Escolar Documentos
Profissional Documentos
Cultura Documentos
Renal Clinical
Enviado por
vinDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Renal Clinical
Enviado por
vinDireitos autorais:
Formatos disponíveis
Clinical
Resource: Ghosh, Mayo Clinic Internal Medicine Board Review 2008, 8th
Edition, Lippincott, Williams & Wilkins. Part I Nephrology (pages 614-625)
Glomerular Disease Clinical Presentation
1.
Contrast microalbuminuria and overt proteinuria.
Microalbuminuria - Urinary albumin excretion of 30-300
mg/1.73 m2 per 24 hrs
Over proteinuria - Urinary albumin > 300 mg/1.73 m2 per
24 hrs
Even minimal proteinuria is associated w/
cardiovascular risk; no such thing as normoalbuminuria
1.
1.
1.
Define the nephrotic syndrome.
Urinary protein > 3.5 g/1.73 m2 per 24 hours,
hypoalbuminemia (<3.0 g/dL), peripheral edema,
hypercholesteremia, and lipiduria
Describe the laboratory and physical findings associated with
the nephrotic syndrome.
Edema can be prominent
Urinalysis: waxy casts, free fat, oval fat bodies, lipiduria
(Maltese crosses)
Complications:
hypogammaglobulinemia (inc risk of infections, e.g.
cellulitis, spontaneous peritonitis)
Vit D deficiency (d/t loss of Vit D-binding protein)
iron deficiency anemia (d/t hypotransferrinemia)
Name the thrombotic complication of nephrotic syndrome.
Thrombotic complications d/t increased levels of
prothrombotic factors and decreased antithrombin III and
antiplasmin
renal vein thrombosis
1.
Describe the urinary findings in nephritic syndrome.
Urinary protein < 3.5 g/1.73 m2 per 24 hours,
hypoalbuminemia (<3.0 g/dL), peripheral edema,
hypercholesteremia, and lipiduria
Oliguria, edema, HTN, proteinuria ( usually < 3.5 g/1.73
2
m per 24 hours), and an active urinary sediment
Glomerular Disease that Presents with Nephritic Syndrome
Discuss the causes, glomerular changes, microscopic findings and lab findings,
of post streptococcal glomerulonephritis.
o
Cause- acute glomerulonephritis nephritis that develops 1-4 weeks
after pharyngitis or skin infection w/ (nephritogenic) strains of group A hemolytic streptococci
o
Presentation is the abrupt onset of nephritic syndrome
Active urinary sediment (dysmorphic RBCs or RBC casts or both)
is present in all cases.
Urine has a cola or smokey appearance; due to
methemoglobin formation
Oliguria, HTN, edema, and proteinuria (<3 g/1.73 m 2 per 24 hrs)
o
Lab findings: cultures are negative, but titers for antistreptolysin (ASO),
antistreptokinase, antihyaluronidase, and antideoxyribonuclease (antiDNAse B) may provide evidence of recent streptococcal infection
Total hemolytic complement (CH50) and C3 levels are usually
decreased; but C4 levels are normal
Immunofluoresence: granular deposition of IgG and C3 in a
starry-sky, meseangial, or garland pattern
o
Microscopic findings: diffuse hypercellularity of the glomerular tufts, w/
mesangial and endothelial cell proliferation, infiltration of PMNs
(exudative), and subepithelial humps w/ silver stain
o
Pathologic characteristic: presence of large humps, which are domeshaped subepithelial deposits in the glomerular basement membrane
(GBM)
1 Discuss the clinical presentation of IgA nephropathy.
o
Mesangial proliferative glomerulonephritis; diffuse deposition of IgA in
the mesangium
o
Typical presentation: episodic macroscopic hematuria (usually
accompanying an intercurrent upper respiratory tract infection
[synpharyngitic]), often w/ RBC casts, but most commonly w/
asymptomatic microscopic hematuria and proteinuria
o
Pathogenesis is linked to abnormal integrity of the intestinal mucosa
resulting in overexposure to ubiquitous environmental antigens
exaggerated production of galactose-deficient (GD)-IgA1 by B cells
1 Discuss the light microscopy findings and the immunofluorescence findings of
IgA nephropathy.
o
Microscope- glomeruli may look normal or may show mesangial
expansion
o
Immunoflourescence is diagnostic and demonstrates strong IgA
staining w/in the mesangium
1 Describe the presentation of Henock-Schonlein purpura.
o
Systemic form of IgAN; microscopic or gross hematuria (or both) along
with RBC casts, purpura, and abdominal pain
1 Discuss the presentation, lab findings, and causes of membranoproliferative
glomerulonephritis.
o
Diffuse proliferation of the mesangium and thickening of glomerular
capillary walls, as seen w/ light microscopy
MPGN Type I- affects mainly kids (8-16 y/o); main cause is
cryoglobulinemia in a pt w/ hep C virus infection.
MPGN Type II- rare disease found in adults; associated w/ partial
lipodystrophy and drusen bodies in the retina (macular degeneration)
o
Presentation
1/3 of pts present w/ asymptomatic hematuria and proteinuria
Another 1/3rd have nephrotic syndrome and preserved renal
function
10-20% of pts present w/ nephritic syndrome
HTN is very common
o
Lab Findings
MPGN type I and cryoglobulinemic MPGN the levels of C3 & 4,
and CH50 are persistently low, due to activation of both complement
pathways
MPGN type II the alternative pathway is active therefore they
have persistently low C3 levels but normal C4.
A C3 nephritic factor is typically present; autoantibody to
alternating pathway C3 convertase persistent C3 breakdown
Renal biopsy: diffuse global thickening of capillary walls and
endocapillary hypercellularity lobular appearance
Silver staining: tram-track or double contour appearance due
to the interposition of mesangium btwn the GBM and endothelium
resulting in a neomembrane deposition and development of
glomerular capillaries
Immunofluorescence shows granular deposition of IgG and C3 in
the mesangium and outlines the lobular contours
1 Discuss the treatment of membranoproliferative glomerulonephritis.
o
MPGN type I
Long-term: corticosteroids
Temporary relief (slows progression): dipyridamole and aspirin
o
MPGN type II - Tx in adults is unknown
Rapidly Progressive Glomerulonephritis Crescentic
Glomerulonephritis
Define RPGN.
o
Acute, rapidly progressive (days to weeks to months) deterioration of
renal function associated with active urinary sediment and a focal
necrotizing crescenteric glomerulonephritis seen on light microscopic
examination of renal biopsy specimens
Describe Wegeners Granulomatosis.
Granulomatous inflammation involving the respiratory tract and
necrotizing vasculitis affecting small and medium-size vessels; a
necrotizing glomerulonephritis is common
Describe Polyarteritis Nodosa vasculitis.
o
Presentation: necrotizing inflammation of medium-size or small arteries
w/o glomerulonephritis or vasculitis in capillaries, or venules.
o
ANCA-negative; in some pts the disease is associated w/ hepatitis B
virus infection; normal glomeruli
Describe the other major organ system involved with Goodpasture Disease and
describe the mechanism of renal impairment.
o
Pulmonary-renal syndrome caused by circulating anti-GBM Abs and
linear staining seen along the GBM and alveolar basement membrane on
immunofluorescence
Ab is directed against the 3 chain of type IV collagen
Glomerular Disease That Usually Presents as Nephrotic Syndrome
Discuss the usual presentation of minimal change nephropathy.
o
Absence of structural glomerular abnormalities, except for the
widespread fusion of epithelial cell foot process seen on electron
microscopy, in a pt w/ nephrotic syndrome
Most common cause of nephrotic syndrome in kids (<10 y/o)
o
Kids present with an abrupt onset of nephrotic syndrome
The presence of nephrotic syndrome in a pt w/ normal urinalysis
results indicates MCN
o
In Adults, HTN and renal insufficiency may be present
1 Discuss the causes, of minimal change nephropathy.
o
Pathogenesis is unknown
o
Association w/ Hodgkin lymphoma suggests that MCN may be of Tlymphocyte abnormalities, w/ t cell producing a lymphokine that is toxic to
glomerular epithelial cells
Results in fusion of foot processes and detachment of podocytes,
loss of heparin sulfate negative-charge barrier of the basement
membrane and increased glomerular permeability to protein.
o
Clear association w/ drugs, allergy, and malignancy (lymphoma and
thymoma)
o
Secondary causes
Viral- MONO and HIV
Drugs- NSAIDs
Tumors- Hodgkin lymphoma, mycosis fungoides, and thymoma
Allergies- food, immunization, bee sting, and poison ivy
1 Discuss the treatment of minimal change nephropathy.
o
Responds to corticosteroid tx (cornerstone therapy)
Given for 4-8 wks after remission
Alt tx:cyclophosphamide, chlorambucil, and cyclosporine
1 Discuss the clinical features of membranous nephropathy.
o
Leading cause of nephrotic syndrome in white adults; rare in kids
o
Pathogenic cause is not known
Causes immune complex localization and the subsequent
development of proteinuria and nephrotic syndrome
Presence of autoantibodies to the M-type phospholipase A 2
receptor
o
Present w/ Proteinuria > 2.0 g/1.73 m2 per 24 hrs
o
Initially, renal function is preserved in the majority of patients and
glomeruli may appear normal under the light microscope
Advanced disease- capillary walls are thickened and there are
subepithelial projections (spikes) along the capillary walls
o
Spontaneous complete remission occurs in 25% of pts and partial
remission in 50%
Spontaneous remission is rare in pts w/ proteinuria >10 g/1.73
2
m per 24 hours
1 Discuss the causes of membranous nephropathy (primary vs. secondary).
o
Primary- in the majority of cases, the etiologic agent is unknown and
the disorder is termed idiopathic nephrotic syndrome
o
Secondary- associated w/ autoimmune diseases (ex: SLE), infections
(ex: Hep B and C), medications (ex: NSAIDs, penicillamine, gold), and
neoplasia (ex: colon and lung cancer)
o
Both types have similar presentation
1 Briefly list major medication classes that can cause membranous nephropathy.
o
NSAIDs and Penicillamine
1 Discuss treatment of membranous nephropathy.
o
Initial therapy is directed to control of edema, HTN, hyperlipidemia,
and reduction of proteinuria via ACEs and ARBs
o
Immunosuppressive therapy for pts who remain nephrotic after a trial
of maximal Angiotensin II Blockade (6 months)
Combo use of corticosteroids and cytotoxic agents, cyclosporine,
or tacrolimus
o
Pathoma: Poor response to steroids; progresses to renal failure
Other Glomerular Disorders
Name the most common cause of End Stage Renal Disease (ESRD) in
the United States.
diabetic nephropathy.
Name the early manifestation of renal disease associated with diabetic
nephropathy.
The first manifestation of diabetic nephropathy is microalbuminuria (20200mcg/min or 30-300mg/1.73m^2 per 24 hours). This is important because it
is a good primary predictor of renal disease. Over time, microalbuminuria can
evolve to proteinuria (>300mg/1.73m^2 per 24 hours) and then full-blown
nephrotic syndrome.
Name the lesion on renal biopsy pathognomonic for diabetic
nephropathy.
Renal biopsies will show different things depending on the stage of the
disease (You only need to know what is in red, everything else is background
info):
Earliest stage: Glomerular hypertrophy and thickening of the glomerular base
membrane.
As it progresses: Arteriolar hyalinosis and arteriosclerosis.
Then: Progressive mesangial expansion (diffuse diabetic glomerulosclerosis)
and nodular formation (Kimmelstiel-Wilson nodules, which are pathognomic for
diabetic nephropathy). Capsular drop lesions and fibrin cap lesions are also
pathognomic findings.
Late: Tubular atrophy and interstitial fibrosis.
Name two factors/interventions that can slow the rate of progression
of diabetic nephropathy.
The progression of diabetic nephropathy can be slowed down with tight
glycemic control (glycated hemoglobin <7.0%) and the use of ACEI or ARBs (to
keep systolic BP <125mmHg).
Discuss the role of ACE inhibitors and/or Angiotensin Receptor
Blockers in the diabetic patient.
They keep systolic BP under 125mmHg. If the patient with diabetes develops
microalbuminuria, they should start ACEIs or ARBs even if they have normal BP
(remember, microalbuminuria is an indicator of renal disease).
In what circumstances is renal biopsy necessary regarding the patient
with diabetic nephropathy?
Renal biopsy is indicated for patients with an atypical course of the disease
(eg. Nephrotic-range proteinuria within the first 10 years in type 1 diabetes or if
loss of renal function is rapidly progressive.
Renal biopsies are not necessary for patients with long-term diabetes,
especially if retinopathy is present.
Describe the immune deposit location in SLE nephritis.
Immune deposits (in the case of SLE nephritis, its IgG, IgM, IgA, C1q, and C4)
are localized to the glomerular capillary subendothelium (wire-loop).
*Not part of this objective but also seen under electron microscopy are
tubuloreticular inclusions which are characteristic but not diagnostic of SLE
nephritis.
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- High Yield Surgery Compatible Version PDFDocumento77 páginasHigh Yield Surgery Compatible Version PDFDuke71% (7)
- ATLS Chapter Review QuestionsDocumento36 páginasATLS Chapter Review QuestionsKen Evans89% (57)
- Surgical Notes A Pocket Survival GuideDocumento197 páginasSurgical Notes A Pocket Survival Guidevin100% (12)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Drug CardsDocumento16 páginasDrug Cardsp_dawg100% (7)
- AnatomyDocumento4 páginasAnatomyvinAinda não há avaliações
- Type I HSDocumento3 páginasType I HSvinAinda não há avaliações
- High Yield Internal Medicine Compatible VersionDocumento100 páginasHigh Yield Internal Medicine Compatible VersionAhsan X Baig100% (5)
- Uw2 Ome: Online Meded Su2M: Mim BB HimDocumento1 páginaUw2 Ome: Online Meded Su2M: Mim BB HimvinAinda não há avaliações
- Sample Step 1 ScheduleDocumento2 páginasSample Step 1 ScheduleAmparo Cortes IllanesAinda não há avaliações
- AscitesDocumento3 páginasAscitesvinAinda não há avaliações
- High Yield EmbryologyDocumento14 páginasHigh Yield EmbryologyvinAinda não há avaliações
- Geriatrics Article On NutritionDocumento10 páginasGeriatrics Article On NutritionvinAinda não há avaliações
- TirukuralDocumento623 páginasTirukuralvin100% (2)
- Renal 1 - Anatomy, Em, HistoDocumento24 páginasRenal 1 - Anatomy, Em, HistovinAinda não há avaliações
- Feature Hepatitis A Hepatitis B Hepatitis C: Common Name Virus Structure Transmission Onset Incubation Period (Days)Documento2 páginasFeature Hepatitis A Hepatitis B Hepatitis C: Common Name Virus Structure Transmission Onset Incubation Period (Days)vinAinda não há avaliações
- CardiologyDocumento32 páginasCardiologyvinAinda não há avaliações
- Cardiac TransplantDocumento27 páginasCardiac TransplantvinAinda não há avaliações
- Hodgkins ChartsDocumento3 páginasHodgkins ChartsvinAinda não há avaliações
- Heart Sounds OutlineDocumento31 páginasHeart Sounds OutlinevinAinda não há avaliações
- OMT ReviewDocumento114 páginasOMT Reviewvin100% (2)
- Lung Cancer Translational and Emerging Therapies by Kishan J. PandyaDocumento276 páginasLung Cancer Translational and Emerging Therapies by Kishan J. PandyaADEEL ARSALANAinda não há avaliações
- Drug-Induced Acute-onChronic Liver FailureDocumento18 páginasDrug-Induced Acute-onChronic Liver FailureVerónica Bello HorizonteAinda não há avaliações
- Conversion Disorder BrochureDocumento2 páginasConversion Disorder BrochurerobktfAinda não há avaliações
- Overuse Injuries: Table 1. Common Causes of Acute and Overuse InjuriesDocumento7 páginasOveruse Injuries: Table 1. Common Causes of Acute and Overuse InjuriesJonah TongcoAinda não há avaliações
- Adrenal CrisisDocumento6 páginasAdrenal CrisisSteven SetioAinda não há avaliações
- Introduction To Special Education: Taylor-White Elementary SchoolDocumento23 páginasIntroduction To Special Education: Taylor-White Elementary SchoolEric D. ValleAinda não há avaliações
- Respiratory Syncytial Virus in LowerDocumento6 páginasRespiratory Syncytial Virus in LowerShailendra ParajuliAinda não há avaliações
- Video Conten - 2017 - Blumgart S Surgery of The Liver Biliary Tract and PancreaDocumento1 páginaVideo Conten - 2017 - Blumgart S Surgery of The Liver Biliary Tract and PancreaJoe JoeAinda não há avaliações
- Gangguan Elminasi Pada Ibu HamilDocumento10 páginasGangguan Elminasi Pada Ibu HamilRismawatiAinda não há avaliações
- Level 10 Quiz V2 - RevisedDocumento4 páginasLevel 10 Quiz V2 - RevisedGordon B.J.Ainda não há avaliações
- Dr. Dian Kusumaningrum - PRESENTASI JCCA-ANTIBIOTIC DOSING IN CRITICALLY ILLDocumento31 páginasDr. Dian Kusumaningrum - PRESENTASI JCCA-ANTIBIOTIC DOSING IN CRITICALLY ILLRestu TriwulandaniAinda não há avaliações
- Merged TDL Files 20210111112759Documento2 páginasMerged TDL Files 20210111112759api-545768247Ainda não há avaliações
- HIV AIDS NCLEX Questions Nursing Review QuizDocumento10 páginasHIV AIDS NCLEX Questions Nursing Review QuizShella Mae UsquisaAinda não há avaliações
- Cardiac Rehabilitation and Exercise Therapy in Pediatric and Adult PatientsDocumento24 páginasCardiac Rehabilitation and Exercise Therapy in Pediatric and Adult PatientsebookAinda não há avaliações
- Erythema Nodosum Associated With Terbinafine Therapy A Case ReportDocumento5 páginasErythema Nodosum Associated With Terbinafine Therapy A Case ReportAthenaeum Scientific PublishersAinda não há avaliações
- Sample NCLEX-RN Quiz:: Safe and Effective Care EnvironmentDocumento2 páginasSample NCLEX-RN Quiz:: Safe and Effective Care EnvironmentSneha PatelAinda não há avaliações
- CBC Reference Value TableDocumento2 páginasCBC Reference Value Tabletommy areanAinda não há avaliações
- COVID-19 IDS 2nd 2020Documento185 páginasCOVID-19 IDS 2nd 2020Morita TakaAinda não há avaliações
- Per-Pl 206Documento266 páginasPer-Pl 206Wan YusufAinda não há avaliações
- CASE-STUDY-DM AmputationDocumento32 páginasCASE-STUDY-DM AmputationJerushamae Castillo0% (1)
- Bluebook PDFDocumento39 páginasBluebook PDFDumitrache MihaelaAinda não há avaliações
- Vats Bullectomy: Initial Shillong ExperienceDocumento21 páginasVats Bullectomy: Initial Shillong ExperiencelmdarlongAinda não há avaliações
- Amikinhal TrialDocumento11 páginasAmikinhal TrialBreno Bertozo SilvaAinda não há avaliações
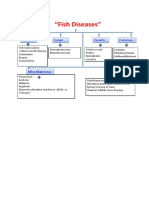
- 202004061939435276sptrivedi Fish DiseasesDocumento19 páginas202004061939435276sptrivedi Fish DiseasesSaravanan arnoldAinda não há avaliações
- GoodPractice WL U02PresentingComplaint PDFDocumento4 páginasGoodPractice WL U02PresentingComplaint PDFFlorina TrutescuAinda não há avaliações
- CortisolDocumento2 páginasCortisolkitu_alagappan4720Ainda não há avaliações
- EntDocumento3 páginasEntmerna hazazahAinda não há avaliações
- Brad Blanton - Radical HonestyDocumento10 páginasBrad Blanton - Radical HonestyraduAinda não há avaliações