Escolar Documentos
Profissional Documentos
Cultura Documentos
V11n3oa04 PDF
Enviado por
Gohar Ali UsmanDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
V11n3oa04 PDF
Enviado por
Gohar Ali UsmanDireitos autorais:
Formatos disponíveis
Original Article
Excessive Placental Calcification Observed in PIH Patients and its
Relation to Fetal Outcome
Pushpa Goswami, Hem Lata, Samreen Memon, Lal Baksh Khaskhelli
ABSTRACT
OBJECTIVE: To see the morphological changes in excessive placental calcification in pregnancy induced hypertension (PIH) and its relation with fetal outcome.
STUDY DESIGN: Prospective comparative study.
PLACE AND DURATION: This study was conducted from June 2008 to July 2009 at the department of Anatomy of Liaquat University of Medical & Health Sciences Jamshoro and placentae
were collected from department of Gynecology & Obstetrics of Liaquat University Hospital.
MATERIAL AND METHODS: Eighty freshly delivered placentae were collected from labor room
and gynecology operation theatre of Liaquat University Hospital. Forty placentae from parturient that had pregnancy induced hypertension (PIH) & forty placentae from parturient belonged
to uncomplicated pregnancy (control group). Ages of all parturient were between 17 to 32 years.
Fetal outcome and data was recorded. Placentae were measured on a weighing machine graduated in grams and diameter was measured with the help of a measuring tape in centimeters. Approximately five mm piece of placenta was taken and processed for histological examination.
RESULTS: The weight of placenta in control group ranges from 450 to 650 gm with a mean
weight of 526.258.414 gm having diameter from 19 to 24 cm with a mean of 21.2250.2148cm.
In PIH group weight of placenta ranges from 200 to 550gm with a mean weight of 432.25
11.889gm with diameter ranges from 10 to 16cms with a mean14.208 0.1914cm. The difference
in weight and diameter of placenta in PIH was found statistically significant when compared
with weight and diameter of normal placentae.
The birth weight of new born babies in control group was 1.8 kg to 3.6 kg with mean of 2.790
0.0689kg. In PIH group the fetal weight was 1.4 kg to 3.0 kg with mean weight of 2.195
0.0703kg.
CONCLUSION: Fetal outcome in terms of birth weight of newborn to mother having PIH and calcification of placentae (grossly and microscopically) was poor as compared to control group.
KEY WORDS: Placenta, PIH, calcification.
INTRODUCTION
The placenta is unique organ. Short lived by design,
its brief existence ensures survival of human embryo/
fetus in the intrauterine environment. The placenta
performs diversity of functions, ranging from anchoring
the fertilized ovum, preventing its rejection by the maternal immune system to enabling the transport of nutrients and wastes between the mother and the embryo/fetus 1.
The placenta was first recognized by early Egyptian,
while named by Realdus Columbus in 1559. The word
placenta comes from the Latin word plakos for cake or
from Greek plakenta mean flat, slab-like", referring
to its round and flat appearance in humans 2,3 .
Calcification is common in human placentae and recognized as a normal feature of maturation and aging
of this organ. The placental calcification is a constant
process occurring at a time in different parts of placenta to variable degree. The incidence of fetal distress in excessively calcified placenta is four times
JLUMHS SEPTEMBER-DECEMBER 2012; Vol 11: No. 03
more than in the uncalcified group. During pregnancy
placental growth must correspond with fetal growth
because increased calcification of placenta has serious negative consequences. Pathological maturation
of placenta leads to fetal growth restriction. During
pregnancy minor placental calcification tend to be
found at late stages of gestation which is associated
with tissue aging due to the induction of some age
related dystrophic changes in the placenta 4, 5.
Deposition of calcium salts is more on the maternal
surface, in the basal plate, along the septa and basement membrane of placental villi, perivillous space,
and subchorionic space, degenerative villi also show
calcification 6-8.
Morphologically calcium deposits are seen as white or
pale colored fine granules or clumps often felt as gritty
deposits. Microscopically calcification appears intracellular as well as extracellular basophilic deposits
when stained with haemotoxylin and eosin staining 9.
Excessive placental calcification may be associated
with Pregnancy induced hypertension (PIH), Placental
143
Excessive Placental Calcification Observed in PIH Patients
abruption, intra uterine growth restriction (IUGR), cigarette smoking 10.
Pregnancy-induced hypertension (PIH), also known as
toxemia of pregnancy, is a life-threatening disorder
that usually develops late in the second trimester or in
the third trimester. The ratio of this complication is
approximately 1:1500 pregnancies. It is a major cause
of maternal and perinatal morbidity and mortality
worldwide. It is an etiologically heterogeneous disorder that occurs in at least two subsets, one with normal or enhanced placental function, and another involving placental dysfunction and fetal growth restriction, often with asymmetric fetal body proportion, reduced fetal length, and preterm delivery 11, 12.
PIH significantly increases the risk of low birth weight,
both by increasing preterm birth as well as decreasing
fetal growth because of hypoxia consequent upon
utero-placental insufficiency; which when severe can
cause intrauterine death. Mothers with moderate to
severe PIH have smaller, irregular placentae, marginal
insertion of umbilical cord. Also calcification and histological features of vascular insufficiency like thrombosis, infarctions etc were observed. These changes
are directly proportional to the severity of the disease
and perinatal outcome becomes worse with advancing
grades of pregnancy induced hypertension.13,14,15
This study was conducted to examine excessive calcification in the placentae and its relation to fetal outcome in pregnancies complicated by PIH.
MATERIAL AND METHODS
This case control (prospective) study was conducted
from June 2008 to July 2009 at the department of
Anatomy of Liaquat University of Medical & Health
Sciences Jamshoro. Placentae were collected from
department of Gynecology & Obstetrics of Liaquat
University Hospital.
Eighty placentae were collected from labor room and
gynecology operation theatre of Liaquat University
Hospital. Forty placentae from parturient that had
pregnancy complicated by pregnancy induced hypertension & forty cases belonged to uncomplicated
pregnancy (control group). All samples collected randomly from singleton pregnancy. In control group,
women with normal blood pressure were included. In
pregnancy-induced hypertension, women having
blood pressure ranged 140/90mm of Hg or above
were included. The patients having hypertension or
diabetes before pregnancy were excluded. Age of all
women was between 17 to 32 years.
The data was collected on the prescribed proforma.
Fetal outcome was also recorded.
Method of sample collection
Placenta with umbilical cord and membranes was
JLUMHS SEPTEMBER-DECEMBER 2012; Vol 11: No. 03
collected after delivery. In all cases, the amnion and
chorion were removed from the placenta. The umbilical cord was cut at a distance of 5 centimeters from
the site of attachment. Placenta was washed with water, dried with the help of blotting paper and weighed.
The placentae along with the umbilical cord identified
by code numbers and were preserved in 10 % formalin solution in plastic jar for 48 hours for fixation. [16]
The study of gross morphology of placenta was conducted in the Department of Anatomy at Liaquat University of Medical & Health Sciences Jamshoro. Placentae were weighted on a weighing machine graduated in grams (gm) and diameter was measured with
the help of a measuring tape in centimeters (cm). All
placentae were cut in two equal halves and then were
further cut in small pieces. The cut pieces were labeled and randomly selected for further processing.
Slides were stained with H & E for routine histological
study and Von Kossa stain for calcium.17,18
RESULTS
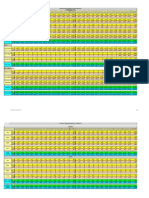
Morphological changes (gross and histological) were
recorded on the proforma. The results of the study are
depicted in text and tables.
The excessive calcification of placenta in women of
different parity and age group from PIH and control
group is shown in Table I. In both groups 80% cases
were between 17-28 years age. The primiparous in
control group were 20%, while it was 50% in PIH
group. Gravida 1-2 were equal in both groups and
representing 30% for each group. Gravida 3-7 were
50% for control group while it was 20% for PIH group.
The variables of interest related to placentae are
shown in Table II and III. The weight and diameter for
both groups were compared using t test. The results
show statistically significant (p=<0.001) difference in
weight and diameter of placenta in PIH group as compared to control group. The weight of placenta in control group ranges from 450 to 650 gm with a mean
weight of 526.25 8.414 gm (mean SEM). In PIH
group weight of placenta ranges from 200 to 550gm
with a mean weight of 432.25 11.889gm (mean
SEM). The diameter of placenta in control group
ranges from 19 to 24 cm with a mean of
21.2250.2148cm (mean SEM). In PIH group diameter of placenta ranges from 10 to 16cms with a
mean14.208 0.1914cm (mean SEM).
Fetal outcome was considered with respect to the
birth weight of the newborn. The birth weight of newborn in control group was 2.790 Kg (ranges from 1.8
to 3.6 Kg) as compare to mean birth weight of 2.195
Kg (ranges from 1.4 to 3.0 Kg). The difference in
mean birth weight was statistically significant as
shown in Table IV.
Microscopic examination was done by identifying
144
Pushpa Goswami, Hem Lata, Samreen Memon, Lal Baksh Khaskhelli
number of calcified areas per low power field. Numbers of classifications were counted by moving slide
from right to left then above downwards. There was a
tendency of more placental calcification in PIH placentae than that of control group. In control group the
number of calcified areas per/lpf ranges from 01 to 05
with a mean of 2.930.210 (mean SEM) while it was
10 to 20 with a mean of 14.97 0.445 (mean SEM)
in placentae from PIH group. The difference was statistically highly significant with p= <0.001 as shown in
table V. In general fetal outcome found poor in PIH
group than control when compared with respect to still
birth, intrauterine death, alive with Apgar score 03 or
more than 05.
When comparing still birth , it was 5% in control group
while it was 12.5% for PIH group, only 2.5% intrauterine death recorded in control as compared to 12.5%
in PIH group. Alive with Apgar score 03 was seen in
05(12.5%) in control, in PIH it was 10(25%). Apgar
score more than 05was seen high in control 32 (80%)
as compared with 20 (50%) in PIH shown in table VI.
TABLE IV: BIRTH WEIGHT OF NEWBORN (n = 40)
TABLE I: SHOWING AGE AND PARITY
still birth (sb)
Age Groups
No. of Cases
Control
PIH
17-20 years
10(25%)
04(10%)
21-24 years
07(17.5%)
12(30%)
25-28 years
15(37.5%)
16(40%)
29-32 years
08(20%)
08(20%)
Po
08(20%)
20(50%)
P1-2
12(30%)
12(30%)
P3-7
20(50%)
08(20%)
Parity
TABLE II: WEIGHT OF PLACENTAE
Placental
weight in
gms.
Min.
wt
Max.
wt
Mean
Sd
P
value
In control
450
650
526.25
53.214
<0.0001
In PIH
200
550
432.25
75.192
TABLE III: DIAMETER OF PLACENTAE
Placental
diameter in Min
cms
Max
Mean
SD
P
value
<0.0001
In control
19
24
21.225
1.3585
In PIH
10
16
14.208
1.2103
JLUMHS SEPTEMBER-DECEMBER 2012; Vol 11: No. 03
Weight of
newborn in Min
kg.
Max
Mean
Std
P
value
In control
1.8
3.6
2.790
.4361
<0.0001
In PIH
1.4
3.0
2.195
.4449
TABLE V: CALCIFICATIONS SEEN ON LIGHT
MICROSCOPY/LPF (10/20) (n = 40)
std.
Min
Max
Mean
Deviation
control
2.93
1.328
PIH
10
20
14.97
2.815
p
value
<0.0001
TABLE VI: SHOWING FETAL OUTCOME
n=40 Cases
Fetal out come
Control
PIH
02 (5%)
05 (12.5%)
Intra uterine death (iud)
01 (2.5%)
05 (12.5%)
apgar score of 03 or less
at 05 min
05 (12.5%)
10 (25%)
32 (80%)
20 (50%)
alive with apgar more
than 05
DISCUSSION
The placenta is a highly specialized organ of pregnancy that supports the normal growth and development of the fetus. The fetus, placenta and mother form
a composite triad of dynamic equilibrium, and dysfunction of any one of them can affect the others. Calcification is common in human placentae and recognized
as a normal part of maturation and aging of this organ.
The pathological maturation of placenta can lead to
fetal growth restriction which is the second most common cause of perinatal death after prematurity.[19, 20]
Excessive placental calcification is seen in Pregnancy
induced hypertension (PIH) which is the major cause
of perinatal morbidity and mortality globally, especially
in the developing world. PIH is associated with uteroplacental disease causing reduced uteroplacental perfusion, dysfunction resulting in fetal growth restriction,
reduced fetal length, and preterm delivery.21
Placental weight reduction is probably a consistent
finding in PIH. Our study showed reduced placental
145
Excessive Placental Calcification Observed in PIH Patients
weight in 66% patient of PIH then in placentae from
parturient of control group; this is reported to be 50%
by Sultana S, et al23 and Rahman24 while Palaskar PA
et al25 find it to be 77%.
The mean diameter of placentae from PIH found
about 66% less when compared to placentae of normal parturient (14.2 cm, 21.22 cm), a finding almost
identical to the finding reported earlier17.
In our study mean birth weight of babies born to PIH
mother was significantly low when compare to newborn of normal parturient (p <0.0001). This is attributed to uteroplacental insufficiency and same finding
has previously been reported by Udaina21 and Sarwan25.
Mufti P et al 26 has stated the Perinatal Mortality Rate
(PMR) in Pakistan is 50-60/1000 which is one of the
highest in the world. They attribute this to low birth
weight. PIH is associated with 3.4-fold increased in
perinatal mortality as shown in studies conducted by
Xiong X et al27, and Abbasi RM et al28. PIH is also
considered to be leading cause of still birth in 45%
cases as reported by Patil Y et al. The perinatal mortality was 52.0% in hypertensive women compared
with 29.8% for normotensive.. [29, 30]
Placental calcification is seen more frequently in primigravidas as reported by Russel J G B, Fielden P.
Identical results were observed in this study as well.
Similar results have previously been cited by Spirit B
A,Cohen W N, Weinstein H M. [31,32]
The calcium deposits are mostly observed in the villi
and basement membrane of the villi which is strongly
suggestive of uteroplacental insufficency because of
narrow lumen. We see calcification from one millimeter to biggest one of about 5 millimeters. In placentae
from PIH women, mean number of calcified areas on
gross as well as on microscopy seen were more than
in normal placenta. In the study conducted by Majumandar S form India observed similar findings [14] .
The still birth in this study was 12.5%, however the
fetal mortality and morbidity associated with PIH is
found to be responsible for 28% of stillbirths. [33]
Although placental abnormalities cannot be modified
to improve the perinatal outcome, identification in the
antenatal period, and early referral to hospitals, can
decrease the associated maternal and perinatal morbidity and mortality.
JLUMHS SEPTEMBER-DECEMBER 2012; Vol 11: No. 03
FIGURE I:
Placenta from normal
Placenta in PIH showing
parturient showing No
reduced diameter and
gross morphological ab- visible calcification
normality or calcification
PHOTOMICROGRAPH I: AREAS OF CALCIFICATION IN NORMAL PLACENTA IN VILLI AND IN THE
BASAL PLATE OF THE THIRD TRIMESTER PLACENTA (H & E10 MAGNIFICATION)
PHOTOMICROGRAPH II OF PLACENTA IN PIH
SHOWING CALCIFICATION BY ARROWS VON
KOSSA STAIN X10 MAGNIFICATION
146
Pushpa Goswami, Hem Lata, Samreen Memon, Lal Baksh Khaskhelli
PHOTOMICROGRAPH III OF PLACENTA IN PIH
SHOWING CALCIFICATION BY ARROWS IN VILLI
ON H & E X 20
REFERENCES
1. Emin M, Anna I. Bakardjiev and Susan J. The placenta: transcriptional, epigenetic, and physiological integration during development. J Clin Invest.
2010; 120(4):101625.
2. Huppertz B, Kingdom J.C.P. The placenta and
fetal membranes. In: Edmond DK editor. Dew
hurts Text book of Gynecology and obstetrics. 7th
ed. London: Blackwell publisher; 2007. p. 19- 25.
3. Wikipedia The free enclyopedia .Available from
Url http://en.wikipedia.org/ wiki/Placenta#cite_note
-0.
4. Sarkar M, Ingole IV, Ghosh SK, Bhakta A, Das
RS, Tandale S, et al. Calcification in Placenta. J
Anat Soc India 2007; 56(1):01-06.
5. Agababov RM, Abshina TN, Suzina NE, Vainshtein MB, Schartburd PM. Link between the early
calcium deposition in placenta and nanobacterial
like infection. J Biosic 2007; 32(6): 1163-8.
6. Kurjak A, Chervenak FA editors. Donald School
Textbook of Ultrasound in Obstetrics and Gynecology. 1st ed. New Dehli: Jaypee brothers; 2003.
7. Avery CR, Aterman K. Calcification of the basement membrane of placental villi J Path 2005; 103
(3):199-200.
8. Wentworth P. Macroscopic Placental Calcification
and Its Clinical Significance. Bjog 2005;72 (2):215
-222.
9. Kumar V, Abbas AK, Fausto N. Robbins & Cotran
pathological basis of disease. 7th ed. Phildilphia:
Elesevier ; 2004 pp 41-42.
10. Protocol/us_exam_obs_2.htm available from Url
http://www.droid.cuhk.edu.hk/ web/service/
ultrasound/exam_
11. Reilly BO, Bottomley C Rymer J. Essential of obstetrics and gynecology. Philadelphia: Elsevier;
JLUMHS SEPTEMBER-DECEMBER 2012; Vol 11: No. 03
2005.
12. Rasmussen S, Irgens LM. Fetal growth and body
proportion in Preeclampsia. Obstet Gynaecol
2003; 101(3):575-83.
13. Rath G, Garg K, Sood M. Insertion of umbilical
cord on the placenta of Hypertensive mothers.J
Anat Soc India 2005; 49(2):149-152.
14. Majumdar S, Dasgupta H, Bhattacharya K, Bhattacharya A. A Study of Placenta in Normal and
Hypertensive Pregnancies.J Anat Soc India 2005;
54 (2): 1-9.
15. Moldenhauer JS, Stanek J, Warshak C, Khoury J,
Sibai B.The frequency and severity of placental
findings in women with pre-eclampsia are gestational age dependent. Am J Obstet Gynaecol
2003; 189:1173-7
16. Udaina A, Bhagwat SS, Mehta CD. Relation b/w
placental surface area, Infarction and fetal distress in pregnancy induced hypertension with its
clinical relevance. J Anat Soc India 2004; 53 (1)
27-30.
17. Ashfaq M, Janjua M.Z, Channa M.A. Effect of gestational diabetes and maternal hypertension on
gross morphology of placenta. JAMCA 2005; 17
(1):44-7.
18. Qamar K, Minhas LA, Khan M Y. Histological
study of human placenta with emphasis on capillaries and syncytial knots of terminal villi. Pakistan
Armed Forces Medical journal 2009(4).
19. Guimares Filho HA, da Costa LL et al. Placenta:
angiogenesis and vascular assessment through
three-dimensional power Doppler ultrasonography. Arch Gynecol Obstet 2008; 277(3):195-200.
20. Jain K, Kavi V, Raghuveer CV, Sinha R. Placental
pathology in pregnancy induced hypertension
(PIH) with or without intrauterine growth retardation. Indian J Pathol Microbial 2007; 50(3): 533-7.
21. Gagnon R. Placental insufficiency and its consequences. European journal of
obstetrics and
gynecology Biology 2003; issue null (110):99-107.
22. Sarwar I, Abbasi A, Islam A. Abruptio placentae
and its complications at Ayub teaching hospital
Abbottabad. J Ayub Med Coll Abbottabad. 2006
Jan-Mar;18(1):27-31.
23. Sultana S, Hossain GA, Rahman H, Hasan
N,Manan S,Zannat S. Gross morphometry of human placenta in eclampsia. Mymensingh Med J
2006; 15(1):10-4.
24. Rahman MA, Rahman MH, Habib MA, Selimuzzaman SM. Placental changes in eclampia and
fetal outcome. Mymensingh Med J 2007; 16
(2):191-96.
25. Palaskar PA, Chaudhary KR, Mayadeo NM. Foeto
-placental weight relationship in normal pregnancy
and pre-eclampsia-eclampsia - a comparative
147
Excessive Placental Calcification Observed in PIH Patients
study. Bombay Hospital Journal 2001;43(3):361-3.
26. Udainia, A, Jain M.L. Morphological study of Placenta in pregnancy induced hypertension with its
clinical relevance. J Anat Soc India 2001; 50
(01):01-06.
27. Mufti P, Setna F, Nazir K. Early neonatal mortality:
Effects of interventions on survival of low birth
babies weighing 1000-2000g. J Pak Med
Assoc. 2006 Apr;56(4):174-6.
28. Xiong X, Buekens P, Pridjian G, Fraser WD. Pregnancy-induced hypertension and perinatal mortality. J Reprod Med 2007; 52(5):402-6.
29. Abbasi RM, Rizwan N, Mumtaz F, Farooq S. Feto
Maternal Outcome among Abruptio Placentae
Cases at a University Hospital of Sindh. JLUMHS
2008; 2: 106-109
30. Patil Y, Dcosta GF. Causes of mortality in still
birth-An Autopsy study. Bombay hospital journal
2007: 49 (2).
31. Sharief M, Manther AA. Abruptio placentae: perinatal outcome in normotensive and hypertensive
patients in Basra, Iraq. Eastern Mediterranean
Health Journal 1998; 04(2):319-323.
32. Spirit BA, Cohen N, Weinstein H. The incidence of
placental calcification in normal pregnancy. Radiology 1982; 142:707-11.
33. Hossain N, Khan N, Khan NH. Obstetric causes of
stillbirth at low socioeconomic settings. JPMA
2009; 59:744-46.
AUTHOR AFFILIATION:
Dr. Pushpa Goswami (Corresponding Author)
Department of Anatomy
Liaquat University of Medical & Health Sciences
(LUMHS), Jamshoro, Sindh-Pakistan.
Email: dr-pushparamesh1998@gmail.com
Dr. Hem Lata
Muhammad Medical College
Mirpurkhas, Sindh-Pakistan.
Dr. Samreen Memon
Department of Anatomy
LUMHS, Jamshoro, Sindh-Pakistan.
Dr. Lal Baksh Khaskhelli
Department of Anatomy
LUMHS, Jamshoro, Sindh-Pakistan.
JLUMHS SEPTEMBER-DECEMBER 2012; Vol 11: No. 03
148
Você também pode gostar
- Name: Activity 1: Microorganism Exercise 1 - Underline The Correct AnswerDocumento8 páginasName: Activity 1: Microorganism Exercise 1 - Underline The Correct AnswerSukanya SomasundaramAinda não há avaliações
- Fowler He Is Wise Who WatchesDocumento5 páginasFowler He Is Wise Who Watchesapi-351278812Ainda não há avaliações
- Research Proposal On Prevalence of PneumoniaDocumento26 páginasResearch Proposal On Prevalence of Pneumoniasolomon demissew62% (13)
- Oligohydramnion PDFDocumento6 páginasOligohydramnion PDFhusain abdul halimAinda não há avaliações
- Morfologi PlasentaDocumento6 páginasMorfologi PlasentayueldiAinda não há avaliações
- Breech Presentation: Caron J. Gray Meaghan M. ShanahanDocumento3 páginasBreech Presentation: Caron J. Gray Meaghan M. ShanahanTiwiAinda não há avaliações
- Comparative Study of Placental Cytoarchitecture in Mild and Severe Hypertensive Disorders Occurring During Pregnancy.Documento54 páginasComparative Study of Placental Cytoarchitecture in Mild and Severe Hypertensive Disorders Occurring During Pregnancy.prasadAinda não há avaliações
- D Farrar, A, B R Airey, C GR Law, B D Tuffnell, C B Cattle, B L DuleybDocumento6 páginasD Farrar, A, B R Airey, C GR Law, B D Tuffnell, C B Cattle, B L DuleybJoseLuisTiconaAinda não há avaliações
- Role of Gastric Lavage in Newborn With Meconium Stained Amniotic Fluid:a Randomized Controlled TrailDocumento3 páginasRole of Gastric Lavage in Newborn With Meconium Stained Amniotic Fluid:a Randomized Controlled TrailtriaanggareniAinda não há avaliações
- Can Placental Growth Factor in Maternal Circulation Identify Fetuses With Placental Intrauterine Growth RestrictionDocumento7 páginasCan Placental Growth Factor in Maternal Circulation Identify Fetuses With Placental Intrauterine Growth RestrictionagusAinda não há avaliações
- Constitutional Macrosomia - A Case ReportDocumento3 páginasConstitutional Macrosomia - A Case ReportIOSRjournalAinda não há avaliações
- RJME - Oficial Article - 63 - 02 - 2022 - 357-367Documento11 páginasRJME - Oficial Article - 63 - 02 - 2022 - 357-367mihail.boldeanuAinda não há avaliações
- Hadlock Ultrassonography in Obstetrics and Gynecology Cap 9 1994Documento16 páginasHadlock Ultrassonography in Obstetrics and Gynecology Cap 9 1994Antonio Alfim Malanchini RibeiroAinda não há avaliações
- Clinical Significance and Changes in The Morphology of Placenta in Pregnancy Induced HypertensionDocumento6 páginasClinical Significance and Changes in The Morphology of Placenta in Pregnancy Induced HypertensionIJAR JOURNALAinda não há avaliações
- Short Stature Is Associated With An Increased Risk of Caesarean Deliveries in Low Risk PopulationDocumento6 páginasShort Stature Is Associated With An Increased Risk of Caesarean Deliveries in Low Risk PopulationManangioma ManAinda não há avaliações
- Effects of Prepregnancy Dietary Patterns On Infant Birth Weight A Prospective Cohort StudyDocumento11 páginasEffects of Prepregnancy Dietary Patterns On Infant Birth Weight A Prospective Cohort StudyLola SantiaAinda não há avaliações
- Placental Histopathological Abnormalities and Poor Perinatal OutcomesDocumento8 páginasPlacental Histopathological Abnormalities and Poor Perinatal OutcomesMayada OsmanAinda não há avaliações
- Environmental Health PerspectivesDocumento36 páginasEnvironmental Health Perspectiveshubik38Ainda não há avaliações
- Fetal Biometei PDFDocumento134 páginasFetal Biometei PDFfariska amanizataAinda não há avaliações
- Comparison of The Accuracy of Clinical Methods For Estimation of Fetal WeightDocumento7 páginasComparison of The Accuracy of Clinical Methods For Estimation of Fetal WeightArdika PutraAinda não há avaliações
- The Impact of Maternal Body Mass Index On The Phenotype of Pre-Eclampsia: A Prospective Cohort StudyDocumento7 páginasThe Impact of Maternal Body Mass Index On The Phenotype of Pre-Eclampsia: A Prospective Cohort StudyAchmad Deza FaristaAinda não há avaliações
- Original ArticleDocumento8 páginasOriginal ArticleFelicia DympnaAinda não há avaliações
- Maternal NutDocumento7 páginasMaternal NutShirleuy GonçalvesAinda não há avaliações
- Accepted Manuscript: 10.1016/j.jpag.2018.09.005Documento8 páginasAccepted Manuscript: 10.1016/j.jpag.2018.09.005monicamoniccAinda não há avaliações
- Disorders in Amniotic FluidDocumento5 páginasDisorders in Amniotic FluidLatansa DinaAinda não há avaliações
- O@g Maternal and Fetal Mesures ContentDocumento22 páginasO@g Maternal and Fetal Mesures Contentjeya maniAinda não há avaliações
- Perinatal - Outcome - in - Oligohydramnios SynopsisDocumento16 páginasPerinatal - Outcome - in - Oligohydramnios SynopsisdhanrajramotraAinda não há avaliações
- Increasing Fetal Ovine Number Per Gestation Alters Fetal Plasma Clinical Chemistry ValuesDocumento12 páginasIncreasing Fetal Ovine Number Per Gestation Alters Fetal Plasma Clinical Chemistry ValuesHuang GlivecAinda não há avaliações
- Vol93 No.6 661 5058Documento6 páginasVol93 No.6 661 5058Titi Afrida SariAinda não há avaliações
- Amniotic Fluid Inflammatory Proteins and Digestive Compounds Profile in Fetuses With Gastroschisis Undergoing AmnioexchangeDocumento6 páginasAmniotic Fluid Inflammatory Proteins and Digestive Compounds Profile in Fetuses With Gastroschisis Undergoing AmnioexchangeMOACHAAinda não há avaliações
- OLIGOHIDRAMNIOSDocumento20 páginasOLIGOHIDRAMNIOSJorge Luis Sánchez AlarcónAinda não há avaliações
- Umbilical Cord Hernias: Prenatal Diagnosis and Natural HistoryDocumento4 páginasUmbilical Cord Hernias: Prenatal Diagnosis and Natural HistoryFriska GriffinAinda não há avaliações
- Abdominal Pregnancy: A Rare Presentation of Ectopic PregnancyDocumento3 páginasAbdominal Pregnancy: A Rare Presentation of Ectopic PregnancynajmulAinda não há avaliações
- Managing Newborn Ileostomies: Irish Medical Journal May 2014Documento4 páginasManaging Newborn Ileostomies: Irish Medical Journal May 2014VianAinda não há avaliações
- BergenDocumento13 páginasBergenElena VisterniceanAinda não há avaliações
- Gross Study of Placenta in Normal and IUGR CasesDocumento4 páginasGross Study of Placenta in Normal and IUGR CasesinventionjournalsAinda não há avaliações
- IUGRDocumento6 páginasIUGRabhagaurAinda não há avaliações
- Pregnancy Outcomes in Familial Hypercholesterolemia: Epidemiology and PreventionDocumento10 páginasPregnancy Outcomes in Familial Hypercholesterolemia: Epidemiology and PreventionsenkonenAinda não há avaliações
- Anupama Sharma, Et AlDocumento10 páginasAnupama Sharma, Et AlAGERI PUSHPALATHAAinda não há avaliações
- Crecimiento Fetal AnormalDocumento13 páginasCrecimiento Fetal AnormalShirley AntezanaAinda não há avaliações
- Ectopic Pregnancy Literature ReviewDocumento7 páginasEctopic Pregnancy Literature Reviewwgizkdvkg100% (1)
- The External Version in Modern Obstetrics: Esther Fandiño García and Juan Carlos Delgado HerreroDocumento21 páginasThe External Version in Modern Obstetrics: Esther Fandiño García and Juan Carlos Delgado HerreroCitrast NursyahidahAinda não há avaliações
- Increase Fetal Adiposity1Documento7 páginasIncrease Fetal Adiposity1Hervi LaksariAinda não há avaliações
- Obstetrics 2Documento6 páginasObstetrics 2najmulAinda não há avaliações
- Changes in Maternal Hemoglobin During Pregnancy and Birth OutcomesDocumento10 páginasChanges in Maternal Hemoglobin During Pregnancy and Birth OutcomesNimas Ayu Lestari NAinda não há avaliações
- Kobayashi 2014Documento7 páginasKobayashi 2014Mauricio Lopez MejiaAinda não há avaliações
- Bjo0118 0578 PDFDocumento11 páginasBjo0118 0578 PDFwe sagara dewiAinda não há avaliações
- The Interactive Effect of Prepregnancy Overweight/Obesity and Isolated Maternal Hypothyroxinemia On MacrosomiaDocumento8 páginasThe Interactive Effect of Prepregnancy Overweight/Obesity and Isolated Maternal Hypothyroxinemia On MacrosomiaAndres GallegosAinda não há avaliações
- Gastro SCH Is IsDocumento13 páginasGastro SCH Is IsferoAinda não há avaliações
- The Effect of Obesity On Pregnancy and Its Outcome in The Population of Oman, Seeb ProvinceDocumento12 páginasThe Effect of Obesity On Pregnancy and Its Outcome in The Population of Oman, Seeb ProvinceHazley ZeeAinda não há avaliações
- PREMATURE MedscapeDocumento10 páginasPREMATURE MedscapeKelompok BelajarAinda não há avaliações
- Article in Press: Effects of Central Obesity On Maternal Complications in Korean Women of Reproductive AgeDocumento8 páginasArticle in Press: Effects of Central Obesity On Maternal Complications in Korean Women of Reproductive AgeMhmmd FasyaAinda não há avaliações
- The Macrosomic Fetus: A Challenge in Current Obstetrics: Tore HenriksenDocumento12 páginasThe Macrosomic Fetus: A Challenge in Current Obstetrics: Tore HenriksenLNFAinda não há avaliações
- Doppler Ultrasound in The Assessment of Suspected Intra-Uterine Growth RestrictionDocumento10 páginasDoppler Ultrasound in The Assessment of Suspected Intra-Uterine Growth RestrictionGheavita Chandra DewiAinda não há avaliações
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocumento6 páginasEuropean Journal of Obstetrics & Gynecology and Reproductive BiologyDhia UlfajriAinda não há avaliações
- Katd 830Documento3 páginasKatd 830Anonymous SeK7brdMc4Ainda não há avaliações
- Jurnal Reading ObygnDocumento6 páginasJurnal Reading ObygnLimastani FebrianaAinda não há avaliações
- The Placental Basis of FetalDocumento18 páginasThe Placental Basis of FetalWuinnyLiHolguinAinda não há avaliações
- Solutio Plasenta JournalDocumento7 páginasSolutio Plasenta JournalAndi NatalonnaAinda não há avaliações
- A Case Report Abdominal Pregnancy MRI Vs USG RevisedDocumento14 páginasA Case Report Abdominal Pregnancy MRI Vs USG Revisedarnovareswari28Ainda não há avaliações
- 02 003 ValsamakisDocumento13 páginas02 003 ValsamakisCostin VrabieAinda não há avaliações
- Induction of Labor Using Foley Catheter With Weight Attached Vs Without WeightDocumento14 páginasInduction of Labor Using Foley Catheter With Weight Attached Vs Without Weightgrace liwantoAinda não há avaliações
- Medical School Companion Obstetrics and Gynecology Practice Question BookNo EverandMedical School Companion Obstetrics and Gynecology Practice Question BookAinda não há avaliações
- PathReport4 PDFDocumento4 páginasPathReport4 PDFGohar Ali UsmanAinda não há avaliações
- NYS PERB Contract Collection - Metadata HeaderDocumento63 páginasNYS PERB Contract Collection - Metadata HeaderGohar Ali UsmanAinda não há avaliações
- VG-165/D-765 VG-180/D-770: Instruction ManualDocumento65 páginasVG-165/D-765 VG-180/D-770: Instruction ManualGohar Ali UsmanAinda não há avaliações
- Top Passenger Car Brands On Social Media (India) : October, 2014Documento8 páginasTop Passenger Car Brands On Social Media (India) : October, 2014Gohar Ali UsmanAinda não há avaliações
- Clinical and Pathological Study of Retained Placenta in Iraqi BuffaloesDocumento6 páginasClinical and Pathological Study of Retained Placenta in Iraqi BuffaloesGohar Ali UsmanAinda não há avaliações
- AP.3.23.0.145 Manual PDFDocumento32 páginasAP.3.23.0.145 Manual PDFsike1977Ainda não há avaliações
- Production Sales PDFDocumento4 páginasProduction Sales PDFGohar Ali UsmanAinda não há avaliações
- Flare October 2014 PDFDocumento100 páginasFlare October 2014 PDFGohar Ali UsmanAinda não há avaliações
- Ahmed Shah AbdaliDocumento162 páginasAhmed Shah AbdaliAziz kakarAinda não há avaliações
- PSM 1 PapersDocumento16 páginasPSM 1 PapersP100% (1)
- Laboratory Diagnosis of Viral InfectionsDocumento54 páginasLaboratory Diagnosis of Viral InfectionsDeepak Singh Sangwan100% (2)
- DONNING and DOFFINGDocumento39 páginasDONNING and DOFFINGCatherine AteradoAinda não há avaliações
- MalariaDocumento4 páginasMalarianafrabAinda não há avaliações
- CHS MCQ Self AssessmentDocumento7 páginasCHS MCQ Self AssessmentDipesh ShresthaAinda não há avaliações
- ENT (Supposedly) 2.4 RhinitidisDocumento6 páginasENT (Supposedly) 2.4 RhinitidisDaniel Yakin Eliamar AritonangAinda não há avaliações
- Top 100 Ports 2021 Digital EditionDocumento124 páginasTop 100 Ports 2021 Digital EditionjatinAinda não há avaliações
- Procedure For Validating Digital SignatureDocumento3 páginasProcedure For Validating Digital SignatureAman BindAinda não há avaliações
- Term Paper Tungkol Sa DengueDocumento5 páginasTerm Paper Tungkol Sa Dengueaflsikxgf100% (1)
- Communityandenvironmentalhealth 180123140950Documento36 páginasCommunityandenvironmentalhealth 180123140950Grace RoseteAinda não há avaliações
- Final DraftDocumento5 páginasFinal Draftapi-451064930Ainda não há avaliações
- Practical MedicineDocumento630 páginasPractical MedicineYong Lim80% (5)
- Neonatal SepsisDocumento18 páginasNeonatal SepsissunnyisnghsingjAinda não há avaliações
- Neonatal Fungal InfectionDocumento4 páginasNeonatal Fungal InfectionirdinamarchsyaAinda não há avaliações
- Cholera: (Vibrio Cholerae)Documento2 páginasCholera: (Vibrio Cholerae)Freddy PanjaitanAinda não há avaliações
- The American Journal of Homoeopathy Vol. 3-4, 1849Documento362 páginasThe American Journal of Homoeopathy Vol. 3-4, 1849music75manAinda não há avaliações
- 1 Corona Says by Bishnu RaiDocumento9 páginas1 Corona Says by Bishnu RaiHuluu SmithAinda não há avaliações
- Pher SpeechDocumento2 páginasPher SpeechAlessaAinda não há avaliações
- Ischemic Optic NeuropathyDocumento7 páginasIschemic Optic NeuropathyJhoni Akbar DalimuntheAinda não há avaliações
- Health Survey and Development CommitteeDocumento10 páginasHealth Survey and Development CommitteeNidhiAinda não há avaliações
- VirologyDocumento131 páginasVirologyvaidyamAinda não há avaliações
- Insufficient Portable Water Threatens The Health and Development of The People in KibaweDocumento3 páginasInsufficient Portable Water Threatens The Health and Development of The People in KibaweDesiree Aranggo MangueraAinda não há avaliações
- Espiratory System AutopsyDocumento80 páginasEspiratory System AutopsyAbu ArshadAinda não há avaliações
- Covid-19 - Have We Ignored The Full Picture?Documento1 páginaCovid-19 - Have We Ignored The Full Picture?Shaun WoodageAinda não há avaliações
- Case Study CovidDocumento6 páginasCase Study CovidAngel Faith TirolAinda não há avaliações
- Reportable Diseases ConditionsDocumento1 páginaReportable Diseases Conditionsapi-297383596Ainda não há avaliações
- International Headache Classification III ICHD III 2013 Beta 1Documento180 páginasInternational Headache Classification III ICHD III 2013 Beta 1Fityan Aulia RahmanAinda não há avaliações