Escolar Documentos
Profissional Documentos
Cultura Documentos
SIDS: Parental Awareness and Infant Care Practices in Contrasting Socioeconomic Areas in Cardi V
Enviado por
Dewi LarasatiDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
SIDS: Parental Awareness and Infant Care Practices in Contrasting Socioeconomic Areas in Cardi V
Enviado por
Dewi LarasatiDireitos autorais:
Formatos disponíveis
Downloaded from adc.bmj.com on December 6, 2012 - Published by group.bmj.
com
52
Archives of Disease in Childhood 1997;77:5253
SIDS: parental awareness and infant care practices
in contrasting socioeconomic areas in CardiV
A Shrivastava, P Davis, D P Davies
Abstract
Parental awareness of risk factors for sudden infant death syndrome (SIDS) and
infant care practices were compared in an
area of relative deprivation and one of
relative aZuence in CardiV. Awareness
was high in both areas. More infants slept
on the side in the deprived area (p < 0.02).
One in three babies was exposed to
cigarette smoking, significantly more in
the deprived area (p < 0.001). Health professionals should discourage side sleeping
and smoking, especially in areas of deprivation.
(Arch Dis Child 1997;77:5253)
CardiV Community
Health Care Trust,
Lansdowne Hospital,
CardiV
A Shrivastava
Department of Child
Health, University of
Wales College of
Medicine, CardiV
P Davis
D P Davies
Correspondence to:
Dr A Shrivastava,
Department of Paediatrics,
Southend Hospital,
Prittlewell Chase,
Southend-on-Sea SS0 0RY.
Accepted 18 March 1997
Keywords: SIDS; awareness; parenting practices;
socioeconomic factors
Sudden infant death syndrome (SIDS) remains a major cause of postneonatal mortality,
accounting for 29% of postneonatal deaths in
Wales.1 Recent studies, in particular the recent
Confidential Enquiry into Stillbirths and
Deaths in Infancy,2 have highlighted the link
between SIDS and socioeconomic deprivation,
and particularly the link with smoking. Reducing the residuum of deaths from SIDS is a particular challenge and will probably require new
strategies. This study aims to guide the delivery
of prevention strategies by comparing mothers
awareness of SIDS and their current infant
care practices on reducing the risk between two
contrasting socioeconomic areas of CardiV.
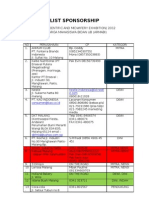
Table 1 Data on parental awareness and infant care practices of mothers in two diVerent
socioeconomic areas; results are number (%) except for social class
Mothers
Social class 3-5 (%)
Mothers awareness
Cot death awareness
Sleeping position: back/side
No smoking
Avoiding overheating
Summoning medical help
Mothers practice
Sleeping position
Back
Side
Back or side
Sleeping with parents
In parents room
In parents bed
Smoking
During pregnancy
At home
Overheating
> 3 blankets/duvets/quilts used
Room heating comfortable
Knows room temperature
Summoning medical help
Breast feeding
2 test
Deprived area
AZuent area
81 (55)
91
67 (45)
30
76 (94)
70 (86)
57 (73)
69 (85)
6 (7)
66 (98)
62 (92)
48 (72)
50 (75)
2 (3)
NS
NS
NS
NS
NS
18 (22)
42 (52)
21 (26)
33 (49)
20 (30)
14 (21)
p < 0.003
p < 0.02
NS
80 (99)
10 (12)
60 (90)
10 (15)
NS
NS
34 (42)
42 (52)
10 (15)
13 (19)
p < 0.002
p < 0.001
13 (16)
71 (88)
30 (37)
65 (80)
30 (37)
9 (13)
57 (85)
23 (34)
57 (85)
40 (60)
NS
NS
NS
NS
p < 0.02
Methods
Two district wards in the area of deprivation
were matched with four district wards in the
more aZuent area. These areas were chosen
from 1991 census data to give an approximately equal birth rate. Mothers of all babies
born in these areas between January 1996 and
March 1996 were asked to participate in the
study. Health visiting for both areas was
derived from the same team, with common
training and policies. Each mother was interviewed by her own health visitor at the first
routine postnatal visit following a standard
questionnaire. The questionnaire included
both data on the mothers awareness of SIDS
and the advice on the reduction of the SIDS
rate, and also questions on infant care practices. Socioeconomic status of individual families studied was determined by occupation of
either parent. Data were analysed using 2 tests
(table 1).
Results
One hundred and forty eight questionnaires
were completed, 81 from the more disadvantaged area (91% in social classes 35) and 67
from the more aZuent area (30% in social
classes 35). No parent refused to be interviewed.
Awareness of SIDS and of the risk reducing
measures was high in both areas, apart from the
advice on seeking medical help for symptoms
and signs of illness (in the leaflet circulated by
the Foundation for the Study of Infant Deaths
this point is phrased If you think your baby is
unwell contact your doctor). This piece of
advice was only mentioned by eight mothers.
There were important diVerences in infant
care practices. Mothers from the more deprived area were more likely to lay the baby on
its side (p < 0.02) and mothers in the more
aZuent area were more likely to lay the baby on
its back (p < 0.003). Only two infants were lain
to sleep prone, and both of these were from the
more aZuent area. Infants in the more
deprived area were more likely to be exposed to
cigarette smoke, both during and after pregnancy (p < 0.001). Twenty two infants (15%)
were lain to sleep with more than the
recommended amount of bedding, that is,
more than three blankets or a duvet or quilt,
though this did not vary between the two areas
under study. The majority of infants (140)
slept in the parents room, and 17 infants
(12%) slept in the parents bed at night. Breast
feeding was more prevalent in the more
aZuent area (p < 0.02).
Downloaded from adc.bmj.com on December 6, 2012 - Published by group.bmj.com
53
Parental awareness and infant care practices in SIDS
Discussion
Mothers were almost universally aware of
SIDS, and the vast majority were also aware of
current advice on simple measures to reduce
the risk. Recent observational studies have
focused on the risks of sleeping babies on their
sides3 and of parental smoking.4 The fact that
42% of mothers in our study slept their babies
on their sides while only one third slept their
babies exclusively on their backs suggests that
this advice needs to be reaYrmed.
Thirty per cent of mothers smoked during
pregnancy and 37% of infants were exposed to
smoke after birth. Smoking was much more
common in the deprived area. Mothers are
therefore reluctant to change their cigarette
smoking habits despite their awareness that this
is a risk factor for SIDS.4 The observation that
15% of infants are still lain to sleep with excessive bedding indicates that this piece of advice
should also be re-emphasised.5
That 14% of infants slept with their parents in
the parental bed (co-sleeping) is interesting but
diYcult to interpret, given that the families were
interviewed only once when the infant was
around 10 days old. In this district eight of the
last 23 infants dying of SIDS had been
co-sleeping with their parents at the time. It is
possible that co-sleeping is a risk factor for
SIDS6 and local advice to parents is to keep the
baby in a cot adjacent to the parent bed, avoiding co-sleeping, especially if the parents smoke
or drink alcohol. Parents are advised to pay particular attention that the bedding is not too
warm when the infant is in their bed. This advice
is contained in the local parent held record.
CONCLUSION
The variation in SIDS rates between the more
deprived and more aZuent areas of CardiV is
not adequately explained by a lack of awareness
of the reduce the risk factors. Future health
promotion strategies might more usefully be
focused on avoiding the practice of laying
babies to sleep on their sides and more specifically on practical measures to reduce smoking,
especially in the areas of deprivation. It has also
to be appreciated that the association of SIDS
with parental smoking may not be causal. The
social variables that are closely correlated with
smoking and SIDS must also be determined in
seeking to reduce the risk of SIDS even further.
We thank all the mothers for their cooperation and the health
visitors for enthusiastically filling in the questionnaires.
1 Cartlidge PHT, Stewart JH, Hopkins JM. All Wales perinatal
survey and confidential enquiry into stillbirths and deaths in
infancy. Annual Report, 1995.
2 National Advisory Body for CESDI. Annual report, 1994.
London: Department of Health, 1996.
3 Fleming PJ, Blair PS, Bacon C, et al. Environment of infants
during sleep and risk of the sudden infant death syndrome:
results of 1993-5 case-control study for confidential
inquiry into stillbirths and deaths in infancy. BMJ
1996;313:1915.
4 Blair PS, Fleming PJ, Bensley D, et al. Smoking and the
sudden infant death syndrome: results of 19935 casecontrol study for confidential inquiry into stillbirths and
deaths in infancy. BMJ 1996;313:1958.
5 Gilbert RE, Rudd PT, Berry PJ, et al. Combined eVect of
infection and heavy wrapping on the risk of sudden
unexpected infant death. Arch Dis Child 1992;67:1717.
6 Mitchell EA. Co-sleeping and sudden infant death syndrome. Lancet 1996;348:1466.
Downloaded from adc.bmj.com on December 6, 2012 - Published by group.bmj.com
SIDS: parental awareness and infant care
practices in contrasting socioeconomic areas
in Cardiff
A Shrivastava, P Davis and D P Davies
Arch Dis Child 1997 77: 52-53
doi: 10.1136/adc.77.1.52
Updated information and services can be found at:
http://adc.bmj.com/content/77/1/52.full.html
These include:
References
This article cites 4 articles, 3 of which can be accessed free at:
http://adc.bmj.com/content/77/1/52.full.html#ref-list-1
Article cited in:
http://adc.bmj.com/content/77/1/52.full.html#related-urls
Email alerting
service
Topic
Collections
Receive free email alerts when new articles cite this article. Sign up in the
box at the top right corner of the online article.
Articles on similar topics can be found in the following collections
Child health (1997 articles)
Health education (322 articles)
Health promotion (357 articles)
Smoking (103 articles)
Smoking and tobacco (103 articles)
Infant health (334 articles)
SIDS (84 articles)
Notes
To request permissions go to:
http://group.bmj.com/group/rights-licensing/permissions
To order reprints go to:
http://journals.bmj.com/cgi/reprintform
To subscribe to BMJ go to:
http://group.bmj.com/subscribe/
Você também pode gostar
- 214 Research Papers Supporting The Vaccine/Autism LinkDocumento180 páginas214 Research Papers Supporting The Vaccine/Autism LinkGinger Taylor79% (291)
- 99 Names of AllahDocumento14 páginas99 Names of Allahapi-3857534100% (9)
- Summary & Study Guide - The Gene Machine: How Genetic Technologies Are Changing the Way We Have Kids - and the Kids We HaveNo EverandSummary & Study Guide - The Gene Machine: How Genetic Technologies Are Changing the Way We Have Kids - and the Kids We HaveNota: 5 de 5 estrelas5/5 (1)
- The Terror of Pediatric MedicineDocumento360 páginasThe Terror of Pediatric MedicineNasir Khan100% (2)
- Sudden Infant Death Syndrome SidsDocumento19 páginasSudden Infant Death Syndrome Sidsapi-32844872067% (3)
- Consolidation Physical Fitness Test FormDocumento5 páginasConsolidation Physical Fitness Test Formvenus velonza100% (1)
- Chase Dimond - The Ultimate BFCM Email Marketing PlaybookDocumento92 páginasChase Dimond - The Ultimate BFCM Email Marketing Playbookgreg redAinda não há avaliações
- Crime and Punishment Vocabulary 93092Documento2 páginasCrime and Punishment Vocabulary 93092Rebeca Alfonso Alabarta50% (4)
- List SponsorshipDocumento2 páginasList SponsorshipDewi Larasati86% (7)
- Maternity and Women Health Care 10th Edition Lowdermilk Test BankDocumento10 páginasMaternity and Women Health Care 10th Edition Lowdermilk Test Bankkevincharlesfztodrpwck100% (14)
- Nursing Research PaperDocumento19 páginasNursing Research Paperapi-401771498Ainda não há avaliações
- Activity 1 Part 1 2Documento2 páginasActivity 1 Part 1 2api-457299309Ainda não há avaliações
- Sudden Infant Death SyndromeDocumento5 páginasSudden Infant Death SyndromeAndrewloquitoAinda não há avaliações
- Infant Mortality Rates PaperDocumento7 páginasInfant Mortality Rates PaperLauren HutsonAinda não há avaliações
- NURS4060 - AshleyVigne - Assessment 4 - Attempt1Documento7 páginasNURS4060 - AshleyVigne - Assessment 4 - Attempt1ashleyAinda não há avaliações
- Vaccinations Are Your Friends Not Your EnemiesDocumento9 páginasVaccinations Are Your Friends Not Your Enemiesapi-316237120Ainda não há avaliações
- Jurnal Buk Okta 4 EngDocumento17 páginasJurnal Buk Okta 4 EngRosy OktaridaAinda não há avaliações
- Sids BabyDocumento7 páginasSids Babyreski ulpayaniAinda não há avaliações
- Content ServerDocumento18 páginasContent ServerMelindaDuciagAinda não há avaliações
- Depression Among CD and VDDocumento7 páginasDepression Among CD and VDnoam tiroshAinda não há avaliações
- Essay 3Documento7 páginasEssay 3Adrian FiforAinda não há avaliações
- Running Head: Factors Influencing Vaccine Hesitancy 1Documento18 páginasRunning Head: Factors Influencing Vaccine Hesitancy 1api-395650878Ainda não há avaliações
- Smoking and CHDDocumento19 páginasSmoking and CHDAnonymous NeRC5JYiSAinda não há avaliações
- Questions and Answers For Health Care Providers: Sudden Infant Death Syndrome (SIDS) and Other Sleep-RelatedDocumento35 páginasQuestions and Answers For Health Care Providers: Sudden Infant Death Syndrome (SIDS) and Other Sleep-Relatednur'aina suryaAinda não há avaliações
- NIH Public Access: Author ManuscriptDocumento20 páginasNIH Public Access: Author ManuscriptWestiAinda não há avaliações
- Jessica Kreck Neonatal Abstinence Syndrome Germanna Community CollegeDocumento9 páginasJessica Kreck Neonatal Abstinence Syndrome Germanna Community Collegeapi-506562771Ainda não há avaliações
- 157 Research Papers Supporting The Vaccine Autism LinkDocumento123 páginas157 Research Papers Supporting The Vaccine Autism Linkdon fabAinda não há avaliações
- Nursing Research PaperDocumento24 páginasNursing Research Paperapi-455624162Ainda não há avaliações
- Childhood Obesity and Parental Smoking As Risk Factors For Childhood ADHD in Liverpool ChildrenDocumento8 páginasChildhood Obesity and Parental Smoking As Risk Factors For Childhood ADHD in Liverpool ChildrenFabricio CardosoAinda não há avaliações
- 64076-Article Text-124903-1-10-20110303Documento4 páginas64076-Article Text-124903-1-10-20110303Maricris EspinaAinda não há avaliações
- 2019 Research Proposal Palliative Needs - YOGYA - Alexandra Pangarso 020519Documento26 páginas2019 Research Proposal Palliative Needs - YOGYA - Alexandra Pangarso 020519atikahanifahAinda não há avaliações
- Antiseizure Medication Use During Pregnancy and Risk of ASD and ADHD in ChildrenDocumento10 páginasAntiseizure Medication Use During Pregnancy and Risk of ASD and ADHD in Childrenmhegan07Ainda não há avaliações
- Open Letter To AASDDocumento4 páginasOpen Letter To AASDWBAYAinda não há avaliações
- ENG 110 Argumentative EssayDocumento4 páginasENG 110 Argumentative EssayTammy Marie Amos0% (2)
- Sobrecarga CuidadoresDocumento6 páginasSobrecarga CuidadoresMARIA FRANCISCA VERGARA AGUILARAinda não há avaliações
- 2019.04.AntenatalNeoNatalPostnatal Practitioners Guide KPDocumento24 páginas2019.04.AntenatalNeoNatalPostnatal Practitioners Guide KPISABELLA PETRIEAinda não há avaliações
- Vaccination Hesitancy: Presented byDocumento21 páginasVaccination Hesitancy: Presented byZiad ZfAinda não há avaliações
- Thesis Statement On Autism and VaccinesDocumento7 páginasThesis Statement On Autism and VaccinesPaperHelperUK100% (2)
- Pre-Hospital Management of Febrile Seizures in Children Seen at The University College Hospital, Ibadan, Nigeria Feature ArticleDocumento5 páginasPre-Hospital Management of Febrile Seizures in Children Seen at The University College Hospital, Ibadan, Nigeria Feature Articlechaz5727xAinda não há avaliações
- FX RX Perinatales TGDDocumento10 páginasFX RX Perinatales TGDopi1966Ainda não há avaliações
- Preventing Chronic Disease: Prevalence of and Risk Factors For Adolescent Obesity in Southern Appalachia, 2012Documento6 páginasPreventing Chronic Disease: Prevalence of and Risk Factors For Adolescent Obesity in Southern Appalachia, 2012Makmur SejatiAinda não há avaliações
- Familial, Social and Environmental Risk Factors in Autism: A Case-Control StudyDocumento5 páginasFamilial, Social and Environmental Risk Factors in Autism: A Case-Control StudyFarhadAinda não há avaliações
- Yes Depression Is Nature or NatureDocumento2 páginasYes Depression Is Nature or NatureAnonymousPlatypusAinda não há avaliações
- Babies Are Still Dying of SIDS.26Documento6 páginasBabies Are Still Dying of SIDS.26heartbcglAinda não há avaliações
- Edited Peds-Neonates Research Paper Sids Research Class - FinalDocumento6 páginasEdited Peds-Neonates Research Paper Sids Research Class - Finalapi-733590799Ainda não há avaliações
- Exploring Women Knowledge of Newborn Danger Signs: A Case of Mothers With Under Five ChildrenDocumento8 páginasExploring Women Knowledge of Newborn Danger Signs: A Case of Mothers With Under Five ChildrenJohnjohn MateoAinda não há avaliações
- Identify Etiology of Morbidity Events of Earlier Children Among Multigravida Women.Documento11 páginasIdentify Etiology of Morbidity Events of Earlier Children Among Multigravida Women.snehal DharmadhikariAinda não há avaliações
- SIDSDocumento13 páginasSIDSrevwilliec6490Ainda não há avaliações
- 2015 JainDocumento7 páginas2015 JainkendyAinda não há avaliações
- Wright2016 PDFDocumento28 páginasWright2016 PDFMarco Alejandro RojasAinda não há avaliações
- SD Down - Pediatrics 2001Documento10 páginasSD Down - Pediatrics 2001Carolina BeovideAinda não há avaliações
- Pedpallcare ResidentsoverviewDocumento54 páginasPedpallcare ResidentsoverviewSvitlana YastremskaAinda não há avaliações
- Sudden: Infant Death SyndromeDocumento8 páginasSudden: Infant Death SyndromeBunga RamadhaniAinda não há avaliações
- Parental Delay or Refusal of Vaccine Doses, Childhood Vaccination Coverage at 24 Months of Age, and The Health Belief ModelDocumento12 páginasParental Delay or Refusal of Vaccine Doses, Childhood Vaccination Coverage at 24 Months of Age, and The Health Belief ModelariAinda não há avaliações
- Autism RiskDocumento14 páginasAutism RiskAlina Topor Psi-MedicalAinda não há avaliações
- Pathways Between Risk and Protective Factors and Maternal Postnatal Depressive SymptomsDocumento16 páginasPathways Between Risk and Protective Factors and Maternal Postnatal Depressive SymptomsAmáta JakusAinda não há avaliações
- AAP Committee On Nutrition-Pediatrics. 2003 112Documento9 páginasAAP Committee On Nutrition-Pediatrics. 2003 112Rang PasamanAinda não há avaliações
- Pregnancy and ParenthoodDocumento16 páginasPregnancy and ParenthoodJuliana Rossi RosinhaAinda não há avaliações
- Medical Management of Children With Down SyndromeDocumento8 páginasMedical Management of Children With Down SyndromeMariana OrozcoAinda não há avaliações
- Literature Review On Sudden Infant Death SyndromeDocumento8 páginasLiterature Review On Sudden Infant Death Syndromenynodok1pup3Ainda não há avaliações
- Open Letter To NJSDDocumento4 páginasOpen Letter To NJSDWBAYAinda não há avaliações
- Jurnal ReproDocumento6 páginasJurnal ReproSiti AliyahAinda não há avaliações
- Manajemen Failure To ThriveDocumento5 páginasManajemen Failure To ThriveIndri WahyuniAinda não há avaliações
- Vaccines EssayDocumento12 páginasVaccines Essayapi-233200175Ainda não há avaliações
- The Preemie Parents' Companion: The Essential Guide to Caring for Your Premature Baby in the Hospital, at Home, and Through the First YearsNo EverandThe Preemie Parents' Companion: The Essential Guide to Caring for Your Premature Baby in the Hospital, at Home, and Through the First YearsAinda não há avaliações
- Baby-Friendly Hospital Initiative: Implementation GuidanceDocumento64 páginasBaby-Friendly Hospital Initiative: Implementation GuidanceDewi LarasatiAinda não há avaliações
- The Effect of Rooming-In Care On The Emotional Stability of Newborn InfantsDocumento5 páginasThe Effect of Rooming-In Care On The Emotional Stability of Newborn InfantsDewi LarasatiAinda não há avaliações
- Mi2018 2845352 PDFDocumento5 páginasMi2018 2845352 PDFDewi LarasatiAinda não há avaliações
- 2018 Initial Certification Fee ScheduleDocumento3 páginas2018 Initial Certification Fee ScheduleDewi LarasatiAinda não há avaliações
- Denver II Test Form PDFDocumento2 páginasDenver II Test Form PDFDewi LarasatiAinda não há avaliações
- Pathway 3 Plan GuideDocumento10 páginasPathway 3 Plan GuideDewi LarasatiAinda não há avaliações
- "Every Mother Is Able To Breast Feed": Breast Milk Contains All Nutrients Needed For Baby's Growth and DevelopmentDocumento4 páginas"Every Mother Is Able To Breast Feed": Breast Milk Contains All Nutrients Needed For Baby's Growth and DevelopmentDewi LarasatiAinda não há avaliações
- Puberty and Tanner StagesDocumento2 páginasPuberty and Tanner StagesDewi LarasatiAinda não há avaliações
- General Terms Conditions For Sales Purchases LPG and Chemical TankersDocumento34 páginasGeneral Terms Conditions For Sales Purchases LPG and Chemical TankersSally AhmedAinda não há avaliações
- 2 Quiz of mgt111 of bc090400798: Question # 1 of 20 Total Marks: 1Documento14 páginas2 Quiz of mgt111 of bc090400798: Question # 1 of 20 Total Marks: 1Muhammad ZeeshanAinda não há avaliações
- 10.4324 9781003172246 PreviewpdfDocumento76 páginas10.4324 9781003172246 Previewpdfnenelindelwa274Ainda não há avaliações
- Adobe Scan 03-May-2021Documento22 páginasAdobe Scan 03-May-2021Mohit RanaAinda não há avaliações
- Script PDFDocumento1 páginaScript PDFWahid KhanAinda não há avaliações
- Chapter 1 Introduction To Quranic Studies PDFDocumento19 páginasChapter 1 Introduction To Quranic Studies PDFtaha zafar100% (3)
- Lean Supply Chains: Chapter FourteenDocumento29 páginasLean Supply Chains: Chapter FourteenKshitij SharmaAinda não há avaliações
- Gujarat Technological UniversityDocumento5 páginasGujarat Technological Universityvenkat naiduAinda não há avaliações
- Census 2011 PDFDocumento2 páginasCensus 2011 PDFvishaliAinda não há avaliações
- Financial Report: The Coca Cola Company: Ews/2021-10-27 - Coca - Cola - Reports - Continued - Momentum - and - Strong - 1040 PDFDocumento3 páginasFinancial Report: The Coca Cola Company: Ews/2021-10-27 - Coca - Cola - Reports - Continued - Momentum - and - Strong - 1040 PDFDominic MuliAinda não há avaliações
- GHMC Results, 2009Documento149 páginasGHMC Results, 2009UrsTruly kotiAinda não há avaliações
- Remote Lab 1013Documento3 páginasRemote Lab 1013cloud scapeAinda não há avaliações
- EnglishDocumento3 páginasEnglishYuyeen Farhanah100% (1)
- Elaine Makes Delicious Cupcakes That She Mails To Customers AcrossDocumento1 páginaElaine Makes Delicious Cupcakes That She Mails To Customers Acrosstrilocksp SinghAinda não há avaliações
- Shop Decjuba White DressDocumento1 páginaShop Decjuba White DresslovelyAinda não há avaliações
- Module Letter 1Documento2 páginasModule Letter 1eeroleAinda não há avaliações
- Pentesting ReportDocumento14 páginasPentesting Reportazeryouness6787Ainda não há avaliações
- The Call For The Unity of Religions (Wahdatul Adyaan) A False and Dangerous Call. - An Elimination of The Truth by DR - Saleh As-SalehDocumento52 páginasThe Call For The Unity of Religions (Wahdatul Adyaan) A False and Dangerous Call. - An Elimination of The Truth by DR - Saleh As-SalehMountainofknowledge100% (1)
- 4-Cortina-Conill - 2016-Ethics of VulnerabilityDocumento21 páginas4-Cortina-Conill - 2016-Ethics of VulnerabilityJuan ApcarianAinda não há avaliações
- Coursework Assignment: Graduate Job ImpactDocumento13 páginasCoursework Assignment: Graduate Job ImpactmirwaisAinda não há avaliações
- Philippine Literature During Spanish ColonizationDocumento4 páginasPhilippine Literature During Spanish ColonizationCharisel Jeanne CasalaAinda não há avaliações
- How To Claim Your VAT RefundDocumento5 páginasHow To Claim Your VAT Refundariffstudio100% (1)
- Correctional Case StudyDocumento36 páginasCorrectional Case StudyRaachel Anne CastroAinda não há avaliações
- The History of Land Use and Development in BahrainDocumento345 páginasThe History of Land Use and Development in BahrainSogkarimiAinda não há avaliações
- Budo Hard Style WushuDocumento29 páginasBudo Hard Style Wushusabaraceifador0% (1)
- Vivekananda Institute of ManagementDocumento8 páginasVivekananda Institute of ManagementShubham YadavAinda não há avaliações