Escolar Documentos
Profissional Documentos
Cultura Documentos
Beta Adrenergic Receptor Blockers
Enviado por
niwas0 notas0% acharam este documento útil (0 voto)
36 visualizações7 páginasphamacology beta blockers notes
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
DOCX, PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentophamacology beta blockers notes
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato DOCX, PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
36 visualizações7 páginasBeta Adrenergic Receptor Blockers
Enviado por
niwasphamacology beta blockers notes
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato DOCX, PDF, TXT ou leia online no Scribd
Você está na página 1de 7
Beta adrenergic receptor blockers
1.Review the effects of stimulation and blockade of beta receptors
1.Adrenoreceptors
Location
Postsynaptic,Excitatory
Agonist
Epinephrine,Norepinephrine,Isoprenaline,Dobutamine
Antagonist
Propanolol,Atenolol
Effects of beta receptor block
Heart
Negative inotropic Decrease in FOC
Negative chronotropic Decrease in HR,COP and BP
Decrease in AV conduction,Decrease automatically
Decrease in oxygen consumption of heart
Other actions
Decrease in secretion of Renin
Decrease in glycogenolysis,decrease in gluconeogenesis which
results in delayed recovery from hypoglycemia
2.Adrenoreceptors
Location
Postsynaptic,Inhibitory
Agonist
Epinephrine,Isoprenaline,Salbutamol
Antagonist
Butoxamine
Effects of beta receptor block
Eye
Decrease in IOT by decrease in aqueous humor formation
Lungs
Bronchospasm(in asthmatics)
BV of skeletal
muscle
Unopposed alpha action
Vasoconstriction , Increase in PR
Uterus
No significant effect
2. Classify beta blockers with suitable example. To discuss
the pharmacology of various beta blockers.
Classification of -blockers
Nonselective -blockers
Propranolol (LA) (high lipid solubility)
Oxprenolol (ISA), Acebutolol (ISA), Timolol
Nonselective blockers with 1 blockade
Carvedilol
Labetolol (ISA + LA)
Selective 1-blockers
Metoprolol, Atenolol, Esmolol (short acting)
Selective 1-blocker with 2 agonist activity
Celiprolol
Cardiovascular effects of Beta Blockers
Heart:
FOC, HR, O2 consumption
AV conduction, Automaticity
Pure antagonists produce
At rest little or no change in HR, COP & BP
During exercise or excitement minimise or reduce the effect on CV
system (HR, COP & BP).
-blockers with ISA - HR at rest but during exercise.
-blockers Protect against arrhythmias.
Coronary vasoconstriction occurs. But, overall, ischaemia of
myocardium decreases as oxygen requirement is decreased. Increase
exercise tolerance. Hence, useful in angina pectoris & for
cardioprotective effect following MI.
Peripheral resistance increases.
In Hypertension - there is a gradual fall in BP over a period of few days
due to
in COP
in renin release from kidney
Central sympathetic activity
Advantages: No postural hypotension
Pulmonary effects of Beta Blockers
Healthy people only slight increase in bronchial resistance without
any effect on pulmonary function.
Asthmatics nonselective betablockers can cause life threatening
bronchoconstriction.
Beta1 selective (cardioselective) blockers are less likely to cause
respiratory problems in asthmatics. But, at higher doses even selective
beta blockers may cause bronchoconstriction. so caution is to be
exercised even with cardioselective beta blockers.
Renal: decrease renal blood flow (RBF) & may cause sodium and water
retention.
Eye: decrease tension by decreasing the production of aqueous humor.
Timolol is used topically in glaucoma treatment as it does not have
local anaesthetic action.
Advantages over parasympathomimetics in the treatment of
glaucoma: No significant action on pupil or accommodation.
Diabetes mellitus:
Mask symptoms of hypoglycemia such as palpitation, tremor, sweating
etc.
Non-selective Beta blockers delay recovery from hypoglycemia in
insulin dependent diabetics by inhibiting compensatory
neoglucogenesis & glycogenolysis.
Caution the patient about possible hypoglycemia & delayed recovery
from it. Cardioselective beta blockers are preferable if required.
Plasma lipids: May increase LDL & decrease HDL.
Absorption: orally absorbed.
Bioavailability: most of them, especially propranolol undergo extensive
first pass metabolism & have low bioavailability.
Hence, parenteral doses are relatively lower than oral doses.
Liver disease decreases first pass metabolism
Atenolol is longer acting.
Esmolol is fast & short acting.
Propranolol crosses BBB.
Adverse effect
CVS: Bradycardia, Heart block,
Congestive heart failure may be by removing the sympathetic drive
required to maintain COP. (Drugs with ISA may overcome this ADR).
CNS: sedation, fatigue, depression, bad dreams (propranolol cross into
CNS), sleep alterations
Sudden withdrawal can lead to rebound sensitivity to sympathetic
stimulation resulting in angina or MI.
ADR related to 2 blockade (1 selective drugs may be preferable)
RS: In asthmatics an attack may be precipitated by nonselective drugs.
Respiratory distress is seen in chronic bronchitis and emphysema.
Diabetes mellitus: Severe hypoglycemia & delayed recovery from
hypoglycemia.
Cold extremities
Contraindications: Bradycardia, unstable CHF, Bronchial asthma ,
depression
Uses
Hypertension Mild hypertension,
Synergistic with other antihypertensives
Ishaemic heart disease
Angina pectoris
Myocardial infarction
To limit the area of damage
To prevent cardiac rupture
In secondary prophylaxis by preventing arrhythmias & recurrent
infarction.
Clinically stable Congestive Heart Failure (CHF):
treatment with certain blockers with vasodilatory (1 block) action
eg. Carvedilol or those with ISA eg. Acebutolol to maintain a certain
degree of sympathetic drive to the heart prolongs survival .
Arrhythmias:
Ischaemia induced arrhythmias
Atrial arrhythmias (by increasing AV block)
Glaucoma - aqueous humor formation Timolol is used topically.
Why not propranolol?
Prophylaxis of Migraine
Benign essential tremor - tremor of peripheral origin (by 2- adrenergic
receptor block in skeletal muscle)
Hyperthyroidism immediate relief from signs & symptoms caused by
receptor over activity.
Anxiety states to control peripheral somatic symptoms of
sympathetic over activity such as palpitation & tremor
Prevention of stage fright
receptor blockers
Propranolol: Nonselective -blocker with local anaesthetic activity.
Undergoes extensive first pass metabolism. Crosses into CNS. ADR due
to 2 blockade are present.
Metoprolol: cardioselective beta blocker.
Atenolol: cardioselective, long acting beta blocker.
Esmolol: cardioselective and very short acting beta blocker
Mixed alpha and receptor blockers
Labetalol & Carvedilol
Competitive antagonist at both & -receptors
1 = 2 blockade > 1 blockade
Uses
Pheochromocytoma
hypertensive emergencies
1 blockade promotes vasodilation & hypotension
1 blockade reduces reflex & direct tachycardia.
Você também pode gostar
- Case Study 2 - Emotions & MoodsDocumento3 páginasCase Study 2 - Emotions & Moodsniwas100% (3)
- Plan - ANW-1-1Documento4 páginasPlan - ANW-1-1niwasAinda não há avaliações
- Translation Word To Tamil (Khasturi) 2Documento4 páginasTranslation Word To Tamil (Khasturi) 2niwasAinda não há avaliações
- Case Study 2 - Emotions & MoodsDocumento3 páginasCase Study 2 - Emotions & Moodsniwas100% (3)
- Shout For Help, To Alert Others: EclampsiaDocumento3 páginasShout For Help, To Alert Others: EclampsianiwasAinda não há avaliações
- Individual Assignment TemplateDocumento5 páginasIndividual Assignment TemplateniwasAinda não há avaliações
- Financial Management:: The Cost of CapitalDocumento94 páginasFinancial Management:: The Cost of CapitalSarah SaluquenAinda não há avaliações
- Patient Safety Awareness Course Test 2017Documento5 páginasPatient Safety Awareness Course Test 2017MochaLover0% (1)
- COVID-19 and The Great Reset: Briefing Note #28, October 21, 2020Documento3 páginasCOVID-19 and The Great Reset: Briefing Note #28, October 21, 2020niwasAinda não há avaliações
- Presentation Slides For CLO3 & CLO4 - Q1Documento4 páginasPresentation Slides For CLO3 & CLO4 - Q1niwasAinda não há avaliações
- Individual Assignment TemplateDocumento5 páginasIndividual Assignment TemplateniwasAinda não há avaliações
- O&G Off-Tag Assesment Logbook: Traces-Pdf-248732173Documento9 páginasO&G Off-Tag Assesment Logbook: Traces-Pdf-248732173niwasAinda não há avaliações
- Individual Assignment TemplateDocumento5 páginasIndividual Assignment TemplateniwasAinda não há avaliações
- Presentation Slides For CLO3 & CLO4 - Q1Documento4 páginasPresentation Slides For CLO3 & CLO4 - Q1niwasAinda não há avaliações
- Plan - BS: in Active Phase of LabourDocumento5 páginasPlan - BS: in Active Phase of LabourniwasAinda não há avaliações
- O&G OT Survival TipsDocumento2 páginasO&G OT Survival TipsniwasAinda não há avaliações
- Innovation in MarketingDocumento12 páginasInnovation in MarketingniwasAinda não há avaliações
- Innovation StrategyDocumento73 páginasInnovation StrategyniwasAinda não há avaliações
- Innovation StrategyDocumento73 páginasInnovation StrategyniwasAinda não há avaliações
- Innovation StrategyDocumento73 páginasInnovation StrategyniwasAinda não há avaliações
- Interpretation of Cardiotocograph Traces PDF 248732173Documento4 páginasInterpretation of Cardiotocograph Traces PDF 248732173Auliana FEAinda não há avaliações
- Innovation in MarketingDocumento12 páginasInnovation in MarketingniwasAinda não há avaliações
- Innovation in MarketingDocumento12 páginasInnovation in MarketingniwasAinda não há avaliações
- Carcinoma of PancreasDocumento24 páginasCarcinoma of PancreasniwasAinda não há avaliações
- Duodenal Ulcer - FinalDocumento42 páginasDuodenal Ulcer - FinalniwasAinda não há avaliações
- Emerging&Re-emerging Disease Y4Documento65 páginasEmerging&Re-emerging Disease Y4niwas100% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Brain Injury Fact SheetDocumento1 páginaBrain Injury Fact SheetAnonymous NUidh1TiuAinda não há avaliações
- Review 02Documento2 páginasReview 02Vicki KimAinda não há avaliações
- Individualized Neoantigen-Specific ImmunotherapyDocumento16 páginasIndividualized Neoantigen-Specific ImmunotherapyEhed AymazAinda não há avaliações
- G128 0066721 MSDSDocumento8 páginasG128 0066721 MSDSfiguev2208Ainda não há avaliações
- ACE2 Expression in Kidney and Testis May Cause Kidney and Testis Damage After 2019-nCoV InfectionDocumento16 páginasACE2 Expression in Kidney and Testis May Cause Kidney and Testis Damage After 2019-nCoV InfectionSY LodhiAinda não há avaliações
- We Are What... What We EatDocumento17 páginasWe Are What... What We EatАнастасия Пинькевич100% (1)
- Sonopuls 490 User ManualDocumento57 páginasSonopuls 490 User ManualMaryam BushraAinda não há avaliações
- Amended Modern Pharmacology Syllabus 051218Documento26 páginasAmended Modern Pharmacology Syllabus 051218harshad patelAinda não há avaliações
- Toxins: Use of Botulinum Toxin in Orofacial Clinical PracticeDocumento16 páginasToxins: Use of Botulinum Toxin in Orofacial Clinical PracticeAfiliado LendárioAinda não há avaliações
- Name_Naw Aung_La Mai Patient Focused ProceduresDocumento2 páginasName_Naw Aung_La Mai Patient Focused ProceduresEileenAinda não há avaliações
- Head Eyes: Head To Toe AssessmentDocumento2 páginasHead Eyes: Head To Toe AssessmentVijungco88% (8)
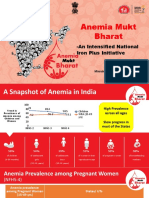
- Anemia Mukt Bharat: - An Intensified National Iron Plus InitiativeDocumento23 páginasAnemia Mukt Bharat: - An Intensified National Iron Plus InitiativeAnggun100% (1)
- Cholera: Key FactsDocumento9 páginasCholera: Key FactsDennis NjorogeAinda não há avaliações
- Njala University: Bo Campus-Kowama LocationDocumento32 páginasNjala University: Bo Campus-Kowama LocationALLIEU FB SACCOHAinda não há avaliações
- FJMCW Lahore MbbsDocumento9 páginasFJMCW Lahore MbbsRayan ArhamAinda não há avaliações
- Effects of Vasopressors On Cerebral Circulation.6Documento11 páginasEffects of Vasopressors On Cerebral Circulation.6diego morenoAinda não há avaliações
- Laporan Diet Pasca BedahDocumento13 páginasLaporan Diet Pasca BedahYuliza RosalinaAinda não há avaliações
- Zirconia Crowns Improve Patient SmileDocumento4 páginasZirconia Crowns Improve Patient SmileWiwin Nuril FalahAinda não há avaliações
- Need To Call To Confirm HoursDocumento35 páginasNeed To Call To Confirm HoursRadyusman RajagukgukAinda não há avaliações
- South African Family Practice ManualDocumento468 páginasSouth African Family Practice ManualMahiba Hussain96% (23)
- Article 2 - NZMJ Midface FracturesDocumento9 páginasArticle 2 - NZMJ Midface FracturesIndra D KristionoAinda não há avaliações
- Fournier's Gangrene: Yang Lu MS3 AUC School of MedicineDocumento15 páginasFournier's Gangrene: Yang Lu MS3 AUC School of MedicineYang JunAinda não há avaliações
- Manage High-Risk PregnanciesDocumento33 páginasManage High-Risk PregnanciesDakshayini MbAinda não há avaliações
- Halozyme Therapeutics, Inc. 2009 Investor Day PresentationDocumento88 páginasHalozyme Therapeutics, Inc. 2009 Investor Day Presentationsstrumello7395Ainda não há avaliações
- Management of The Urologic Sepsis SyndromeDocumento10 páginasManagement of The Urologic Sepsis SyndromeNur Syamsiah MAinda não há avaliações
- How China Is Fighting HIV/AIDS Stigma (Wang Longde)Documento22 páginasHow China Is Fighting HIV/AIDS Stigma (Wang Longde)National Press FoundationAinda não há avaliações
- Pre-Surgical Hand WashDocumento2 páginasPre-Surgical Hand WashRatna LamaAinda não há avaliações
- Preventing Diabetes in Pregnant WomenDocumento5 páginasPreventing Diabetes in Pregnant WomenJulina Br SembiringAinda não há avaliações
- Referral for dietitian assessment of swallowing riskDocumento72 páginasReferral for dietitian assessment of swallowing riskjykaAinda não há avaliações
- Final Exam Review - Bio 172Documento21 páginasFinal Exam Review - Bio 172Erin McElhaney QuirkAinda não há avaliações