Escolar Documentos
Profissional Documentos
Cultura Documentos
Section 5: Problems of Oxygenation: Ventilation
Enviado por
JonathonDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Section 5: Problems of Oxygenation: Ventilation
Enviado por
JonathonDireitos autorais:
Formatos disponíveis
598
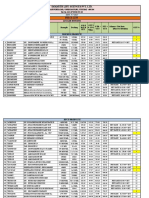
SECTION 5 Problems of Oxygenation: Ventilation
TABLE 29-7
DRUG THERAPY
Asthma and Chronic Obstructive Pulmonary Disease
ROUTE OF
DRUG
ADMINISTRATION
Antiinflammatory Agents
Corticosteroids
SIDE EFFECTS (SE)
COMMENTS*
With long-term use: cushingoid
appearance, skin changes (acne, striae,
bruising), osteoporosis, increased
appetite, obesity, peptic ulcer,
hypertension, hypokalemia, cataracts,
menstrual irregularities, muscle
weakness, immunosuppression,
catabolism.
With short-term use (e.g., <2 wk): sleep
disturbances, increased appetite.
Oral candidiasis (thrush), hoarseness,
irritated throat, headache, sinus
infection, upper respiratory infection.
Alternate-day therapy minimizes SE. Oral dose
should be taken in morning with food or milk.
When given in high doses, observe for epigastric
distress. Long-term corticosteroid therapy
requires supplementation with vitamin D and
calcium to prevent osteoporosis.
Discontinue gradually over time to prevent adrenal
insufficiency. If during tapering symptoms recur,
health care provider should be notified.
hydrocortisone (Solu-Cortef)
methylprednisolone
(Medrol, Solu-Medrol)
prednisone
IV
Oral, IV
fluticasone (Flovent HFA,
Flovent Diskus)
MDI, DPI
beclomethasone (Qvar)
MDI
budesonide (Pulmicort
Turbuhaler)
mometasone (Asmanex
Twisthaler)
ciclesonide (Alvesco)
DPI
Oral candidiasis, hoarseness, irritated
throat, dry mouth, cough, few systemic
effects except for headache.
Same as above.
DPI
Same as above.
MDI
Headache, nasopharyngitis.
Oral candidiasis and other localized oropharyngeal
effects (e.g., hoarseness). Fewer SE than other
ICSs because of small particle size with minimal
activation in oropharynx.
Nebulizer, MDI
Drying of oral mucosa, cough, flushing
of skin, bad taste.
Alternating schedules of -adrenergic agonists
and atropine administration may be helpful
in some patients. Temporary blurred vision if
sprayed in eyes. Use cautiously in patients with
narrow-angle glaucoma or prostatic enlargement.
Ongoing review to determine if this class
of anticholinergics places patients at risk for
cardiovascular events, including strokes.
DPI
Dry mouth, upper respiratory infection.
Blurred vision if powder comes in contact with
eyes. Must discontinue use of ipratropium while
on tiotropium. Patient must use short-acting
-adrenergic agonists for quick-relief medication.
See above related to class risk.
Subcutaneous
injection
Injection site reaction (e.g., bruising,
redness, warmth, pain).
Only for moderate to severe persistent allergic
asthma with symptoms not adequately
controlled by ICS. Not for acute bronchospasm.
Administer only under direct medical supervision
and observe patient for a minimum of 2 hr
following administration as anaphylaxis has been
reported with use.
Oral
Anticholinergics
Short-Acting
ipratropium (Atrovent HFA)
Not recommended for acute asthma attack. Rinse
mouth with water or mouthwash after use to
prevent oral fungal infections. Use of spacer
device with MDI may decrease incidence of oral
candidiasis. With inhaled corticosteroids, may
not see effects until after at least 2 wk of regular
treatment.
Same as fluticasone except less oral candidiasis
because of very small particle size which is
deposited deeper in the airways.
Long-Acting
tiotropium (Spiriva
HandiHaler)
Anti-IgE
omalizumab (Xolair)
BP, Blood pressure; CNS, central nervous system; DPI, dry powder inhaler; GI, gastrointestinal; HFA, hydrofluoroalkane (propellant); ICSs, inhaled corticosteroids; IV, intravenous;
MDI, metered-dose inhaler.
*For patient instructions in English and Spanish for the devices, see www.chestnet.org/patients/guides/inhaledDevices.php.
FDA is continuing to review clinical trial data to assess mood and behavioral adverse events related to drugs that act through the leukotriene pathway, and further updated
information can be found at www.fda.gov/medwatch.
CHAPTER 29 Obstructive Pulmonary Diseases
TABLE 29-7
599
DRUG THERAPYcontd
Asthma and Chronic Obstructive Pulmonary Disease
ROUTE OF
DRUG
ADMINISTRATION
Leukotriene Modifiers
Leukotriene Receptor Blocker
SIDE EFFECTS (SE)
COMMENTS*
Not for acute asthma attacks.
Take at least 1 hr before or 2 hr after meals.
Affects metabolism of erythromycin and theophylline. Not to be used to treat acute asthma
episodes.
Not to be used to treat acute asthma episodes.
zafirlukast (Accolate)
Oral tablets
Headache, dizziness; nausea, vomiting,
diarrhea, fatigue, abdominal pain.
montelukast (Singulair)
Oral tablets, chewable
tablets, oral granules
Well tolerated.
Oral tablets
Liver enzymes; dyspepsia, pain,
Monitor liver enzymes. May interfere with
metabolism of warfarin (Coumadin) and
theophylline. Not to be used to treat acute
asthma episodes.
Tachycardia, BP changes, nervousness,
palpitations, muscle tremors, nausea,
vomiting, vertigo, insomnia, dry mouth,
headache, hypokalemia.
Use with caution in patients with cardiac disorders
as -agonists may cause BP and heart rate,
CNS stimulation/excitation, and risk of
dysrhythmias. Has rapid onset of action
(1-3 min). Duration of action is 4-8 hr.
Tachycardia, nervousness, tremor (less
than albuterol).
Same as albuterol but cardiac effects
are less.
Too frequent use can result in loss of
effectiveness.
Leukotriene Inhibitor
zileuton (Zyflo CR)
headache.
2-Adrenergic Agonists
Inhaled: Short-Acting (SABA)
albuterol (Proventil HFA,
Ventolin HFA, ProAir HFA,
AccuNeb, VoSpire ER [oral
only])
levalbuterol (Xopenex,
Xopenex HFA)
pirbuterol (Maxair Autohaler)
Nebulizer, MDI, oral
tablets including
extended release
Note: Oral tablets not
for acute use, only
long acting
Nebulizer, MDI
MDI
Inhaled: Long-Acting (LABA)
salmeterol (Serevent)
DPI
formoterol (Foradil Aerolizer,
Perforomist)
DPI, nebulizer
Perforomist is for
nebulizer
Nebulizer
arformoterol (Brovana)
In asthma: Should never be used as
monotherapy. Should be used in
combination with inhaled steroids.
In COPD: Can be used as monotherapy.
Not used for rapid relief of dyspnea.
Headache, throat dryness, tremor,
dizziness, pharyngitis.
Angina, tachycardia, nervousness,
headache, tremor, dizziness.
Not to exceed two puffs q12hr. Not to be used
for acute exacerbations. Has a counter.
Can affect blood glucose levels. Should be used
with caution in patients with diabetes.
See formoterol.
See formoterol. For chronic COPD use.
Tachycardia, BP changes, dysrhythmias,
anorexia, nausea, vomiting,
nervousness, irritability, headache,
muscle twitching, flushing, epigastric
pain, diarrhea, insomnia, palpitations.
Wide variety of response to drug metabolism
exists. Half-life is by smoking and by heart
failure and liver disease. Cimetidine, ciprofloxacin, erythromycin, and other drugs may
rapidly theophylline levels. Taking drug with
food or antacids may help GI effects. Patient
must be encouraged to take drugs even when
feeling well.
Methylxanthines
IV agent: aminophylline
(second-line therapy)
Oral: theophylline
Oral tablets, IV, elixir,
sustained-release
tablets
Combination Agents
ipratropium and albuterol
(Combivent, DuoNeb)
fluticasone/salmeterol
(Advair Diskus or HFA)
budesonide/formoterol
(Symbicort)
mometsone furoate/
formoterol fumarate
(Dulera)
MDI, Nebulizer
DPI, MDI
MDI
MDI
Also see each component of medications for SE.
Chest pain, pharyngitis, diarrhea, nausea.
Patients must be careful not to overuse. Must take
as prescribed.
Headache, pharyngitis, oral candidiasis.
See salmeterol and fluticasone. Has a counter.
Comes in three different strengths.
Dysrhythmias, hypertension, paradoxic
See budesonide and formoterol. Has a counter.
bronchospasm.
Nasopharyngitis, sinusitis, headache
Você também pode gostar
- Treatment of Resistant and Refractory HypertensionDocumento21 páginasTreatment of Resistant and Refractory HypertensionLuis Rodriguez100% (1)
- CAMH Referral Form PDFDocumento3 páginasCAMH Referral Form PDFDeisel AssisAinda não há avaliações
- IvabradineDocumento33 páginasIvabradinepashaAinda não há avaliações
- NCLEX Cram SheetDocumento8 páginasNCLEX Cram SheetKaloy Kamao100% (5)
- FINAL Hypertension Medication Summary SSDocumento1 páginaFINAL Hypertension Medication Summary SSronique reidAinda não há avaliações
- Psych Notes Case FilesDocumento5 páginasPsych Notes Case FilesMitz JuneAinda não há avaliações
- Psych HX, MSEDocumento4 páginasPsych HX, MSELana AngelicaAinda não há avaliações
- Depression in Older Adults: A Treatable Medical ConditionDocumento12 páginasDepression in Older Adults: A Treatable Medical ConditionJose Alonso Aguilar Valera100% (1)
- Pharma Week 1-5Documento25 páginasPharma Week 1-5Rachelle CambaAinda não há avaliações
- Diabetes Medication SummaryDocumento1 páginaDiabetes Medication Summarywoody_2512Ainda não há avaliações
- E-CPG Management of Dementia (Third Edition) - 10 11Documento106 páginasE-CPG Management of Dementia (Third Edition) - 10 11Precious ChaiAinda não há avaliações
- PriceDocumento5 páginasPriceMubarak MHAinda não há avaliações
- Second-Generation Antipsychotics and Pregnancy ComplicationsDocumento9 páginasSecond-Generation Antipsychotics and Pregnancy ComplicationsDian Oktaria SafitriAinda não há avaliações
- Choose The Correct Answer For Questions (1 - 90)Documento12 páginasChoose The Correct Answer For Questions (1 - 90)حمزة الفنيني100% (3)
- Hypertensive Heart DiseasesDocumento5 páginasHypertensive Heart DiseasesserubimAinda não há avaliações
- Chapter 39 - Introduction To The Reproductive SystemDocumento13 páginasChapter 39 - Introduction To The Reproductive SystemJonathonAinda não há avaliações
- Clinical Guideline DepressionDocumento2 páginasClinical Guideline DepressionAllan DiasAinda não há avaliações
- Mechanisms of Vascular Disease: Robert FitridgeDocumento739 páginasMechanisms of Vascular Disease: Robert FitridgeasaAinda não há avaliações
- Chapter 49 - Drugs Used To Treat AnemiasDocumento12 páginasChapter 49 - Drugs Used To Treat AnemiasJonathon100% (2)
- Psychiatry Chapter 3Documento54 páginasPsychiatry Chapter 3Online Money In EthiopiaAinda não há avaliações
- NCSBN Practice Knowledge Network Call: Off-Label Drug Use 1/10/2013Documento23 páginasNCSBN Practice Knowledge Network Call: Off-Label Drug Use 1/10/2013Ari NurfikriAinda não há avaliações
- Psych History ScriptDocumento8 páginasPsych History ScriptRyan Loyd MarquezAinda não há avaliações
- Rational Use of AntibioticsDocumento39 páginasRational Use of Antibioticsjun sian100% (1)
- 640 802 Exam TopicsDocumento3 páginas640 802 Exam TopicsSajjad AhmadAinda não há avaliações
- Group 9 Huntingtons DiseaseDocumento7 páginasGroup 9 Huntingtons DiseaseLuis LazaroAinda não há avaliações
- Respiratory DrugsDocumento56 páginasRespiratory DrugsIra G. Delos Santos100% (1)
- Hearing LossDocumento26 páginasHearing LossNeicoAinda não há avaliações
- Acute Otitis Media - 6435 SOAPDocumento21 páginasAcute Otitis Media - 6435 SOAPMelinda Powell100% (1)
- Med - PPT Pneumonia For LectureDocumento79 páginasMed - PPT Pneumonia For Lectureapi-3856051100% (23)
- OsteoporosisDocumento19 páginasOsteoporosisLasa SiahaanAinda não há avaliações
- Global Albumin MarketDocumento3 páginasGlobal Albumin MarketiHealthcareAnalyst, Inc.0% (1)
- U4L2 Student GuideDocumento5 páginasU4L2 Student Guide-Esha-Ainda não há avaliações
- Se Insulin Stability ChartDocumento2 páginasSe Insulin Stability ChartWirmanAinda não há avaliações
- Preventive Care Checklist Form ExplanationsDocumento3 páginasPreventive Care Checklist Form ExplanationsKak KfgaAinda não há avaliações
- DiureticsDocumento61 páginasDiureticsJoyce WacukaAinda não há avaliações
- 1000 Ques & Ans File 2Documento54 páginas1000 Ques & Ans File 2bibin joyAinda não há avaliações
- Adhd Deficit Atencion AafpDocumento9 páginasAdhd Deficit Atencion AafpLisandro Marco del PontAinda não há avaliações
- GYNECOLOGY Chief ComplaintsDocumento3 páginasGYNECOLOGY Chief ComplaintsJennifer HerediaAinda não há avaliações
- Nose To Brain (Physiology of Nose)Documento26 páginasNose To Brain (Physiology of Nose)Soma YasaswiAinda não há avaliações
- Psychiatric Medication 2021Documento15 páginasPsychiatric Medication 2021Gyanendra ChaudharyAinda não há avaliações
- Foot and Toe Nail Care GuidelinesDocumento6 páginasFoot and Toe Nail Care GuidelineskyleAinda não há avaliações
- 6 - Pediatric Disorders - Rosales (P2) - AfssstDocumento11 páginas6 - Pediatric Disorders - Rosales (P2) - AfssstFranz Earl Niño AlbesaAinda não há avaliações
- Oncology Outpatient Provider Note 02-02-2023Documento5 páginasOncology Outpatient Provider Note 02-02-2023Randell ManjarresAinda não há avaliações
- IMG EmpAposterDocumento1 páginaIMG EmpAposterChiu LeoAinda não há avaliações
- North of Tyne Formulary Version 5 4finalDocumento194 páginasNorth of Tyne Formulary Version 5 4finalAnonymous VfSIDMyrmEAinda não há avaliações
- Agitated Patient Treatment MapDocumento1 páginaAgitated Patient Treatment MapMuhammed ElgasimAinda não há avaliações
- Prevalence of Long COVID Symptoms: An Observational, Cross-Sectional Follow-Up Study in Haryana, IndiaDocumento32 páginasPrevalence of Long COVID Symptoms: An Observational, Cross-Sectional Follow-Up Study in Haryana, IndianavneethAinda não há avaliações
- Skilled Immigration-Assessment-FormDocumento10 páginasSkilled Immigration-Assessment-FormBousekine Siham100% (1)
- Drug Recommendation GuideDocumento6 páginasDrug Recommendation GuideGenAinda não há avaliações
- SGLT 2 Inhibitors: Newer Paradigms in The Treatment of Heart Failure With Reduced Ejection FractionDocumento4 páginasSGLT 2 Inhibitors: Newer Paradigms in The Treatment of Heart Failure With Reduced Ejection FractionIJAR JOURNALAinda não há avaliações
- Blood Pressure Target: Insight From New ACC/AHA Hypertension GuidelineDocumento36 páginasBlood Pressure Target: Insight From New ACC/AHA Hypertension GuidelineRetnofAinda não há avaliações
- PG - M.Sc. - Psycology - 36333 PSYCHOPATHOLOGYDocumento203 páginasPG - M.Sc. - Psycology - 36333 PSYCHOPATHOLOGYAnanta ChaliseAinda não há avaliações
- Hpi Cheat Sheet PDFDocumento2 páginasHpi Cheat Sheet PDFTimothy HarwichAinda não há avaliações
- Health History - in Progress Attempt - Shadow HealthDocumento5 páginasHealth History - in Progress Attempt - Shadow HealthDaveAinda não há avaliações
- Drug Prescription in CKD and DialysisDocumento24 páginasDrug Prescription in CKD and DialysisAnitha SAinda não há avaliações
- Social Determinants of Health PDF - 3 Per Page NotesDocumento8 páginasSocial Determinants of Health PDF - 3 Per Page Notesapi-657470217Ainda não há avaliações
- Depression in Older Adults (Problem Tree Analysis)Documento8 páginasDepression in Older Adults (Problem Tree Analysis)Ishie De LeonAinda não há avaliações
- Patient Evaluation and PhysicalDocumento12 páginasPatient Evaluation and PhysicalsinAinda não há avaliações
- Macroeconomics Study GuideDocumento13 páginasMacroeconomics Study GuideChanelleAinda não há avaliações
- NYPD Discipline Matrix DraftDocumento53 páginasNYPD Discipline Matrix DraftepraetorianAinda não há avaliações
- Introduction To Nursing PharmacologyDocumento97 páginasIntroduction To Nursing PharmacologyLiel TorresAinda não há avaliações
- Step 2 CS Differential DiagnosesDocumento4 páginasStep 2 CS Differential DiagnosesnaimAinda não há avaliações
- Management of Hepatic Encephalopathy EASL - 220926 - 154633Documento19 páginasManagement of Hepatic Encephalopathy EASL - 220926 - 154633Charchit MehtaAinda não há avaliações
- Mnemonic PharmaDocumento13 páginasMnemonic Pharmamanoj kumarAinda não há avaliações
- Food Eponyms in Pathology PDFDocumento6 páginasFood Eponyms in Pathology PDFJose PhilipeAinda não há avaliações
- Chapter 25 - Muscle RelaxantsDocumento12 páginasChapter 25 - Muscle Relaxantslarry blueAinda não há avaliações
- Chapter 15 - Introduction To The ImmuneDocumento13 páginasChapter 15 - Introduction To The ImmuneJonathonAinda não há avaliações
- Infection Control ChartDocumento11 páginasInfection Control ChartbrittanyAinda não há avaliações
- Chapter 59 - Antiemetic AgentsDocumento11 páginasChapter 59 - Antiemetic AgentsJonathonAinda não há avaliações
- Care Map UtiDocumento1 páginaCare Map UtiJonathonAinda não há avaliações
- Chapter 56 - Introduction To The Gastrointestinal SystemDocumento11 páginasChapter 56 - Introduction To The Gastrointestinal SystemJonathonAinda não há avaliações
- Chapter 58 - Drugs Affecting Gastrointestinal MotilityDocumento12 páginasChapter 58 - Drugs Affecting Gastrointestinal MotilityJonathonAinda não há avaliações
- Chapter 55 - Drugs Acting On The Lower Respiratory TractDocumento13 páginasChapter 55 - Drugs Acting On The Lower Respiratory TractJonathonAinda não há avaliações
- Chapter 57 - Drugs Affecting Gastrointestinal SecretionsDocumento11 páginasChapter 57 - Drugs Affecting Gastrointestinal SecretionsJonathonAinda não há avaliações
- Antibiotics-AntiInfectives 2Documento1 páginaAntibiotics-AntiInfectives 2JonathonAinda não há avaliações
- Endocrine PharmDocumento2 páginasEndocrine PharmJonathonAinda não há avaliações
- Analgesics Non-Opiod Analgesics: Acetominophen (Tylenol) Therapuetic ClassDocumento5 páginasAnalgesics Non-Opiod Analgesics: Acetominophen (Tylenol) Therapuetic ClassJonathonAinda não há avaliações
- Chapter 51 - Diuretic AgentsDocumento11 páginasChapter 51 - Diuretic AgentsJonathon100% (2)
- Chapter 47 - Lipid-Lowering AgentsDocumento13 páginasChapter 47 - Lipid-Lowering AgentsJonathonAinda não há avaliações
- Pad Vs PVD ChartDocumento1 páginaPad Vs PVD ChartJonathonAinda não há avaliações
- Chapter 52 - Drugs Affecting The Urinary Tract and The BladderDocumento12 páginasChapter 52 - Drugs Affecting The Urinary Tract and The BladderJonathonAinda não há avaliações
- Chapter 48 - Drugs Affecting Blood CoagulationDocumento12 páginasChapter 48 - Drugs Affecting Blood CoagulationJonathon100% (1)
- Chapter 53 - Introduction To The Respiratory SystemDocumento13 páginasChapter 53 - Introduction To The Respiratory SystemJonathonAinda não há avaliações
- Chapter 54 - Drugs Acting On The Upper Respiratory TractDocumento13 páginasChapter 54 - Drugs Acting On The Upper Respiratory TractJonathonAinda não há avaliações
- Depressive Disorders, Care, and Safety ConsiderationsDocumento9 páginasDepressive Disorders, Care, and Safety ConsiderationsJonathonAinda não há avaliações
- MS Case Study: Patient HistoryDocumento2 páginasMS Case Study: Patient HistoryJonathonAinda não há avaliações
- Strategies For The in Vitro Production .. 2019bDocumento13 páginasStrategies For The in Vitro Production .. 2019bternyAinda não há avaliações
- Fact Sheet: BiologicsDocumento4 páginasFact Sheet: BiologicsAldiarsoAinda não há avaliações
- BioavailabilityDocumento76 páginasBioavailabilityprashil charkariAinda não há avaliações
- 2 Abubakar Et Al. Neuropharmacological Activity of Various Fractions Obtained From Solanum Aethiopicum Linn. Fruit in MiceDocumento13 páginas2 Abubakar Et Al. Neuropharmacological Activity of Various Fractions Obtained From Solanum Aethiopicum Linn. Fruit in MiceRabiu Abubakar AbdullahiAinda não há avaliações
- The Integrated Abc/fmr/ved-Analysis of Drug Consumption Among Hospice PatientsDocumento6 páginasThe Integrated Abc/fmr/ved-Analysis of Drug Consumption Among Hospice PatientsСофія ШунькінаAinda não há avaliações
- Aromatherapy 26 03 2021Documento168 páginasAromatherapy 26 03 2021Pelumi OninuireAinda não há avaliações
- PAR - 4849 - Nitrofurantoin MC Mylan - 9 MRT 2022Documento12 páginasPAR - 4849 - Nitrofurantoin MC Mylan - 9 MRT 2022Marcel JinihAinda não há avaliações
- Risk, Prevention, Diagnosis, and Management of Cellulitis and ErysipelasDocumento10 páginasRisk, Prevention, Diagnosis, and Management of Cellulitis and ErysipelasHanunAinda não há avaliações
- Drug Study: General Malvar ST., Davao CityDocumento2 páginasDrug Study: General Malvar ST., Davao CityKurt RoseteAinda não há avaliações
- PBL Parkinsons DiseaseDocumento23 páginasPBL Parkinsons DiseaseAyen PaloAinda não há avaliações
- Nejmoa 2204462Documento13 páginasNejmoa 2204462raphaelcspAinda não há avaliações
- Anderson S. Making Medicines A Brief History of Pharmacy and Pharmaceuticals. 1st Ed. New YorkDocumento1 páginaAnderson S. Making Medicines A Brief History of Pharmacy and Pharmaceuticals. 1st Ed. New YorkEdin SmajicAinda não há avaliações
- Pharmacy Endorsement LetterDocumento2 páginasPharmacy Endorsement LetterShielo Marie CabañeroAinda não há avaliações
- FIP Medication Use ReviewDocumento20 páginasFIP Medication Use ReviewIka RizkyAinda não há avaliações
- Phar 102 - Pharmaceutical CalculationsDocumento5 páginasPhar 102 - Pharmaceutical CalculationsojyrdAinda não há avaliações
- Pain and Palliative - Topic DiscussionDocumento7 páginasPain and Palliative - Topic Discussionapi-535001113Ainda não há avaliações
- Ondansetron A Selective 5-HT3 Receptor AntagonistDocumento16 páginasOndansetron A Selective 5-HT3 Receptor AntagonistRonald WiradirnataAinda não há avaliações
- The Pharmacokinetics of Long-Acting Antipsychotic Medications. 9 (2011)Documento8 páginasThe Pharmacokinetics of Long-Acting Antipsychotic Medications. 9 (2011)SolomonAinda não há avaliações
- Maudsley MRW FlyerDocumento2 páginasMaudsley MRW Flyerfabioviana67Ainda não há avaliações
- Dapus JurnalDocumento5 páginasDapus JurnalDwina RamadhaniAinda não há avaliações
- Handouts in NGCM103 Oxygenation Cardiovascular SystemDocumento7 páginasHandouts in NGCM103 Oxygenation Cardiovascular SystemJeenah HannahAinda não há avaliações
- Montra PharmacologyDocumento19 páginasMontra PharmacologytressAinda não há avaliações
- Antioxidant and Lipid Lowering Effects of Elaeocarpus Ganitrus in Cholesterol Fed RabbitsDocumento9 páginasAntioxidant and Lipid Lowering Effects of Elaeocarpus Ganitrus in Cholesterol Fed RabbitsKuberBajgainAinda não há avaliações
- Bahasa Inggris Hari Minggu DiambilDocumento7 páginasBahasa Inggris Hari Minggu DiambilWasid BaeAinda não há avaliações
- Alcohol Pharmacotherapy Meta AnalysisDocumento13 páginasAlcohol Pharmacotherapy Meta Analysisksqvrkz4dmAinda não há avaliações
- Anti CholinergicsDocumento25 páginasAnti Cholinergicsshahid kAinda não há avaliações