Antibody-Alpha-Smooth Muscle ActinDocumento5 páginasAntibody-Alpha-Smooth Muscle ActinLauraNiiñoMartínezAinda não há avaliações
- DR - Asdala TransDocumento8 páginasDR - Asdala TransthorheavenAinda não há avaliações
- The Peptide-Hormone Glucagon-Like Peptide-1 Activates cAMP and Inhibits Growth of Breast Cancer CellsDocumento13 páginasThe Peptide-Hormone Glucagon-Like Peptide-1 Activates cAMP and Inhibits Growth of Breast Cancer CellsRidha Surya NugrahaAinda não há avaliações
- Handout For PatientsDocumento1 páginaHandout For Patientsapi-640781324Ainda não há avaliações
- Katalog TatambaDocumento19 páginasKatalog Tatambaarbendi ibatueAinda não há avaliações
- 1200S AlodineDocumento7 páginas1200S AlodineCodrin HarcoveanuAinda não há avaliações
- MG 2 - TEMA 1 Limba EnglezaDocumento4 páginasMG 2 - TEMA 1 Limba Englezamimi12345678910Ainda não há avaliações
- The Breast - Comprehensive Management of Benign and Malignant Diseases 5e WWW Bookbaz IrDocumento1.435 páginasThe Breast - Comprehensive Management of Benign and Malignant Diseases 5e WWW Bookbaz Irzahra mAinda não há avaliações
- Cannafest 2012 - Medical Cannabis in Israel v6Documento39 páginasCannafest 2012 - Medical Cannabis in Israel v6cannajoyAinda não há avaliações
- Secondary OsteoporosisDocumento22 páginasSecondary OsteoporosisBenny Chris TantoAinda não há avaliações
- Gastritis Symptoms, Causes, Types & TreatmentDocumento10 páginasGastritis Symptoms, Causes, Types & TreatmentMario100% (2)
- EndometriomaDocumento7 páginasEndometriomaErick Rafael AncaAinda não há avaliações
- Gallbladder cholesterolosis diagnosis in shortDocumento3 páginasGallbladder cholesterolosis diagnosis in shortfadoAinda não há avaliações
- LumnereDocumento232 páginasLumnereAlkaAinda não há avaliações
- Cancer of The Ovary PDFDocumento12 páginasCancer of The Ovary PDFDiego Fernando Alzate GomezAinda não há avaliações
- 0003489414532777Documento10 páginas0003489414532777Lilia ScutelnicAinda não há avaliações
- REFLEX Final ReportDocumento291 páginasREFLEX Final ReportDisicienciaAinda não há avaliações
- Entrepreneurship ProjectDocumento21 páginasEntrepreneurship Projectmansi_2460% (5)
- HemostasisDocumento58 páginasHemostasisRade GrbićAinda não há avaliações
- Jurnal Hafis Fix TampilDocumento14 páginasJurnal Hafis Fix TampilAnonymous Skzf3D2HAinda não há avaliações
- Handbookofvitaminc PDFDocumento436 páginasHandbookofvitaminc PDFQUOC HAAinda não há avaliações
- Milestone 8 PresentationDocumento6 páginasMilestone 8 PresentationericAinda não há avaliações
- C-Reactive Protein Test Details for Inflammation and InfectionDocumento2 páginasC-Reactive Protein Test Details for Inflammation and InfectionPorcha PacsayAinda não há avaliações
- Medical Application of Doppler TechniqueDocumento7 páginasMedical Application of Doppler TechniqueCharlotte LambardiAinda não há avaliações