Escolar Documentos
Profissional Documentos
Cultura Documentos
Biochem Disease Chart
Enviado por
Umbe ChinakaDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Biochem Disease Chart
Enviado por
Umbe ChinakaDireitos autorais:
Formatos disponíveis
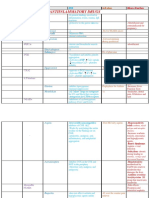
DISORDER
ENZYME
NOTES
HEMOGLOBINOPATHIES
Sickle Cell anemia (Hemoglobin S disease)
Glutamate (HbA) replaced with valine (HbS) on beta chain; anemia, pain, dec. circulation, infections
Hemoglobin C disease
Glutamate (HbA) replaced with lysine (HbC) , mild anemia
Hemoglobin SC disease
Hbs + HbC, undiagnosed until childbirth / surgery, can be fatal
Methemoglobinemia
NADH cytochrome b5
reductase
Diminished oxygen-carring capacity of ferric Hb (metHb) headache, lightheadedness, dyspenea and chocolate
cyanosis
THALASSEMIAS
-thalassemia: Silent Carrier
1 defective
No symptoms
Mild Symptoms
2 defective
2 alpha chains missing
Hb B
4 defective
Accumulation of 4 tetramers in newborns, HYDROPS FATALIS
HbH
3 defective
Accumulation of 4 tetramers in newborns, severe anemia
Deletion of both betas
Both chains defective, fatal HEINZ bodies, inability of HbF HbA, manifests around 8 mos old.
Deletion of 1 beta chain
Only 1 chain defective, not fatal
Scurvy
Proly/lysyl hydroxylase
Vit C def. no hydroxylation
Ehlers-Danlos
Lysyl hydroxylase
Stretchy skin, loose joints, aortic aneurysm, ruptured colon,
Osteogenesis Imperfecta
Collagen Type 1 defect
Brittle bones in babies, blue sclera, multiple fractures, slowed healing
Type 1: heterozygous, postnatal, can survive
Type 2: homozygous, perinatal, death in utero
Emphysema
1- anti-trypsin deficiency
Inherited defect in alpha 1 anti-trypsin resulting in emphysema
-thalassemia: major
Minor
COLLAGEN DISEASES
Alports
Affect glomerular basement membrane, hearing loss, ocular defects
Goodpastures
Antibodies destroy basement membrane of pulmonary and glomerular capillaries
2+
Menkes
ETC INHIBITORS
Electron transport blockers
Lysyl oxidase/Cu
Deficient cross linking secondary to functional copper deficiency; depigmented
(steely) hair, arterial tortuosity and rupture, cerebral degeneration, anemia, osteoporosis.
Complex1 NADH
dehydrogenase
Amobarbital, rotenone
Complex III cytochrome
reductase
Antimycin A
Complex IV cytochrome
oxidase
CO,CN
Complex V (ATP
synthase)
Oligomycin
Aconitase
Inhibited
TCA CYCLE
Fluoroacetate
Malonate
Succinate dehydrogenase
Inhibited
Arsenite
-ketogluconate
dehydrogenase
Inhibited
Complex 1 (NADH
dehydrogenase)
Degeneration of optic nerve, blindness in early adult
HEREDITARY MITOCHONDRIAL
DISEASES
Lebers hereditary optic neuropathy
Kearns-Sayre
Ragged red fibers, heart block, retinal pigmentation
MELAS
Mitochondrial myopathy, encephalomyopathy, lactic acidosis, stroke-like episodes
MERRF
Myoclonus epilepsy with ragged red fibers; ataxia, sensorineural deafness
GLUCOSE & PYRUVATE
METABOLISM
Pyruvate dehydrogenase deficiency
Pyruvate dehydrogenase
Lactic acidosis, neurologic defects (Wernicke-Korsakoff)
Pyruvate DH complex deficiency
Pyruvate DH complex
Pyuvate to lactate, neonatal death, infancy death, episodic ataxia after meal
Arsenic poisoning
G3PDH
Lost NADH, pyruvate accumulates
Pyruvate kinase deficiency
Pyruvate kinase
Most common enzyme deficiency in glycolytic pathway; hemolytic anemia, jaundice
GALACTOSE METABOLISM
Classical galactosemia
GALT
Cirrhosis, mental retardation, cataracts, galactosuria
Galactokinase deficiency
Galactokinase
Cataracts, galactosemia, galactosuria
UDP galactose 4-epimerase deficiency
Benign: affects RBCs and WBCs Malignant: similar to GALT def
FRUCTOSE METABOLISM
Hereditary fructose intolerance
Aldolase B
Toxic liver damage, renal disease, hypophosphatemia, gout
Essential fructosuria
Fructokinase
Benign condition, fructosuria
HMP PATHWAY/NADPH RELATED
DISORDERS
Hemolytic Anemia
G6PD
X linked, hemolytic anemia often induced by infections, oxidant drugs & fava beans; inadequate NADPH
production results in reduction in antioxidant activity of glutathione in mature RBCs
Class I: chronic nonspherocytin anemia, most severe
Class II: Mediterranean, normal stability, scarce activity in RBCs
Class III: A-, oldest RBCs removed
Amyotrophic Lateral Sclerosis
Superoxide dismutase
Degenerated motor neurons in CNS
Chronic granulomatosis
NADPH oxidase
Persistant chronic pyogenic infections; deficiency of enzyme located in leukocyte membrane
Glycogen synthase
Hypoglycemia, death, hyperketonia
GLYCOGEN STORAGE DISEASES
Type 0
VON Gierkes (Type 1)
Glucose 6-phosphate
Hepatosplenomegaly, severe fasting hypoglycemia
Pompes (Type II)
-1-4 glucosidase
(acid maltase)
Infants: mental retardation, cardiomegaly, death by 2 yrs; juvenile myopathy
Adult: gradual skeletal myopathy
Coris (Type III)
-1-6 glucosidase
Mild hypoglycemia, hepatomegaly
Andersens (Type IV)
Glucosyl-4-6-transferase
Hepatosplenomegaly, liver failure, death by 2 yrs
McArdles (Type V)
Muscle glycogen
phosphorylase
Muscle cramping, fatigue, no increase in lactic acid after exercise
Hers (Type VI)
Liver glycogen
phosphorylase
Mild hypoglycemia
Hurlers
-L-iduronidase
Corneal clouding, MR, coarse facial features, early death
Hunters
Iduronate sulfatase
X-linked, physical deformity, MR
Sanfilippos Types A-D
Type-Aheparan sulfate
Type BNacetylglucosaminidase
Type CNacetyltransferase
Type D Nacetylglucosamine
Severe nervous system disorders; mental retardation
Scheies
-L-iduronidase
Like Hurlers but normal life span
Slys
-glucronidase
Hepatosplenomegaly, physical deformity
Lysosomal hydrolytic
enzymes
Deficiency in ability to phosphorylated mannose residuesof potential lysosomal enzymes;
results in incorrect targeting of glycoproteins; death by 8 yrs; elevated N-linked glycoproteins in urine.
Congenital A-beta-lipoproteinemia
Apo B-48
Accum of chylomicrons in enterocytes
Type 1 hyperlipidemia (familial
hyperchylomicronemia)
Apo C-II, Capillary
lipoprotein lipase
Accumulation of chylomicrons in plasma; high plasma TAGs and eruptive xanthomas
(TAG deposits in skin) and pancreatitis.
Mucopolysaccharidoses
Synthesis of glycoproteins
I-cell disease
Metabolism of Dietary Lipids
Type II hyperlipidemia
Type III hyperlipidemia (familial
dysbetalipoproteinemia)
Genetic defect in synthesis, processing or functioning of LDL receptor; elevated LDL levels
Familial hypercholesterolemia
Apolipoprotein E
Accumulation of chylomicron remnants in plasma
Type IV hyperlipidemia
Inc. VLDL due to obesity, alcohol, diabeties
Type V hyperlilidemia
Inc. chylomicrons, TAGs, VLDL, pancreatitis
Wolman disease
Cannot hydrolyze lysosomal cholesteryl esters
Familial LCAT deficiency
Complete absence of LCAT, low HDL
Fish Eye Disease
Partial LCAT absense
Zellweger syndrome
Defective peroxisomal biogenesis, accumulated VLCFAs in blood
X-linked Leukodystrophy
Defective peroxisomal activation of VLCFAs, destroyed myelin
Mobilization of Stored Fats & [FA]
Carnitine deficiency
inability to use long chain FA as fuel, causes: congenital, liver disease
CAT-1 def
Liver cannot synthesize glucose during fast, hypoglycemia, coma, death
CAT-2 def
Cardiomyopathy, muscle weakness following exercise
Medium chain Fattyacyl CoA
dehydrogenase deficiency
Medium chain fatty acyl
CoA
Decreased FA oxidation, severe hypoglycemia; cause of 10% SIDS cases, Reyes syndrome; treat with
high carb diet
Paroxysomal Nocturnal Hemoglobinuria
GPI synthase
In hematopoietic cells
Refsum disease
Fatty acid alphahydroxylase
AR, increased phytanic acid, neurologic symptoms
Vit B12 def
Methylmalonic academia and aciduria, metabolic acidosis
Phospholipid metabolism
Niemann-Pick Type A
Sphingomyelinase
Type B
Type C
Cherry red macula, hepatosplenomegaly, severe mental retardation, death in early childhood
Chronic lung damage, death in early adulthood
Sphingomyelinase
Cannot transport unesterified cholesterol out of lysosomes
Tay-Sachs
-hexoaminidase A
Cherry-red macula inc. GM2, blindness, MR, early death
Gauchers
-glucosidase
Sphingolipidosis, inc. glucocerebrosides, hepatosplenomegaly, MR, frequently fatal
Metachromatic leukodystrophy
Arylsuldatase A
MR, demyelination, fatal in 1st decade
Krabbes
-galactosidase
Inc. galactocerebrosides, MR, almost total absence of myelin, fatal
GM1 gangliosidosis
-galactosidase
GM1 accumulation, MR, skeletal deformities, death
Sandhoffs disease
-hexosaminidase A & B
Inc. globosides; same symptoms as Tay-Sachs with rapid progression.
Fabrys
-galactosidase
Inc. globosides; X linked, kidney & heart failure, redish purple skin rash
Farbers
Ceraminidase
Inc. ceramide, painful and progressively deformed joints; granulomas, fatal early in life
Cholesterol & steroid metabolism
CAH Congenital
Adrenal
Hyperplasia
SPHINGOLIPIDOSES
Smith-Lemli-Opitz Syndrome
7-hydrocholesterol-7reductase
AR, double bond migration (Lanosterol to Cholesterol)
Fatty Liver
Imbalanced TG synthesis
and VLDL secretion
Causes: obesity, diabetes mellitus, alcoholism
Cholelithiasis
Cholesterol gallstones
Malabsorption, obstructed biliary tract, hepatic dysfunction; treat: laparoscopic cholecystectomy
3--hydroxysteroid dehydrogenase def
3--hydroxysteroid
dehydrogenase
Inc. pregnenolone, No glucocorticoids, mineralocorticoids, androgens, or estrogen; early death
17- -hydroxylase deficiency
17- -hydroxylase
Sex hormones & cortisol not produced inc. production of aldosterone gives HTN, phenotypically female
but unable to mature
21- -hydroxylase deficiency
21- -hydroxylase
Most common CAH; ACTH levels inc. gives inc. sex hormones & masculinization
11--hydroxylase deficiency
11- -hydroxylase
Dec. cortisol & aldesterone; masculization
Classic PKU
Phenylalanine hydroxylase
MR, dec. melanin synthesis; fair skin, mousy odor, congenital pyloric stenosis, screen after 1st
exposure to phenylalanine in breat milk, restrict phenylalanine intake, increase tyrosine
Malignant PKU
Dihydrobiopterin
reductase/ synthase
Similar to classic PKU, melatonin and serotonin synthesis also compromised., restrict phenylalanine,
add tyrosine, L-dopa, 5-hydroxytryptophan
Maternal PKU
Mother with either classic
or malignant
Developmental abnormalities, microcephaly, MR, mother didnt stay within dietary restrictions during
pregnancy
Alcaptonuria
Homogentisate oxidase
Benign; homogentisate accumulation forms polymers which darkens standing urine. Ochronosis;
darkening of articular cartilage
Maple Syrup Urine Disease
Branched chain ketoacid dehydrogenase
Elevated levels of amino acids and their keto analogues in plasma and urine; high mortality rate;
neurologic problems
Propionyl CoA Carboxylase Deficiency
Elevated propionate in blood; accumulation of odd chain FA in liver; developmental problems
Cystathioninuria
Propionyl CoA
Carboxylase
Cystathionase
Homocystinuria
Cystathionine synthetase
Accumulation of homocysteine in urine, elevated methionine & metabolites in blood, MR, osteoporosis
Histidinemia
Histidase
Elevated histadine in blood and urine, sometimes MR
Albinism
Tyrosinase
Inability to convert tyrosine to melanin
Tyrosinosis
Eumarylacetoacetate
hydrolase
Liver & kidney damage
Nonketogenic hyperglycinemia
Glycine cleavage complex
Severe mental deficiencies & low survival rate past infancy, inc. glycine in blood.
Carbamoylphosphate
synthetase I
Within 24-48 hrs after birth infant becomes increasingly lethargic, needs stimulation to feed, vomiting,
hypothermia, & hyperventilation; without appropriate intervention death occurs; treat with arginine which
AMINO ACID METABOLISM
Accumulation of cystathionine and metabolites, no clinical symptoms
UREA CYCLE
Type I Hyperammonemia
activates N-acetylglutamate synthetase
N-acetylglutamate synthetase deficiency
N-acetylglutamate
synthetase
Severe/mild hyperammonemia associated wuth deep coma, acidosis, recurrent diarrhea, ataxia, hypoglycemia,
hyperornithinemia; treatment includes administration of carbamoyl glutamate which activates CPS I
Type 2 hyperammonemia
Ornithine
transcarbmoylase
Most commonly occurring UCD, only X linked, increased ammonia and aa in serum, increased serum
orotic acid due to mitochondrial carbamoylphosphate entering cytosoland incorporating in pyrimidine
nucleotides leading to excess productin and excess catabolic products; treat with high carb, low protein diet,
and sodium phenylacetate/benzoate for ammonia detox
Classic Citrullinemia
Argininosuccunate
synthetase
Episodic hyperammonemia, vomiting, lethargy, ataxia, seizures, coma; treat with arginine to increase
citruline excertion and sodium benzoate to detox ammonia
Argininosuccinate Aciduria
Argininosuccinate lyase
(argininosuccinase)
Episodic symptoms similar to classic citrullinemia, elevated plasma and CSF argininosuccunate;
treat with argentine and sodium benzoate.
Hyperargininemia
Arginase
Rare UCD progressive spastic quadriplegia and MR high ammonia & arginine in CSF & serum, high arginine,
lysine, and ornithine in urine; treat with low protein diet including essential AA but no arginine
Acute Intermittent porphyria
Uroporphyrinogen
synthase
Autosomal dominant, inc. porphobilinogen & ALA in urine, attacks precipitated by drugs that induce
cytochrome P450 in liver
Congenital erythropoietic porphyria
Uroporphyeinogen III
synthase
Inc. uroporphyrinogen I & uroporphyninI
Prophyria Cutanea Tarda
Uroporphyrinogen
decarboxylase
Inc. uroporphyrinogen III which converts to uroporphyrinogen I & coproporphyrinogen I
Hereditary Coproporphyria
Coproporphyrinogen
oxidase
Inc. coproporphyrinogen III
Varigate Porphyria
Protoporphyrin oxidase
Accumulation of protoporphyrinogen IX
Erythropoietic Protoporphyria
Ferrochelatase
Accumulation of protoporphyrin IX
Sideroblastic Anemia
ALA synthase
X-linked
Crigler-Najjar syndrome
Bilirubin glucuronyl
transferase
In newborns: newborn jaundice, treat with blue light
Lead poisoning
ferrochelatase/
ALA dehydratase
Inc. ALA and protoporphyrin XI, DEC. heme
HEME BIOSYNTHESIS/DEGREDATION
CONGENITAL ADRENAL HYPERPLASIA
3--hydroxysteroid DH def.
No glucocorticoids, mineralocorticoids, androgens/estrogens, hyponatremia, feminine genitalia,
early death
17--hydroxylase def.
No sex hormones, cortisol, inc. mineralocorticoids, hypernatremia, HTN, feminine genitalia,
early death
21--hydroxylase def.
Greater than 90% CAH, no mineralo/glucocorticoids, inc. androgens, masculinization
11--hydroxylase def.
Dec. cortisol, aldesterone, and corticosterone, inc. deoxycorticosterone; fluid retention, HTN,
masculinization
LETTER
NAME
COENZYME/
ACTIVE FORM
DEFICIENCY
REACTIONS
TYPE
B1
Thiamine
TPP
Beri-beri; Wernicke-Korsakoff
Transketolase, PDC and -KG
Dehydrogenase
Oxidative, decaeboxyl
ation, transfer of -ketols
B2
Riboflavin
FAD, FMN
Dermatitis, cheilosis, glossitis
Succinate DH
Redox
B3
Niacin
NAD, NADP
Pellagra; 3 Ds,
B6
Biotin
Biotin
Adivin; dermatitis, glossitis, anorexia, nausea
Acetyl carboxylase,propionyl
carboxulase, pyruvate
carboxylase
Carboxylation
B6
Pantothenic acid
CoA
Not significant
Citrate & FA synthase
Acyl carrier
Folic Acid
THF
Megaloblastic anemia, neural tube defects, PABA
analogues, dihydrofolate inhibitors
Purine & thymine sntesis, Met,
Ser, Gly, Cys
1 C metabolism
B12
Cobalamin
5deoxyadenosyl
cobalamin,
methylcobalamin
Pernicious anemia, CNS symotoms, folate trap
Synth of Met & isomerization
of methylmalonyl CoA
succinyl CoA
B6
Pyridoxine,
pyridoxal
Pyridoxal PO4
Rare, isoniazid can induce deficiency
AST,ALT
Transamination,
deamination
Ascorbic acid
Ascorbic acid
Scurvey
Hydroxylation of praline in
collagen
Antioxidant, hydrox of
Praline & lysine
Retinol
Retinol in vision,
retinoic acid in
epithelial cells
Blindness, sterility, skin problems
Visual cycle
Cholecalciferol
1,25-diOH D3
Children: rickets, adults: osteomalacia
Calcium levels in plasma
Phyllo/menaquinones
Same
Hypothrombinemia
Formation of gcarboxyglutamate
Tocopherols
-tocopherol
Abnormal cell membranes
Redox
Carboxylation of
certain Glu residues
Anti-oxidant
Você também pode gostar
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- PALS Book 1Documento18 páginasPALS Book 1Umbe ChinakaAinda não há avaliações
- Drug Sheet 2Documento88 páginasDrug Sheet 2Umbe ChinakaAinda não há avaliações
- ACLS Provider Manual Supplementary Material: © 2016 American Heart AssociationDocumento76 páginasACLS Provider Manual Supplementary Material: © 2016 American Heart AssociationUmbe ChinakaAinda não há avaliações
- A - B A B Cosø Axbx + Ayby + Azbz - A X B - Absinø: Chapter 7Documento3 páginasA - B A B Cosø Axbx + Ayby + Azbz - A X B - Absinø: Chapter 7Umbe ChinakaAinda não há avaliações
- Digestive System: 1. Mechanical Processing 2. Secretion 3. DigestionDocumento14 páginasDigestive System: 1. Mechanical Processing 2. Secretion 3. DigestionUmbe ChinakaAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Soil Color and Texture MeaningDocumento9 páginasSoil Color and Texture MeaningTinashe KatsuroAinda não há avaliações
- Alfa Laval Hvo Pre Treatment Webinar Final 003Documento27 páginasAlfa Laval Hvo Pre Treatment Webinar Final 003Lim Chee SiangAinda não há avaliações
- Lec 6Documento21 páginasLec 6Loganathan SelvamAinda não há avaliações
- Centricast CL 1520 Data SheetDocumento6 páginasCentricast CL 1520 Data SheetOlmer Romero MendezAinda não há avaliações
- Egyptian Blue Cuprorivaite A Window To Ancient Egyptian TechnologyDocumento13 páginasEgyptian Blue Cuprorivaite A Window To Ancient Egyptian TechnologyDοмenıκ CaesarAinda não há avaliações
- Gas Processing Fundamentals Manual1Documento12 páginasGas Processing Fundamentals Manual1Ahmed Khamees ShatlaAinda não há avaliações
- Drizo IranDocumento12 páginasDrizo IranDiego1980bAinda não há avaliações
- SpECcell Fibre TDSDocumento2 páginasSpECcell Fibre TDSNgọc Đức ĐoànAinda não há avaliações
- Yamaha Project ReportDocumento19 páginasYamaha Project ReportRohit OberoiAinda não há avaliações
- Introduction To TextileDocumento30 páginasIntroduction To Textileumar.niift3049100% (1)
- Ionic EquilibriumDocumento4 páginasIonic EquilibriumFu HongAinda não há avaliações
- Police Photography/CriminalisticDocumento11 páginasPolice Photography/CriminalisticNoy Decierdo100% (2)
- NuHeat AR500 Datasheet 2 2014Documento2 páginasNuHeat AR500 Datasheet 2 2014paul ArcosAinda não há avaliações
- Analysis of Trihalomethanes: and Related Pentane-Extractable Organic HalidesDocumento33 páginasAnalysis of Trihalomethanes: and Related Pentane-Extractable Organic HalidesaviantaraAinda não há avaliações
- GC Application: Alcohols On ZB-WAX 30x.25x.25Documento2 páginasGC Application: Alcohols On ZB-WAX 30x.25x.25qncargbAinda não há avaliações
- Kinetics of The Iodination of Acetone PDFDocumento6 páginasKinetics of The Iodination of Acetone PDFsamAinda não há avaliações
- Exercises: Sections 10.3, 10.4: The Gas Laws The Ideal-Gas EquationDocumento6 páginasExercises: Sections 10.3, 10.4: The Gas Laws The Ideal-Gas EquationPcd MickeyAinda não há avaliações
- Material Safety Data Sheet: Your Safety Is Our PriorityDocumento2 páginasMaterial Safety Data Sheet: Your Safety Is Our PriorityPutri CipoetAinda não há avaliações
- Anchor Bolt For Brick MasonryDocumento11 páginasAnchor Bolt For Brick MasonryEdmond Chow100% (1)
- Tanks and Equipment: For Liquefied Petroleum Gases - Storage and ServiceDocumento48 páginasTanks and Equipment: For Liquefied Petroleum Gases - Storage and ServiceAlroukn MechanicalAinda não há avaliações
- Latex & RubberDocumento4 páginasLatex & RubberLựuLiềuLìAinda não há avaliações
- Experiment 10 - Quantitative Determination of The Purity and Dissociation of Potassium Hydrogen Phthalate by Potentiometric Titration AtqDocumento3 páginasExperiment 10 - Quantitative Determination of The Purity and Dissociation of Potassium Hydrogen Phthalate by Potentiometric Titration AtqDoom RefugeAinda não há avaliações
- MITOCHONDRIADocumento3 páginasMITOCHONDRIAAbid RazaAinda não há avaliações
- BatteriesDocumento29 páginasBatteriesgihan5dhananjaya5katAinda não há avaliações
- Carbon & It's Compounds (X)Documento27 páginasCarbon & It's Compounds (X)Pakhi MauryaAinda não há avaliações
- 2009 H2 Chemistry Paper 2 (MCQ) + AnsDocumento11 páginas2009 H2 Chemistry Paper 2 (MCQ) + AnsIliyana IliAinda não há avaliações
- Ammonia Based Refrigeration SystemsDocumento19 páginasAmmonia Based Refrigeration SystemsHoainam NguyenAinda não há avaliações
- Types of Dosage Forms Lecture2,2Documento34 páginasTypes of Dosage Forms Lecture2,2Bhuvana TejaAinda não há avaliações
- Electroanalytical Methods: Presented ToDocumento36 páginasElectroanalytical Methods: Presented ToSyed UmairAinda não há avaliações
- Braskem Braskem PP PCD 0140BR Polypropylene Impact CopolymerDocumento2 páginasBraskem Braskem PP PCD 0140BR Polypropylene Impact CopolymerBFCAinda não há avaliações