Escolar Documentos
Profissional Documentos
Cultura Documentos
Untitled
Enviado por
api-193771047Descrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Untitled
Enviado por
api-193771047Direitos autorais:
Formatos disponíveis
Journal of Psychosomatic Research 75 (2013) 467474
Contents lists available at ScienceDirect
Journal of Psychosomatic Research
Psychosocial predictors of irritable bowel syndrome diagnosis and
symptom severity
Kristy Phillips, Bradley J. Wright, Stephen Kent
School of Psychological Science, La Trobe University, Melbourne, Australia
a r t i c l e
i n f o
Article history:
Received 14 April 2013
Received in revised form 1 August 2013
Accepted 2 August 2013
Keywords:
Alexithymia
Coping
Early life experiences
Emotional processing
Maladaptive schemas
Psychological distress
a b s t r a c t
Objective: This study explored the role of psychosocial factors in predicting both membership to either an irritable
bowel syndrome (IBS) or control group, and the severity of IBS symptoms.
Methods: A total of 149 participants (82 IBS and 67 controls) completed a battery of self-report inventories
assessing disposition and environment, cognitive processes, and psychological distress. Logistic regression analyses were used to assess predictive contribution of psychosocial variables to IBS diagnosis. Hierarchical linear regression was then used to assess the relationship of psychosocial variables with the severity of IBS symptoms.
Results: Signicant predictors of IBS were found to be alexithymia, the defectiveness/shame schema, and four coping
dimensions (active coping, instrumental support, self-blame, and positive reframing), 2 (6, N = 130) = 46.99,
p b .001, with predictive accuracy of 72%. Signicant predictors of IBS symptom severity were two of the
alexithymia subscales (difculty identifying feelings, and difculty describing feelings), gender, the schemas of
defectiveness/shame and entitlement, and global psychological distress. This model predicted IBS severity
F (6, 64) = 16.94, p b .001 and accounted for 61.3% of the variability in IBS severity scores.
Conclusion: Psychosocial variables account for a large percentage of the differences between an IBS and control group, as well as the variance of symptoms experienced within the IBS group. Alexithymia and the defectiveness schema appear to be related to both IBS and symptom severity.
2013 Elsevier Inc. All rights reserved.
Introduction
Irritable bowel syndrome (IBS) is a chronic functional gastrointestinal disorder (FGID). Characteristically IBS presents with intestinal problems including abdominal pain, diarrhoea, and constipation, with
additional symptoms of bloating, gas, swelling, and urgency [1]. Currently, no identiable structural abnormality, biological marker, or specic bacterial imbalance has been identied to explain these symptoms
[2]. IBS is diagnosed in around 10% of the general population and up to
25% in Western countries, making it the most common cause of referral
to a gastroenterologist [3,4]. Presently, the Rome III criteria is the most
comprehensive diagnostic tool for IBS; specifying that an individual experience abdominal pain, or discomfort for at least 3 days per month for
a 3 month period. These symptoms must be accompanied with two of
the following: changes in stool frequency (more or less), or form
(harder or looser), or the discomfort is relieved with defecation [5]. Patients' symptomology can appear medically unexplainable, meaning a
diagnosis is often accompanied with feelings of misunderstanding and
stigmatisation [6], which potentially reduces help-seeking behaviours
[7].
Corresponding author at: School of Psychological Science, La Trobe University,
Bundoora, VIC 3086, Australia. Tel.: +61 3 9479 2798; fax: +61 3 9479 1956.
E-mail address: s.kent@latrobe.edu.au (S. Kent).
0022-3999/$ see front matter 2013 Elsevier Inc. All rights reserved.
http://dx.doi.org/10.1016/j.jpsychores.2013.08.002
IBS signicantly impacts on an individual's quality of life and
wellbeing in areas including diet, travel, physical appearance, work,
family, education, and normal physical and sexual relationships [8,9].
In addition, IBS presents a burden to the health care system through
costs associated with primary-care doctors, gastroenterologists, hospital admissions, and prescription of pharmaceuticals [10].
Research into a biopsychosocial model for IBS [11] has identied a
number of psychosocial factors that strongly inuence IBS in three main
pathways: mediating the function and sensation of the gut, specically
inuencing the presenting symptom type and severity of pain reported;
causing certain illness behaviours; and lastly, mediating the risk of
onset, due to stress or trauma. Psychological interventions (e.g., cognitive
and behavioural, psychosocial, and long-term interpersonal psychotherapy) have been found to help IBS sufferers improve not only in psychopathology, social functioning, and quality of life, but also in gastrointestinal
symptoms and pain [1013] independent of psychological distress
[14,15]. However, the mechanisms relating to the efcacy of psychological treatments in IBS remain relatively unclear [15,16]. It is possible that
psychological interventions may help to address deeper issues not yet
understood.
Unlike short-term cognitive therapy that primarily focuses on two
levels of thoughts (automatic thoughts and underlying assumptions),
schema-focused cognitive behavioural therapy (CBT) addresses what
is believed to be the deepest level of cognitions, early maladaptive
schemas. Schemas are understood as pervasive implicit themes that a
468
K. Phillips et al. / Journal of Psychosomatic Research 75 (2013) 467474
person holds about self, others, and the world; formed in early years as a
result of some ongoing dysfunction in childhood where core emotional
needs were unmet [17]. Schemas interfere with relationships and
boundaries, self-acceptance, and a person's ability to satisfy basic
needs. Schemas have been related to a number of pathologies including
substance use, personality disorders, eating disorders, depression, and
psychosomatic illnesses [1720]. However, to date no research has explored the potential role schemas may play in explaining IBS.
Comorbid with IBS is often varying degrees of emotional and psychological distress, with many reaching diagnostic criteria for mood
and anxiety disorders [2123]. A recent review found that 40% to 60%
of patients with FGID, most commonly IBS, met criteria for a comorbid
psychiatric diagnosis, compared with only 25% of patients with structural bowel diseases, and 20% of the general population [24]. No causal relationship has been established between psychopathology and IBS;
however, pre-existing psychological disorders have been associated
with increased severity of IBS symptoms [25]. Hypochondriasis,
somatisation, and dissociation have been identied in some IBS sufferers [7,23,2528], although no study has found a unique psychological
prole for IBS.
IBS has been associated with higher traits of neuroticism
(characterised by emotional instability) and introversion, and
lower levels of openness and agreeableness [29]. Several studies
have also found that a many IBS sufferers score high in the personality
trait alexithymia [3032]. Alexithymia is dened as dysfunction in affect regulation, relating to difculties identifying and distinguishing between feelings and the physiological sensations of arousal; difculty
describing feelings and identifying them in others; a constricted imagination; and an outward cognitive style. Alexithymia does not always
present as blunted affect, but can present as emotional outbursts
where the individual is unable to identify the feeling state or relate it
to situations, memories, or higher-order emotions [33]. Alexithymia in
FGID and specically IBS impacts on responsiveness to treatment after
controlling for baseline gastrointestinal symptoms [30,31] and is associated with increased symptom severity [34].
More generally, the degree to which people actively avoid or are
unable to express and process difcult or distressing emotions has
been related to different illness symptoms; increased tension, perceived pain symptoms, and psychosomatic illnesses [3537]. Emotional processing is a process in which emotional disturbances are
absorbed, so that following the disturbance subsiding, the individual is able to return to normal functioning. Objectively this involves
returning to routine behaviours with diminished distress, even
when presented with reminders of the emotional disturbance [38].
The psychological mechanisms underlying emotional processing
are believed to be related to modications in associative memory
structures [39]. Despite the link between emotional processing and
psychosomatic illness, to our knowledge it has not yet been investigated in an IBS population.
Environmental factors that cause considerable emotional distress,
such as chronic stress, trauma, and abuse have been linked to IBS and
the severity of symptoms [4042]. Even a person's ability to manage
day to day stressors can inuence health and well-being. Recent research suggests that IBS patients rely more heavily on passive and
emotion-focused coping strategies [4345]. There is limited information, however, explaining how these coping strategies relate to IBS
symptomology.
The overall aim of the present study was to gain a better understanding of the differences in psychosocial functioning within an IBS group,
and when compared to a healthy control group. Firstly, we planned to
explore and ascertain the differences between groups. Secondly, we
aimed to formulate a comprehensive psychosocial prole for IBS. Finally,
we aimed to develop a psychosocial prole relating the severity of IBS
symptoms. Three groups of psychosocial determinants were explored:
dispositional and environmental factors; cognitive processes; and
psychological distress. Dispositional and environmental factors are
important risk factors for IBS, while cognitive and psychological distress
factors provide avenues for clinical intervention. By exploring these factors in combination we can determine the unique contribution of each
towards explaining IBS, and differences in symptomology.
Method
Participants
Participants presented as two discrete groups: a diagnosed IBS group
and a control group, comprising of 149 participants (82 IBS and 67 controls). IBS participants were diagnosed prior to participation, with diagnoses from a doctor (n = 34), a gastroenterologist (n = 46), or another
health professional (n = 2); diagnoses duration ranged from 2 weeks
to 40 years. IBS participants reported their predominant symptom to
be diarrhoea (n = 28), constipation (n = 20), alternating between diarrhoea and constipation (n = 28), or pain/bloating (n = 6) (Table 1).
Both IBS and control participants were excluded if they had a current or
previous diagnosis of bowel disease (e.g., ulcerative colitis). Inclusion
criteria specied Australian residents 18 years and over.
Study measures
IBS Symptom Severity Score (IBS-SSS) [46], a simple 5-question
self-report assessment tool, measured the severity of symptoms in
participants with a diagnosis of IBS. Symptoms range from mild to
severe and the maximum score is 500. Diagnosis classications are:
mild (75 to b 175), moderate (175 to b300), and severe (N 300). Reliability for the IBS severity score for the current study was good
(Cronbach's = .64).
Dispositional and environmental variables
The standardised version of the Life Events Inventory (LEI) [47] was
used to measure the incidence of stressful events experienced in the
previous 12 months. Participants respond in the negative or afrmative
to a list of 55 events, each item having an assigned weighting score to
represent the severity of stress typically associated. The LEI is a useful
tool to quantify stress in epidemiological studies, and to investigate
the relationship between stressful life events and vulnerability to psychopathology and illness outcomes [48,49]. Reliability for the LEI was
good (Cronbach's = .71).
Alexithymia was assessed with the 20-item Toronto Alexithymia
Scale (TAS-20) [50]. The TAS-20 has a three-factor structure: difculty identifying feeling, difculty describing feelings, and externally
Table 1
Demographic characteristics
Gender (%)
Males (females)
Age, year M (SD)
Relationship (%)
In a relationship
Single
Employment status (%)
Employed
Not employed
Highest level of education (%)
Pre-university level
Undergraduate level
IBS diagnosis duration, year M (SD)
IBS currently on medication for symptoms (%)
Predominant IBS symptom (n)
Constipation/Diarrhoea/Alternating/Pain
IBS
participants
(n = 82)
Control
participants
(n = 67)
22 (78)
43.8 (16.5)
25 (75)
38.8 (14.2)
69.5
30.5
77.6
22.4
62.2
37.8
76.1
23.9
51.2
48.8
10.2 (10.6)
39
20/28/28/6
40.3
59.7
.627
.051
.265
.066
.186
K. Phillips et al. / Journal of Psychosomatic Research 75 (2013) 467474
orientated thinking. The reliability of the scale is well established
( = .76 to .87). Internal consistency in the present study was
good (Cronbach's = .86). The TAS-20 has been used with IBS and
other FGID populations [3032].
Cognitive variables
The Emotional Processing Scale (EPS-25) [51], a 25-item questionnaire, was used to explore individuals' emotional experience, emotional
processing, and control of emotions in the past week. It has good reliability ( = .89) and sound testretest reliability. Cronbach's in the
present study was .82 to .90. To our knowledge the current study is
the rst to use the EPS-25 specically with an IBS clinical population.
Emotional processing has been linked with numerous other physical
and psychological health indicators [3537,52,53].
The Young Schema Questionnaire Short Form (YSQ-S2) [54] was used
to explore participants' maladaptive schemas (i.e., dysfunctional pervasive ideas that an individual holds about themselves and others believed
to have been formed in childhood by failing to have core emotional needs
met) [55]. The self-report questionnaire assesses 15 maladaptive schemas
(emotional deprivation, abandonment, mistrust/abuse, social isolation,
defectiveness/shame, failure, dependence/incompetence, vulnerability
to harm/illness, enmeshment, subjugation, self-sacrice, emotional inhibition, unrelenting standards, entitlement, and insufcient self-control/
self-discipline). It has sound reliability and validity; Cronbach's in the
present study was .83 to .89. The YSQ is a modest predictor of psychopathology scores [20] and personality disorders [56]. To our knowledge this
scale has no history in IBS research.
The Brief COPE, a 28-item self-report inventory [57] assessed commonly used coping strategies. The scale yields fourteen subscales, comprised of two items each. Reliability for the scale has been established
(Cronbach's = .42 to .93; .39 to .89 in the present study).
Psychological distress variables
The Symptom Checklist-90-Revised (SCL-90-R) [58] was used to assess psychological distress. This inventory has been standardised to differentiate healthy controls from psychiatric patients. Responses on a 5-point
Likert scale provide a global score of psychological distress, and scores on
9 major symptom dimensions: somatisation, obsessivecompulsive behaviour, interpersonal sensitivity, depression, anxiety, hostility, phobic
anxiety, paranoid ideation, and psychoticism. Psychometric properties
are good with testretest reliability ranging from = .78 to .90. In the
present study the Cronbach's ranged from .85 to .94. The SCL-90-R
has previously been used to assess psychological distress in IBS and
other FGID [59,60].
Procedure
Institutional ethics approval for this study was granted from the La
Trobe University Faculty of Science, Technology & Engineering Human
Ethics Committee. Following this, participants were recruited via print
advertisements distributed to IBS support services, local gastroenterologists, and around university campus. An online advertisement was also
placed with The Gut Foundation. Most participants completed the battery of self-reported questionnaires directly on-line, accessed remotely,
while a minority (n = 14), who were unable to access the internet,
were mailed out hard copies, that were later posted back to La Trobe.
All questionnaires were completed anonymously.
Statistical analysis
SPSS Windows Version 21.0 software (SPSS Inc., Chicago) was used
for all statistical analyses. Missing value analysis was conducted. Normality was assessed using visual inspection of histograms and stem
and leaf plots. Skew and kurtosis were examined at an alpha level of
b.001 [61]. Natural logarithmic transformations were necessary for
the subscales of the LEI, the Brief COPE, and the SCL-90-R. Non-
469
parametric testing (MannWhitney U) was necessary for four of the
subscales of SCL-90-R, which remained skewed. Due to signicant
skew in the Brief COPE subscales of denial, substance use, and religion,
these variables were omitted from the analysis. In order to normalise
the YSQ-S2 each variable was dichotomized. Following transformations,
group differences were explored using parametric (student t-tests) and
non-parametric (chi-square analysis and Mann-Whitney U) analyses.
An alpha level of .05 was used unless otherwise specied by the
Bonferroni adjustments. A logistic regression analysis was conducted
using a forward solution to predict group membership (IBS versus control) from predictor variables. Removal of 8 multivariate outliers was
necessary based on leverage and standardised residuals. A stepwise hierarchical linear regression analysis was then performed creating a predictive model for severity of symptoms in the IBS group. Six participants
were excluded from the analysis due to missing data and 5 outliers were
removed based on leverage, covariance ratios, and standardised residuals. All statistical procedures were devised a priori to assess our specic
research questions.
Results
Descriptive statistics
A MANOVA revealed no signicant multivariate F (5,149) = 1.75, p = .127, or
univariate differences in demographic characteristics for the IBS and control groups
using the Bonferroni correction (.05/5 = .01) (Table 1). Mean current symptoms
(over the previous 10 days) for the IBS group were reported to be moderately severe
(M = 261.9, SD = 98.5). One-way ANOVA determined a main effect due to symptom
type (constipation, diarrhoea, and alternating) F (3, 77) = 3.29, p = .025. Post hoc
analyses found that there was no signicant difference between the groups in symptom severity.
Psychosocial differences between IBS and control group
Signicant differences were detected for total alexithymia and two subscales of
alexithymia (difculty identifying feelings and externally orientated thinking), emotional
processing, instrumental support coping, somatisation, interpersonal sensitivity, depression, phobic anxiety, psychoticism, and global psychological distress (Table 2). Due to
multiple comparisons, the Bonferroni adjusted alpha levels apply to the COPE variables
(.05/11 = .004), LEI variables (.05/2 = .025), TAS-20 variables (.05/4 = .0125), and
the SCL-90-R variables (.05/10 = .005). Phi describes the correlation between two discrete variables, and as such the values range from 0 to 1, with Cohen suggesting that .1,
.3, and .5 correspond with small, medium, and large effects. Cohen's d effects of .2, .5,
and .8, also correspond to small, medium, and large effects [62].
Between-group differences for maladaptive schemas were determined by chi-square
analyses. A signicant group difference was identied for the emotional inhibition schema
(Table 3). Due to multiple comparisons the Bonferroni adjusted alpha levels were used
(.05/15 = .003).
Predicting IBS or control group membership
A forward-step logistic regression was performed in order to determine the signicant
predictors of IBS and control group membership (Table 4). Disposition and environmental
factors (age, gender, relationship status, education, total alexithymia, and alexithymia subscales, and exposure to signicant life events) were scrutinised rst as these factors are
considered stable risk factors. Cognitive factors (coping strategies, maladaptive schemas,
and emotional processing) were compared next. Lastly psychological distress variables
were compared. Six signicant predictors were identied in the forward regression,
which were then entered into a hierarchical logistic regression.
A test of the full model against a constant only model was statistically signicant, indicating that 6 of the predictors as a set reliably distinguished between the IBS and a control group, 2 (6, N = 130) = 46.99, p b .001. According to Cox and Snell R2 and
Nagelkerke R2 between 30% and 41% of the variability in scores between the IBS group
and the control group is explained by this set of variables. Overall, the model correctly
categorised 72% of participants as IBS or control (64% for controls and 79% for the IBS
group).
The Wald criterion demonstrated that all 6 predictors made statistically signicant
contributions. Odds ratios indicated that a person reporting IBS was 10 times higher for
each 1 unit increase in active coping, 6.5 times higher for a 1 unit increase in the maladaptive schema defectiveness/shame, and 5 times higher for a 1 unit increase in instrumental
support coping.
Predicting the severity of IBS symptoms
A linear regression using a forward-step solution was used to isolate the most significant variables that predicted IBS symptom severity. The variables that remained were
470
K. Phillips et al. / Journal of Psychosomatic Research 75 (2013) 467474
Table 2
Mean group differences for alexithymia, life events, coping strategies, emotional processing, and psychological distress
Scales
LEI
LEI
TAS-20
TAS-F1
TAS-F2
TAS-F3
EPS-25
COPE
COPE
COPE
COPE
COPE
COPE
COPE
COPE
COPE
COPE
COPE
SCL-90-R
SCL-90-R
SCL-90-R
SCL-90-R
SCL-90-R
SCL-90-R
SCL-90-R
SCL-90-R
SCL-90-R
SCL-90-R
Subscale predictor variables
Severity of life events
Frequency of life events
Total alexithymia
Difculty identifying feelings
Difculty describing feelings
Externally-orientated thinking
Total emotional processing
Self-distraction
Active coping
Emotional support
Instrumental support
Behaviour. disengagement
Venting
Positive reframing
Planning
Humour
Acceptance
Self-blame
Somatisation
Obsessivecompulsive
Interpersonal sensitivity
Depression
Anxiety
Hostility a
Phobic anxiety a
Paranoid ideation
Psychoticism a
Global psych distress a
IBS
Control
SD
SD
1.68
1.68
50.8
17.78
13.17
19.87
3.74
1.61
1.85
1.64
1.37
1.53
1.54
1.81
1.45
1.84
1.71
1.48
0.64
0.70
0.63
0.73
0.51
0.50
0.29
0.47
0.30
0.73
0.68
0.68
12.5
6.91
4.51
4.74
1.88
0.35
0.31
0.34
0.32
0.32
0.36
0.31
0.35
0.31
0.36
0.37
0.34
0.43
0.43
0.43
0.40
0.170.83
0.000.71
0.42
0.100.90
0.341.24
1.61
1.60
43.4
14.51
11.58
17.35
3.09
1.56
1.70
1.58
1.27
1.46
1.63
1.69
1.48
1.70
1.53
1.48
0.44
0.54
0.45
0.53
0.39
0.33
0.00
0.32
0.20
0.39
0.59
0.59
12.2
6.91
4.51
4.26
1.73
0.36
0.36
0.35
0.28
0.30
0.37
0.37
0.37
0.36
0.36
0.35
0.29
0.36
0.34
0.36
0.36
0.170.50
0.000.14
0.31
0.000.50
0.230.73
0.73
0.73
3.57
2.83
2.11
3.31
2.15
0.91
2.60
0.90
2.92
2.05
1.52
1.41
2.18
0.45
2.46
0.11
3.82
2.42
2.89
2.97
1.87
1.99
3.71
2.41
3.20
3.23
.464
.464
b.001
.005
.037
.001
.034
.365
.010
.368
.004
.043
.130
.162
.031
.584
.015
.914
b.001
.017
.005
.004
.063
.047
b.001
.017
.001
.001
0.11
0.13
0.60
0.47
0.35
0.56
0.36
0.14
0.45
0.17
0.33
0.23
0.25
0.35
0.08
0.42
0.50
0.00
0.63
0.40
0.46
0.50
0.32
0.41
The sample size differs from the total sample of participants due to missing data across subscales. Control participants n ranged from 64 to 67; IBS n ranged from 78 to 82.
a
Indicates that the variable is non-normally distributed as such non-parametric testing of MannWhitney U has been performed with descriptive statistics of median and interquartile
ranges reported, and Z-scores.
entered into a hierarchical regression. Disposition and environmental factors (age, gender,
relationship status, education, total alexithymia, and alexithymia subscales: difculty
identifying feelings, difculty describing feelings, and externally-orientated thinking,
and exposure to signicant life events) were scrutinised rst as these factors are considered stable risk factors. Cognitive factors (coping strategies, maladaptive schemas, and
emotional processing) were compared next. Lastly psychological distress variables were
compared. Six signicant predictors were identied in the forward-step regression,
which were then entered into a hierarchical linear regression. A statistically signicant
change was detected at each step of the model (Table 5).
The full model signicantly predicted IBS severity F (6, 64) = 16.94, p b .001 and
accounted for 61.3% of the variability in IBS severity scores. Two of the alexithymia subscales (difculty identifying feelings, and difculty describing feelings) and gender
explained approximately 38.5% of the variance in IBS severity. Maladaptive schemas of
defectiveness/shame, and entitlement explained 14% of the variance, and global psychological distress explained a further 8.5% of the variance.
Discussion
The results of the current study illustrate important psychosocial differences between the IBS group and the control group. Psychosocial factors can signicantly predict, within this group, whether a person has a
diagnosis of IBS or not. Further, psychosocial factors also predict the
subjective severity of IBS symptoms experienced.
Table 3
Group differences for cognitive schemas (YSQ-S2)
Maladaptive
IBS (n = 72)
Schemas
Response f
Response f
Endorsing Schema
Endorsing Schema
Emotional deprivation
Abandonment
Mistrust/abuse
Social isolation
Defectiveness/shame
Failure
Dependence
Vulnerable to harm/illness
Enmeshment
Subjugation
Self-sacrice
Emotional inhibition
Unrelenting standards
Entitlement
Insufcient self-control
Control (n = 61)
Yes
No
Yes
No
31
14
16
24
14
13
14
18
9
16
30
20
51
21
17
41
58
56
48
58
59
58
54
63
56
42
52
21
51
55
15
4
6
10
3
4
8
7
4
6
24
4
41
18
11
46
57
55
51
58
57
53
54
57
55
37
57
20
43
50
Phi
4.98
4.69
3.67
4.98
6.25
3.92
0.96
3.96
1.32
3.67
0.074
10.01
0.20
0.002
0.62
.026
.030
.055
.026
.012
.048
.328
.047
.250
.055
.786
.002
.652
.966
.432
0.19
0.19
0.17
0.19
0.22
0.17
0.09
0.17
0.10
0.17
0.02
0.28
0.04
0.01
0.07
K. Phillips et al. / Journal of Psychosomatic Research 75 (2013) 467474
471
Table 4
Hierarchical logistic regression analysis of the contributions of disposition/environment, cognitive, and psychological distress in predicting IBS or control group membership
95% condence interval
for odds ratio
Predictors
Disposition/environment
Alexithymia
Cognitive/coping
COPEactive coping
COPEinstrumental support
COPEself blame
COPEpositive reframing
YSQdefectiveness/shame
SE
Wald 2 test
df
0.64
0.21
9.64
.002
1.07
1.02
1.11
2.31
1.61
2.31
2.09
1.87
0.87
0.69
0.77
0.75
0.82
7.14
5.43
8.94
7.73
5.14
1
1
1
1
1
.008
.020
.003
.005
.023
10.09
5.01
0.10
0.12
6.48
1.85
1.29
0.02
0.03
1.29
54.98
19.43
0.45
0.54
32.53
Comparisons between IBS and controls
Several studies to date have investigated the psychological and social
differences between controls and individuals suffering from IBS. However, to our knowledge this is the rst study to investigate the dimensions
of emotional processing and maladaptive schemas in IBS. It is also, to our
understanding, the rst to look at psychosocial predictors of both categorical classication, and dimensional symptom severity. This in-depth
approach informs our understanding of how psychological interventions
can assist with varying presentations of this disorder. Consistent with
previous research [25,30,44,60,63], differences between the IBS and the
control groups were observed in psychological (i.e., somatisation, depression, phobic anxiety, and psychoticism and global psychological distress),
social (i.e., help seeking through instrumental support, and interpersonal
sensitivity), and emotional (alexithymia, emotional inhibition, and emotional processing) domains. Based on both signicant p values and medium effect sizes the most important group differences appear to exist on
the subscales of psychological distress (Cohen's d ranged from .35
to.60), total alexithymia (Cohen's d = .60), two alexithymia subscales;
externally orientated thinking (Cohen's d = .56) and difculty identifying feelings (Cohen's d = .47), and the emotional inhibition schema
(Phi = .28) [62].
One of our primary objectives was to develop a comprehensive psychosocial prole for IBS. A number of predictors were explored using a
regression model to distinguish between the two groups. Six predictors
were found to independently predict group membership to either the
IBS or control group; in combination they explained 30% to 41% of the
variance between the groups, correctly classifying 72% of the participants. Predictors of IBS included disposition (alexithymia) and cognitive
strategies (defectiveness/shame schema, seeking instrumental social
support, and active coping). Predictors of membership to the healthy
control group were cognitive strategies (positive reframing and selfblame). The most important discriminator was active coping with a
person scoring high in active coping being 10 times more likely to belong to the IBS group.
Table 5
Hierarchical linear regression depicting the contributions of dispositional/environmental,
cognitive, and psychological distress factors on IBS symptom severity (IBS-SSS)
Predictors
Final
summary
Beta
Step 1
TAS-20 difculty identifying feelings
TAS-20 difculty describing feelings
Gender
Step 2
YSQ entitlement
YSQ defectiveness/shame
Step 3
SCL-90R global psychological distress
Dependent variable: IBS-SSS.
Step
summary
r
sr
.238
.370
.153
.232
.510
.004
.149
.167
.318
.261
.069
.497
.344
.231
.053
.474
.643
.293
R2 ch
.384
b.001
.143
b.001
.086
b.001
Odds ratio
Lower
Upper
Several studies have reported a link between alexithymia and IBS in
both diagnosis and responsiveness to treatment [3032,34,64]. In the
present study one-fth of the IBS group's scores indicated that they
were highly alexithymic, however, on average the IBS group were within
the borderline alexithymic classication [32]. The control group differed
signicantly from the IBS group with a medium effect size (Cohen's
d = .6); reporting mean scores indicative of low alexithymia, also termed
non-alexithymic. In reecting on these ndings it is important to note
that alexithymia is not unique to IBS. Alexithymia has been reliably linked
to physical illness including chronic pain, and physical trauma (i.e., rape
and burn victims) [65,66]. Although alexithymia appears to be a relatively
stable and enduring personality trait in the general population [67], some
research has found that it emerged in individuals following a physical illness, and similarly decreased following illness resolution [66,68]. Due to
the cross-sectional nature of this study it is not possible to determine if
alexithymia is an antecedent to IBS, or a response. However, a common
thread that appears present in both alexithymia [69,70] and IBS [71,72]
is somatosensory amplication. Alexithymia may play a role in altering
and intensifying perception of physical sensations commonly found in
IBS, leading to health care seeking and subsequent diagnosis [2,7375].
This relationship requires further exploration.
Maladaptive schemas, which form a template of how we relate to
ourselves and others, are believed to be pervasive and enduring, having
origins in early childhood life experiences [55]. As this is the rst study
to explore schemas in IBS, these ndings suggest that the schema of defectiveness/shame formed prior to a diagnosis of IBS. People with this
schema may see themselves as innately awed and fear rejection. It
has been suggested that this schema may develop from a home environment that is detached and critical; where needs for stability, nurturance,
and empathy are unmet [55]. One study [76] found that parenting style
(particularly one that is rejecting and hostile) was a stronger predictor
of IBS somatic complaints, than specic abuse experiences. Our ndings
offer further evidence that negative parenting and family environments
are related to IBS, comparatively we found no relationship with reported stressful life experiences. It appears that substandard parentalchild
interactions may create vulnerabilities that impede psychological functioning and normal stress responses [76,77].
A further nding from the present study was that actively seeking
social support to cope with stresses predicted membership to the IBS
group. Despite a link between IBS and vulnerability to social isolation
[78], our ndings may potentially reect the fact that a large proportion
of participants were recruited from support groups and this may confound interpretation. Social support in IBS has been related to a reduction in pain symptomology by way of lowering stress levels [79].
Despite the identied group differences in reports of psychological distress (as measured by the SCL-90-R), psychological distress factors were
not found to signicantly contribute to a diagnosis of IBS.
Predictors of IBS symptom severity
The secondary objective of our investigation was to determine
which factors were predictive of IBS symptom severity, with an aim of
472
K. Phillips et al. / Journal of Psychosomatic Research 75 (2013) 467474
identifying predictors of severe symptomology. Despite recent increased interest in IBS severity subtypes (mild, moderate, and severe),
especially as an outcome measure for clinical intervention, to date
there has been limited research into the psychological predictors of
symptom severity [79,80]. The current research utilised the IBS-SSS to
assess IBS symptoms on a number of dimensions including, pain (both
severity and duration), distension (bloating and abdominal tightness),
satisfaction with bowel habits, and overall impact of symptoms on quality of life. A comprehensive psychosocial prole utilising dispositional,
cognitive, and psychological distress factors was determined to distinguish between IBS symptom severity. Six factors signicantly predicted
IBS symptom severity: two alexithymia subscales (difculty identifying
feelings and difculty describing feelings), gender, the maladaptive
schemas of entitlement and defectiveness/shame, and global psychological distress. In combination these factors accounted for 61.3% of
the variance in severity of symptoms.
Gender was found to signicantly predict IBS severity, with females
more likely to report severe symptomology. This could be indicative of
an unequal gender split; however, previous research into IBS has identied gender differences in brain activation and sensory amplication
to visceral stimulation [8183]. These ndings suggest possible different
gender-specic cognitive pathways involved in the processing of symptoms [82,83]. Psychological distress was also found to be a signicant
predictor of IBS symptom severity; consistent with previous research
[63,80]. As we did not assess for pre-existing psychopathology, it is
not possible to distinguish whether psychological distress inuenced
the severity of symptoms reported, or if the distress was a result of managing severe symptomology. However, gender and psychological distress appear to be the variables most related to IBS severity, with both
factors uniquely explaining 32% and 29% of the variance respectively.
Alexithymia predicted IBS group membership; however, it was the
subscales related to identifying and describing emotions that predicted
the severity of symptoms. It has been suggested that individuals high
in alexithymia have an impaired ability to identify and process emotions, including identifying stress or negative emotions [84], which is associated with reduced activation of the anterior cingulate cortex, a
critical region in cognitive and emotional processing [85]. The stress
alexithymia hypothesis suggests that in the presence of stressful life
events alexithymia prevents appropriate coping mechanisms [65]. Consequently, individuals may fail to act in a timely manner to reduce or
manage stress, or they may respond in unhealthy ways that prolong exposure to stress. The compounding impacts of stress may lead to somatosensory amplication, where somatic and visceral sensations are
experienced as more intense and unpleasant [84] as seen in severe IBS.
To our knowledge the relationship between maladaptive schemas
and IBS symptom severity has not previously been investigated. Along
with predicting a diagnosis of IBS, the schema of defectiveness/shame
also predicted the severity of symptoms experienced. The entitlement
schema also predicted symptom severity. Underlying this schema is believed to be a fragility that is related to emotional deprivation. People
with this schema may long for emotional intimacy, but fear it because
of a belief that they are defective, and consequently push others away.
They may believe that exposing aws will result in rejection [55], likely
leading to physical and emotional isolation. These ndings highlight the
importance of exploring early life experiences in IBS, and the long-term
implication for symptom exacerbation. As suggested earlier, adaption to
a hostile, or emotionally invalidating early home environment may result in profound cognitive and physiological changes [75]. Maladaptive
schemas have been found to play a role in addiction, personality disorders, and psychopathology [20,54,55], however only limited research
has been conducted into the relationship with medical illnesses [85],
and this should be an avenue for future research.
Although this study took a comprehensive approach to IBS there are
notable limitations. All data was self-reported including participants' diagnosis of IBS; therefore it is unclear if a common diagnostic measure
was used (such as the Rome III criteria). However, participants were
only accepted into the study if they reported that a formal diagnosis
had been provided by a health professional. While we report no differences between groups in their demographics (Table 1), we did not assess either group on dimensions of physical health, aside from IBS and
IBD; hence we cannot be certain that there are no other differences in
health status separating the groups. Another limitation was the data collection method; completion of questionnaires took place in the home,
university, or work environment, and hence we cannot discount that socially desirable responding, biased responses. A further limitation is that
the life event inventory only explored events in the past 12 months, yet
our participants' diagnosis ranged from 2 weeks to 40 years. While the
sample population may impact on the generalizability of the ndings, it
did not impact on the power of the study, with signicant ndings attributed to very large effect sizes. Finally, while we used the Bonferroni
adjustment for each cluster of related variables, we did not adjust for all
variables considered together; as such readers are advised to refer to
both p values and effect sizes when interpreting ndings.
In conclusion, meaningful differences were identied between the
IBS and control group on a number of environmental, cognitive, and
psychological distress factors, further supporting the role of psychosocial factors in IBS [11]. We determined the most important elements
that inuenced both diagnosis of IBS, and the severity of those symptoms. Our ndings suggest that IBS has a strong emotional component.
We found in both diagnosis and severity of symptoms there was a relationship with invalidating emotional experiences, as well as difculties
with emotional expression and recognition. Our ndings allude to the
importance of early life experiences in possibly creating a psychological
and physiological vulnerability to IBS and the severity of symptoms.
These ndings offer further support for the importance of psychological
interventions, most specically CBT and schema-focused CBT to assist
with core issues relating to IBS. Previous research has found that CBT
can directly improve quality of life and gastrointestinal symptoms in
IBS independent to addressing any psychological distress [15]. Although
we identied that psychological distress was predictive of increased
symptomology, other psychological aspects evidently play an inuential
role in IBS and its severity. CBT is currently the most effective psychological intervention for alexithymia [86,87], and CBT addresses maladaptive or inaccurate thoughts, beliefs, and behaviours, which often
maintain maladaptive schemas. IBS is not a uniform diagnosis; there
are important psychosocial variances. We have provided a rationale
for the value of thorough psychosocial assessment and therapeutic interventions targeted at individual symptom proles.
Conict of interest
All authors declare no conicts of interest in relation to the submitted manuscript.
Acknowledgments
We are grateful to the participants and thank the Irritable Bowel Information and Support (IBIS) group, Gut Foundation, and Gastro North
for their invaluable assistance in advertising and recruiting for this research study. We are also grateful to Dr. Ben Ong, of La Trobe University,
for his support regarding statistical analysis.
All authors had access to all the data in the study and have been
involved in the drafting and revisions of this paper, and provided approval for the nal version of this paper to be published. The corresponding author takes responsibility for the integrity and accuracy
of the data.
This study has been funded by La Trobe University, Melbourne.
However, the university had no role in the collection, management,
analysis, and interpretation of the data, or the preparation of this
manuscript.
K. Phillips et al. / Journal of Psychosomatic Research 75 (2013) 467474
References
[1] Schoepfer AM, Trummler M, Seeholzer P, Seibold-Schmid B, Seibold F. Discriminating
IBD from IBS: comparison of the test performance of fecal markers, blood leukocytes,
CRP, and IBD antibodies. Inamm Bowel Dis 2007;14:329.
[2] Rutter CL, Rutter DL. Illness representation, coping and outcome in irritable bowel
syndrome (IBS). Br J Health Psychol 2002;7:37791.
[3] Clarke G, Quigley EMM, Cryan JF, Dinan TG. Irritable bowel syndrome: towards biomarker identication. Trends Mol Med 2009;15:47887.
[4] Jones R, Lydeard S. Irritable bowel syndrome in the general population. Br
Med J 1992;304:8790.
[5] Gwee K. Irritable bowel syndrome and the Rome III criteria: for better or for worse?
Eur J Gastroenterol Hepatol 2007;19:4379.
[6] Crane C, Martin M. Perceived vulnerability to illness in individuals with irritable
bowel syndrome. J Psychosom Res 2002;53:111522.
[7] Trikas P, Vlachonkolis I, Fragkiadakis N, Vasilakis S, Manousos O, Paritsis N. Core
mental state in irritable bowel syndrome. Psychosom Med 1999;61:7818.
[8] Whitehead W, Burnett CK, Cook EW, Taub E. Impact of irritable bowel syndrome on
quality of life. Dig Dis Sci 1996;41:224853.
[9] Hungin AP, Whorwell PJ, Tack J, Mearin I. The prevalence, patterns and impact of irritable bowel syndrome: an international survey of 40,000 subjects. Aliment
Pharmacol Ther 2003;17:64350.
[10] Ljotsson B, Andreewitch S, Hedman E, Ruck C, Andersson G, Lindefors N. Exposure
and mindfulness based therapy for irritable bowel syndrome an open pilot
study. J Behav Ther Exp Psychiatry 2010;41:18090.
[11] Lackner JM, Mesmer C, Morley S, Dowzer C, Hamilton S. Psychological treatments for
irritable bowel syndrome: a systematic review and meta-analysis. J Consult Clin
Psychol 2004;72:110013.
[12] Craske ]MG, Wolitzky-Taylor KB, Labus J, Wu S, Frese M, Mayer E, et al.
A cognitive-behavioral treatment for irritable bowel syndrome using interoceptive
exposure to visceral sensations. Behaviour Research and Therapy 2011;49:41321.
[13] Garland EL, Gaylord SA, Palsson O, Faurot K, Mann JD, Whitehead WE. Therapeutic
mechanisms of a mindfulness-based treatment for IBS: effects on visceral sensitivity,
catastrophizing, and affective processing of pain sensations. Journal of Behavioral
Medicine 2012;35(6):591602.
[14] Creed F, Guthrie E, Ratcliffe J, Fernandes L, Rigby C, Tomenson B, et al. Does psychological treatment help only those patients with severe irritable bowel syndrome who also have a concurrent psychiatric disorder? Australian and New
Zealand Journal of Psychiatry 2005;39(9):80715. http://www.ncbi.nlm.nih.
gov/pubmed/16168039.
[15] Lackner JM, Jaccard J, Krasner SS, Katz LA, Gudleski GD, Blanchard EB. How does cognitive behavior therapy for IBS work?: a mediational analysis of a randomized clinical trial. Gastroenterology 2007;133:43344.
[16] Naliboff BD, Frese MP, Rapgay L. Mind/body psychological treatments for irritable
bowel syndrome. Evid Based Complement Alternat Med 2008;5:4150.
[17] Salkovskis PM. Frontiers of cognitive therapy. New York: Guilford Press; 1996 .
[18] Ball SA. Manualized treatment for substance abusers with personality disorders:
dual focus schema therapy. Addict Behav 1998;22:88391.
[19] Leung N, Waller G, Thomas G. Outcome of group cognitive-behavior therapy for bulimia nervosa: the role of core belief. Behav Res Ther 2000;38:14556.
[20] Stopa L, Thorne P, Waters A, Preston J. Are the short and long forms of the young
schema questionnaire comparable and how well does each version predict psychopathology scores? J Cogn Psychother 2001;15:25361.
[21] Mykletun A, Jacka F, Williams L, Pasco J, Henry M, Nicholson GC, et al. Prevalence of
mood and anxiety disorder in self-reported irritable bowel syndrome (IBS). An epidemiological population based study of women. Br Med J Gastroenterol 2010;10:
8897.
[22] Roy-Byrne PP, Davidson KW, Kessler RC, Asmundson GJG, Goodwin RD, Kubzansky
L, et al. Anxiety disorders and comorbid medical illness. J Lifeline Learn Psychiatry
2008;1:46781.
[23] Sykes MA, Blanchard EB, Lackner J, Keefer L, Krasner S. Psychopathology in irritable
bowel syndrome: support for a psychophysiological model. J Behav Med 2003;26:
36171.
[24] Levy RL, Olden KW, Naliboff BD, Bradley LA, Francisconi C, Drossman DA, et al. Psychosocial aspects of the functional gastrointestinal disorders. Gastroenterology
2006;130:144758.
[25] Gwee KA, Leong YL, Graham C, McKendrick MW, Collins SM, Walters SJ, et al. The
role of psychological and biological factors in postinfective gut dysfunction. Gut
1999;44:4006.
[26] Alim MA, Hussain AM, Haque MA, Ahad MA, Islam QT, Ekram ARMS. Assessment of
psychiatric disorders in irritable bowel syndrome patients. The Journal of Teachers
Association 2005;18:103.
[27] Salmon P, Skaife K, Rhodes J. Abuse, dissociation and somatisation in irritable bowel
syndrome: towards and explanatory model. J Behav Med 2003;26:118.
[28] Wilhelmsen I. The role of psychosocial factors in gastrointestinal disorders. Gut
2000;47:735.
[29] Dinan TG, O'Keane V, O'Boyle C, Chua A, Keeling PWN. A comparison of the mental
status, personality proles and life events of patients with irritable bowel syndrome
and peptic ulcer disease. Acta Psychiatr Scand 1991;84:268.
[30] Portincasa P, Moschetta A, Baldassarre G, Altomare DF, Palasciano G. Pan-enteric
dysmotility, impaired quality of life and alexithymia in a large group of patients
meeting ROME II criteria for irritable bowel syndrome. World J Gastroenterol
2003;9:22939.
[31] Porcelli P, Bagby RM, Taylor GJ, De Carne M, Leandro G, Todarello O. Alexithymia as
predictor of treatment outcome in patients with functional gastrointestinal disorders. Psychosomatic Medicine 2003;65:9118.
473
[32] Porcelli P, Taylor GJ, Bagby RM, De Carne M. Alexithymia and functional gastrointestinal
disorders: a comparison with inammatory bowel disease. Psychother Psychosom
1999;68:2639.
[33] Taylor GJ, Bagby RM, Parker JDA. Disorders of affect regulation: alexithymia in medical and psychiatric illness. Cambridge, UK: Cambridge University Press; 1997 .
[34] Endo Y, Shoji T, Fukudo S, Machida T, Machida T, Noda S, et al. The features of adolescent irritable bowel syndrome in Japan. Journal of Gastroenterology and Hepatology
2011;26:1069.
[35] Keefe FJ, Lumley J, Anderson T, Lynch T, Carson KL. Pain and emotion. J Clin Psychol
2001;57:587607.
[36] Brosschot JF, Aarsse HR. Restricted emotional processing and somatic attribution in
bromyalgia. Int J Psychiatry Med 2001;31:12746.
[37] Walter S, Leissner N, Jerg-Bretzke L, Hrabal V, Traue HC. Pain and emotional processing in psychological trauma. Psychiatr Danub 2010;22:46570.
[38] Rachman S. Emotional processing. Behav Res Ther 1980;18:5160.
[39] Foa E, Kozak MJ. Emotional processing of fear: exposure to corrective information.
Psychol Bull 1986;99:2035.
[40] Bennett EJ, Tennant CC, Piesse C, Badcock CA, Kellow JE. Level of chronic life stress
predicts clinical outcome in irritable bowel syndrome. Gut 1998;43:25661.
[41] Blanchard E B, Lackner JM, Jaccard J, Rowell D, Carosella AM, Powell C, et al. The role
of stress in symptom exacerbation among IBS patients. J Psychosom Res 2008;64:
11928.
[42] Leserman J, Drossman DA. Relationship of abuse history to functional gastrointestinal disorders and symptoms. Trauma Violence Abuse 2007;8:33143.
[43] Goodhand J, Rampton D. Psychological stress and coping in IBD. Gut 2008;57:
13457.
[44] Jones MP, Weissinger S, Crowel MD. Coping strategies and interpersonal support in
patients with irritable bowel syndrome and inammatory bowel disease. Clin
Gastroenterol Hepatol 2008;4:47481.
[45] Pelissier S, Dantzer C, Canini F, Mathieu N, Bonaz B. Psychological adjustment and
autonomic disturbances in inammatory bowel diseases and irritable bowel syndrome. Psychoneuroendocrinology 2010;35:65362.
[46] Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Aliment
Pharmacol Ther 1997;11:395402.
[47] Spurgeon A, Jackson CA, Beach JR. The life events inventory: re-scaling based on an
occupational sample. J Occup Med 2001;51:28793.
[48] Enns ME, Cox BJ. Perfectionism, stressful life events, and the 1-year outcome of depression. Cogn Ther Res 2005;29:54153.
[49] Lillberg K, Verkasalo PK, Kaprio J, Teppo L, Helenius H, Koskenvuo M. Stressful life
events and risk of breast cancer in 10,808 women: a cohort study. Am J Epidemiol
2003;157:41523.
[50] Bagby RM, Parker JDA, Taylor GJ. The 20-item Toronto alexithymia scale I: item selection and cross-validation of the factor structure. J Psychosom Res 1994;38:2332.
[51] Baker R, Thomas S, Thomas PW, Gower P, Santonastaso M, Whittleasea A. The emotional processing scale: scale renement and abridgement (EPS-25). J Psychosom
Res 2010;68:838.
[52] Baker R, Holloway J, Thomas PW, Thomas S, Owens M. Emotional processing and
panic. Behav Res Ther 2004;42:127187.
[53] Rachman S. Emotional processing, with special reference to post traumatic stress
disorder. Int Rev Psychiatry 2001;13:16471.
[54] Young JE, Brown G. Young schema questionnaire (revised ed.). In: Young JE, editor.
Cognitive therapy for personality disorders: a schema-focused approach. 2nd ed.
New York: Cognitive Therapy Center; 1994. p. 6376.
[55] Young JE, Klosko J, Weishaar ME. Schema therapy: a practitioner's guide. New York:
Guilford Press; 2003 .
[56] Reeves M, Taylor J. Specic relationships between core beliefs and personality
disorder symptoms in a non-clinical sample. Clin Psychol Psychother 2007;14:
96104.
[57] Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically
based approach. J Pers Soc Psychol 1989;56:26783.
[58] Derogatis LI. The SCL-90-R administration, scoring, and procedures manual. 3rd
ed.Minneapolis: National Computer Systems, Inc.; 1994.
[59] Drossman DA. Do psychosocial factors dene symptom severity and patient status in
irritable bowel syndrome? Am J Med 1999;107:41S50S.
[60] Locke GR, Weaver AL, Melton LJ, Talley NJ. Psychosocial factors are linked to functional gastrointestinal disorders: a population based nested casecontrol study.
Am J Gastroenterol 2004;99:3507.
[61] Tabachnick BG, Fidell LS. Using multivariate statistics. 5th ed.Boston: Pearson Education Inc.; 2007.
[62] Cohen J. A power primer. Psychol Bull 1992;112:1559.
[63] Jarrett M, Heitkemper M, Cain KC, Tuftin M, Walker EA, Bond EF, et al. The relationship between psychological distress and gastrointestinal symptoms in women with
irritable bowel syndrome. Nurs Res 1998;47:15461.
[64] Arun P. Alexithymia in irritable bowel syndrome. Indian J Psychiatry 1998;40:7983.
[65] Martin JB, Pihl RO. The stress alexithymia hypothesis: theoretical and empirical considerations. Psychother Psychosom 1985;43:16976.
[66] Wise TN, Mann LS, Mitchell D, Hryvniak M, Hill B. Secondary alexithymia: an empirical validation. Compr Psychiatry 1990;31:2848.
[67] Saarijaervi S, Salminen JK, Toikka T. Temporal stability of alexithymia over a
ve-year period in outpatients with major depression. Psychother Psychosom
2006;75:10712.
[68] Keltikangas-Jarvinen L. Concept of alexithymia: II. The consistency of alexithymia.
Psychother Psychosom 1987;47:11320.
[69] Wise TN, Mann LS. The relationship between somatosensory amplication,
alexithymia, and neuroticism. J Psychosom Res 1994;38:51521.
474
K. Phillips et al. / Journal of Psychosomatic Research 75 (2013) 467474
[70] Lumley MA, Strettner L, Wehmer F. How are alexithymia and physical illness
linked: a review and critique of pathways. J Psychosom Res 1996;41:
50518.
[71] Duddu V, Isaac MK, Chaturvedi SK. Somatization, somatosensory amplication,
attribution styles and illness behaviour: a review. Int Rev Psychiatry 2006;18:
2533.
[72] Chang L. Brain responses to visceral and somatic stimuli in irritable bowel syndrome:
a central nervous system disorder? Gastroenterol Clin North Am 2005;34:27180.
[73] Porcelli P, Affatati V, Bellomo A, De Carne M, Todarello O, Taylor GJ. Alexithymia and
psychopathology in patients with psychiatric and functional gastrointestinal disorders. Psychother Psychosom 2004;73:8491.
[74] Wilhelmsen I. Biological sensitisation and psychological amplication: gateways to
subjective health complaints and somatoform disorders. Psychoneuroendocrinology
2005;30:9905.
[75] Lackner JM, Gudleski GD, Blanchard EB. Beyond abuse: the association among parenting
style, abdominal pain, and somatization in IBS patients. Behav Res Ther 2004;42:4156.
[76] Repetti RL, Taylor SE, Seeman TE. Risky families: family social environments and the
mental and physical health of offspring. Psychol Bull 2002;128:23066.
[77] Porcelli P. Psychological abnormalities in patients with irritable bowel syndrome.
Indian J Gastroenterol 2004;23:639.
[78] Bertram S, Kurland M, Locke GR, Lydick E, Yawn BP. The patient's perspective of irritable bowel syndrome. J Fam Pract 2001;50:5217.
[79] Lackner JM, Brasel AM, Quigley BM, Keefer L, Krasner SS, Powell C, et al. The ties
that bind: perceived social support, stress, and IBS in severely affected patients.
Neurogastroenterol Motil 2010;22:893900.
[80] Spiegel B, Strickland A, Naliboff BD, Mayer EA, Chang L. Predictors of patient-assessed
illness severity in irritable bowel syndrome. Am J Gastroenterol 2008;103:253643.
[81] Lee OY, Mayer EA, Schmulson M, Chang L, Naliboff B. Gender-related differences in
IBS symptoms. Am J Gastroenterol 2001;96:218493.
[82] Naliboff BD, Berman S, Chang L, Derbyshire SW, Suyenobu B, Vogt BA, et al.
Sex-related differences in IBS patients: central processing of visceral stimuli. Gastroenterology 2003;124:173847.
[83] Berman S, Munakata J, Naliboff BD, Chang L, Mandelkern M, Silverman D, et al.
Gender differences in regional brain response to visceral pressure in IBS patients. Eur J Pain 2000;4:15772.
[84] Kano M, Fukudo S. The alexithymic brain: the neural pathways linking alexithymia
to physical disorders. Biopsychosoc Med 2013;7:19.
[85] Mizara A, Papadopoulos L, McBride SR. Core beliefs and psychological distress in patients with psoriasis and atopic eczema attending secondary care: the role of
schemas in chronic skin disease. Br J Dermatol 2012;166:98693.
[86] Bermond B, Vorst HC, Moormann PP. Cognitive neuropsychology of alexithymia: implications for personality typology. Cogn Neuropsychiatry 2006;11:33260.
[87] Kojima M. Alexithymia as a prognostic risk factor for health problems: a brief review
of epidemiological studies. Biopsychosoc Med 2012;6:19.
Você também pode gostar
- Prevalence of Irritable Bowel Syndrome in Caregivers of Patients With Chronic DiseasesDocumento8 páginasPrevalence of Irritable Bowel Syndrome in Caregivers of Patients With Chronic Diseasesapi-193771047Ainda não há avaliações
- Irritable Bowel Syndrome: Physicians' Awareness and Patients' ExperienceDocumento6 páginasIrritable Bowel Syndrome: Physicians' Awareness and Patients' Experienceapi-193771047Ainda não há avaliações
- Partner Burden in Irritable Bowel Syndrome: See Editorial On Page 156Documento5 páginasPartner Burden in Irritable Bowel Syndrome: See Editorial On Page 156api-193771047Ainda não há avaliações
- Anxiety-Depressive Disorders Among Irritable Bowel Syndrome Patients in Guilan, IranDocumento7 páginasAnxiety-Depressive Disorders Among Irritable Bowel Syndrome Patients in Guilan, Iranapi-193771047Ainda não há avaliações
- Anxiety, Stress, & Coping: An International JournalDocumento17 páginasAnxiety, Stress, & Coping: An International Journalapi-193771047Ainda não há avaliações
- Health Effects of Expressive Letter Writing: Mosher and Danoff-BurgDocumento19 páginasHealth Effects of Expressive Letter Writing: Mosher and Danoff-Burgapi-193771047Ainda não há avaliações
- Behaviour Research and TherapyDocumento9 páginasBehaviour Research and Therapyapi-193771047Ainda não há avaliações
- Healing Words: Using Affect Labeling To Reduce The Effects of Unpleasant Cues On Symptom Reporting in IBS PatientsDocumento9 páginasHealing Words: Using Affect Labeling To Reduce The Effects of Unpleasant Cues On Symptom Reporting in IBS Patientsapi-193771047Ainda não há avaliações
- Health Psychology Review: Click For UpdatesDocumento25 páginasHealth Psychology Review: Click For Updatesapi-193771047Ainda não há avaliações
- Original Papers: The Lifetime Prevalence of Anxiety Disorders Among Patients With Irritable Bowel SyndromeDocumento6 páginasOriginal Papers: The Lifetime Prevalence of Anxiety Disorders Among Patients With Irritable Bowel Syndromeapi-193771047Ainda não há avaliações
- Autonomic Effects of Expressive Writing in Individuals With Elevated Blood PressureDocumento13 páginasAutonomic Effects of Expressive Writing in Individuals With Elevated Blood Pressureapi-193771047Ainda não há avaliações
- Illness Perceptions Mediate The Relationship Between Bowel Symptom Severity and Health-Related Quality of Life in IBS PatientsDocumento12 páginasIllness Perceptions Mediate The Relationship Between Bowel Symptom Severity and Health-Related Quality of Life in IBS Patientsapi-193771047Ainda não há avaliações
- Does Expressive Writing Reduce Stress and Improve Health For Family Caregivers of Older Adults?Documento11 páginasDoes Expressive Writing Reduce Stress and Improve Health For Family Caregivers of Older Adults?api-193771047Ainda não há avaliações
- Feature: Biofeedback and Expressive Writing: Emotional Disclosure and Its Effects On HealthDocumento6 páginasFeature: Biofeedback and Expressive Writing: Emotional Disclosure and Its Effects On Healthapi-193771047Ainda não há avaliações
- In Search of Attachment: A Qualitative Study of Chronically Ill Women Transitioning Between Family Physicians in Rural Ontario, CanadaDocumento12 páginasIn Search of Attachment: A Qualitative Study of Chronically Ill Women Transitioning Between Family Physicians in Rural Ontario, Canadaapi-193771047Ainda não há avaliações
- Learning About Oneself Through Others: Experiences of A Group-Based Patient Education Programme About Irritable Bowel SyndromeDocumento10 páginasLearning About Oneself Through Others: Experiences of A Group-Based Patient Education Programme About Irritable Bowel Syndromeapi-193771047Ainda não há avaliações
- Psychodynamic Interpersonal Therapy and Improvement in Interpersonal Difficulties in People With Severe Irritable Bowel SyndromeDocumento8 páginasPsychodynamic Interpersonal Therapy and Improvement in Interpersonal Difficulties in People With Severe Irritable Bowel Syndromeapi-193771047Ainda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5795)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- ISBDFinal Book 2012 BDocumento53 páginasISBDFinal Book 2012 BvadamadaAinda não há avaliações
- The NysseDocumento208 páginasThe NysseSiti Nur JariyahAinda não há avaliações
- C1 Ob-Gyn-2020Documento33 páginasC1 Ob-Gyn-2020yabsera mulatuAinda não há avaliações
- Mentha Cordifelia TeaDocumento10 páginasMentha Cordifelia TeaMia Pearl Tabios ValenzuelaAinda não há avaliações
- Icpc 2 R PDFDocumento204 páginasIcpc 2 R PDFagni sukma fahiraAinda não há avaliações
- 0-0013 PDFDocumento24 páginas0-0013 PDFisabellaprie3Ainda não há avaliações
- Sample Only - Not For Clinical UseDocumento6 páginasSample Only - Not For Clinical Usenostra83Ainda não há avaliações
- CV - Microbiology Infection ControlDocumento14 páginasCV - Microbiology Infection ControlDrRahul KambleAinda não há avaliações
- Evedenced Based Rectal ProlapseDocumento16 páginasEvedenced Based Rectal Prolapsesub_zero9909Ainda não há avaliações
- II-E Altered PerceptionDocumento16 páginasII-E Altered PerceptionDharylle CariñoAinda não há avaliações
- Icmr Specimen Referral Form For Covid-19 (Sars-Cov2) : (These Fields To Be Filled For All Patients Including Foreigners)Documento2 páginasIcmr Specimen Referral Form For Covid-19 (Sars-Cov2) : (These Fields To Be Filled For All Patients Including Foreigners)Recruitment Cell Aiims BilaspurAinda não há avaliações
- Pap SmearDocumento75 páginasPap SmearRaine BowAinda não há avaliações
- Geriatric NursingDocumento64 páginasGeriatric NursingMark Elben100% (2)
- Takayasu S Arter It IsDocumento5 páginasTakayasu S Arter It IsButarbutar MelvaAinda não há avaliações
- Cholinergic SyndromeDocumento3 páginasCholinergic SyndromeEmman AguilarAinda não há avaliações
- (2020) (Libro) Health Psychology - The BasicsDocumento267 páginas(2020) (Libro) Health Psychology - The BasicsERIKA REYES GOMEZAinda não há avaliações
- 11 - Precautions For Handling Organic SolventDocumento2 páginas11 - Precautions For Handling Organic SolventMummy TheAinda não há avaliações
- Dr. Ernst Ziegler-1stEd PDFDocumento392 páginasDr. Ernst Ziegler-1stEd PDFcasAinda não há avaliações
- 3 Minute Exam DFSDocumento2 páginas3 Minute Exam DFSWeeChuan NgAinda não há avaliações
- Buildings and Structures: Padua EsteDocumento2 páginasBuildings and Structures: Padua EsteKevin LavinaAinda não há avaliações
- 1-Disease MechanismsDocumento5 páginas1-Disease MechanismsMarian Dane PunzalanAinda não há avaliações
- Clonazepam Drug CardDocumento1 páginaClonazepam Drug CardSheri490Ainda não há avaliações
- Sarcoidosis Pathophysiology, Diagnosis AtfDocumento6 páginasSarcoidosis Pathophysiology, Diagnosis AtfpatriciaAinda não há avaliações
- Chest Physician in Pune - Dr. Sharadchandra YadavDocumento8 páginasChest Physician in Pune - Dr. Sharadchandra YadavSharad YadavAinda não há avaliações
- Classical Western FormulasDocumento4 páginasClassical Western FormulasSofia MirandaAinda não há avaliações
- RANZCPdepression 2Documento120 páginasRANZCPdepression 2Random_EggAinda não há avaliações
- CASE PRESENTATION NEPHROTIC Syndrome-1Documento20 páginasCASE PRESENTATION NEPHROTIC Syndrome-1rohankananiAinda não há avaliações
- 2.1 NCM 109 - Pregestational ConditionsDocumento6 páginas2.1 NCM 109 - Pregestational ConditionsSittie Haneen TabaraAinda não há avaliações
- Panadeine: What Is in This LeafletDocumento3 páginasPanadeine: What Is in This Leafletradzi66Ainda não há avaliações
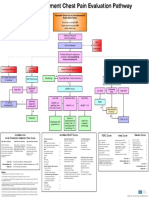
- Emergency Department Chest Pain Evaluation PathwayDocumento2 páginasEmergency Department Chest Pain Evaluation Pathwaymuhammad sajidAinda não há avaliações