Escolar Documentos
Profissional Documentos
Cultura Documentos
KJR 16 604
Enviado por
Winna Eka PTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
KJR 16 604
Enviado por
Winna Eka PDireitos autorais:
Formatos disponíveis
Original Article | Musculoskeletal Imaging
http://dx.doi.org/10.3348/kjr.2015.16.3.604
pISSN 1229-6929 eISSN 2005-8330
Korean J Radiol 2015;16(3):604-612
Cervical Interlaminar Epidural Steroid Injection for
Unilateral Cervical Radiculopathy: Comparison of Midline
and Paramedian Approaches for Efficacy
Ji Young Yoon, MD1, Jong Won Kwon, MD1, Young Cheol Yoon, MD1, Jongseok Lee, PhD2
1
Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul 135-710,
Korea; 2School of Business Administration, Hallym University, Chuncheon 200-702, Korea
Objective: The objective of this study was to compare the clinical outcomes of the cervical interlaminar epidural steroid
injection (CIESI) for unilateral radiculopathy by the midline or paramedian approaches and to determine the prognostic
factors of CIESI.
Materials and Methods: We retrospectively analyzed 182 patients who underwent CIESI from January 2009 to December
2012. Inclusion criteria were no previous spinal steroid injection, presence of a cross-sectional image, and presence of
follow-up records. Exclusion criteria were patients with bilateral cervical radiculopathy and/or dominant cervical axial pain,
combined peripheral neuropathy, and previous cervical spine surgery. Short-term clinical outcomes were evaluated at the
first follow-up after CIESI. We compared the clinical outcomes between the midline and paramedian approaches. Possible
prognostic factors for the outcome, such as age, gender, duration of radiculopathy, and cause of radiculopathy were also
analyzed.
Results: Cervical interlaminar epidural steroid injections were effective in 124 of 182 patients (68.1%) at the first followup. There was no significant difference in the clinical outcomes of CIESI, between midline (69.6%) and paramedian (63.7%)
approaches (p = 0.723). Cause of radiculopathy was the only significant factor affecting the efficacy of CIESI. Patients with
disc herniation had significantly better results than patients with neural foraminal stenosis (82.9% vs. 56.0%) (p < 0.001).
Conclusion: There is no significant difference in treatment efficacy between the midline and paramedian approaches in
CIESI, for unilateral radiculopathy. The cause of the radiculopathy is significantly associated with the treatment efficacy;
patients with disc herniation experience better pain relief than those with neural foraminal stenosis.
Index terms: Cervical spine; Epidural steroid injection; Radiculopathy; Spinal stenosis; Intervertebral disc
INTRODUCTION
Cervical interlaminar epidural steroid injection (CIESI)
Received September 22, 2014; accepted after revision February 23,
2015.
Corresponding author: Jong Won Kwon, MD, Department of
Radiology and Center for Imaging Science, Samsung Medical
Center, Sungkyunkwan University School of Medicine, 81 Irwon-ro,
Gangnam-gu, Seoul 135-710, Korea.
Tel: (822) 3410-2568 Fax: (822) 3410-0049
E-mail: jwjwkwon@gmail.com
This is an Open Access article distributed under the terms of
the Creative Commons Attribution Non-Commercial License
(http://creativecommons.org/licenses/by-nc/3.0) which permits
unrestricted non-commercial use, distribution, and reproduction in
any medium, provided the original work is properly cited.
604
is used for the conservative management of neck pain or
cervical radiculopathy. A systematic evaluation concluded
that CIESI significantly relieves chronic intractable pain
of cervical origin and also provides long-term relief (1, 2).
Compared with lumbar epidural steroid injections, CIESI
has additional technical challenges associated with more
narrowed epidural space and inconsistent loss of resistance
technique due to a high incidence of discontinuity in the
ligamentum flavum at the cervical region (3, 4).
There are two approach techniques used in CIESI: midline
and paramedian. The paramedian approach is sometimes
preferred, because it is believed to provide a better
therapeutic outcome due to the delivery of a relatively high
volume of injectate directly into the affected nerve root
Copyright 2015 The Korean Society of Radiology
Cervical Interlaminar ESI: Midline vs. Paramedian Approaches
sleeve; but this has not been verified in clinical trials.
The aim of this study was to compare the clinical outcome
of CIESI for unilateral radiculopathy, by using midline and
paramedian approaches, and to identify factors that are
predictive of therapeutic outcome after CIESI.
MATERIALS AND METHODS
Patients
This retrospective study was approved by our Institutional
Review Board and did not require informed consent.
From January 2009 to December 2012, 1157 CIESIs were
performed in our department. This investigation was
based on medical records, CT or MR images, and sets of
anteroposterior and lateral fluoroscopic views obtained
during CIESI.
The patients received CIESI by either a midline or
paramedian approach under fluoroscopic guidance. We
defined the midline approach as a confined needle tip
within the vertical lines of the spinous process in an
anteroposterior fluoroscopic view. The paramedian approach
was defined when the needle tip was located outside of the
vertical lines of the spinous process in an anteroposterior
fluoroscopic view. After the CIESIs were completed,
anteroposterior and lateral epidurogram were obtained to
document the extent and dispersal pattern of the injectate
within the epidural space. Patients were included in this
study, if the patterns of epidural contrast material flow
of the injectate were bilaterally symmetric with a midline
approach or ipsilateral in more than two thirds of the
areas of the injectate distributions with a paramedian
approach. Since we were only evaluating impact of the
injection on unilateral radiculopathy, we excluded the
cases with unintended consequences of midline approach
with asymmetric distribution or paramedian approach with
symmetric or contralateral distribution of the injectate on
unilateral radiculopathy.
Further inclusion criteria were patients with the following
conditions: 1) unilateral cervical radiculopathy; 2) first time
of receiving CIESI at our institute; 3) no previous (within
3 months) spinal steroid injection; 4) presence of a crosssectional image, such as CT or MR image, of the cervical
spine; and 5) presence of follow-up records after CIESI.
Exclusion criteria were as follows: 1) bilateral cervical
radiculopathy and/or dominant cervical axial pain; 2)
combined peripheral neuropathy; and 3) previous cervical
spine surgery. A total of 975 procedures were excluded
kjronline.org
Korean J Radiol 16(3), May/Jun 2015
for the following reasons: prevenient CIESIs in 539, other
spinal steroid injection within three months in 71, bilateral
cervical radiculopathy and/or dominant cervical axial pain
in 142, no cross-sectional image in 154, previous cervical
spine surgery in 11, asymmetric distribution of injectate
with midline approach in 27, and symmetric or contralateral
distribution of the injectate with paramedian approach in
31. Thus, 182 procedures of 182 patients were included in
this study.
Cervical axial pain consisted of pain or soreness in the
posterior neck muscles, with frequent radiation to the
occiput or shoulder regions that did not usually follow a
dermatomal distribution. Cervical radiculopathy manifested
as pain traveling down the neck and shoulder into the arm
of the patient, with radicular distribution (5).
Injection Technique
All CIESIs were performed under biplane fluoroscopic
guidance by two musculoskeletal radiologists experienced
in spinal intervention. The patient was placed in the
prone position. A pillow was placed under the patients
chests to elevate the shoulders, which helps to widen the
interlaminar space by flexing the spine. The skin of the
posterior neck was prepared and draped in sterile fashion.
A local anesthetic was administered with a 26-gauge
needle. The epidural space was entered between C4 and C5
to C7 and T1. A 22-gauge 12-cm spinal needle was then
advanced into the epidural space, with a midline (Fig. 1) or
paramedian (Fig. 2) approach. The side of the paramedian
approach was selected to match the symptomatic side.
When the needle was just posterior to the spinolaminar
line, where it had engaged the ligamentum flavum, test
injections of contrast material (Omnipaque 300 [iohexol,
300 mg I/mL]; Amersham Health, Princeton, NJ, USA) were
administered while the needle was being advanced until
the epidural space was entered. When the contrast material
in the needle was spreading in epidural space, we stopped
advancing the needle and confirmed that the needle tip
was in the epidural space with an additional test injection
of contrast agent. Anteroposterior and lateral epidurogram
were obtained to document the needle position and to
evaluate the extent of opacification. This was followed by
the injection of 1 mL of a suspension containing 40 mg
of triamcinolone acetonide (Tamceton [40 mg/mL]; Hanall
Pharmaceutical, Seoul, Korea) and 1.5 mL of preservativefree normal saline solution.
605
Yoon et al.
Image Analysis
All images were reviewed on a picture archiving and
communication system workstation monitored by two
musculoskeletal radiologists. The images were analyzed
by consensus between the two reviewers. The CT or MRI
images were assessed for the cause of radiculopathy: disc
A
B
Fig. 1. 68-year-old woman with pain in left shoulder and upper arm for duration of 5 months, due to neural foraminal stenosis.
Anteroposterior (A) and lateral (B) epidurogram showing midline approach at C56 level, and symmetric spreading of contrast media. One month
after cervical interlaminar epidural steroid injection, patients symptom was much improved with mild residual pain in left shoulder.
A
B
Fig. 2. 41-year-old man with left shoulder pain for duration of 3 months, due to neural foraminal stenosis.
Anteroposterior (A) and lateral (B) epidurogram showing left paramedian approach at C67 level, and asymmetric spreading of contrast media.
This patient had slightly reduced left shoulder pain and tingling sensation, 1 month after cervical interlaminar epidural steroid injection.
606
Korean J Radiol 16(3), May/Jun 2015
kjronline.org
Cervical Interlaminar ESI: Midline vs. Paramedian Approaches
herniation versus neural foraminal stenosis. Disc herniation
was defined as a localized displacement of disc material
beyond the limits of the intervertebral disc space (6).
Neural foraminal stenosis was defined as neural foraminal
narrowing with uncovertebral joint hypertrophy and facet
joint hypertrophy (5). The MR imaging characteristic of
a disc herniation was isointense to parent disc on T1weighted images, and iso- to increased signal intensity on
gradient-recall images. An osteophyte or uncovertebral spur
appeared as hypointense on T1- and T2-weighted images.
On CT examination, disc herniation was in intermediate
density similar to the parent disc, and osteophyte or
uncovertebral spur had bone density (7). Anteroposterior
and lateral fluoroscopic views obtained during CIESI
were reviewed for procedure-related problems, such as
penetration of the thecal sac or intravascular injection.
Review of Clinical Data
A retrospective review of patients medical records was
performed by an independent researcher. After CIESI,
first follow-up was done in the department of radiology,
neurosurgery, orthopedic surgery, or rehabilitation within 2
months. Pain intensity was quantified by a horizontal 100mm visual analog scale (VAS). The treatment outcome of
CIESI was also assessed by using five-point outcome scale
as follows: 0 (aggravated), 1 (the same as before), 2 (slightly
improved), 3 (much improved), and 4 (no residual pain).
Effective outcome was defined as at least 50% reduction
of VAS score or an outcome scale score of 3 or more after
CIESI. The researcher reviewed the medical records of the
patients for clinical data including age, gender, duration of
radiculopathy, and first follow-up period after CIESI.
For the patients with previously failed CIESI, we reviewed
the methods of additional treatments. If the patients had
been given an additional transforaminal epidural steroid
injection after ineffective CIESI, the effectiveness of
the transforaminal injection was also evaluated by the
same criteria as CIESI. For the patients with previously
successful CIESI, we checked the number of patients who
had been given an additional CIESI for the recurrence of
the symptoms within one year. Among all of the patients,
we counted the number of patients who had undergone
an operation after CIESI within one year and described
each number of operated patients according to injection
approaches.
kjronline.org
Korean J Radiol 16(3), May/Jun 2015
Statistical Analysis
An independent reviewer provided statistical analysis.
Factors such as age, gender, approach technique, duration
of radiculopathy, and cause of radiculopathy were evaluated
as possible prognostic factors of the treatment effect of
CIESI.
Continuous variables were summarized as medians and
ranges. Categorical variables were summarized by frequency
and percentage. The Mann-Whitney U exact test was used
for non-normal continuous variables, and Fishers exact
test was used for categorical variables. Univariate and
multivariate logistic regression analysis were used to
evaluate potential prognostic factors.
A Mantel-Haenszel test was also performed to control the
effects of other possible confounding variables on the effect
of CIESI, between the midline and paramedian approaches.
A post hoc power analysis was performed to calculate the
statistical power. A p value less than 0.05 was considered
statistically significant. Odds ratios are presented with a
95% confidence interval. Statistical analysis was performed
using the SPSS software package (version 20.0.; SPSS Inc.,
Chicago, IL, USA).
RESULTS
In 1157 CIESIs, a total of 182 procedures were included
in this study. The patients underwent CIESI with a midline
(n = 69) or paramedian (n = 113) approach. This study
included 97 males and 85 females; the median age was 54
years, with a range of 27 to 79 years. The median duration
of radiculopathy until the time of the procedure was 3
months, with a range of 3 days to 36 months. The median
period of the first follow-up was 20 days, with a range of
5 to 46 days. Disc herniation was found in 82 patients,
and neural foraminal stenosis was in 100 patients. Patients
with midline approach were significantly older than those
with paramedian approach (p = 0.006). No statistically
significant differences were found between the midline and
paramedian approach, with respect to gender, duration of
radiculopathy, cause of radiculopathy, and first follow-up
period. These results are summarized in Table 1.
Cervical interlaminar epidural steroid injections were
effective in 124 of 182 patients (68.1%), and it was
ineffective in 58 of 182 patients (31.9%). Five variables
were included in the univariate logistic regression analysis
for prognostic significance, as listed in Table 2. The only
factor significantly associated with clinical outcomes was
607
Yoon et al.
the cause of radiculopathy. Sixty eight of 82 patients
(82.9%) with disc herniation had effective pain relief,
and 56 of 100 patients (56.0%) with neural foraminal
stenosis had effective pain relief (p < 0.001). We found
no significant difference in the clinical outcomes between
midline (69.6%) and paramedian (63.7%) approach (p =
0.749), at short-term follow-up. Post hoc power analysis
revealed the power of the study to be 12.3% in detecting
a significant difference of clinical outcome between the
approaches.
After controlling for the cause of radiculopathy, there was
no significant association between the approach technique
and clinical outcome (p = 0.790). These results are shown
in Table 3. After controlling for gender, there was no
significant association between the approach technique and
clinical outcomes (p = 0.896).
When we controlled for predictive factors using
the multivariate logistic regression analysis, cause of
radiculopathy was the only significant factor related
to the treatment effect of CIESI (p < 0.001). CIESI was
significantly more efficacious for cervical radiculopathy in
disc herniation than in neural foraminal stenosis. There was
no significant association between the approach technique
and the treatment efficacy, after controlling for any other
variables examined (p = 0.723). Table 4 summarizes the
multivariate logistic regression analysis of the possible
predictive factors related to the efficacy of CIESI.
Among the 58 patients who had failed to improve after
Table 1. Baseline Characteristics of Midline and Paramedian Approaches
Parameter
Total (n = 182)
Age (years)*
Duration (months)*
Follow-up period (days)*
Gender
Male
Female
Cause
Disc herniation
NF stenosis
54 (2779)
3.0 (0.136.0)
20 (546)
97 (53.3)
85 (46.7)
Midline (n = 69)
57 (2779)
3.0 (0.136.0)
20 (545)
Approach
Paramedian (n = 113)
52 (2778)
3.0 (0.234.0)
20 (546)
33 (47.8)
36 (52.2)
P
0.006
0.378
0.922
0.285
64 (56.6)
49 (43.4)
0.761
82 (45.1)
100 (54.9)
30 (43.5)
39 (56.5)
52 (46.0)
61 (54.0)
*Values were presented as median with range in parentheses, Values were presented as number of patients with percentages in
parentheses, Statistical significances were tested by Mann-Whitney U exact test, Statistical significances were tested by Fishers exact
test. NF = neural foramen
Table 2. Univariate Logistic Regression Results for Predicting Clinical Outcome
Parameter
Approach
Gender
Cause
Category
Midline
Paramedian
Male
Female
Disc herniation
NF stenosis
Effective (n = 124)
48 (69.6%)
76 (63.7%)
65 (67.0%)
59 (69.4%)
68 (82.9%)
56 (56.0%)
Ineffective (n = 58)
21 (30.4%)
37 (32.7%)
32 (33.0%)
26 (30.6%)
14 (17.1%)
44 (44.0%)
Age (years)
Duration (months)
Exp (B)
1.113
1
0.895
1
3.816
1
0.992
0.954
95% CI for Exp (B)
P*
(0.583, 2.123)
0.749
(0.479, 1.674)
0.759
(1.899, 7.667)
< 0.001
(0.964, 1.021)
(0.910, 1.001)
0.586
0.053
*Statistical significances were tested by Fishers exact test. CI = confidence interval, Exp (B) = estimated odds ratio, NF = neural foramen
Table 3. Association between Technical Approach and Efficacy Stratified by Cause of Radiculopathy
Cause
Disc herniation
NF stenosis
Approach
Midline
Paramedian
Midline
Paramedian
Effective
27 (90.0%)
41 (78.8%)
21 (53.8%)
35 (57.4%)
Ineffective
3 (10.0%)
11 (21.2%)
18 (46.2%)
26 (42.6%)
P*
COR
0.859
0.790
0.237
0.837
*Statistical significances were tested by Fishers exact test, Mantel-Haenszel common odds ratio for approach (paramedian/midline),
Statistical significances were tested by Mantel-Haenszel test of conditional independence. NF = neural foramen
608
Korean J Radiol 16(3), May/Jun 2015
kjronline.org
Cervical Interlaminar ESI: Midline vs. Paramedian Approaches
Table 4. Multivariate Logistic Regression Results for Predicting Clinical Outcome
Parameter
Approach
Gender
Cause
Age (years)
Duration (months)
Constant
Category
Exp (B)
Midline
Male
Disc herniation
1.135
1.125
3.964
1.013
0.972
0.651
95% CI for Exp (B)
Lower
0.564
0.575
1.829
0.979
0.925
Upper
2.287
2.201
8.592
1.048
1.023
P
0.723
0.730
< 0.001
0.459
0.279
0.683
Estimated odds ratio (after controlling for all other independent variables). CI = confidence interval, Exp (B) = estimated odds ratio
a previous CIESI, 32 patients were given an additional
CIESI. Transforaminal epidural steroid injection was done
in 14 patients. Nine patients were only prescribed with
medications, and three patients underwent operation
without additional injection. An additional transforaminal
injection was effective in six (42.9%) patients of the 14
patients, and it was ineffective in eight (57.1%) patients.
Among the 124 patients with previously successful CIESI,
36 (29.0%) patients were given an additional CIESI for the
recurrence of the symptoms within one year. Among all of
the patients, operation was performed after the CIESI in
9 (4.9%) out of 182 patients: 3 (4.3%) out of 69 patients
with midline approach and 6 (5.3%) out of 113 patients
with paramedian approach.
DISCUSSION
In the present study, effective outcome was achieved
in 68.1% of patients with CIESI, at short-term follow-up.
Several other studies have reported with excellent clinical
outcomes in 63% to 83% of cases with cervical epidural
steroid injection (8-14). To the best of our knowledge, no
study has compared the clinical effects of the midline and
paramedian approaches. According to our study, the efficacy
of CIESI was 69.6% in the midline approach versus 63.7%
in the paramedian approach, which were not significantly
different (p = 0.723).
The epidural space is a space inside of the spinal canal
but outside of the dural sac. It extends from the foramen
magnum to the sacral hiatus. The space contains adipose
tissue, loose areolar tissue, arteries, lymphatics, venous
plexus in abundance, and spinal nerve roots. It is limited
posteriorly by the vertebral laminae and the ligamentum
flavum, and limited anteriorly by the posterior longitudinal
ligament. The lateral border is the pedicle and intervertebral
foramen. The epidural space is anatomically subdivided into
anterior and posterior compartments. The anterior epidural
kjronline.org
Korean J Radiol 16(3), May/Jun 2015
space is a fairly well-defined space anteriorly limited by
the concavity of the vertebral body, intervertebral disc,
and posterior longitudinal ligament, and posteriorly
limited by the thecal sac. The posterior epidural space is
bordered anteriorly by the thecal sac and posteriorly by the
ligamentum flavum and the vertebral laminae (3, 15, 16).
In CIESI, a needle is inserted into the posterior epidural
space. The posterior epidural space is triangularly shaped
in transverse sections, with its widest part lying posteriorly
in the median sagittal plane. The posterior epidural space
is filled by a fat pad that becomes narrow towards its
lateral margin, and the cervical epidural space is extremely
narrow. Above C7T1 level, no posterior epidural space is
evident. A bigger problem with the paramedian approach
is that there may not be an approachable epidural space
and the intradural space may be more easily entered, which
is completely undesirable (3). Thus, midline approaches
are considered to be safer than paramedian approaches.
In addition, inserting the needle, using a paramedian
approach, away from the midline increases the likelihood of
facet joint puncture.
When confirming proper needle placement for interlaminar
procedures, the spinolaminar line is used as an anatomic
landmark. To avoid dural and cord puncture, the needle
should not be inserted beyond the spinolaminar line (16).
In the paramedian approach, the spinolaminar line is a
less reliable anatomic landmark for entering the posterior
epidural space. When the needle tip is not midline, it
will need to be advanced more ventrally beyond the
spinolaminar line, due to the cylindrical shape of the thecal
sac (Fig. 3).
The minor complications of CIESI include increased
axial pain, non-positional headache, facial flushing, and
vasovagal episodes. The major complications include
permanent spinal cord injury, epidural hematoma or abscess,
dural puncture, and post-dural puncture headache (17).
In our series, no symptomatic procedural complications
609
Yoon et al.
A
B
Fig. 3. 60-year-old woman with right shoulder pain for duration of 4 months, due to neural foraminal stenosis.
Anteroposterior (A) and lateral (B) epidurogram showing right paramedian approach at C67 level, and asymmetric spreading of contrast media.
Needle tip is located more ventrally beyond spinolaminar line.
occurred during or after treatment.
In previous studies, investigators have reported with
some contradicting results regarding the predictive factors
of the efficacy in cervical epidural steroid injection. Kwon
et al. (10) showed that the patients with disc herniations
showed better response to CIESIs than the patients with
spinal stenoses; and Rivest et al. (18) reported with
a similar result while discussing about lumbar spine
pathologies. However, Fish et al. (19) reported that central
canal stenosis is a significant predictor for a better response
to CIESI. Ferrante et al. (20) also reported that a radiologic
diagnosis of spondylosis or spinal stenosis was associated
with good pain relief. Lee et al. (21) showed that the
causes of radiculopathy did not make any differences in
the clinical outcomes of cervical paramedian interlaminar
epidural steroid injections. In our study, we did not evaluate
the difference in efficacy of the approach techniques on
patients with central canal stenosis. We did find that CIESI
was significantly more efficacious in patients with disc
herniation, than in those with neural foraminal stenosis.
This is probably due to the antigenic effect of nucleus
pulposus and local immune response. Clinical and radiologic
studies suggest that multiple inflammatory mediators are
associated with the pathogenesis of radicular pain due to
610
nucleus pulposus material (22). Anti-inflammatory effects
of steroids had been described many years ago (23), and
current studies have reported the anti-inflammatory effect
of local anesthetics on cells of the immune system as well
as other cells (24).
In addition, there are different research results regarding
the influence of age. In transforaminal approach, Lin et al.
(9) found that when comparing the patients of 50 years
of age or below to males older than 50 years of age, the
patients older than 50 years had more favorable outcomes.
Ferrante et al. (20) also reported that older patients had
significantly better outcomes after cervical epidural steroid
injection. Other studies, however, have suggested that age
was not a significant predictor of an improved outcome in
transforaminal approach (25) and interlaminar approach
(10). In this study, no statistically significant difference
was found in the efficacy of CIESI with respect to the age
of the patients.
Other studies have also evaluated the prognostic factors
for cervical epidural injections. Lee et al. (26) concluded
that the significant factors predisposing failure of epidural
steroid injection were intensity of symptoms and a previous
episode of cervical radiculopathy. Lee et al. (25) reported
that previous operation was a poor outcome predictor in
Korean J Radiol 16(3), May/Jun 2015
kjronline.org
Cervical Interlaminar ESI: Midline vs. Paramedian Approaches
transforaminal approach. In this study, we did not evaluate
previous episodes of cervical radiculopathy and excluded
the patients with previous cervical operation.
There are some limitations to our study. First, it
was a retrospective study without a uniform follow-up
schedule. Second, there was a lack of data on the longterm pain relief. The results of this study may be helpful
when counseling patients for short-term outcomes. Third,
treatment effect was measured only by the subjective relief
of symptom; there was no objective functional outcome
measurement. Fourth, our case definitions for the causes
of radiculopathy, disc herniation, and neural foraminal
stenosis might have resulted in some misclassifications;
but, this is unlikely to introduce biases. Fifth, we excluded
the cases of midline approach with asymmetric distribution
or paramedian approach with symmetric or contralateral
distribution of the injectate, which could have either
exaggerated or minimized the impact of either approach in
CIESI. In addition, due to the low number of patients, the
study was insufficiently powered to detect a statistically
significant difference.
We conclude that CIESI with midline or paramedian
approach shows similar results in terms of the shortterm outcome; therefore, the midline approach may be
recommended, especially for the beginners who have
difficulty in deciding the proper position for the paramedian
approach. CIESI is significantly more efficacious in disc
herniation than in neural foraminal stenosis.
REFERENCES
1. Benyamin RM, Singh V, Parr AT, Conn A, Diwan S, Abdi S.
Systematic review of the effectiveness of cervical epidurals
in the management of chronic neck pain. Pain Physician
2009;12:137-157
2. Diwan S, Manchikanti L, Benyamin RM, Bryce DA, Geffert S,
Hameed H, et al. Effectiveness of cervical epidural injections
in the management of chronic neck and upper extremity pain.
Pain Physician 2012;15:E405-E434
3. Hogan QH. Epidural anatomy examined by cryomicrotome
section. Influence of age, vertebral level, and disease. Reg
Anesth 1996;21:395-406
4. Lirk P, Kolbitsch C, Putz G, Colvin J, Colvin HP, Lorenz I, et al.
Cervical and high thoracic ligamentum flavum frequently fails
to fuse in the midline. Anesthesiology 2003;99:1387-1390
5. Abbed KM, Coumans JV. Cervical radiculopathy:
pathophysiology, presentation, and clinical evaluation.
Neurosurgery 2007;60(1 Supp1 1):S28-S34
6. Fardon DF, Milette PC; Combined Task Forces of the North
kjronline.org
Korean J Radiol 16(3), May/Jun 2015
American Spine Society, American Society of Spine Radiology,
and American Society of Neuroradiology. Nomenclature and
classification of lumbar disc pathology. Recommendations
of the Combined task Forces of the North American
Spine Society, American Society of Spine Radiology, and
American Society of Neuroradiology. Spine (Phila Pa 1976)
2001;26:E93-E113
7. Czervionke LF, Fenton DS. Imaging painful spine disorders, 1st
ed. Philadelphia: Saunders, 2011:180-187
8. Castagnera L, Maurette P, Pointillart V, Vital JM, Erny P,
Sngas J. Long-term results of cervical epidural steroid
injection with and without morphine in chronic cervical
radicular pain. Pain 1994;58:239-243
9. Lin EL, Lieu V, Halevi L, Shamie AN, Wang JC. Cervical epidural
steroid injections for symptomatic disc herniations. J Spinal
Disord Tech 2006;19:183-186
10. Kwon JW, Lee JW, Kim SH, Choi JY, Yeom JS, Kim HJ, et al.
Cervical interlaminar epidural steroid injection for neck pain
and cervical radiculopathy: effect and prognostic factors.
Skeletal Radiol 2007;36:431-436
11. Strub WM, Brown TA, Ying J, Hoffmann M, Ernst RJ, Bulas RV.
Translaminar cervical epidural steroid injection: short-term
results and factors influencing outcome. J Vasc Interv Radiol
2007;18:1151-1155
12. Manchikanti L, Cash KA, Pampati V, Wargo BW, Malla Y. The
effectiveness of fluoroscopic cervical interlaminar epidural
injections in managing chronic cervical disc herniation and
radiculitis: preliminary results of a randomized, double-blind,
controlled trial. Pain Physician 2010;13:223-236
13. Manchikanti L, Cash KA, Pampati V, Wargo BW, Malla Y.
Management of chronic pain of cervical disc herniation and
radiculitis with fluoroscopic cervical interlaminar epidural
injections. Int J Med Sci 2012;9:424-434
14. Manchikanti L, Malla Y, Cash KA, McManus CD, Pampati V.
Fluoroscopic cervical interlaminar epidural injections in
managing chronic pain of cervical postsurgery syndrome:
preliminary results of a randomized, double-blind, active
control trial. Pain Physician 2012;15:13-25
15. Douglas S, Leo FC. Image-guided spine intervention, 1st ed.
Philadelphia: Saunders, 2002:99-126
16. Huston CW. Cervical epidural steroid injections in the
management of cervical radiculitis: interlaminar versus
transforaminal. A review. Curr Rev Musculoskelet Med
2009;2:30-42
17. Abbasi A, Malhotra G, Malanga G, Elovic EP, Kahn S.
Complications of interlaminar cervical epidural steroid
injections: a review of the literature. Spine (Phila Pa 1976)
2007;32:2144-2151
18. Rivest C, Katz JN, Ferrante FM, Jamison RN. Effects of
epidural steroid injection on pain due to lumbar spinal
stenosis or herniated disks: a prospective study. Arthritis Care
Res 1998;11:291-297
19. Fish DE, Kobayashi HW, Chang TL, Pham Q. MRI prediction
of therapeutic response to epidural steroid injection in
patients with cervical radiculopathy. Am J Phys Med Rehabil
611
Yoon et al.
2009;88:239-246
20. Ferrante FM, Wilson SP, Iacobo C, Orav EJ, Rocco AG, Lipson
S. Clinical classification as a predictor of therapeutic outcome
after cervical epidural steroid injection. Spine (Phila Pa 1976)
1993;18:730-736
21. Lee JW, Hwang SY, Lee GY, Lee E, Kang HS. Fluoroscopic
cervical paramidline interlaminar epidural steroid injections
for cervical radiculopathy: effectiveness and outcome
predictors. Skeletal Radiol 2014;43:933-938
22. Goupille P, Jayson MI, Valat JP, Freemont AJ. The role of
inflammation in disk herniation-associated radiculopathy.
Semin Arthritis Rheum 1998;28:60-71
23. Flower RJ, Blackwell GJ. Anti-inflammatory steroids induce
biosynthesis of a phospholipase A2 inhibitor which prevents
612
prostaglandin generation. Nature 1979;278:456-459
24. Cassuto J, Sinclair R, Bonderovic M. Anti-inflammatory
properties of local anesthetics and their present and potential
clinical implications. Acta Anaesthesiol Scand 2006;50:265282
25. Lee JW, Park KW, Chung SK, Yeom JS, Kim KJ, Kim HJ, et
al. Cervical transforaminal epidural steroid injection for the
management of cervical radiculopathy: a comparative study
of particulate versus non-particulate steroids. Skeletal Radiol
2009;38:1077-1082
26. Lee SH, Kim KT, Kim DH, Lee BJ, Son ES, Kwack YH. Clinical
outcomes of cervical radiculopathy following epidural steroid
injection: a prospective study with follow-up for more than 2
years. Spine (Phila Pa 1976) 2012;37:1041-1047
Korean J Radiol 16(3), May/Jun 2015
kjronline.org
Você também pode gostar
- How to Perform Ultrasonography in EndometriosisNo EverandHow to Perform Ultrasonography in EndometriosisStefano GuerrieroAinda não há avaliações
- Percutaneous Endoscopic Lumbar DiscectomyDocumento9 páginasPercutaneous Endoscopic Lumbar DiscectomyAshish KallaAinda não há avaliações
- Interventional Radiology of the Spine: Image-Guided Pain TherapyNo EverandInterventional Radiology of the Spine: Image-Guided Pain TherapyJ. Kevin McGrawAinda não há avaliações
- Figure of 8Documento6 páginasFigure of 8Muhammad Ichsan PrasetyaAinda não há avaliações
- X-Ray: Correlation Study Between Cervical X-Ray Sagittal Parameters and Chuna Posture Analysis ResultsDocumento13 páginasX-Ray: Correlation Study Between Cervical X-Ray Sagittal Parameters and Chuna Posture Analysis Resultskang soon cheolAinda não há avaliações
- Jkns 2018 0153Documento7 páginasJkns 2018 0153ioAinda não há avaliações
- Lumbal Spinal Stenosis ODI ScoreDocumento10 páginasLumbal Spinal Stenosis ODI ScoreTusan SidhartaAinda não há avaliações
- Surgical Outcomes of Posterior Spinal Fusion Alone Using Cervical Pedicle ScrewDocumento26 páginasSurgical Outcomes of Posterior Spinal Fusion Alone Using Cervical Pedicle ScrewprototyposAinda não há avaliações
- Comparative Study of Intra-Capsular Fracture Neck of Femur Treated by Two Dif-Ferent Methods of Screw FixationDocumento7 páginasComparative Study of Intra-Capsular Fracture Neck of Femur Treated by Two Dif-Ferent Methods of Screw FixationnjmdrAinda não há avaliações
- March Case StudyDocumento9 páginasMarch Case Studyapi-247959633Ainda não há avaliações
- Lateral Oblique Superior To Lateral View CESI 2015Documento14 páginasLateral Oblique Superior To Lateral View CESI 2015Michael HuntAinda não há avaliações
- Quantitative Assessment of Inferior Oblique Muscle Overaction Using Photographs of The Cardinal Positions of GazeDocumento9 páginasQuantitative Assessment of Inferior Oblique Muscle Overaction Using Photographs of The Cardinal Positions of GazenysAinda não há avaliações
- Assessment of Follow-Up Sonography and Clinical ImDocumento6 páginasAssessment of Follow-Up Sonography and Clinical ImTelman ResidovAinda não há avaliações
- Different Episiotomy TechniquesDocumento8 páginasDifferent Episiotomy TechniquesMikeAinda não há avaliações
- Ultrasonics Sonochemistry: Jae-Seong Lee, Gi-Youn Hong, Byung-Joon Park, Tea-Eung KimDocumento6 páginasUltrasonics Sonochemistry: Jae-Seong Lee, Gi-Youn Hong, Byung-Joon Park, Tea-Eung KimTantonio Tri PutraAinda não há avaliações
- Diagnostic Values of Tests For Acromioclavicular Joint PainDocumento6 páginasDiagnostic Values of Tests For Acromioclavicular Joint Painarum_negariAinda não há avaliações
- JCM 10 00913Documento11 páginasJCM 10 00913Delivery ServiceAinda não há avaliações
- Choi 2021Documento12 páginasChoi 2021paul_androideAinda não há avaliações
- Ultrasoud Guidance For Lumbar PunctureDocumento12 páginasUltrasoud Guidance For Lumbar PunctureDavid Avellaneda TalledoAinda não há avaliações
- ChinosDocumento10 páginasChinosGilberto González LópezAinda não há avaliações
- Cao Et Al. 2018Documento10 páginasCao Et Al. 2018Fábio LanferdiniAinda não há avaliações
- Apm 20072Documento7 páginasApm 20072ida wahyuni mapsanAinda não há avaliações
- Biswas2014 PDFDocumento7 páginasBiswas2014 PDFDhruv MahajanAinda não há avaliações
- ptrs009 03 03 PDFDocumento6 páginasptrs009 03 03 PDFGusti Ayu KrisnayantiAinda não há avaliações
- Changes in The Sagittal Cranio-Cervical Posture Following A 12-Week Intervention Using A Simple Spinal Traction DeviceDocumento18 páginasChanges in The Sagittal Cranio-Cervical Posture Following A 12-Week Intervention Using A Simple Spinal Traction Device박진영Ainda não há avaliações
- Extracorporeal Shock Wave Therapy VersusDocumento7 páginasExtracorporeal Shock Wave Therapy VersusGiannis SaramantosAinda não há avaliações
- JurnalDocumento4 páginasJurnalBIntangsinagaAinda não há avaliações
- 2022 25 E1351 E1366Documento16 páginas2022 25 E1351 E1366Ricardo PietrobonAinda não há avaliações
- Pinhole Versus Parallel-Hole Collimators For Parathyroid Imaging: An Intraindividual ComparisonDocumento6 páginasPinhole Versus Parallel-Hole Collimators For Parathyroid Imaging: An Intraindividual ComparisonDaniela BrancoAinda não há avaliações
- JURNALDocumento6 páginasJURNALPutu erwanAinda não há avaliações
- Comprehensive Ultrasound Diagnosis For Intraductal Spread of Primary Breast CancerDocumento10 páginasComprehensive Ultrasound Diagnosis For Intraductal Spread of Primary Breast CancerferdiAinda não há avaliações
- AsianJNeurosurg104272-2469213 065132 PDFDocumento4 páginasAsianJNeurosurg104272-2469213 065132 PDFSucipto HartonoAinda não há avaliações
- Abstracts of The 2018 AANS/CNS Joint Section On Disorders of The Spine and Peripheral Nerves Annual MeetingDocumento109 páginasAbstracts of The 2018 AANS/CNS Joint Section On Disorders of The Spine and Peripheral Nerves Annual MeetingEka Wahyu HerdiyantiAinda não há avaliações
- J Neurol Sci (Turk)Documento9 páginasJ Neurol Sci (Turk)nulaeli Siti AAinda não há avaliações
- Utilityofimage-Guidance Infrontalsinussurgery: Gretchen M. Oakley,, Henry P. Barham,, Richard J. HarveyDocumento14 páginasUtilityofimage-Guidance Infrontalsinussurgery: Gretchen M. Oakley,, Henry P. Barham,, Richard J. HarveyJuan Pablo Mejia BarbosaAinda não há avaliações
- Clinical Trials in BrainDocumento16 páginasClinical Trials in Brainmadhukar1978Ainda não há avaliações
- Anterior Versus Posterior Surgical Approach For Lumbosacral TuberculosisDocumento9 páginasAnterior Versus Posterior Surgical Approach For Lumbosacral TuberculosisI Made Dhita PriantharaAinda não há avaliações
- Alesina Et Al., 2021Documento9 páginasAlesina Et Al., 2021NyomantrianaAinda não há avaliações
- PNC 1Documento5 páginasPNC 1Magu LaraAinda não há avaliações
- FocusDocumento9 páginasFocusDaniel FélizAinda não há avaliações
- Poster PapersDocumento262 páginasPoster PapersLeonardo RodríguezAinda não há avaliações
- Draconaki Et Al. (2011) - Efficacy of Ultrasound-Guided Steroid Injections For Pain Management of Midfoot Joint Degenerative DiseaseDocumento7 páginasDraconaki Et Al. (2011) - Efficacy of Ultrasound-Guided Steroid Injections For Pain Management of Midfoot Joint Degenerative DiseasextraqrkyAinda não há avaliações
- Assessing Pain Relief Following Medical and Surgical Interventions For Lumbar Disc HerniationDocumento4 páginasAssessing Pain Relief Following Medical and Surgical Interventions For Lumbar Disc HerniationInternational Journal of Innovative Science and Research TechnologyAinda não há avaliações
- Vertical Expandable Prosthetic Titanium Rib Device Insertion: Does It Improve Pulmonary Function?Documento4 páginasVertical Expandable Prosthetic Titanium Rib Device Insertion: Does It Improve Pulmonary Function?hayputriAinda não há avaliações
- Nice 1stDocumento6 páginasNice 1staldiAinda não há avaliações
- Uterine Artery Embolization FoDocumento4 páginasUterine Artery Embolization FoAlexandre Campos Moraes AmatoAinda não há avaliações
- 2015 6 jns1546Documento7 páginas2015 6 jns1546ROHITAinda não há avaliações
- Comparative Analysis of Clinical Outcomes of Open Appendectomy and Laparoscopic AppendectomyDocumento6 páginasComparative Analysis of Clinical Outcomes of Open Appendectomy and Laparoscopic AppendectomyIJRASETPublicationsAinda não há avaliações
- Structured Versus Narrative Reporting of Pelvic MRI in Perianal Fistulizing Disease: Impact On Clarity, Completeness, and Surgical PlanningDocumento10 páginasStructured Versus Narrative Reporting of Pelvic MRI in Perianal Fistulizing Disease: Impact On Clarity, Completeness, and Surgical PlanningqrscentralAinda não há avaliações
- New England Journal Medicine: The ofDocumento11 páginasNew England Journal Medicine: The ofnaufal12345Ainda não há avaliações
- Early Surgery Compared To Nonoperative ManagementDocumento11 páginasEarly Surgery Compared To Nonoperative ManagementantoniowidiaAinda não há avaliações
- RNM Dinamica 2Documento6 páginasRNM Dinamica 2Alfredo GuiroyAinda não há avaliações
- Park 2014Documento7 páginasPark 2014Nurfitrianti ArfahAinda não há avaliações
- Aksha Poster AbstractDocumento14 páginasAksha Poster Abstractडॉ यश तलेराAinda não há avaliações
- 2022 Article 3254Documento8 páginas2022 Article 3254Mendoza Vázquez MarcoAinda não há avaliações
- 16 Van Leerdam Et Al J Hand Surg Eur Vol. 2017 Jun 42 5 501 506 AAMDocumento13 páginas16 Van Leerdam Et Al J Hand Surg Eur Vol. 2017 Jun 42 5 501 506 AAMChristopher Freddy Bermeo RiveraAinda não há avaliações
- 2014 Rehabilitación Después de Una Cirugía Por Estenosis Espinal Lumbar. RevisiónDocumento12 páginas2014 Rehabilitación Después de Una Cirugía Por Estenosis Espinal Lumbar. Revisiónjuan pabloAinda não há avaliações
- Transforaminal Debridement With A Posterior Only.62Documento6 páginasTransforaminal Debridement With A Posterior Only.62Jean Marcel Castelo VegaAinda não há avaliações
- 1 UsDocumento7 páginas1 UsJenny VibsAinda não há avaliações
- Cervical Epidural Pressure Measurement: Comparison in The Prone and Sitting PositionsDocumento6 páginasCervical Epidural Pressure Measurement: Comparison in The Prone and Sitting PositionsGabriel PaezAinda não há avaliações
- Daftar PustakaDocumento2 páginasDaftar PustakaWinna Eka PAinda não há avaliações
- Poster Cuci Tangan 2Documento1 páginaPoster Cuci Tangan 2Winna Eka PAinda não há avaliações
- Management of Persistent Vaginitis .99281 PDFDocumento12 páginasManagement of Persistent Vaginitis .99281 PDFWinna Eka PAinda não há avaliações
- Vol 3 No 1 2013 - 25Documento6 páginasVol 3 No 1 2013 - 25Winna Eka PAinda não há avaliações
- Committee Opinion No 611 Method For Estimating.43Documento4 páginasCommittee Opinion No 611 Method For Estimating.43Winna Eka PAinda não há avaliações
- Correction: VOL. 124, NO. 5, NOVEMBER 2014 Obstetrics & Gynecology 1035Documento1 páginaCorrection: VOL. 124, NO. 5, NOVEMBER 2014 Obstetrics & Gynecology 1035Winna Eka PAinda não há avaliações
- Ondansetron Compared With Doxylamine And.13Documento8 páginasOndansetron Compared With Doxylamine And.13Satria Panca KartaAinda não há avaliações
- Management of Persistent Vaginitis .99281 PDFDocumento12 páginasManagement of Persistent Vaginitis .99281 PDFWinna Eka PAinda não há avaliações
- Pi Is 0020729213005055Documento4 páginasPi Is 0020729213005055Winna Eka PAinda não há avaliações
- Milieu TherapyDocumento2 páginasMilieu Therapysivagiri.pAinda não há avaliações
- RMDocumento10 páginasRMdanielAinda não há avaliações
- Lotus Home Care Induction Manual © 2012 Inspire Education April 2012Documento20 páginasLotus Home Care Induction Manual © 2012 Inspire Education April 2012Nhung NguyenAinda não há avaliações
- Homeopathic Materia Medica by Farrington Causticum (Caust) : Lecture Lxxi Lecture LxxiiDocumento7 páginasHomeopathic Materia Medica by Farrington Causticum (Caust) : Lecture Lxxi Lecture LxxiimyoxusAinda não há avaliações
- Congenital DiseaseDocumento39 páginasCongenital DiseaseRavi SharmaAinda não há avaliações
- Latecia 2023 ResumeDocumento6 páginasLatecia 2023 Resumeapi-643213493Ainda não há avaliações
- Post Op Management Following Surgery For Rectal ProlapseDocumento2 páginasPost Op Management Following Surgery For Rectal ProlapseChris NewallAinda não há avaliações
- Anti Neoplastic AgentsDocumento116 páginasAnti Neoplastic AgentsAbii KetiAinda não há avaliações
- Alcohol and Drug Abuse Flow ChartDocumento1 páginaAlcohol and Drug Abuse Flow Chartboen jaymeAinda não há avaliações
- Basic EKG Dysrhythmia IdentificationDocumento40 páginasBasic EKG Dysrhythmia IdentificationIlda Dhe Devis Spaho100% (1)
- IntegumentaryDocumento1 páginaIntegumentaryCoffee CojjeeAinda não há avaliações
- CSDT GMDDocumento40 páginasCSDT GMDSyafiqAinda não há avaliações
- Guia Nice CesareaDocumento7 páginasGuia Nice Cesarealorena brachoAinda não há avaliações
- Dialysis Products Catalog PDFDocumento52 páginasDialysis Products Catalog PDFAFRIANSYAHAinda não há avaliações
- Quality by Design For ANDAs - MR TabletsDocumento161 páginasQuality by Design For ANDAs - MR TabletsShilpa Kotian100% (1)
- Fundamentals of Rheumatoid Arthritis and Various Homoeopathic Trials in Patients of Rheumatoid Arthritis: An UpdateDocumento6 páginasFundamentals of Rheumatoid Arthritis and Various Homoeopathic Trials in Patients of Rheumatoid Arthritis: An UpdateHomoeopathic PulseAinda não há avaliações
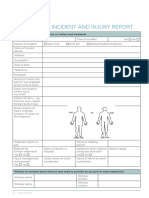
- Whs Form 10: Incident and Injury Report: 22 Safework NSWDocumento2 páginasWhs Form 10: Incident and Injury Report: 22 Safework NSWalexAinda não há avaliações
- Thyriodectomy BrochureDocumento2 páginasThyriodectomy BrochureHeedahAinda não há avaliações
- JCI-Sentinel Event AlertDocumento3 páginasJCI-Sentinel Event AlertDewi Ratna SariAinda não há avaliações
- 14 WartsprotocolDocumento9 páginas14 WartsprotocolLakshmi Deepak IAinda não há avaliações
- SyllabusDocumento4 páginasSyllabusMădă IorgaAinda não há avaliações
- Veris TOHDocumento35 páginasVeris TOHtofssbiAinda não há avaliações
- List-European-Union-Reference-Dates-Frequency-Submission-Periodic-Safety-Update-Reports - en (2) UpdatedDocumento40 páginasList-European-Union-Reference-Dates-Frequency-Submission-Periodic-Safety-Update-Reports - en (2) UpdatedMai MostafaAinda não há avaliações
- Renal Learning OutcomesDocumento11 páginasRenal Learning OutcomesBhuwan TandonAinda não há avaliações
- Practice and Opinion Towards Disposal of Unused Medication in KuwaitDocumento6 páginasPractice and Opinion Towards Disposal of Unused Medication in KuwaitAmirul AdamAinda não há avaliações
- Kleihauer TestDocumento3 páginasKleihauer Testteo2211Ainda não há avaliações
- Ebj M3 Rle24Documento6 páginasEbj M3 Rle24Ayen PaloAinda não há avaliações
- Iron Deficiency Anemia 2012Documento41 páginasIron Deficiency Anemia 2012peanadssAinda não há avaliações
- Lactose Intolerance: Diano, Gabriella Hilde Fanged, Paula Mandy Marrero, Xandra 9-KryptonDocumento15 páginasLactose Intolerance: Diano, Gabriella Hilde Fanged, Paula Mandy Marrero, Xandra 9-KryptonArrianne AcopAinda não há avaliações
- "Understanding Vitamins For Poultry": Chicks With Vitamin DeficienciesDocumento4 páginas"Understanding Vitamins For Poultry": Chicks With Vitamin DeficienciesGrowel Agrovet Private Limited.Ainda não há avaliações
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNo EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNota: 5 de 5 estrelas5/5 (3)
- The Age of Magical Overthinking: Notes on Modern IrrationalityNo EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityNota: 4 de 5 estrelas4/5 (30)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNota: 2 de 5 estrelas2/5 (1)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)No EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Nota: 3 de 5 estrelas3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNo EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNota: 4 de 5 estrelas4/5 (404)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNo EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNota: 4 de 5 estrelas4/5 (4)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNo EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNota: 4.5 de 5 estrelas4.5/5 (42)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNo EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNota: 5 de 5 estrelas5/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsAinda não há avaliações
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNo EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNota: 5 de 5 estrelas5/5 (81)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsNo EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsNota: 4.5 de 5 estrelas4.5/5 (170)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNo EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNota: 4.5 de 5 estrelas4.5/5 (266)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.No EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Nota: 4.5 de 5 estrelas4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityNo EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityNota: 4 de 5 estrelas4/5 (5)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisNo EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisNota: 5 de 5 estrelas5/5 (8)
- Empath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainNo EverandEmpath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainNota: 4 de 5 estrelas4/5 (95)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeNo EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeNota: 4.5 de 5 estrelas4.5/5 (253)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessNo EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessNota: 4.5 de 5 estrelas4.5/5 (328)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedNo EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedNota: 4 de 5 estrelas4/5 (61)
- The Obesity Code: Unlocking the Secrets of Weight LossNo EverandThe Obesity Code: Unlocking the Secrets of Weight LossNota: 4 de 5 estrelas4/5 (6)
- The Marshmallow Test: Mastering Self-ControlNo EverandThe Marshmallow Test: Mastering Self-ControlNota: 4.5 de 5 estrelas4.5/5 (60)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesNo EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesNota: 4.5 de 5 estrelas4.5/5 (1412)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryNo EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryNota: 4 de 5 estrelas4/5 (45)