Escolar Documentos
Profissional Documentos
Cultura Documentos
Complications of Chronic Use of Skin Lightening Cosmetics PDF
Enviado por
Ichsan IrwantoDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Complications of Chronic Use of Skin Lightening Cosmetics PDF
Enviado por
Ichsan IrwantoDireitos autorais:
Formatos disponíveis
Report
Oxford, UK
International
IJD
Blackwell
0011-9059
XXX
Publishing
Journal Ltd,
Ltd
of Dermatology
2007
Complications of chronic use of skin lightening cosmetics
Complications
Olumide
Case
report
et al. of skin lightening cosmetics
Yetunde M. Olumide, MD, Ayesha O. Akinkugbe, MD, Dan Altraide, MD, Tahir Mohammed,
MD, Ngozi Ahamefule, MD, Shola Ayanlowo, MD, Chinwe Onyekonwu, MD,
and Nyomudim Essen, MD
From the Dermatology Unit, epartment of
Medicine, College of Medicine, Lagos, Nigeria
Correspondence
Y. Mercy Olumide
Department of Medicine
College of Medicine of the University of Lagos
P M B 12003, Lagos, Nigeria
E-mail: mercyolumide2004@yahoo.co.uk
Abstract
Skin lightening (bleaching) cosmetics and toiletries are widely used in most African countries.
The active ingredients in these cosmetic products are hydroquinone, mercury and
corticosteroids. Several additives (conconctions) are used to enhance the bleaching effect.
Since these products are used for long duration, on a large body surface area, and under hot
humid conditions, percutaneous absorption is enhanced. The complications of these products
are very serious and are sometimes fatal. Some of these complications are exogenous
ochronosis, impaired wound healing and wound dehiscence, the fish odor syndrome,
nephropathy, steroid addiction syndrome, predisposition to infections, a broad spectrum of
cutaneous and endocrinologic complications of corticosteroids, including suppression of
hypothalamic-pituitary-adrenal axis. In this era of easy travels and migration, African patients
with these complications can present to physicians anywhere in the world. It is therefore critical
for every practicing physician to be aware of these complications.
A middle-aged Nigerian lady was recently brought home to
die from a Western European country because she developed an
uncontrollable diabetes mellitus and evidence of hypothalamicpituitary-adrenal axis suppression. On clinical examination,
the lady had dense stigmatas of chronic use of skin lightening
creams, which was confirmed through history. Majority of
medical practitioners outside subsaharan Africa may not be
familiar with this habit of bleaching the skin nor the cutaneous
and extra-cutaneous complications of this widespread
cosmetic habit of black Africans. Furthermore, these cosmetics
and toiletries are not sold in the regular departmental stores nor
pharmacy shops in Europe and North America. They are either
manufactured purely for export to Africa or are exported
from Africa to Europe and N. America so that they are sold only
in local shops in ghettos patronized by the black Africans.
This paper sets out to give a brief review of this problem so
that practitioners worldwide would be aware of these complications which may at times be fatal.
Literature review
344
The use of skin bleaching agents or lighteners has been
reported in many parts of the world, such as Kenya,1 Ghana2
South Africa3,4 Zimbabwe5 USA6,7 Great Britain8 and SaudiArabia.9 Various chemicals have been used with consequent
undesirable side-effects. While phenols were reported to have
International Journal of Dermatology 2008, 47, 344 353
been associated with ochronosis10 the mercurials were
implicated in nephropathy.1,9 Addo in Ghana has also
reported squamous cell carcinoma associated with prolonged
bleaching.11
A survey done in Mali reported that 25% of two hundred
and ten women developed 74 different side-effects from the
use of bleaching creams.12 Similarly, in a refugee camp in
Balkan, 22.3% of the inhabitants including children were
found to have high concentrations of urinary mercury, which
was traced to the use of mercury containing bleaching
ointments, supplied.13
Exogenous ochronosis was first reported in 1906.14 It
commonly presents as asymptomatic blue-black macules on
the malar areas, temples, inferior cheeks and neck.15 This
condition resembles endogenous ochronosis in the skin
histologically, but does not exhibit any systemic complications
or the urinary abnormality. Hydroquinones are by far the
most common offending agents, but phenol, quinine injection
and resorcinol have also been implicated.16
In South Africa, where the first reports of complications of
hydroquinone abuse was reported, the government was prevailed upon in 1980 to set an upper limit of 2% hydroquinone
content in cosmetic products.17 Britain and the United States
of America also limit the concentration of hydroquinone in
cosmetic products to a maximum of 2%, and in dermatological
preparations to 4%. Although it was originally believed that
2008 The International Society of Dermatology
Olumide et al.
only high concentrations of hydroquinone were causal there
have been reports of ochronosis after use of 2% hydroquinone
preparations.1820 It has also been suggested that the percentage
of hydroquinone quoted by a manufacturer may not represent
the true concentration of hydroquinone in a product.21 It may
be that it is not the high concentration of hydroquinone, but
rather, extended use of this substance, which causes the
disease. An analysis of 41 bleaching creams available over the
counter in the UK in 1986 by Boyle and Kennedy revealed
that eight contained more than 2% hydroquinone.22
The scenario in Nigeria2333
The use of skin lightening creams has become a serious
phenomenon widely practiced by both men and women in
Nigeria. In a study of four hundred and fifty Nigerians who
confessed the use of bleaching creams, 73.3% were women
and 27.6% were men. The use of bleaching creams cuts
across all sociodemographic characteristics. People of all
religious groups, single or married, rich and poor, literate and
illiterate, low, middle and upper class use the products.
Various reasons were given for using the products. Some of
these are to look more attractive; to go with existing fashion
trend; to treat skin blemishes like acne or melasma; to cleanse
or tone the face and body; or to satisfy the taste of ones spouse.
Although the men also use the products for the above reasons,
some of them claimed they use the creams because their wives
use them; and some male marketers of female cosmetics and
toiletries claim they use the products to advertise their wares.
Some of the men are homosexuals. The habit of bleaching the
skin is most rampant among commercial sex workers who
camouflage their occupation in the clinic data as fashion
designer because of the opprobium attached to prostitution.
It is noteworthy that even some people who are naturally fair
in complexion, still use the bleaching creams to maintain the
light skin color and prevent tanning or blotches from sunlight.
As a result of both medical and public outcry against the
damaging effects of the skin lightening creams, the National
Food and Drug Agency of Nigeria (NAFDAC) had initially
allowed a maximum of 2% hydroquinone in bleaching
creams. However, due to the adverse side-effects associated
with long-term hydroquinone use and also lack of compliance
with content and labeling requirements, all forms of bleaching
agents were prohibited in cosmetics and toiletries. However,
in spite of the ban on these products, both the importation
and manufacture of the products have continued unabated.
This situation has been fostered largely by the vulnerability
of the consumers, the inexpensive nature of some of these
products, and the advertising agencies, who use lightcomplexioned ladies to advertise most consumer products
(e.g. alcoholic and nonalcoholic beverages, toiletries, cosmetics,
textiles, telephone handsets, etc.) both on the electronic and
print media. Hence, the dominant signal being sent to an
2008 The International Society of Dermatology
Complications of skin lightening cosmetics Report
undiscerning mind is that light complexioned people are
the beautiful ones.
In regard to ingredient labeling of cosmetics and toiletries
in Nigeria, most products are not registered by NAFDAC,
and bear no ingredient labeling nor address of manufacturers.
Some are even misbranded, e.g. a product which was labeled
as Betnovate-N was found to contain Mercury. Furthermore, the concentrations of chemicals on the labeled
products were largely found to be inaccurate on analysis as
most products exceeded the concentrations displayed on the
products. Since hydroquinone and mercury in cosmetics and
toiletries have been prohibited and have gained some notoriety,
manufacturers have now resorted to using synonyms of
hydroquinone to camouflage the products. Some of these
synonyms include 1, 4-Benzenediol, Quinol, Benzene-1,
4-diol, p-Diphenol, p-Dihydroxyl benzene, Hydrochinone,
p-hydroxylphenol, Hydrochinonium, Hydroquinol, and
Tequinol. All corticosteroid preparations can be purchased
over-the-counter in Nigeria. Hence, these products are readily
available not only in the pharmacy shops but also among
drug vendors in the open market place.
Chemicals often used and methods of use
The list of some of the bleaching creams used are given in
Table 1, and the contents of some analyzed products are on
Table 2. The same products are largely available in the African
countries mentioned above because of easy cross country
trade links. The active ingredients commonly used are hydroquinone, mercury, and a broad spectrum of the very potent
Table 1 A list of some of the bleaching creams used by patients
in Nigeria and ingredients as labeled
Cream
Ingredients
Movate
Crusader
Looking Good
Peauclair
Mic
Tura
Betamethasone dipropionate
Vitamed B3 toner 2%, Escalol UV 507, Vit E Allantoin
2% hydroquinone, Allantoin, Sunscreen, Vit E
Hydroquinone, Clobetasol propionate
Hydroquinone, Dimethicone, D-methyl-PABA
Octyl-Dimethyl PABA, Dimethicone,
Aqua glyceryl, propylene glycol mubbery
A-hydroxyl acids, methyl p-ben
Vitamed B3 toner 2%, Escalol UV 507, Vit E Allantoin
Benzophone 3-Dimethicone, Cyclomethicone
Triethanolamine, Carbomer, Dimethicone
Betamethasone dipropionate
Triethanolamine
Natural Essences from botany
2% hydroquinone padimate
2% hydroquinone Octisalate
2% hydroquinone, Vit E 1.0
Clobetasol propionate 0.05
Stearic Acid, MPG, Sorbitol Jelly, Fragrance
A3
Ultra
Venus
Swiss collagen
Fashion Fair
IKB
Shirley
Ambi
Skin Success
Sivoclaire
Fashoin Fair
Tony Montana
International Journal of Dermatology 2008, 47, 344 353
345
346
Report Complications of skin lightening cosmetics
Olumide et al.
25
Table 2 Contents of some creams analyzed
Cream
Hydroquinone (mg%)
Mercury (mg/kg)
Looking Good
Movate
Crusader
Sivoclaire
Peauclaire
Mercury
Mic
Tura
A3
1.36
5.10
3.45
0.06
0.06
1.68
0.06
1.45
0.42
0.17
0.20
0.26
0.22
0.21
0.82
0.22
0.23
0.18
corticosteroid preparations containing, e.g. Betamethasone
valerate and Clobetasol propionate.
Furthermore, the products are hardly used as marketed and
various additives are used to enhance the bleaching effect.
Some of the additives (concoction) are lemon juice, potash,
tooth paste, liquid milk, pulverized Naphthalene (camphor)
balls a mothproofing agent, Vitamin C, peroxides and
chlorates used in hair dyes. At times detergents are added to the
concoction. Some of the creams have equivalent soaps with
same chemicals incorporated. Indeed, the above listed additives
are not exhaustive.
At the initiation of the bleaching habit, a total body surface
immersion bath is often used for maximum effect. The
bleaching is then maintained with daily applications of the
creams. Most of the creams are very cheap so it is possible to
spend as little as 2 US dollars (about 300 Nigerian Naira) a
month on the bleaching creams to maintain the light complexion. Continuous use of the chemical is mandatory so that
the skin does not repigment. Even when the complications
appear, the bleachers often intensify the use of the chemicals
with the hope that the skin complications would eventually
be bleached away. Multiple products containing different
chemicals may be used concurrently or sequentially.
The duration of use of the bleaching creams before the
onset of complications vary from 6 to 60 months. However,
history from patients is often inaccurate, and some even deny
use of the bleaching creams, or pretend not to know their
functions due to a guilt complex, because various religious
groups and the press continue to condemn the practice of
changing the color of the natural skin.
Pathogenesis and complications
Hydroquinone
Hydroquinone is a dihydric phenol that has two important
derivatives viz monobenzyl and monomethyl ether of hydroquinone. Hydroquinone is known to competitively inhibit
melanin production by inhibiting sulfhydryl groups and acting
as a substrate for tyrosinase. The melanosomes and ultimately
International Journal of Dermatology 2008, 47, 344 353
the melanocytes are damaged by semiquinone free radicals
released during the above reaction.3436
With prolonged application and sun stimulation, the
melanocytes recover from the damaging effect of the hydroquinone which passes down into the papillary dermis of the
skin. Hence they are actively taken up by fibroblasts and lead
to altered elastic fiber production and excretion of abnormal
material into new fiber bundles.37 Furthermore, benzoquinone
acetic acid formed during the oxidative processes in which
hydroquinone is involved, bind and cross link collagen fibers
leading to degenerative changes due to altered physico-chemical
bonds.
Histologic examination of exogenous ochronotic lesions
reveals yellow-brown banana-shaped fibers in the papillary
dermis. Homogenization and swelling of the collagen bundles
is noted and a moderate histiocytic infiltrate may be present.
Sarcoid-like granulomas with multinucleated giant cells
engulfing ochronotic particles have been noted.38 Transfollicular
elimination of ochronotic fibers has also been described.39
Fibers stain black with Fontana stain and blue-black with
methylene blue stain.18,40 Ultrastructural examination reveals
homogenous electron-dense, irregular structures embedded
in an amorphous granular material infiltrating adjacent
collagen fibril bundles.42,43 The source of these ochronotic
fibers is not clear. Topical hydroquinones may inhibit
homogentisic acid oxidase in the skin, resulting in the local
accumulation of homogentisic acid that then polymerizes to
form ochronotic pigment.37,44,45 Pigmented particles may be
elastic or collagen fibers.19,46 Melanocytes may be involved;
most cases involve sun-exposed sites and one case is reported
of ochronosis that avoided areas of vitiligo.19,47 The changes
in the collagen bundles may be responsible for the loss of
elasticity and poor wound healing.
Complications of hydroquinone use that have been
reported are dermatitis, exogenous ochronosis, cataract,
pigmented colloid milia, scleral and nail pigmentation and
patchy depigmentation.3,4,15,20,26 The pigmented exogenous
ochronotic lesions are most marked on sun-exposed areas of
the body namely, face, upper chest and upper back. Dogliotte48
described 3 stages of this condition: (1) Erythema and mild
pigmentation; (2) hyperpigmentation, black colloid milia and
scanty atrophy; and (3) papulonodules with or without
surrounding inflammation. Figures 13 show exogenous
ochronosis. Since most commercial sex workers use these skin
lightening creams, some of them are HIV positive; and in an
attempt to bleach away the pruritic papular eruption (PPE)
commonly seen in HIV/AIDS patients, the skin of the extremities appear scruffy with the excoriated papules on a
background of ochronotic pigmentation on bleached skin as
shown in Figs 4 and 5. A patient developed squamous cell
carcinoma on the site of chronic exogenous ochronosis
(Fig. 6). It is not clear if this is a chance finding or an expected
sequelae of hydroquinone induced exogenous ochronosis
2008 The International Society of Dermatology
Olumide et al.
Complications of skin lightening cosmetics Report
Figure 1 Exogenous ochronosis (EO)
with superimposed chronic sun damage on the vulnerable
skin. Coalescence of multiple colloid milia may give rise to big
nodular lesions particularly on the upper back. The fawn
colored pigmentation of all 20 nails may mimic the yellow
nail syndrome hence the authors call the phenomenon
pseudo yellownail syndrome. Abnormal repigmentation
of depigmented skin has also been reported on discontinuing
therapy. This abnormal repigmentation has been attributed
to the Meirowsky effect of long wavelengths of ultraviolet
light darkening melanin already present in the skin and leading
to a skin color darker than that prior to bleaching. Because of
this repigmentation, users find it compelling to continue to
use the bleaching creams to maintain the newly acquired light
colored skin. Hence, the inevitable complications from
prolonged use. A more serious complication is loss of elasticity
of the skin and impaired wound healing. When cutting
through the skin, either for incisional biopsy or other surgical
procedures, it is as if one was cutting through the skin of a
cadaver. There is difficulty in apposing the edges of the
wounds when stitching, hence the skin often tears through the
suture material. Furthermore, there is often delayed wound
healing. After major abdominal surgeries like Caesarian
section, myomectomy, hysterectomy, etc., there may be
catastrophic wound dehiscence, burst abdomen, and death
from overwhelming infection.
The chronic bleachers also exude an offensive fish odor in
the sweat like the fish odor syndrome.39,40 The fish odor
2008 The International Society of Dermatology
Figure 2 Exogenous ochronosis in man
Figure 3 Exogenous ochronosis (EO)
syndrome, also known as trimethylaminuria, is characterized
by body odor of rotten fish. This is due to excretion of a
chemical, trimethylamine in the breath, urine, sweat, saliva,
and vaginal secretions.41
Trimethylamine (TMA) is produced in the gut mainly by
bacterial degradation of choline and lecithin-rich foods, such
International Journal of Dermatology 2008, 47, 344 353
347
348
Report Complications of skin lightening cosmetics
Olumide et al.
Figure 6 Squamous cell epithelioma on exogenous ochronosis
Figure 4 Exogenous ochronosis in a patient with PPE
Figure 5 Exogenous ochronosis in a patient with PPE
International Journal of Dermatology 2008, 47, 344 353
as salt water fish, eggs, offals (such as intestines, liver, and
kidney), and leguminous vegetables such as soya beans.
Normally, this compound is converted by TMA oxidase into
a stable nonodorous trimethylamine N-oxide (TMA-oxide)
that is then excreted in the urine. In the presence of a defective
TMA oxidase activity, the accumulated TMA is eliminated as
a volatile product in the urine, sweat, and breath, giving the
affected individual the characteristic fishy smell.
The TMA oxidase activity may be defective because of a
congenital, inherited impairment of N-oxidation (primary
trimethylaminuria) or for other acquired reasons that
interfere with the action of the enzyme (secondary trimethylaminurias). Some of these causes are: (1) overload with
TMA precursors, such as choline and lecithin, leading to
the formation of an increased burden of TMA through
enterobacterial degradation; (2) intake of inhibitors of
TMA oxidase, both dietary (e.g. Brussels sprouts) and
pharmacologic (e.g. thiourea), and (3) liver and kidney
diseases. In all these cases, the causative agent may act
rather as an inducing, precipitating factor in predisposed
subjects, who are carriers of the potential defect as heterozygotes. Other causes of fish odor are bacterial vaginosis, and
pemphigus vulgaris or foliaceus due to muco-cutaneous
bacterial degradation of body fluids.
Hydroquinone is an antioxidant, it may cause the fish odor
by reducing the ability to oxidize trimethylamine in chronic
bleachers, or hydroquinone may act rather as an inducing,
precipitating factor in predisposed subjects, who are carriers
of the potential defect as heterozygotes.
Treatment of exogenous ochronosis has been disappointing.
Tretinoin gel, cryotherapy, and trichloroacetic acid have
been tried without benefit. Cases of exogenous ochronosis
successfully treated with dermabrasion and CO2 laser16 and
Q-switched ruby laser49 have been reported.
2008 The International Society of Dermatology
Olumide et al.
Mercury
Mercury exists in three forms: organic, inorganic and
elemental. Mercury is a protoplasmic poison, which can be
absorbed by the respiratory tract as vapor or through the
skin and gastrointestinal tract as finely dispersed granules,
and excreted through the kidneys and colon. Cole50 observed
that the amount of mercury excreted by the kidneys was
proportional to the quantity applied on the skin. Until some
decades ago, mercury was ubiquitous in medicinal products
such as those used for treating syphilis, psoriasis, ringworm,
ophthalmic solutions, teething powders, and diuretics.
Though it is no longer commonly used in medications.
Mercury toxicity after topical applications was noted in
1923.51 Mercury toxicity may manifest in an acute or chronic
form. Acute toxicity usually manifests as a pneumonitis and
gastric discomfort. Chronic toxicity may be evidenced by
neurological manifestations and nephrotoxicity. Both organic
and inorganic preparations of mercury have been associated
with acute and chronic toxicity. Nephrotic syndrome due to
topical or systemic use of mercury has been well documented.1,52 Both membranous glomerulonephritis and
proliferative glomerulonephritis were found in patients
who had used mercury containing skin lightening creams.
Mercurious chloride, oxide and ammoniated mercury were
first introduced into the market during the first decade of the
20th century as the active ingredient in cosmetics and toiletries.
They eventually became popular as skin lighteners. Following
studies with electron microscope, mercury bleaches the skin
by probably inactivating the sulfhydryl enzymes.34,53 These
enzymes, which are called mercaptans due to their ability to
capture mercurial ions, then replace copper by competitive
inhibition leading to inactivation of the tyrosinase molecule
and interrupting melanin production. Paradoxically, chronic
use of mercury can also lead to increased pigmentation,
due to accumulation of mercury granules in the dermis.
These granules are absorbed via the skin appendages such
as the hair follicles and sebaceous glands into the dermis.
Deposition of mercury in keratin also leads to discoloration
and brittleness of the nails.51 Goeckermann54 noted that a
brown-gray discoloration of the face and neck (especially the
skin folds and eyelids) was associated with prolonged use of
mercury containing creams.
Corticosteroids
Corticosteroids bleach the skin. It is believed that they lighten
the skin due to inhibition of endogenous steroid production
and thus a decrease in precursor hormone levels. This precursor
hormone, propiocortin is also the precursor for melanocyte
stimulating hormone and thus, such negative feedback will
lead to decreased amounts of the hormone. Topical steroids
are also cytostatic to the epidermis. When used over a
prolonged period, they decrease the rate of epidermal turnover,
with fewer, abnormal, and less pigmented melanocytes on
2008 The International Society of Dermatology
Complications of skin lightening cosmetics Report
59,60
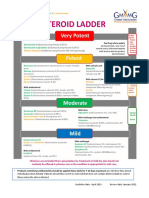
Table 3 Complications of topical steroids
Cutaneous
Atrophy of the skin (thinning and fine wrinkling)
Telangiectasia, purpura, persistent erythema
Skin fragility
Hypertrichosis
Perioral dermatitis
Pustular acneiform eruption (face) steroid rosacea
Folliculitis
Striae
Hypopigmentation
Steroid addiction syndrome
Predisposition and masking of cutaneous infection
(e.g. Tinea incognito, multiple filiform warts)
Allergic contact dermatitis
Ophthalmologic
Glaucoma
Cataracts
Endocrinologic
Cushingoid syndrome with moon facies,
buffalo humps, supraclavicular fat pads
Hyperglycaemia and diabetes mellitus
Suppression of hypothalamic-pituitary-adrenal axis
Suppression of growth in children
Menstrual irregularities
Edema
Electrolyte imbalance
Hypertension
Pseudotumor cerebri
Others
Aseptic necrosis of the head of femur
Predisposition to infection
Protein catabolism with negative nitrogen balance
Weakness, vertigo
Thrombophlebitis
Osteoporosis
histology. The skin lightening properties of these preparations have been found to be directly proportional to their
vasoconstrictor (blanching) effect.
Fluocinonide (Topsyn gel), Betamethasone dipropionate
(Diprosone), and Clobetasol propionate (Temovate) rate as
some of the strongest topical corticoids, and are among the
commonly used bleaching agents in Nigeria. They are readily
available in the market place among the battery of bleaching creams. When used as cosmetics, they are applied over
a large surface area for prolonged periods several months
to years. This factor, coupled with the occlusive effect of
environmental heat and humidity, promote percutaneous
absorption, and hence, complications. The possible complications of chronic corticosteroid use are shown in Table 3.
All these complications have been observed among chronic
bleachers in Nigeria.23,24,3135 Figs 714 show some of the
complications of long-term use of topical corticosteroids
as skin lightening cosmetics. The lower part of the axilla is
a favored site for steroid folliculitis (Fig. 7) and both sides
International Journal of Dermatology 2008, 47, 344 353
349
350
Report Complications of skin lightening cosmetics
Olumide et al.
Figure 7 Steroid folliculitis
are usually symmetrically affected. The striae are often
very wide (gaping) and erythematous (Figs 810). Overt
features of Cushings syndrome mooning of the face
and truncal obesity (Fig. 10) are frequently seen. Some of
them, at the time of presentation, have already developed
systemic manifestations like glucose intolerance and
hypertension.
Figure 8 Steroid folliculitis
Steroid addiction syndrome
The steroid addiction syndrome is the result of chronic daily
application for greater than a 1-month period of a potent or
moderately potent glucocorticosteroid preparation to the
facial skin, neck, scrotum or vulva. These tissues become
addicted to the topical steroid, so that withdrawing
the topical steroid results in severe burning which is only
relieved by further steroid applications. As application
continues, the patient experiences a rebound vasodilatation. Permanent redness of the facial skin eventuates,
with thinning and fine wrinkling of the skin. Indeed the
redness is so striking that the authors call the phenomenon
Lhomme rouge. For unexplainable reason, this permanent redness is more pronounced on male bleachers.
Furthermore, the thinning and wrinkling of the skin on
the neck gives a rippling pattern like the neck of a plucked
chicken, rather reminiscent of pseudoxanthoma elasticum
International Journal of Dermatology 2008, 47, 344 353
Figure 9 Steroid striae
2008 The International Society of Dermatology
Olumide et al.
Figure 10 Cushions syndrome
Complications of skin lightening cosmetics Report
Figure 12 Tinea corporis
Figure 13 Tinea incognito in a child
Figure 11 Tinea faciei andPseudo-pseudo xanthoma elasticum
on the neck
2008 The International Society of Dermatology
International Journal of Dermatology 2008, 47, 344 353
351
352
Report Complications of skin lightening cosmetics
Olumide et al.
multiple tiny filiform warts, common on the neck and upper
trunk (Fig. 14).
Paradoxically, topical corticosteroid preparations may
induce allergic contact dermatitis.58 This complication should
be considered in any patient with an eczematous dermatitis
who becomes worse or is refractory to topical steroid
treatment.
References
Figure 14 Eruptive filiform wart (Pseudo Lesser-Trlat sign)
note gaping striae
hence, the authors code this complication of steroid as
pseudo-pseudoxanthoma elasticum. (Fig. 11) Some
bleachers claim that they developed the habit of chronic
steroid use while trying to treat acne. They experienced
good response initially due to the anti-inflammatory effect
of the steroids. Abruptly stopping the topical steroids
preparation will result in increased numbers of papules and
pustules over the subsequent days a rebound phenomenon.
The patient soon finds it difficult to stop the steroid and the
facial skin then develops persistent redness, and acneiform
papules and pustules located on the nose, chin, cheeks, and
lower eyelids acne rosacea.
Predisposition to infections
A very common observed complication of steroid on
chronic bleachers is dermatophyte infection. Tinea faciei
(Fig. 11) is common in these patients and may mimic cutaneous lupus erythematosus or rosacea.5557 Very bizarre and
extensive Tinea corposis and cruris (Fig. 12) are often seen,
which are readily transmitted to the spouse and baby.
Hence, it is common to find the trio of wife, husband and
baby with Tinea incognito. Older children are not part of
this phenomenon. The wife often transmits the fungal infection to husband and baby because of close body contact.
Figure 13 shows a child with Tinea incognito on the forehead, acquired from the infected skin of the mother while
feeding on her breast. The clinical presentation of these
steroid induced dermatophyte infections are often atypical
hence the term Tinea incognito. Tinea versicolor could
also be very extensive, and is usually pigmented with dirty
brown scales.
Also, multiple histologically proven viral warts are
frequently found on these chronic bleachers. They often
appear in an eruptive manner rather reminiscent of eruptive
seborrheic keratosis (Leser-Trlat sign). Hence the authors
call this complication pseudo-Leser-Trelat sign. They are
International Journal of Dermatology 2008, 47, 344 353
1 Barr RD, Rees PH, Cordy PE, et al. Nephrotic Syndrome in
Adult Africans in Nairobi. Br Med J 1972; 2: 131134.
2 Addo HA. A Clinical study of hydroquinone reaction
in skin bleaching in Ghana. Ghana Med J 1992; 26:
448453.
3 Findlay GH, Morrison JGL, Simson IW. Exogenous
ochronosis and pigmented colloid millium from
hydroquinone bleaching creams. Brit J Dermatol 1975;
613622.
4 Hardwick N, Van Gelder LW, Van Der Merwe CA, et al.
Exogenous ochronosis in an epidemiological study. Br J
Dermatol 1989; 120: 229238.
5 Muchadeyi E, Thompson S, Baker N. A Survey of the
constituents, availability and use of the skin lightening
creams in Zimbabwe. Cent Afr J Med 1982; 29:
225227.
6 Cullison D, Abelle DC, OQuinn JL. Localised exogenous
ochronosis. J Am Acad Dermatol 1983; 8: 882889.
7 Hoshaw RA, Zimmerman KG, Menter A. Ochronosis-like
Pigmentation from Hydroquinone. Arch Dermatol 1985;
121: 105108.
8 Boyle J, Kennedy CTC. British Cosmetic regulations
inadequate. Br Medical J 1984; 288299.
9 Oliveira DGB, Foster G, Savill J, et al. Membranous
Nephropathy caused by mercury-containing skin lightening
cream. Postgrad Med J 1989; 63: 303304.
10 Beddard AP, Plumtre CM. A further note on ochronosis
associated with carboluria. Quart J Med 1912; 5:
505507.
11 Addo HA. Squamous cell cancinoma associated with
prolonged bleaching. Ghana Med J 2000; 34: 3.
12 Mahe A, Keita S, Bobin P. Dermatologic complications of
the cosmetic use of bleaching agents in Bamako (Mali). Ann
Dermatol Venereol 1994; 121: 142146.
13 Otto M, Ahlemeyer C, Tasche H, et al. Endemic mercury
burden caused by a bleaching ointment in Balken refugees.
Gesundheitswesen 1994; 56: 686689.
14 Pick L. Uber die Ochronose. Klin Wochenschr 1906; 43:
478480.
15 Snider RL, Thiers BH. Exogenous ochronosis. J Am Acad
Dermatol 1993; 28: 662664.
16 Diven DG, Smith EB, Pupo RA, et al. Hydroquinoneinduced localized exogenous ochronosis treated with
dermabrasion and CO2 laser. J Dermatol Surg Oncol 1990;
16: 10181022.
17 Ridley CM, Adams SJ. British cosmetic regulations
inadequate. Br Med J 1984; 288: 1537.
2008 The International Society of Dermatology
Olumide et al.
18 Tidman MJ, Horton JJ, MacDonald DM. Hydroquinoneinduced ochronosis light and electron-microscopic
features. Clin Exp Dermatol 1986; 11: 224228.
19 Hoshaw RA, Zimmerman KG, Menter A. Ochronosislike
pigmentation from hydroquinone bleaching creams
in American blacks. Arch Dermatol 1985; 121: 105108.
20 Lawrence N, Reed R, Perret WJ, et al. Exogenous ochronosis
in the United States. J Am Acad Dermatol 1988; 18: 1207
1222.
21 Brauer EW. Safety of over-the-counter hydroquinone
bleaching creams. [letter]. Arch Dermatol 1985; 121: 1239.
22 Boyle J, Kennedy CTC. Hydroquinone concentrations in
skin lightening creams. Br J Derm 1986; 114: 502504.
23 Olumide YM. Cosmetic Hazards and Legislative Needs in
Nigeria. Nig Med Prac 1985; 9: 712.
24 Olumide YM. Abuse of Topical corticosteroids in Nigeria.
Nig. Med. Pract 1986; 11: 1712.
25 Olumide YM, Elesha SO. Hydroquinone induced
exogenous ochronosis. Nig Med Pract 1986; 11: 103106.
26 Olumide YM. Photodermatoses in Lagos. Int J Dermatol
1987; 26: 295299.
27 Olumide YM. Contact leukoderma. Nig Quart J Hosp
Medical 1989; 4: 5362.
28 Olumide YM. A Pictorial Self-Instructional Manual on
Common Skin Diseases. Nigeria: Heinemann Ibadan, 1990.
29 Olumide YM, Odunowo BD, Odiase AO. Regional
dermatoses in the African I. Facial hypermelanosis. Int J
Dermatol 1991; 30: 186189.
30 Cosmetic Product Regulations (Prohibition of bleaching
agents etc). Extraordinary Federal Republic Nigeria Official
Gazette 1995; 82 (31c).
31 Olumide YM. Cosmetic habits and Legislative need in
Nigeria. Paper presented at NAFDAC Workshop on
Cosmetics Safety Issues, 2002.
32 Adebajo SB. An Epidemiological Survey of the Use of
Cosmetic Skin Lightening Cosmetics among Traders in
Lagos. Nigeria. Personal Communication.
33 Ofondu EO. Cosmetic use of bleaching creams in Enugu.
Nigerian FMCP Dissertation, 2003.
34 Lerner AB, Fitzpatrick TB. Inhibition of melanin formation
by chemical agents. J Invest Dermatol 1952; 18: 119135.
35 Jimbow K, Obata H, Pathak MA, et al. Mechanism of
Depigmentation by Hydroquinone. J Invest Dermatol 1974;
62: 436.
36 Findlay GH. Ochronosis following skin bleaching with
hydroquinone (Editorial). J Am Acad Dermatol 1982; 6:
10921093.
37 Goldsmith LA. Cutaneous changes in errors of amino acid
metabolism: alkaptonuria. In: Fitzpatrick TB, Eisen AZ,
Wolff K, Freedberg IM, Austen KF, eds. Dermatology in
General Medicine, Chap 148. New York: McGraw-Hill,
1993: 18411845.
38 Jackyk WK. Annular granulomatous lesions in exogenous
ochronosis are manifestations of sarcoidosis. Am J
Dermatopathol 1995; 17: 1822.
39 Jordaan HF, Van Niekerk DJT. Transepidermal elimination
2008 The International Society of Dermatology
Complications of skin lightening cosmetics Report
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
55
56
57
58
in exogenous ochronosis. Am J Dermatopathol 1991; 13:
418424.
Connor T, Braunstein B. Off-center fold: hyperpgimentation
following the use of bleaching creams: localized
exogenous ochronosis. Arch Dermatol 1987; 123:
105106.
Ruocco V, Florio M. Fish-odor syndrome: an olfactory
diagnosis. Int J Dermatol 1995; 34: 92 93.
Attwood HD, Clifton S, Mitchell RE, et al. A histological,
histochemical and ultrastructural study of dermal
ochronosis. Pathology (Phila) 1971; 3: 115.
Tidman MJ, Horton JJ, Macdonald DM, et al.
Hydroquinone-induced ochronosis: Light and electronmicroscopic features. Clin Exp Dermatol 1986; 11: 224.
Zannoni VG, Lomtevas N, Goldfinger S, et al. Oxidation of
homogentisic acid to ochronotic pigment in connective
tissue. Biochem Biophys Acta 1969; 177: 94.
Penneys ND. Ochronosislike pigmentation from
hydroquinone bleaching creams. [letter]. Arch Dermatol
1985; 121: 1239.
Phillips JI, Isaacson C, Carman H. Ochronosis in black
South Africans who used skin lighteners. Am J
Dermatopathol 1986; 8: 1421.
Hull PR, Procter PR. The melanocyte: An essential link in
hydroquinone induced ochronosis. J Am Acad Dermatol
1990; 22: 529531.
Dogliotte M, Liebowitz M. Granulomatous ochronosis a
cosmetic-induced skin disorder in blacks. S Afr Med J 1979;
56: 757760.
Kramer KE, Lopez A, Stefanato CM, et al. Exogenous
ochronosis. J Am Acad Dermatol 2000; 42: 869871.
Cole HN, Schreider N, Sollman J. Mercurial ointments in
the treatment of syphilis. Arch Dermatol 1930; 21: 372.
Alexander A, Mendel K. Chronishe Quecksilbervertifang
durch langdauernden Gebrauch einer Sommersprossensalbe. Deutsh Med Wschr 1923; 49: 1021.
Silverberg DS, McCall JT, Hunt JC. Nephrotic syndrome
with use of ammoniated mercury. Arch Intern Med 1967;
120: 583585.
Wealtherall DJ, Ledingham JGG, Warrell DA. Chemical
and physical injuries. Climatic and occupational
diseases. Oxford Textbook of Medicine 1985;
6.136.14.
Goeckermann WH. A peculiar discolouration of the skin.
JAMA 1975; 84: 506507.
Meymandi S, Wiseman MC, Crawford RI. Tinea faciei
mimicking cutaneous lupus erythematosus: a
histopathologic case report. J Am Acad Dermatol 2003; 48:
S7S8.
Singh R, Bharu K, Ghazali W, et al. Tinea faciei mimicking
lupus erythematosus. Cutis 1994; 53: 297298.
Lee SJ, Choi HJ, Hann SK. Rosacea-like tinea faciei. Int J
Dermatol 1999; 38: 479480.
Lutz ME, Gibson LE, el-Azhary RA, et al. Allergic contact
dermatitis to topical application of corticosteroids. Mayo
Clin Proc 1997; 72: 1141.
International Journal of Dermatology 2008, 47, 344 353
353
Você também pode gostar
- Risks of Mercury in Skin LighteningDocumento4 páginasRisks of Mercury in Skin LighteningDanyal2222Ainda não há avaliações
- Determination of Hydroquinone Content in Skin-Lightening Creams in Lagos, NigeriaDocumento5 páginasDetermination of Hydroquinone Content in Skin-Lightening Creams in Lagos, NigeriaftmrdrAinda não há avaliações
- Skin Lightening PreparationsDocumento7 páginasSkin Lightening PreparationsMarina BesselAinda não há avaliações
- Health Ministry Bans 9 Cosmetic ProductsDocumento11 páginasHealth Ministry Bans 9 Cosmetic ProductsFarah AmeliaAinda não há avaliações
- Personal-Care Cosmetic Practices in Pakistan: Current Perspectives and ManagementDocumento13 páginasPersonal-Care Cosmetic Practices in Pakistan: Current Perspectives and Managementummekhadija ashraf293Ainda não há avaliações
- SKIN CARE MERCURY RISKDocumento5 páginasSKIN CARE MERCURY RISKAdi PrayogaAinda não há avaliações
- The Phenomenon of Skin Lightening: Is It Right To Be Light?: AuthorsDocumento5 páginasThe Phenomenon of Skin Lightening: Is It Right To Be Light?: AuthorsGiovan GaulAinda não há avaliações
- Jurnal Hawa, 2017 PDFDocumento6 páginasJurnal Hawa, 2017 PDFIzmy PermataAinda não há avaliações
- Topic 5: Pharmacology Perspective in CosmeticsDocumento5 páginasTopic 5: Pharmacology Perspective in CosmeticsgaluhAinda não há avaliações
- Cosmetics Side EffectsDocumento17 páginasCosmetics Side EffectsIrwandyAinda não há avaliações
- Alora Night Glowing Cream DHM 2033Documento4 páginasAlora Night Glowing Cream DHM 2033Muhammad ImranAinda não há avaliações
- Cosmetics Are Substances Used To Enhance: ComponentDocumento10 páginasCosmetics Are Substances Used To Enhance: Componentsiti_wahid_2Ainda não há avaliações
- Evaluation of A Kojic Acid, PDFDocumento6 páginasEvaluation of A Kojic Acid, PDFvanitha13Ainda não há avaliações
- Jps R 06101406Documento4 páginasJps R 06101406Afiqah RahahAinda não há avaliações
- How Can Skincare Products Be ImprovedDocumento4 páginasHow Can Skincare Products Be ImprovedAnnisa RumAinda não há avaliações
- Cosmeceuticals - Current Trends and Market AnalysisDocumento3 páginasCosmeceuticals - Current Trends and Market AnalysisChiper Zaharia DanielaAinda não há avaliações
- Review of Related LiteratureDocumento7 páginasReview of Related LiteratureJamie HaravataAinda não há avaliações
- Sustainability 13 08786Documento13 páginasSustainability 13 08786Rillah LeswanaAinda não há avaliações
- Effects of Skin Lightening Cream Agents - Hydroquinone and Kojic Acid, On The Skin of Adult Female Experimental RatsDocumento7 páginasEffects of Skin Lightening Cream Agents - Hydroquinone and Kojic Acid, On The Skin of Adult Female Experimental Ratsindah ayuAinda não há avaliações
- Chemical Peeling in Ethnic Skin: An Update: What's Already Known About This Topic?Documento9 páginasChemical Peeling in Ethnic Skin: An Update: What's Already Known About This Topic?Rojas Evert AlonsoAinda não há avaliações
- Cosmetics Overview: Quality Control ParametersDocumento77 páginasCosmetics Overview: Quality Control ParametersGulshan DangiAinda não há avaliações
- Growing Fashion Craze: Threat To Public Health and MicrobesDocumento47 páginasGrowing Fashion Craze: Threat To Public Health and MicrobesshivahariAinda não há avaliações
- Odumosu and EkweDocumento4 páginasOdumosu and EkwePutri Nur HandayaniAinda não há avaliações
- Jcad 15 2 12Documento6 páginasJcad 15 2 12Putri IcaAinda não há avaliações
- Beauty Products Causing Cancer: Bachelor of PharmacyDocumento19 páginasBeauty Products Causing Cancer: Bachelor of PharmacyKumar AvinashAinda não há avaliações
- Environmental Research: Mètogbé Honoré Gbetoh, Marc AmyotDocumento8 páginasEnvironmental Research: Mètogbé Honoré Gbetoh, Marc AmyotMaria StfAinda não há avaliações
- Mercury-Laden and Other Harmful Substances in Cosmetic Products BannedDocumento2 páginasMercury-Laden and Other Harmful Substances in Cosmetic Products BannedEmilyn Mata CastilloAinda não há avaliações
- 6 Cosmetics and Its Health RisksDocumento9 páginas6 Cosmetics and Its Health Riskssabrina pusitAinda não há avaliações
- Article 007Documento6 páginasArticle 007Dyah Putri Ayu DinastyarAinda não há avaliações
- Elc550 Test - April2019Documento5 páginasElc550 Test - April2019Muhammad Azri HaziqAinda não há avaliações
- Cosmetics FactsheetDocumento5 páginasCosmetics Factsheetapi-264144691100% (1)
- Comments From The New York City Department of Health and Mental Hygiene On FDA'sDocumento3 páginasComments From The New York City Department of Health and Mental Hygiene On FDA'sMarina BesselAinda não há avaliações
- Cosmetics 07 00092Documento14 páginasCosmetics 07 00092ritaparautaAinda não há avaliações
- Dermatologicals in The PhilippinesDocumento8 páginasDermatologicals in The PhilippinesellochocoAinda não há avaliações
- Cosmetic and HealthDocumento3 páginasCosmetic and HealthharhoneyAinda não há avaliações
- Cosmetics' Safety: Gray Areas With Darker InsideDocumento6 páginasCosmetics' Safety: Gray Areas With Darker InsideA. K. MohiuddinAinda não há avaliações
- FINALIZED 2 Nigeria Call To Action Communique To EU - AAPNDocumento10 páginasFINALIZED 2 Nigeria Call To Action Communique To EU - AAPNOfoegbu Donald IkennaAinda não há avaliações
- Biodeterioration of Cosmetic ProductsDocumento21 páginasBiodeterioration of Cosmetic ProductsSundaralingam RajAinda não há avaliações
- Carcinogenic Effects of Personal Care ProductsDocumento23 páginasCarcinogenic Effects of Personal Care ProductsFatima KhalidAinda não há avaliações
- A Case Report On Hydroquinone Induced Exogenous OchronosisDocumento3 páginasA Case Report On Hydroquinone Induced Exogenous Ochronosisindah ayuAinda não há avaliações
- Cosmetic Testing On AnimalsDocumento19 páginasCosmetic Testing On AnimalsNhi Hoàng Lê NguyễnAinda não há avaliações
- Toxic-free hygiene products: Time to demand changeDocumento5 páginasToxic-free hygiene products: Time to demand changeNataliaAinda não há avaliações
- 0815 COVID-19 and Frequent Use of Hand Sanitizers - Human Health and Environmental Hazards by Exposure PathwaysDocumento50 páginas0815 COVID-19 and Frequent Use of Hand Sanitizers - Human Health and Environmental Hazards by Exposure PathwaysHenrico ImpolaAinda não há avaliações
- Side Effects of CosmeticsDocumento8 páginasSide Effects of CosmeticsTauqeerAhmadRajput100% (1)
- Buletin Farmasi 09/2013Documento12 páginasBuletin Farmasi 09/2013afiq83Ainda não há avaliações
- Fake Cosmetics Product Effects On HealthDocumento5 páginasFake Cosmetics Product Effects On Healthdiana ramzi50% (2)
- Mercury in Skin Whitening Cream PDFDocumento28 páginasMercury in Skin Whitening Cream PDFCristel SerranoAinda não há avaliações
- COSMETICS AND CONSUMERS: A GUIDE FOR INDUSTRY AND CONSUMERSDocumento30 páginasCOSMETICS AND CONSUMERS: A GUIDE FOR INDUSTRY AND CONSUMERSakshayprasadAinda não há avaliações
- Impact of Coronavirus (Covid-19) Pandemic On The Cosmetic Ingredients IndustryDocumento17 páginasImpact of Coronavirus (Covid-19) Pandemic On The Cosmetic Ingredients IndustryZahra GhalamiAinda não há avaliações
- Teen Perceptions Cosmetics Risks AmbonDocumento9 páginasTeen Perceptions Cosmetics Risks AmbonRiskayanti RamadhaniAinda não há avaliações
- EU Recalls 24 Microbe-Contaminated Cosmetics 2005-2008Documento4 páginasEU Recalls 24 Microbe-Contaminated Cosmetics 2005-2008AghniaAinda não há avaliações
- CHEMISTRY PROJECT Shreya ThokalDocumento33 páginasCHEMISTRY PROJECT Shreya Thokal28-Shreya ThokalAinda não há avaliações
- 1.1 Background of The Study: Chen, Qiushi (2009)Documento10 páginas1.1 Background of The Study: Chen, Qiushi (2009)John Fetiza ObispadoAinda não há avaliações
- (Cosmetic Science and Technology Series) Jungermann, Eric - Glycerine - A Key Cosmetic Ingredient-CRC Press - Taylor and Francis (2017)Documento477 páginas(Cosmetic Science and Technology Series) Jungermann, Eric - Glycerine - A Key Cosmetic Ingredient-CRC Press - Taylor and Francis (2017)Hoàng Ngọc AnhAinda não há avaliações
- Rise of the Vegan Cosmetics Industry in IndiaDocumento23 páginasRise of the Vegan Cosmetics Industry in IndiaPrativa KumariAinda não há avaliações
- Cosmetic Dermatology: Products and ProceduresNo EverandCosmetic Dermatology: Products and ProceduresNota: 5 de 5 estrelas5/5 (1)
- Cosmetics for the Skin: Physiological and Pharmaceutical ApproachNo EverandCosmetics for the Skin: Physiological and Pharmaceutical ApproachAinda não há avaliações
- Look Great, Live Green: Choosing Bodycare Products that Are Safe for You, Safe for the PlanetNo EverandLook Great, Live Green: Choosing Bodycare Products that Are Safe for You, Safe for the PlanetNota: 3.5 de 5 estrelas3.5/5 (40)
- Frankincense Oil Cancer RemediesDocumento3 páginasFrankincense Oil Cancer RemediesManea LaurentiuAinda não há avaliações
- Asthma: Assessment, Diagnosis, and Treatment Adherence: Gerri KaufmanDocumento8 páginasAsthma: Assessment, Diagnosis, and Treatment Adherence: Gerri KaufmandessyAinda não há avaliações
- Corticosteroid Classes - A Quick Reference Guide Including Patch Test Substances and Cross-ReactivityDocumento5 páginasCorticosteroid Classes - A Quick Reference Guide Including Patch Test Substances and Cross-ReactivityBreiner PeñarandaAinda não há avaliações
- Florinef SPCDocumento7 páginasFlorinef SPCJohn GoulianosAinda não há avaliações
- Topical Corticosteroid Supply Shortage GuidanceDocumento3 páginasTopical Corticosteroid Supply Shortage GuidancesyahrulroziAinda não há avaliações
- Pharmacology Exam 3 Pharmacology Exam 3Documento44 páginasPharmacology Exam 3 Pharmacology Exam 3LillabinAinda não há avaliações
- Double-Blind Clinical Topical Steroids Uveitis: Trial of in AnteriorDocumento6 páginasDouble-Blind Clinical Topical Steroids Uveitis: Trial of in Anteriorguugle gogleAinda não há avaliações
- Dental Medical History Form English and ArabicDocumento5 páginasDental Medical History Form English and ArabicAbdulrahman QA/QCAinda não há avaliações
- VentolinDocumento13 páginasVentolinFitrah NstAinda não há avaliações
- Adrenocorticosteroids & Adrenocortical AntagonistsDocumento20 páginasAdrenocorticosteroids & Adrenocortical Antagonistsapi-3859918Ainda não há avaliações
- Mellen Center MS Relapse TreatmentDocumento5 páginasMellen Center MS Relapse TreatmentNgakanAinda não há avaliações
- Internal Medicine - DermatologyDocumento125 páginasInternal Medicine - DermatologySoleil DaddouAinda não há avaliações
- Name of Drug Mechanism of Action Indications Contraindication Side Effects Nursing Responsibilities Generic Name: BeforeDocumento5 páginasName of Drug Mechanism of Action Indications Contraindication Side Effects Nursing Responsibilities Generic Name: BeforeWestley RubinoAinda não há avaliações
- O Papel Das Drogas Antiparasitárias e Corticóides No Tratamento Da Covid-19Documento14 páginasO Papel Das Drogas Antiparasitárias e Corticóides No Tratamento Da Covid-19Guilherme marinhoAinda não há avaliações
- Acute Multiple Sclerosis RelapseDocumento16 páginasAcute Multiple Sclerosis RelapseHabib G. Moutran BarrosoAinda não há avaliações
- Cushings Addisons and Acromegaly EdDocumento45 páginasCushings Addisons and Acromegaly EdAny PopAinda não há avaliações
- 2 2015 Nsaid Analgetik AntipiretikaDocumento65 páginas2 2015 Nsaid Analgetik AntipiretikasekarAinda não há avaliações
- Medicine MOMDocumento7 páginasMedicine MOMsushilshsAinda não há avaliações
- ADDISONS DSE - Etio Trends&Issues + DSDocumento9 páginasADDISONS DSE - Etio Trends&Issues + DSgraceAinda não há avaliações
- Drug StudyDocumento17 páginasDrug StudyKenneth ManalangAinda não há avaliações
- Drug Study #4Documento7 páginasDrug Study #4Sarah Kaye BañoAinda não há avaliações
- Mometasone FuroatDocumento8 páginasMometasone FuroatAnonymous ZrLxxRUr9zAinda não há avaliações
- CH 52 Assessment and Management of Patients With Endocrine DisordersDocumento15 páginasCH 52 Assessment and Management of Patients With Endocrine Disordersfiya33Ainda não há avaliações
- Oral CorticosteroidsDocumento29 páginasOral CorticosteroidsloraAinda não há avaliações
- Topical Corticosteroid PotencyDocumento2 páginasTopical Corticosteroid PotencyTeffi Widya JaniAinda não há avaliações
- Topical SteroidsDocumento10 páginasTopical SteroidsMariaAinda não há avaliações
- VitiligoDocumento24 páginasVitiligoAnonymous hTivgzixVNAinda não há avaliações
- Stress y ConceptosDocumento10 páginasStress y ConceptosVivian FTAinda não há avaliações
- Prednisone TabDocumento10 páginasPrednisone TabrantiadrianiAinda não há avaliações
- GM Steroid LadderDocumento2 páginasGM Steroid LadderRenee McGuinnessAinda não há avaliações