Escolar Documentos
Profissional Documentos
Cultura Documentos
33.first Permanent Molars
Enviado por
mirfanulhaqTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
33.first Permanent Molars
Enviado por
mirfanulhaqDireitos autorais:
Formatos disponíveis
Case 33
First permanent molars
Dental history
The child has been a regular patient since the age of 3. She
has required restorations in four primary molars, one
requiring local analgesia. Despite intensive preventive
advice and diet analysis, new carious lesions have been
present at each recall visit.
Examination
You ask the child to point to the painful tooth and she points
to an apparently sound upper left primary canine.
The appearance of the upper left quadrant is shown in
Figure 33.1. What do you see?
SUMMARY
A 7-year-old girl has pain from a first permanent
molar. What is the cause and how might it affect her
dental development?
An amalgam restoration with ditched or raised margins
on the palatal aspect of the first primary molar.
An apparently sound amalgam restoration in the second
primary molar.
Possible caries in an occlusal pit on the second primary
molar.
An erupting first permanent molar with the occlusal
surface not fully through the mucosa.
A small occlusal cavity in the confluence of the mesial
fissures of the permanent molar.
Plaque or food debris in the fissures.
How do you interpret the information so far and what
are the likely diagnoses?
The child is probably pointing at the wrong tooth. The canine
appears intact and children are often poor historians. They
often have difficulty in localizing the source of pain if the pain
is not present at the time of examination.
Pulpitis appears likely because the pain appears poorly
localized and is relatively intermittent. A history of hot or cold
or sweet exacerbating factors would point to this diagnosis.
The likely causes are caries beneath a restoration or carious or
traumatic pulpal exposure in one of the primary molars. Any
primary molar with an unrestored carious cavity or even a
clinically sound restoration should be examined closely for
signs of pulpal necrosis.
What features might suggest a necrotic pulp?
Fig. 33.1 The appearance on presentation.
History
Complaint
The patients mother reports that the child suffers intermittent spontaneous discomfort from the upper left teeth.
History of complaint
The symptoms have been vague, no sleep has been lost and
there has been no facial swelling. The patient has complained of the pain three or four times over the last month.
Medical history
The child is fit and well.
Extension of caries or fracture into the pulp
Discolouration of the crown
Swelling or tenderness in the buccal sulcus adjacent to
the tooth
Pus draining from a sinus in the mucosa, usually buccally
but occasionally lingually or palatally
Pus draining from the gingival margin
Facial swelling
Well-localized pain
None of these symptoms and signs is present. Pulpitis
seems likely.
Investigations
What investigations are indicated? Why?
Bitewing radiographs to check the proximity of
restorations to the pulps, the extent of the occlusal caries
CASE
33
156
First permanent molars
in the permanent molar and to detect small proximal
surface carious lesions.
Clinical examination of the other permanent molars for
caries.
Tests of vitality of primary and permanent molars are
unlikely to help because the results are unreliable in
children.
The left bitewing radiograph is shown in Figure 33.2. What
do you see? (Table 33.1)
to the 1970s, when caries was more prevalent, lesions larger
and fluoride products less available. It has been speculated
that the widespread use of fluoride toothpaste has resulted in
enamel that is resistant to smooth surface caries. Fluoride in
toothpaste has little effect on the progression of dentine
caries and is less effective against fissure caries. Carious
lesions in fissures that progress to dentine might well be able
to enlarge greatly before the occlusal enamel cavitates
significantly. In a partly erupted tooth such as this there is no
significant occlusal force to fracture away any unsupported
enamel. This hypothesis seems feasible but there is no
evidence that the prevalence of occult lesions is affected by
fluoride exposure. An alternative hypothesis is that there is
external resorption of the crown before eruption, hollowing
out the crown through a small occlusal defect. After eruption
the cavity would become carious. Coronal resorption is
usually considered unusual but it is difficult to prove that it
was not present after caries supervenes without pre-eruption
radiographs. Radiographs are required to diagnose occult
lesions.
Does this discovery have significance for other teeth?
Fig. 33.2 The left bitewing radiograph.
Yes, it will be necessary to examine all the other permanent
molars clinically again. Carious lesions may have been missed.
The discovery of this large lesion should make you more
suspicious and you should consider exploration of any other
suspicious fissures.
Table 33.1 Features seen in Figure 33.2
Tooth
Features
First primary molar
The restoration appears to be in the pulp chamber but
reinspection of the tooth clinically will remind you that the
restoration is on the palatal aspect of the tooth and is only
superimposed on the pulp chamber. No proximal surface
caries is present.
Second primary molar
First permanent molar
The restoration appears sound, with no radiolucency between
the base of the restoration and the pulp to suggest caries.
There is sufficient sound dentine (approximately 12mm)
between the restoration and the pulp to make pulpal exposure
unlikely. No proximal surface caries is present.
There is an extensive dentine radiolucency under the small
occlusal cavity indicating caries. The deep aspect of the lesion
is ill-defined, indicating rapid progression. The lesion extends
close to the distobuccal pulp horn and there may be
involvement of the pulp.
Diagnosis
What is your final diagnosis?
Pulpitis in the upper left first permanent molar, in response to
a deep occlusal carious lesion. On the basis that pain has
been intermittent, the pulpitis is probably reversible but the
rapid progression of the caries and proximity to the pulp may
herald involvement of the pulp. Caries must be excavated to
discover the true extent of the caries.
How can caries be so extensive beneath such a small
enamel cavity?
This pattern of caries is sometimes referred to as occult or
hidden caries. This presentation was much less common prior
Further investigation
The child has been cooperative for restorative care under
local analgesia in the past, so you make an appointment to
investigate and, hopefully, restore this tooth. When you
open the small occlusal cavity you discover that the underlying coronal dentine has been almost completely destroyed
by caries. Caries extends into the pulp.
Why did the child not experience the severe symptoms of
irreversible pulpitis?
There is no clear correlation between symptoms and pulpal
status or histological evidence of inflammation in mature
or immature teeth. The concept of irreversible pulpitis is a
useful one for making treatment decisions but it is only an
average reflection of symptoms. It is not unusual for teeth
to become nonvital through caries without any significant
symptoms. This is even more likely in multirooted teeth
or teeth with open apices in which the pulp has a better
blood supply.
Can the tooth be saved by root canal treatment?
Root canal treatment in immature permanent molars is
difficult and unpredictable. The canals are wider and generally
more accessible than in older patients but it is virtually
impossible to create an effective apical seal with gutta percha
in the open apices. If endodontics were necessary and the
child could cooperate for the several long sessions of
treatment required, non-setting calcium hydroxide dressings
could be placed to induce calcific barrier formation apically.
This would require changing every 46 months until an apical
barrier is felt on gentle instrumentation and a longer term
First permanent molars
filling of calcium hydroxide powder or mineral trioxide
aggregate could be placed. However, the chances of success
are reduced because of the multiple canals. The tooth would
remain compromised for future use, for instance as
orthodontic anchorage. The tooth is almost certainly better
extracted.
Compensating extractions prevent overeruption of the
opposing molar to maintain the correct occlusal level.
Balancing extractions maintain the symmetry of the arch.
How will the orthodontist decide whether to perform
compensating or balancing extractions?
The decision depends on weighing several factors:
Treatment planning
What are the effects of extraction of a first permanent
molar on the developing permanent dentition?
The spaces created close more by mesial movement of
posterior teeth than by distal movement of anterior
teeth.
There would be only a small effect on any anterior
crowding and minimal effect on the position of the
midline.
Spaces close more rapidly in the upper arch than in the
lower. Space closure in the lower arch is frequently
incomplete, unless much of the space can be occupied
by distal movement of a crowded second premolar.
Lower second molars tend to tip mesially and roll
lingually producing poor proximal contacts that are
prone to food packing and periodontitis in the long
term. Upper second molars rotate mesiopalatally as they
drift mesially, but produce much better proximal
contacts than in the lower arch.
More satisfactory space closure and proximal contacts
are produced in the lower arch if the first molar is
extracted before eruption of the second molar (see
below).
Do you require an orthodontic opinion?
Yes. If at all possible, an orthodontic opinion should be
sought prior to the extraction of any permanent tooth in a
child. In this particular case the patient may well benefit from
compensating or balancing extractions. This is a complex area
and will require an orthodontic examination to assess
crowding, the occlusion of the buccal segments, overbite and
overjet.
What are compensating and balancing extractions and
what are their benefits?
Compensating extractions are those of the opposing molar;
balancing extractions are extractions of the contralateral
tooth.
The presence of the other permanent teeth including
third molars.
The condition of the other permanent molars are
they already compromised by caries or large
restorations?
The presence of crowding in the buccal and labial
segments.
The acceptability of overbite and overjet.
Stage of dental development.
The patients likely future need and wish for orthodontic
treatment and their likely compliance.
What is the ideal age to extract first permanent molars?
Extraction must be performed at the ideal time to minimize
the adverse effects of extraction listed above. The stage of
dental development rather than the chronological age is
important. The crucial factor is the stage of development of
the lower second molar, because this determines how
satisfactorily space will close in the lower arch. The range of
acceptable development is from crown completion to
mineralization of one-third of the root. One authority quotes
the appearance of an inter-radicular crescent of bone in the
second molar as the optimal stage for first molar extraction
(at approximately 9 12 years of age). Radiography is required
to confirm the stage of development, and ensure that third
molars and second premolars are present and normal.
Does extraction of first permanent molars complicate
orthodontic treatment?
It used to be said that extraction of all four first permanent
molars doubled orthodontic treatment time and reduced the
prognosis. This saying held good only for removable
appliance treatment and does not apply to fixed appliance
treatment. However, closure of residual lower first molar
spaces does pose complex anchorage problems and it will
sometimes be preferable to delay the extraction of
compromised but symptom-free first molars until the second
permanent molars have erupted. This is a further reason why
a full orthodontic assessment is required.
Fig. 33.3 The extracted tooth.
33
CASE
157
CASE
33
158
First permanent molars
Further information
The extracted tooth is shown in Figure 33.3 What do you
see?
Part of the crown has been removed to expose the carious
cavity. On the left you can see a small periapical granuloma at
the apex of the palatal root. The pulp was therefore nonvital
despite the lack of symptoms. On the right you can see a
large defect extending from the enamel to the pulp. The
central occlusal enamel is completely unsupported but has
not fractured. The carious dentine is hardly discoloured
because it is progressing rapidly.
Você também pode gostar
- Pros Exam 1 2002Documento8 páginasPros Exam 1 2002mirfanulhaqAinda não há avaliações
- 2 Saliva PhysiologyDocumento20 páginas2 Saliva PhysiologyvelangniAinda não há avaliações
- Alveolar bone formation and structureDocumento16 páginasAlveolar bone formation and structuremirfanulhaqAinda não há avaliações
- Pros QuestionsDocumento7 páginasPros QuestionsmirfanulhaqAinda não há avaliações
- Fundamentals of SalivaDocumento15 páginasFundamentals of SalivasreedamAinda não há avaliações
- Oral InfectionsDocumento14 páginasOral InfectionsmirfanulhaqAinda não há avaliações
- Pros Exam 1 2003Documento8 páginasPros Exam 1 2003mirfanulhaqAinda não há avaliações
- Gingival InflammationDocumento19 páginasGingival InflammationmirfanulhaqAinda não há avaliações
- Comprehensive Periodontal Exam GuideDocumento40 páginasComprehensive Periodontal Exam GuideKavin SandhuAinda não há avaliações
- Management of Cracked TeethDocumento6 páginasManagement of Cracked Teethsaifuddin suhri100% (2)
- Peds Restorative PDFDocumento4 páginasPeds Restorative PDFmirfanulhaqAinda não há avaliações
- Adhesion SystemsDocumento13 páginasAdhesion SystemsTolean AndreeviciAinda não há avaliações
- Pros Exam 1 2002Documento8 páginasPros Exam 1 2002mirfanulhaqAinda não há avaliações
- Anticoagulation GuidelinesDocumento2 páginasAnticoagulation GuidelinesmirfanulhaqAinda não há avaliações
- Pulp Protection Methods and MaterialsDocumento13 páginasPulp Protection Methods and MaterialsmirfanulhaqAinda não há avaliações
- Wound Healing PDFDocumento7 páginasWound Healing PDFmirfanulhaqAinda não há avaliações
- Oral Healthcare Considerations For The Pregnant WomanDocumento4 páginasOral Healthcare Considerations For The Pregnant WomanmirfanulhaqAinda não há avaliações
- Complications in Dentoalveolar Surgery PDFDocumento37 páginasComplications in Dentoalveolar Surgery PDFmirfanulhaqAinda não há avaliações
- Making Sense of Mouth Ulceration 6Documento3 páginasMaking Sense of Mouth Ulceration 6mirfanulhaqAinda não há avaliações
- Making Sense of Mouth Ulceration 6Documento3 páginasMaking Sense of Mouth Ulceration 6mirfanulhaqAinda não há avaliações
- Guide to Fluoride TherapyDocumento4 páginasGuide to Fluoride TherapymirfanulhaqAinda não há avaliações
- Pulp 2008 HandoutDocumento7 páginasPulp 2008 HandoutNemanja MiticAinda não há avaliações
- Pulp Protection Methods and MaterialsDocumento13 páginasPulp Protection Methods and MaterialsmirfanulhaqAinda não há avaliações
- Making Sense of Mouth Ulceration 5Documento3 páginasMaking Sense of Mouth Ulceration 5mirfanulhaqAinda não há avaliações
- Making Sense of Mouth Ulceration 3Documento4 páginasMaking Sense of Mouth Ulceration 3mirfanulhaqAinda não há avaliações
- Making Sense of Mouth Ulceration 4Documento4 páginasMaking Sense of Mouth Ulceration 4mirfanulhaqAinda não há avaliações
- Scully Oral UlcersDocumento3 páginasScully Oral UlcersdeenmAinda não há avaliações
- Scully Oral UlcersDocumento3 páginasScully Oral UlcersdeenmAinda não há avaliações
- Scully Oral UlcersDocumento3 páginasScully Oral UlcersdeenmAinda não há avaliações
- Opath - Most Common ListDocumento4 páginasOpath - Most Common ListmirfanulhaqAinda não há avaliações
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Duaa Salih Makawi SonDocumento25 páginasDuaa Salih Makawi Sonnnawaz4Ainda não há avaliações
- Endodontic InsrumentDocumento52 páginasEndodontic InsrumentSawsan Z. JwaiedAinda não há avaliações
- Apexogenesis of An Immature Permanent Molar With The Use of Er, Cr:Ysgg Laser and Mineral Trioxide AggregateDocumento4 páginasApexogenesis of An Immature Permanent Molar With The Use of Er, Cr:Ysgg Laser and Mineral Trioxide AggregateEseman DentalAinda não há avaliações
- Removable Orthodontic Appliances - VijayalakshmiDocumento104 páginasRemovable Orthodontic Appliances - Vijayalakshmidrkamesh75% (8)
- Use of Chlorhexidine Varnishes in Preventing and Treating Periodontal DiseaseDocumento4 páginasUse of Chlorhexidine Varnishes in Preventing and Treating Periodontal Diseasetaher adelAinda não há avaliações
- Operative Dentistry: Restoring Primary TeethDocumento35 páginasOperative Dentistry: Restoring Primary TeethNoor AlsanouriAinda não há avaliações
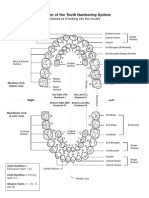
- Diagram of The Tooth Numbering SystemDocumento1 páginaDiagram of The Tooth Numbering Systemsaleh900Ainda não há avaliações
- The Daughter Test in Aesthetic or Cosmetic DentiDocumento8 páginasThe Daughter Test in Aesthetic or Cosmetic DentiRay ChaoAinda não há avaliações
- Evaluation of The Effects of The Hybrid Pendulum in Comparison With The Conventional Pendulum ApplianceDocumento8 páginasEvaluation of The Effects of The Hybrid Pendulum in Comparison With The Conventional Pendulum ApplianceARIANA AMARILES BAENAAinda não há avaliações
- Condiciones ParticularesDocumento19 páginasCondiciones ParticularesBlaise BowlyAinda não há avaliações
- Angkatan 8 Prodi PPDGS Ilmu Bedah Mulut Dan Maksilofasial Universitas Hasanuddin MakassarDocumento16 páginasAngkatan 8 Prodi PPDGS Ilmu Bedah Mulut Dan Maksilofasial Universitas Hasanuddin Makassarreyhan1Ainda não há avaliações
- Removable Prosthodontics: Louis Blatterfein S. Howard PayneDocumento6 páginasRemovable Prosthodontics: Louis Blatterfein S. Howard PayneArjun NarangAinda não há avaliações
- Cleft Lip & Palate Care GuideDocumento10 páginasCleft Lip & Palate Care GuideFarhaana ShaboodienAinda não há avaliações
- Adult Orthodontics SeminarDocumento52 páginasAdult Orthodontics Seminaravanthika krishnaraj100% (2)
- Classification of ArticulatorsDocumento4 páginasClassification of ArticulatorsRishiraj Jaiswal67% (3)
- Oral Surgery 14874Documento4 páginasOral Surgery 14874StanislavNemtanuAinda não há avaliações
- Treatment Impaksi M1 Dengan Removable Appliance PDFDocumento7 páginasTreatment Impaksi M1 Dengan Removable Appliance PDFTokubetsu VidadiAinda não há avaliações
- An Alternative Approach For The Mainframe of Flabby Ridge ©2019Documento3 páginasAn Alternative Approach For The Mainframe of Flabby Ridge ©2019DrAhmed HamzaAinda não há avaliações
- Definition: Purpose: Equipment NeededDocumento3 páginasDefinition: Purpose: Equipment NeededKim VillacorteAinda não há avaliações
- Ada & AnsiDocumento24 páginasAda & Ansikermink100% (3)
- Lec 4 Prosthodontics PDFDocumento7 páginasLec 4 Prosthodontics PDFmustafa7calligrapherAinda não há avaliações
- Ledging and Blockage of Root Canals During Canal Preparation: Causes, Recognition, Prevention, Management, and OutcomesDocumento21 páginasLedging and Blockage of Root Canals During Canal Preparation: Causes, Recognition, Prevention, Management, and Outcomesgemis96Ainda não há avaliações
- Final StomatologyDocumento49 páginasFinal StomatologyRehema MulewaAinda não há avaliações
- CROSSBITE According To GraberDocumento29 páginasCROSSBITE According To GraberAslamCv100% (1)
- New Icon 8pg BrochureDocumento8 páginasNew Icon 8pg BrochureMiruna Maria MiulescuAinda não há avaliações
- Canine Impaction Different MethodsDocumento11 páginasCanine Impaction Different MethodsMSHAinda não há avaliações
- Surgical Guides PDFDocumento8 páginasSurgical Guides PDFjagjit singhAinda não há avaliações
- Significance of Dental Anatomy, Histology, Physiology, and Occlusion (L1)Documento54 páginasSignificance of Dental Anatomy, Histology, Physiology, and Occlusion (L1)Jarrah LumpayAinda não há avaliações
- Chronic Marginal PeriodontitisDocumento21 páginasChronic Marginal PeriodontitisLaslo Mihaela Larisa100% (1)
- Parameters of Care Supplement: Parameter On "Refractory" PeriodontitisDocumento2 páginasParameters of Care Supplement: Parameter On "Refractory" PeriodontitisEllis E. RamadianAinda não há avaliações