Escolar Documentos
Profissional Documentos
Cultura Documentos
Clinical Tips For Halterman Appliance
Enviado por
Rizky AmaliaDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Clinical Tips For Halterman Appliance
Enviado por
Rizky AmaliaDireitos autorais:
Formatos disponíveis
PEDIATRIC DENTISTRY
V 29 / NO 4
JUL / AUG 07
Clinical Article
Clinical Tips for the Halterman Appliance
David B. Kennedy, BDS, LDS RCS (Eng), MSD, FRCD(C)1
Abstract: Ectopic eruption of permanent rst molars occurs infrequently and causes some resorption of the adjacent primary second molar. The
primary second molar can be used as an anchor tooth for the Halterman appliance to disimpact the permanent rst molar, provided root resorption is not extreme. A modication of the Halterman appliance is a reverse band and loop appliance with a bonded button on the permanent
molar and chain elastic for disimpaction. The purpose of this report was to suggest tips regarding placement and clinical management of this
modied Halterman appliance design. (Pediatr Dent 2007;29:327-9)
KEYWORDS: ERUPTION, ECTOPIC TOOTH, HALTERMAN APPLIANCE, ORTHODONTICS, INTERCEPTIVE
Ectopic eruption of permanent rst molars occurs in 3-4%
of children. The maxillary arch is usually aected; only rarely
does this occur in the mandible.1 Etiological factors include
a: (1) sibling with ectopic eruption2; (2) shorter smaller maxilla3,4; (3) larger mesiodistal width of the permanent rst
permanent molar with increased mesial inclination4; (4)
cleft lip and/or palate5; and (5) association with other dental
anomalies.6
Kennedy and Turley7 have described strategies for the
clinical management of ectopically erupting permanent rst
molars. When the primary second molar has not suered extensive resorption and is symptom free, it is recommended
that it be used as an abutment tooth for a Halterman type
appliance.7,8
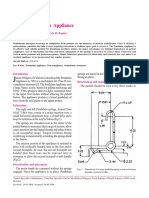
Halterman8 described an appliance for correcting impacted permanent maxillary rst molars. The primary maxillary second molar is banded with a soldered
wire extending distally to the impacted permanent rst
molar with a recurved hook on the distal extension. A
bonded button is attached to the occlusal surface of the
permanent rst molar (Figure 1). Chain elastic is used
from the occlusal button to the recurved hook on the distally extending wire to distalize the impacted molar. The
distal extension must be accurately adapted to avoid tissue
impingement. This appliance has been very predictable, but
1 Dr. Kennedy is an orthodontist and pediatric dentist in private practice in Vancouver, BC,
Canada.
Correspond with Dr. Kennedy at drdavidkennedy@yahoo.ca
some modications and clinical tips are oered to enhance
clinical success.
Figure 1. Halterman appliance.
Appliance design
Since the permanent maxillary rst molar will often rotate
around the palatal cusp coincident with the impaction,9 there
may be a need to move the impacted molar both distally and
to the buccal. Haltermans appliance design does not allow
for this directional force. The authors recommended modication is to use a reverse band and loop appliance extending
distal to the impacted permanent rst molar. The laboratory
can be instructed to place 2 spurs on the distal extension: 1
towards the buccal and 1 towards the lingual (Figure 2). Chain
elastic can be placed using a catapult or sling shot approach
to increase the disimpaction force. The direction of elastic
HALTERMAN APPLIANCE
327
PEDIATRIC DENTISTRY
V 29 / NO 4
JUL / AUG 07
force can be varied, which can assist in improved alignment
of the impacted permanent molar. It is imperative that the lab
make the extension of the Halterman appliance suciently
wide mesiodistally to accommodate the full width of the permanent molar. This requires both an accurate impression of
the hamular notch and good communication with the lab.
Figure 2. Modied Halterman appliance
with reverse band and loop extension,
2 spurs, and an occlusal bonded button
with chain elastic placed in a slingshot or
catapult pattern.
Figure 5. Occlusal view taken 4 months
after Figure 2 shows overcorrection of
impacted tooth #14.
Figure 3. Occlusal view shows impaction
of the permanent maxillary left rst molar
(tooth #14)
Figure 4. Panoramic radiograph shows impaction of tooth #14
Figure 6. Panoramic radiograph taken 4
months after Figure 3 shows overcorrection
of impacted tooth #14. Note root resorption
on the adjacent primary second molar.
Figure 7. Maxillary occlusal view taken 5 years
later shows satisfactory eruption in the permanent dentition.
Placement of the occlusal button
Placing the occlusal button can be challenging in a young
mixed dentition patient because of location and isolation
during acid etching and placement of the bonded attachment.
To facilitate good retention of the occlusal button, the author
recommends working with 2 chairside assistants and placing
a dry foil in the corner of the mouth for saliva control. One
clinical assistant should be responsible exclusively for isolation, and the second assistant should facilitate instrument
transfer. Light-cured composite is used to retain the occlusal
button because of its quicker set in an area that is dicult to
isolate. An alternative would be to use glass ionomer cement.
The occlusal button should be placed as far mesially as
possible to:
1. allow greater length of elastic chain to assist the disimpaction; and
328
HALTERMAN APPLIANCE
2. reduce occlusal trauma, because the mesial inclination
of the impacted molar results in occlusal interference if
the bonded button were placed more distally.
Ideally, the bonded button should be placed no further
distally than the distal slope of the mesiobuccal cusp of the
rst permanent molar.
Clinical management
After appliance placement, the chain elastic is changed at
2- to 3-week intervals. If the impacted permanent molar
needs to be moved to the buccal, the chain is applied from
the bonded button to the buccal-soldered spur. For a purely
distal movement, the elastic can be stretched from the distal
buccal spur to the bonded button and back to the distolingual
spur in a catapult or slingshot design, as shown in Figure 2.
Figures 3 to 7 show short- and long-term results with
this technique. The impaction is usually corrected within 2 to
4 months (Figures 3 through 6), and over correction is recommended (Figure 6). After disimpaction, the chain elastic
is removed and the appliance is left on as the permanent rst
molar erupts. Once the clinician is assured that the permanent rst molar impaction remains corrected, the appliance
is removed (Figure 3, 5, and 6). Because root resorption on
PEDIATRIC DENTISTRY
the primary second molar has occurred, careful monitoring
for premature exfoliation is necessary.7 Provided there is adequate space and no premature loss of the primary maxillary
second molar, there is satisfactory eruption of the permanent dentition (Figure 7).
References
1. Young DH. Ectopic eruption of the rst permanent molar.
J Dent Child 1957;24:153-62.
2. Bjerklin K, Kurol J. Ectopic eruption of the maxillary
rst permanent molar: Etiologic factors. Am. J Orthod
1983;84:147-55.
3. Canut JA, Raga C. Morphological analysis of cases with
ectopic eruption of the maxillary rst permanent molar.
Eur J Orthod 1983;5:249-53.
4. Pulver F. The etiology and prevalence of ectopic eruption of the maxillary rst permanent molar. J Dent Child
1968;35:138-46.
V 29 / NO 4
JUL / AUG 07
5. Bjerklin K, Kurol J, Paulin G. Ectopic eruption of maxillary first permanent molars in children with cleft lip
and/or palate. Eur J Orthod 1993;15:535-40.
6. Bjerklin K, Kurol J, Valentin J. Ectopic eruption of maxillary rst permanent molars and association with other
tooth and developmental disturbances. Eur J Orthod
1992;14:369-75.
7. Kennedy DB, Turley PK. The clinical management of
ectopically erupting rst permanent molars. Am J Orthod
1987;92:336-45.
8. Halterman CW. Simple technique for the treatment of
ectopically erupting rst permanent molars. J Am Dent
Assoc 1982;105:1031-3.
9. Ackerman JL, Prot WR. Diagnosis and planning treatment. In: Graber TM, Swain BF, eds. Current Orthodontic
Concepts and Techniques. Philadelphia, Pa: WB Saunders
Co; 1975:51.
HALTERMAN APPLIANCE
329
Você também pode gostar
- Halterman Technique For The Treatment of Ectopically Erupting Permanent First MolarsDocumento7 páginasHalterman Technique For The Treatment of Ectopically Erupting Permanent First MolarsIOSRjournalAinda não há avaliações
- The Clincal Management of Ectopically Erupting First Permanent MolarsDocumento6 páginasThe Clincal Management of Ectopically Erupting First Permanent MolarsFourthMolar.comAinda não há avaliações
- Orthodontic Uprighting of Impacted Mandibular Permanent Second Molar: A Case ReportDocumento4 páginasOrthodontic Uprighting of Impacted Mandibular Permanent Second Molar: A Case ReportLucy UrrunagaAinda não há avaliações
- Tooth-Supported Telescopic Prostheses in Compromised Dentitions - A Clinical ReportDocumento4 páginasTooth-Supported Telescopic Prostheses in Compromised Dentitions - A Clinical Reportpothikit100% (1)
- The "Ballista Spring" System For Impacted Teeth: Genevu. SwitzerlandDocumento9 páginasThe "Ballista Spring" System For Impacted Teeth: Genevu. Switzerlandapi-26468957100% (1)
- Kokich CaninosDocumento6 páginasKokich CaninosMercedes RojasAinda não há avaliações
- Bite RegistratnDocumento68 páginasBite RegistratnBimalKrishnaAinda não há avaliações
- Pi Is 0889540615013311Documento5 páginasPi Is 0889540615013311msoaresmirandaAinda não há avaliações
- E1 MJAFImaxexpansionusingquadhelixinclp2009Documento5 páginasE1 MJAFImaxexpansionusingquadhelixinclp2009ريام الموسويAinda não há avaliações
- Canine Impaction Different MethodsDocumento11 páginasCanine Impaction Different MethodsMSHAinda não há avaliações
- Non-Rigid Connector Manages Pier AbutmentDocumento3 páginasNon-Rigid Connector Manages Pier AbutmentIana RusuAinda não há avaliações
- Molares InclinadosDocumento13 páginasMolares Inclinadosmaria jose peña rojas100% (1)
- Inclinacion 2 MolarDocumento4 páginasInclinacion 2 MolarMan Sito0% (1)
- Ijcrims 1Documento9 páginasIjcrims 1smritiAinda não há avaliações
- Openbite MIA AJODODocumento10 páginasOpenbite MIA AJODOscribdlptAinda não há avaliações
- Practice: Orthodontics. Part 5: Appliance ChoicesDocumento10 páginasPractice: Orthodontics. Part 5: Appliance ChoicesIon CiobanuAinda não há avaliações
- Clinical: Use of Distal Implants To Support and Increase Retention of A Removable Partial Denture: A Case ReportDocumento4 páginasClinical: Use of Distal Implants To Support and Increase Retention of A Removable Partial Denture: A Case ReportDentist HereAinda não há avaliações
- Rapid Palatal ExpanderDocumento28 páginasRapid Palatal ExpandertonhanrhmAinda não há avaliações
- Management of Impacted Maxillary Canines Using Mandibular AnchorageDocumento4 páginasManagement of Impacted Maxillary Canines Using Mandibular AnchoragedrsankhyaAinda não há avaliações
- Cadman 1975Documento36 páginasCadman 1975Sai KrupaAinda não há avaliações
- Distalization of Maxillary First Permanent Molar by Pendulum Appliance in Mixed Dentition PeriodDocumento3 páginasDistalization of Maxillary First Permanent Molar by Pendulum Appliance in Mixed Dentition PeriodDea favellaAinda não há avaliações
- Scissors Bite-Dragon Helix ApplianceDocumento6 páginasScissors Bite-Dragon Helix ApplianceGaurav PatelAinda não há avaliações
- Uprighting MolarsDocumento7 páginasUprighting MolarsMa Lyn Gabayeron100% (1)
- Anterior Crossbite Correction Using Removable Expansion ScrewsDocumento5 páginasAnterior Crossbite Correction Using Removable Expansion ScrewsElham ZareAinda não há avaliações
- Band and Pontic: A Modified Band and Loop Space Maintainer - Clinical InnovationDocumento3 páginasBand and Pontic: A Modified Band and Loop Space Maintainer - Clinical InnovationIJAR JOURNALAinda não há avaliações
- Space regainers in pediatric dentistryDocumento5 páginasSpace regainers in pediatric dentistryShirmayne TangAinda não há avaliações
- J Pio 2010 08 002Documento8 páginasJ Pio 2010 08 002Jonathan GIraldo MartinezAinda não há avaliações
- New Fixed Acrylic Bite Plane for Deep Bite CorrectionDocumento6 páginasNew Fixed Acrylic Bite Plane for Deep Bite CorrectionFisaAinda não há avaliações
- Molar Distalization With A Partially Integrated Mini-Implant To Correct Unilateral Class II MalocclusionDocumento10 páginasMolar Distalization With A Partially Integrated Mini-Implant To Correct Unilateral Class II MalocclusionNg Chun HownAinda não há avaliações
- Immediate Denture Advantages and TechniquesDocumento11 páginasImmediate Denture Advantages and TechniquesClaudia AngAinda não há avaliações
- Effects Muscular Anchorage Appliances On Deficient Mandibdar Arch Zeng THDocumento11 páginasEffects Muscular Anchorage Appliances On Deficient Mandibdar Arch Zeng THYeraldin EspañaAinda não há avaliações
- Class II Correction Using Sagittal Appliance and Molar ExtractionDocumento7 páginasClass II Correction Using Sagittal Appliance and Molar ExtractionYudia PangestiAinda não há avaliações
- Modified Oral Screen Case ReportDocumento9 páginasModified Oral Screen Case Reportfayasyabmin100% (1)
- Fixed Functional AppliancesDocumento82 páginasFixed Functional Appliancesdisha 146jandialAinda não há avaliações
- Angle 2007 Ene 155-166Documento12 páginasAngle 2007 Ene 155-166André MéndezAinda não há avaliações
- Prosthetic Management of Implants Placed With The Socket-Shield TechniqueDocumento5 páginasProsthetic Management of Implants Placed With The Socket-Shield TechniqueRiya KvAinda não há avaliações
- Guided Eruption of Palatally Impacted Canines Through Combined Use of 3-Dimensional Computerized Tomography Scans and The Easy Cuspid DeviceDocumento14 páginasGuided Eruption of Palatally Impacted Canines Through Combined Use of 3-Dimensional Computerized Tomography Scans and The Easy Cuspid DeviceSaurav Kumar DasAinda não há avaliações
- Herbst ApplianceDocumento21 páginasHerbst Applianceimtiyazorthodontist83% (6)
- Chung2010 PDFDocumento12 páginasChung2010 PDFsmritiAinda não há avaliações
- Isrn Dentistry2012-259891 PDFDocumento7 páginasIsrn Dentistry2012-259891 PDFAdriana Paola Vega YanesAinda não há avaliações
- Jioh 7 65Documento3 páginasJioh 7 65Athira JithendranathAinda não há avaliações
- Slow Maxillary Expansion A Review 209085c4Documento12 páginasSlow Maxillary Expansion A Review 209085c4jabbarAinda não há avaliações
- Orthodontics andDocumento9 páginasOrthodontics andSimona DobreAinda não há avaliações
- Mermigos 11 01Documento4 páginasMermigos 11 01Sankurnia HariwijayadiAinda não há avaliações
- Twin BlockDocumento130 páginasTwin BlockRolando GamarraAinda não há avaliações
- Compomer CrownDocumento2 páginasCompomer CrownIndah SimamoraAinda não há avaliações
- Full Mouth Rehabilitation of The Patient With Severly Worn Out Dentition A Case Report.Documento5 páginasFull Mouth Rehabilitation of The Patient With Severly Worn Out Dentition A Case Report.sivak_198100% (1)
- Distalising Molars How Do You Do It 31 03 2015Documento21 páginasDistalising Molars How Do You Do It 31 03 2015Dorian GrayAinda não há avaliações
- Bilateral Sagittal Split OsteotomyDocumento8 páginasBilateral Sagittal Split OsteotomydoctorniravAinda não há avaliações
- British Journal of Oral and Maxillofacial Surgery 45-1-83 84 Buccal Corticotomy For Removal of Deeply Impacted Mandibular Molars TayDocumento2 páginasBritish Journal of Oral and Maxillofacial Surgery 45-1-83 84 Buccal Corticotomy For Removal of Deeply Impacted Mandibular Molars TayGonzalo BarrientosAinda não há avaliações
- Molar Uprighting Simple TechniqueDocumento4 páginasMolar Uprighting Simple TechniqueMariem DelmasAinda não há avaliações
- Distal Shoes Space MaintainerDocumento5 páginasDistal Shoes Space MaintainerEduardo FernandezAinda não há avaliações
- Clinical Consideration Before Bridge ConstructioDocumento19 páginasClinical Consideration Before Bridge ConstructioAseelAinda não há avaliações
- 7-Maxillary Canine ImpactionDocumento8 páginas7-Maxillary Canine ImpactionAhmed aljumailiAinda não há avaliações
- Bonded Pendulum Appliance: Methods in MedicineDocumento3 páginasBonded Pendulum Appliance: Methods in MedicinesmritiAinda não há avaliações
- Interceptive Orthodontics: A Practical Guide to Occlusal ManagementNo EverandInterceptive Orthodontics: A Practical Guide to Occlusal ManagementAinda não há avaliações
- Treatment Planning Single Maxillary Anterior Implants for DentistsNo EverandTreatment Planning Single Maxillary Anterior Implants for DentistsAinda não há avaliações
- Interstitial Cystitis (Painful Bladder Syndrome) - Causes & TreatmentDocumento12 páginasInterstitial Cystitis (Painful Bladder Syndrome) - Causes & TreatmentJimmy GillAinda não há avaliações
- USMLE Step 1 NBME Top Concepts 2021Documento475 páginasUSMLE Step 1 NBME Top Concepts 2021dalia khamoAinda não há avaliações
- Rundown Iomu 071019 - 08.10 PDFDocumento13 páginasRundown Iomu 071019 - 08.10 PDFEfi OctavianyAinda não há avaliações
- MCQs blood & cell physiology blogDocumento8 páginasMCQs blood & cell physiology bloglubna malikAinda não há avaliações
- The Race Myth (Excerpted)Documento30 páginasThe Race Myth (Excerpted)Wayne Owen Richards100% (1)
- Psychosis ObjectivesDocumento14 páginasPsychosis ObjectivesfatenAinda não há avaliações
- The Politics of The Asia-Pacific Triumphs, Challenges, and Threats (Mark S. Williams (Editor)Documento381 páginasThe Politics of The Asia-Pacific Triumphs, Challenges, and Threats (Mark S. Williams (Editor)lelenaAinda não há avaliações
- Uganda Participatory Poverty Assessment Report 2000Documento193 páginasUganda Participatory Poverty Assessment Report 2000FabioAinda não há avaliações
- Introduction To Community Health Nursing ExposureDocumento33 páginasIntroduction To Community Health Nursing ExposureRay LaderaAinda não há avaliações
- Pediatrics ImpDocumento233 páginasPediatrics Impملك عيسى100% (1)
- Unseen PassageDocumento7 páginasUnseen PassageVinay OjhaAinda não há avaliações
- 2011 Annual Accomplishment Report - MalabonDocumento63 páginas2011 Annual Accomplishment Report - MalabonBernadeth AganaAinda não há avaliações
- Diabetic Ketoacidosis in PregnancyDocumento12 páginasDiabetic Ketoacidosis in PregnancyMuhammad BilalAinda não há avaliações
- Neonatal Disease Severity Scoring SystemsDocumento6 páginasNeonatal Disease Severity Scoring Systemsida ayu agung WijayantiAinda não há avaliações
- Genetics of Mitochondrial Disease: Russell P. SanetoDocumento54 páginasGenetics of Mitochondrial Disease: Russell P. SanetoGréta BotyánszkiAinda não há avaliações
- BBL™ Mueller Hinton Broth: - Rev. 02 - June 2012Documento2 páginasBBL™ Mueller Hinton Broth: - Rev. 02 - June 2012Manam SiddiquiAinda não há avaliações
- Med 1 Block 2 - Wet Lab NotesDocumento36 páginasMed 1 Block 2 - Wet Lab NotesluckyAinda não há avaliações
- KRF Guideline Chest KeloidsDocumento29 páginasKRF Guideline Chest Keloidscanciondemayo3358Ainda não há avaliações
- Knight, Angela - The VampdomDocumento8 páginasKnight, Angela - The VampdomLaviniaAinda não há avaliações
- Important Uses of Neem ExtractDocumento3 páginasImportant Uses of Neem ExtractAbdurrahman MustaphaAinda não há avaliações
- TB PDFDocumento12 páginasTB PDFHana AshrafAinda não há avaliações
- MCQ in MedicineDocumento18 páginasMCQ in MedicineEslamAlmassri75% (4)
- E Book Coffee Leaf TeaDocumento18 páginasE Book Coffee Leaf TeaAsun ArceAinda não há avaliações
- Non-Profit Organization Funds Gregory Grabovoi TeachingsDocumento95 páginasNon-Profit Organization Funds Gregory Grabovoi Teachingsssss87va93% (27)
- Turkish Angora CatDocumento6 páginasTurkish Angora CatprosvetiteljAinda não há avaliações
- Essential Health Services and PlansDocumento4 páginasEssential Health Services and Planszahara mahalAinda não há avaliações
- NEET Biology Through MCQDocumento587 páginasNEET Biology Through MCQAnanth Dharanidharan100% (1)
- Yellow Fever Vaccination Requirements From India - Chalo AfricaDocumento148 páginasYellow Fever Vaccination Requirements From India - Chalo AfricaAbishek ChandranAinda não há avaliações
- SEMINAR-Clinical Microbiology: Topic-Human Immuno-Deficiency Virus (HIV)Documento54 páginasSEMINAR-Clinical Microbiology: Topic-Human Immuno-Deficiency Virus (HIV)sushant_dharAinda não há avaliações