Escolar Documentos
Profissional Documentos
Cultura Documentos
Br. J. Anaesth. 2001 Cherian 502 4
Enviado por
Alief M. ZarendraDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Br. J. Anaesth. 2001 Cherian 502 4
Enviado por
Alief M. ZarendraDireitos autorais:
Formatos disponíveis
British Journal of Anaesthesia 87 (3): 5024 (2001)
Prophylactic ondansetron does not improve patient satisfaction in
women using PCA after Caesarean section
V. T. Cherian1 and I. Smith2*
1
Department of Anaesthesia, Christian Medical College and Hospital, Vellore 632 004, India and
Department of Anaesthesia, North Staffordshire Hospital, Stoke-on-Trent, Staffordshire ST4 6QG, UK
*Corresponding author
Eighty-one consenting women undergoing elective Caesarean section under spinal anaesthesia
were randomly divided into two groups. In Group O patients, ondansetron 4 mg was given
intravenously at the end of the surgery and 8 mg added to the morphine solution in the PCA
syringe. Patients in Group P received only morphine via PCA syringe. Analgesia and nausea
were measured until PCA was discontinued 24 h after the operation. Women in the two
groups were similar with respect to age, duration of use of the PCA, amount of morphine
used, previous history of PONV, and incidence of motion sickness and morning sickness during
the current pregnancy. The number of women who complained of nausea and those needing
rescue antiemetic medication was signicantly less in Group O. However, there was no statistically signicant difference between the two groups in the patient's perception of the control
of nausea and their overall satisfaction. It was noted that PONV was more frequent among
women who had signicant morning sickness during early pregnancy and ondansetron was
benecial in reducing PONV in these women. Although the ondansetron reduced the incidence
of PONV and the need for further antiemetic medication, this did not affect patient's satisfaction regarding their postoperative care.
Br J Anaesth 2001; 87: 5024
Keywords: vomiting, nausea, postoperative; analgesia, patient-controlled; vomiting,
antiemetics, ondansetron; anaesthesia, obstetric
Accepted for publication: March 15, 2001
Patient-controlled analgesia (PCA) with i.v. opioids provides effective postoperative analgesia, but may be limited
by nausea and vomiting (PONV). Adding droperidol
(0.050.2 mg ml1) to morphine in the PCA syringe reduces
the incidence of PONV,16 but is associated with increased
sedation and extrapyramidal side effects. Ondansetron, a
5HT3 receptor antagonist, may be preferable in the
postpartum period because it lacks sedative effects that
may delay bonding with the baby. Although most studies on
ondansetron have shown that it reduces the incidence of
PONV, some workers regard this as only a `surrogate'
endpoint.7 8 Few investigators have examined the patient's
satisfaction with their treatment of PONV, which may be
regarded as the more important outcome.7 8
The aim of our study was to evaluate whether administering prophylactic ondansetron along with morphine via
PCA decreased PONV in obstetric patients and patient
satisfaction.
Methods and results
This double-blind, placebo-controlled study was approved by the local research ethics committee. Eightyone women undergoing elective Caesarean section at
term under spinal subarachnoid block were selected and
gave written informed consent. The sample had 80%
power to detect a halving of PONV from our baseline
value of 60%, found in an earlier audit. Patients with
hepatic, renal, psychiatric or neurological diseases and
those with pre-eclampsia were excluded. History of
PONV, motion sickness, smoking, and morning sickness
were noted. Subarachnoid anaesthesia was administered
using 2.52.8 ml of hyperbaric 0.5% bupivacaine,
through a 25-G pencil-point needle. All patients received
co-amoxyclav 1.2 g and oxytocin 10 units i.v. after the
baby was delivered and diclofenac 100 mg p.r. at the
end of the operation.
The Board of Management and Trustees of the British Journal of Anaesthesia 2001
Prophylactic ondansetron in women using PCA after Caesarean section
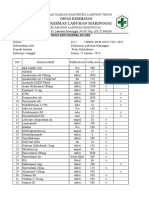
Table 1 Severity of postoperative nausea and vomiting and patient satisfaction with their control of nausea and vomiting and their overall level of care in the
two treatment groups. Values represent the most severe score recorded in the postoperative period (during PCA use) and are number (%) of occurrences or
responses
Nausea and vomiting (none/mild/severe/vomited)
Patients with morning sickness (n=52):
No PONV
Any PONV
Patients without morning sickness (n=29):
No PONV
Any PONV
Control of nausea and vomiting:
Good
Moderate
Poor
Overall satisfaction with care:
Good
Moderate
Poor
Group P (n=40)
Group O (n=41)
P value
15/2/5/18
26 / 5 / 3 / 7
7 (26%)
20 (74%)
16 (64%)
9 (36%)
0.023
0.005
8 (62%)
5 (38%)
10 (63%)
6 (37%)
24 (60%)
10 (25%)
6 (15%)
30 (73%)
9 (22%)
2 (5%)
35 (87.5%)
4 (10%)
1 (2.5%)
35 (85%)
5 (12%)
1 (3%)
Women were randomly allocated into two groups by
computer-generated random numbers in sequentially-numbered envelopes. Group P received a PCA with morphine (1
mg ml1), while Group O received ondansetron 4 mg
intravenously at the end of surgery plus 8 mg added to the
PCA morphine syringe (60 ml) (nal ondansetron concentration 0.13 mg ml1). The PCA pump was programmed to
deliver 1 ml per demand with a 3 min lockout and no
background infusion. Prochlorperazine 12.5 mg i.m. was
available as a rescue antiemetic to any patient who
requested it.
The incidence and severity of pain, sedation, nausea and
vomiting were assessed using four-point scales at 15 min
intervals in the immediate recovery period and then 4 hourly
until the PCA pump was discontinued. A midwife, unaware
of the contents of the PCA syringe, made all postoperative
assessments. Twenty-four hours later, one of the investigators assessed the patient for her perception regarding overall
satisfaction with her care, control of nausea and vomiting
and analgesia, using a scale of good, moderate or poor.
Data were analysed using the StatView statistical
package. Discrete variables were analysed using an
unpaired t-test or non-parametric tests. Categorical variables were analysed using the chi squared or Fisher's exact
test, as appropriate. In all cases a P value of <0.05 was
considered signicant.
Patient characteristics between the two groups were
similar except that the women in Group O were slightly
heavier. There were no signicant differences in the amount
of morphine used, history of motion sickness, morning
sickness, smoking, and PONV. The incidence of intraoperative hypotension and the requirement for an infusion
of oxytocin to assist postoperative uterine contraction did
not differ between the groups. There were no differences in
the degree of pain between the two treatment groups at any
time. Most patients were either pain-free or had only mild
pain. All patients were awake or arousable to voice at all
times.
0.960
0.258
0.9525
The incidence of nausea and vomiting was signicantly
lower in the ondansetron group (Table 1). Twenty-three
(57%) patients in Group P experienced severe nausea or
vomiting compared with 10 (24%) in Group O (P<0.01).
Eighteen women from Group P needed rescue antiemetic,
compared with only ve from Group O (P<0.01).
Ondansetron was effective in reducing the incidence of
PONV in those patients who had previously experienced
morning sickness but not in those who had not (Table 1).
There was no differential efcacy of ondansetron in patients
with and without previous PONV, smoking or motion
sickness, although the number of patients with these risk
factors was relatively small. Six patients in Group P and two
in Group O felt that the control of nausea and vomiting was
`poor', the difference was not signicant. One patient in
each group felt their overall care was unsatisfactory
(Table 1).
Comment
In post-Caesarean section patients, we found that adding
ondansetron to morphine in the PCA syringe reduces the
incidence of PONV and the requirement for antiemetic
rescue without increasing sedation. However, it seemed to
make little difference to the patient's perception of the
control of their nausea or her feeling of satisfaction with the
overall quality of care. This is consistent with other workers
who reported that reducing the incidence of PONV did not
improve patient satisfaction.9
There are various factors that may contribute to PONV.10
The most important predictors are female gender, previous
PONV, prolonged surgery, non-smoking, and motion sickness.10 We found that the incidence of PONV was higher
among women who had signicant morning sickness during
early pregnancy. Ondansetron was benecial in reducing
PONV in these women, but appeared to make little
difference in patients who did not experience signicant
morning sickness.
503
Cherian and Smith
Prophylaxis of PONV is usually administered once or
intermittently. There are a few studies where the antiemetic
was added into the PCA syringe.16 Droperidol was used in
most of these and was found to be effective, but caused
increased sedation, a side effect that we felt was undesirable
in the postpartum period. Postoperative sedation was rare in
our patients and was not increased by the use of
ondansetron. Alexander and colleagues showed that a
bolus of ondansetron 4 mg plus 0.13 mg ml1 in the PCA
syringe was effective in reducing PONV after orthopaedic
surgery.2 This technique has not previously been investigated in postpartum patients.
When questioned about their perception of nausea and
overall care, the responses of the two groups were similar,
despite considerable differences in the incidence of PONV
and request for rescue antiemetics. The high level of
satisfaction could partly be a result of the euphoria of having
a newborn baby and to the extra attention given by a
sympathetic investigator who spent extra time with them.
However, this should have applied equally to both groups.
Ondansetron is safe and effective, with a low incidence of
adverse effects such as headache, dizziness, and increased
liver enzymes. It has also been shown to be compatible with
morphine sulphate.2 There are no reports of adverse effects
of ondansetron in women who are breast feeding, although
the manufacturer cautions against its use in this situation.
However, similar advice applies to droperidol and prochlorperazine.
References
Acknowledgement
This study was conducted at the North Staffordshire Hospital, Stoke-onTrent, and was not funded by the pharmaceutical industry.
504
1 Kaufmann MA, Rosow C, Schnieper P, Schneider M. Prophylactic
antiemetic therapy with patient-controlled analgesia: a doubleblind,
placebo-controlled
comparison
of
droperidol,
metoclopramide and tropisetron. Anesth Analg 1994; 78: 98894
2 Alexander R, Lovell AT, Seingry D, Jones RM. Comparison of
ondansetron and droperidol in reducing postoperative nausea
and vomiting associated with patient-controlled analgesia.
Anaesthesia 1995; 50: 10868
3 Russell D, Duncan LA, Frame WT, Higgins SP, Asbury AJ, Millar
K. Patient-controlled analgesia with morphine and droperidol
following caesarean section under spinal anaesthesia. Acta
Anaesthesiol Scand 1996; 40: 6005
4 Williams OA, Clarke FL, Harris RW, Smith P, Peacock JE.
Addition of droperidol to patient-controlled analgesia: effect on
nausea and vomiting. Anaesthesia 1993; 48: 8814
5 Roberts CJ, Millar JM, Goat VA. The antiemetic effectiveness of
droperidol during morphine patient-controlled analgesia.
Anaesthesia 1995; 50: 55962
6 Walder AD, Aitkenhead AR. A comparison of droperidol and
cyclizine in the prevention of postoperative nausea and vomiting
associated with patient-controlled analgesia. Anaesthesia 1995;
50: 6546
7 Fisher DM. `The big little problem' of postoperative nausea and
vomiting. Do we know the answer yet? (Editorial). Anesthesiology
1997; 87: 12713
8 Fisher DM. Surrogate outcomes: meaningful not! (Editorial).
Anesthesiology 1999; 90: 3556
9 Scuderi PE, James RL, Harris L, Mims GR, III. Antiemetic
prophylaxis does not improve outcomes after outpatient surgery
when compared to symptomatic treatment. Anesthesiology 1999;
90: 36071
10 Watcha MF, White PF. Postoperative nausea and vomiting. Its
etiology, treatment, and prevention. Anesthesiology 1992; 77:
16284
Você também pode gostar
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Upt Puskesmas Labuhan Maringgai: Dinas KesehatanDocumento7 páginasUpt Puskesmas Labuhan Maringgai: Dinas KesehatanAlief M. ZarendraAinda não há avaliações
- MedicalDocumento456 páginasMedicalSri Sakthi Sumanan100% (1)
- Pharm 355Documento3 páginasPharm 355Alief M. ZarendraAinda não há avaliações
- Koagulasi Dan Flokulasi PrinsipDocumento129 páginasKoagulasi Dan Flokulasi PrinsipAndreaHalim0% (1)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Digestive SystemDocumento27 páginasDigestive SystemLealyn Martin BaculoAinda não há avaliações
- Stigma and IddDocumento22 páginasStigma and Iddapi-676636026Ainda não há avaliações
- First Dispensary RegistrationDocumento2 páginasFirst Dispensary RegistrationWBURAinda não há avaliações
- Selection of Site For HousingDocumento4 páginasSelection of Site For HousingAyshwarya SureshAinda não há avaliações
- Woman Burned by Acid in Random Subway Attack Has 16th SurgeryDocumento1 páginaWoman Burned by Acid in Random Subway Attack Has 16th Surgeryed2870winAinda não há avaliações
- List of Shelters in The Lower Mainland, June 2007Documento2 páginasList of Shelters in The Lower Mainland, June 2007Union Gospel Mission100% (1)
- Looking Forward: Immigrant Contributions To The Golden State (2014)Documento2 páginasLooking Forward: Immigrant Contributions To The Golden State (2014)CALimmigrantAinda não há avaliações
- A Sample Hospital Business Plan Template - ProfitableVentureDocumento15 páginasA Sample Hospital Business Plan Template - ProfitableVentureMacmilan Trevor Jamu100% (1)
- Constipation - MRCEM SuccessDocumento5 páginasConstipation - MRCEM SuccessGazi Sareem Bakhtyar AlamAinda não há avaliações
- First - Aid Common Emergencies and Safety Practices in Outdoor ActivitiesDocumento14 páginasFirst - Aid Common Emergencies and Safety Practices in Outdoor ActivitiesJhon Keneth NamiasAinda não há avaliações
- Caravan Tourism in West BengalDocumento2 páginasCaravan Tourism in West BengalUddipan NathAinda não há avaliações
- Anaphylaxis - 2Documento8 páginasAnaphylaxis - 2Ronald WiradirnataAinda não há avaliações
- Mil PRF 680Documento14 páginasMil PRF 680Wisdom SamuelAinda não há avaliações
- Rimso 50Documento1 páginaRimso 50monloviAinda não há avaliações
- Ayahuasca GuideDocumento27 páginasAyahuasca GuidedevoutoccamistAinda não há avaliações
- Errors of Eye Refraction and HomoeopathyDocumento11 páginasErrors of Eye Refraction and HomoeopathyDr. Rajneesh Kumar Sharma MD HomAinda não há avaliações
- Httpsjkbopee Gov InPdfDownloader Ashxnid 13580&type NDocumento221 páginasHttpsjkbopee Gov InPdfDownloader Ashxnid 13580&type NMONISAinda não há avaliações
- Britannia Industry LTD in India: Eat Healthy Think BetterDocumento12 páginasBritannia Industry LTD in India: Eat Healthy Think BetterMayank ParasharAinda não há avaliações
- Reimplantation of Avulsed Tooth - A Case StudyDocumento3 páginasReimplantation of Avulsed Tooth - A Case Studyrahul sharmaAinda não há avaliações
- Mental HealthDocumento80 páginasMental HealthSingYen QuickAinda não há avaliações
- The Trade Effluents (Prescribed Processes and Substances) Regulations 1992Documento2 páginasThe Trade Effluents (Prescribed Processes and Substances) Regulations 1992Lúcio FernandesAinda não há avaliações
- FAQ Mid Day MealsDocumento7 páginasFAQ Mid Day Mealsvikramhegde87Ainda não há avaliações
- Heat StrokeDocumento4 páginasHeat StrokeGerald YasonAinda não há avaliações
- A Case Study of Wastewater Reclamation and Reuse in Hebei Province in China: Feasibility Analysis and Advanced Treatment DiscussionDocumento2 páginasA Case Study of Wastewater Reclamation and Reuse in Hebei Province in China: Feasibility Analysis and Advanced Treatment DiscussionShalynn XieAinda não há avaliações
- Impact of Digital Media On Sleep Pattern Disturbance in Medical and Nursing StudentsDocumento10 páginasImpact of Digital Media On Sleep Pattern Disturbance in Medical and Nursing StudentsValarmathiAinda não há avaliações
- GHGK SDocumento48 páginasGHGK SAnonymous Syr2mlAinda não há avaliações
- STCW Section A-Vi.1Documento6 páginasSTCW Section A-Vi.1Ernesto FariasAinda não há avaliações
- COVID-19: Vaccine Management SolutionDocumento7 páginasCOVID-19: Vaccine Management Solutionhussein99Ainda não há avaliações
- Lifeline Supreme BrochureDocumento5 páginasLifeline Supreme BrochureSumit BhandariAinda não há avaliações
- HR Director VPHR CHRO Employee Relations in San Diego CA Resume Milton GreenDocumento2 páginasHR Director VPHR CHRO Employee Relations in San Diego CA Resume Milton GreenMiltonGreenAinda não há avaliações