Escolar Documentos
Profissional Documentos
Cultura Documentos
Is There A Role For Rifampicin, Ofloxacin and Minocycline (ROM) Therapy in The Treatment of Leprosy? Systematic Review and Meta-Analysis
Enviado por
Lidya ChristyTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Is There A Role For Rifampicin, Ofloxacin and Minocycline (ROM) Therapy in The Treatment of Leprosy? Systematic Review and Meta-Analysis
Enviado por
Lidya ChristyDireitos autorais:
Formatos disponíveis
Tropical Medicine and International Health
doi:10.1111/j.1365-3156.2011.02873.x
volume 16 no 12 pp 15411551 december 2011
Systematic Review
Is there a role for rifampicin, ofloxacin and minocycline (ROM)
therapy in the treatment of leprosy? Systematic review and
meta-analysis
Maninder S. Setia1,5, Santosh S. Shinde2, Hemangi R. Jerajani3 and Jean-Francois Boivin4
1
2
3
4
5
Department of Epidemiology, Biostatistics, and Occupational Health, McGill University, Montreal, QC, Canada
Cutis Skin Clinic and Laser centre, Belgaum, Karnataka, India
Department of Dermatology and Venereology, M.G.M. Medical College and Hospital, Kamothe, Navi Mumbai, India
Clinical Epidemiology, Jewish General Hospital, Montreal, QC, Canada
Consultant Dermatologist and Epidemiologist, Karanam Consultancy, Mumbai, India
Summary
background A combination of rifampicin, ofloxacin and minocycline (ROM) is one of the newer
recommendations for treatment of leprosy. We performed a systematic review and a meta-analysis of
studies that had evaluated the efficacy of ROM therapy in treatment of paucibacillary and multibacillary
leprosy patients.
methods Studies were identified by searching the PubMed, Embase, LILACS and Cochrane databases.
Data were abstracted from all relevant studies, and fixed effects models were used to calculate the
summary estimate of effect in paucibacillary and multibacillary leprosy patients.
results Six studies comparing ROM therapy to multidrug therapy and eight studies that evaluated the
effect of ROM therapy alone (no comparison group) were included in the review and meta-analysis. The
combined estimate for single dose ROM vs. multidrug therapy in paucibacillary leprosy patients suggested that ROM was less effective than multidrug therapy in these patients [relative risk: 0.91, 95%
confidence intervals (CI): 0.860.97]. However, the combined estimate for multiple doses of ROM vs.
multidrug therapy in multibacillary leprosy patients suggested that ROM was as effective as multidrug
therapy in reducing bacillary indices in these patients (proportion change: )4%, 95% CI )31% to 23%).
No major side effects were reported in either the ROM or the multidrug treatment groups.
conclusions Single-dose ROM therapy was less effective than multidrug therapy in paucibacillary
patients. However, there are insufficient data to come to a valid conclusion on the efficacy of multidose
ROM therapy in multibacillary leprosy, and additional studies with ROM therapy in multibacillary
leprosy are needed. Furthermore, multiple doses may be considered as another alternative even for
paucibacillary patients, and randomised controlled trials of this therapy may be useful to understand its
contribution in the treatment and control of leprosy.
keywords rifampicin, ofloxacin and minocycline therapy, leprosy, systematic review
Introduction
Leprosy, a disease known since ancient times, continues to
be a public health concern in many countries around the
world. World Health Organization (2010a) estimated that
there were about 244 000 reported cases of leprosy
globally in 2009. The majority of these cases were in Asia,
Africa and countries of South America. India alone, with
133 717 reported cases, accounted for nearly 55% of the
global cases (World Health Organization 2010a). WHO
2011 Blackwell Publishing Ltd
has initiated the leprosy elimination programme with the
aim to reduce the prevalence of leprosy to less than one
case per 10 000 population, so that it ceases to be a public
health problem in the world. Some of the important
components of this elimination programme are knowledge and information about the diagnosis, prompt
diagnosis and effective treatment. (World Health Assembly
1991; World Health Organization 2010b).
The treatment of leprosy has changed in the past three
decades. Dapsone monotherapy was replaced by multidrug
1541
Tropical Medicine and International Health
volume 16 no 12 pp 15411551 december 2011
M. S. Setia et al. ROM therapy in leprosy: a systematic review and meta-analysis
therapy (with dapsone, rifampicin and clofazimine) in
1982 (World Health Organization 1982; Gautam 2009).
Since its introduction, multidrug therapy has been an
important tool in leprosy elimination; not only has it
helped to reduce the duration of treatment but it has also
been useful in addressing problems related to resistance to
dapsone and relapses (Ji 1998; Visschedijk et al. 2000;
Meima et al. 2004) Indeed, WHO has been providing the
multidrug regimen free of cost for treatment of leprosy
patients since 1995 (World Health Organization 2010c).
The current WHO recommendations for adults are as
follows: rifampicin (600 mg once a month), dapsone
(100 mg daily) and clofazimine (300 mg once a month and
50 mg daily) for 1 year for multibacillary leprosy; and
rifampicin (600 mg once a month) and dapsone (100 mg
daily) for paucibacillary leprosy for 6 months (World
Health Organization 2010d). In addition to these medications for cases of leprosy, studies have also highlighted the
role of vaccines (such as BCG, Mycobacterium vaccae, and
others) in the prevention of leprosy. (Talwar 1985; Fine &
Dockrell 1991; Gupte 1991; Stanford 1994; Setia et al.
2006; Schuring et al. 2009).
These multidrug therapy regimens have been very useful
in treatment and control of leprosy. However, poor
compliance (related to long duration and other socioeconomic factors), drug resistance, and relapses have been
reported (Gautam 2009). Thus, there has been a renewed
effort to find newer regimens that may shorten the duration
of therapy and improve compliance while simultaneously
maintaining or improving the therapeutic advantages of
previous regimens (Sehgal et al. 2008). In 1997, a combination of rifampicin (600 mg), ofloxacin (400 mg) and
minocycline (100 mg) ROM therapy was approved
for single-lesion paucibacillary (PB) leprosy (WHO 1998).
In the late 1990s, there have been many studies of the use
of ROM therapy and some of these have also included
multilesional paucibacillary leprosy and even multibacillary leprosy, although a few authors have expressed some
reservations about this therapy (Lockwood 1997; Katoch
1998; Lockwood & Kumar 2004). Thus, we conducted a
systematic review and a meta-analysis of these studies to
understand the utility of ROM therapy in leprosy.
Methods
Data sources
We performed a comprehensive literature search of the
PubMed, EMBASE, LILACS and Cochrane Database (up to
October 2010) to identify the studies that assessed the role
of ROM therapy in the treatment of leprosy. We used the
terms Rifampicin, Ofloxacin, Minocycline and Leprosy
1542
and ROM and Leprosy to identify these articles. The
search was not limited to English language articles, and we
translated studies in other languages if required. Inclusion
criteria were established prior to identifying the articles to
avoid any selection bias. All the studies that described the
efficacy of ROM in treatment of leprosy in human subjects
(leprosy diagnosed according to clinical and or microscopic
criteria) were eligible for inclusion. We excluded studies
that assessed only changes in immunological status of
individuals after ROM therapy, studies that did not describe
clinical improvement outcomes, case reports of ROM
therapy and reviews of leprosy therapy. We also excluded
studies that had used ROM in combination with other
treatments. Although these studies were excluded from the
meta-review, we read them to identify potentially eligible
studies for our review and for the overall discussion on the
role of ROM therapy in leprosy. If a study had multiple
published reports, the report with the maximum number of
cases and longest duration of follow-up was included. A list
of all the studies (included and excluded) was maintained.
Conference abstracts were not included.
Data abstraction
Two major groups of studies were identified: those that
compared ROM therapy with WHO multidrug therapy
(referred to as comparison studies in this manuscript) and
those that reported the clinical efficacy in ROM only
(referred to as ROM only studies), without inclusion of a
comparison group. For the comparison studies, we abstracted information on the authors, year of publication,
place of study, the inclusion and the exclusion criteria, the
design of the study (randomised controlled trial, nonrandomised study, procedure of randomisation if any,
blinding procedures if any, allocation of the medications),
description of the intervention and control groups, the
number of study participants in each group, duration of
follow-up, the dose and duration of medications in each
group, the clinical, bacteriological, and or histopathological criteria for monitoring the subjects, improvement in each
group, the side effects, reactions and relapses in each group.
For the ROM only studies, we abstracted information on
authors, place of study, year of publication, study population, treatment and follow-up, response to treatment, side
effects, reactions and relapses. Two reviewers (MSS and
SSS) were primarily responsible for data abstraction.
Unresolved issues were addressed by consulting JFB.
Data analysis and statistical methods
Data for the paucibacillary and multibacillary leprosy
studies were analysed separately. We extracted the effect
2011 Blackwell Publishing Ltd
Tropical Medicine and International Health
volume 16 no 12 pp 15411551 december 2011
M. S. Setia et al. ROM therapy in leprosy: a systematic review and meta-analysis
measure (relative risk RR) and its 95% confidence interval
for clearance of lesions (as defined by the authors of the
published papers) in the ROM group compared with the
standard therapy group. For manuscripts without RRs, we
calculated them using the raw data (numbers treated healed
etc.) provided by the authors. We calculated the pooled
summary of these RRs using fixed effects models as
described by Greenland (1987). For each study, the standard
error (SE) of the RR was calculated by dividing the
difference in natural logs of the upper and lower confidence
limits by 3 92 (i.e., SE = [ln CIupper ) ln CIlower] 3 92). The
inverse of the square of this standard error (1 SE2) was used
as the weight (Wa) for pooling of the RRs. The summary
measure was calculated by multiplying this weight by the
natural log of the RR (ln RRa). The sum of all the weighted
P
ln RRs was calculated ( Waln RRa). The pooled summary
P
P
estimates was then calculated as Waln RRa Wa, and the
summary RR was obtained by exponentiating this pooled
summary. We drew a Forest plot of all the studies included
in the meta-analysis. We used methods described by Altman
and Bland (2003) to compare RRs and their respective
confidence intervals (as was the case in sensitivity analyses).
We could not calculate the RRs for multibacillary
leprosy studies; the two included studies only provided
mean bacillary indices (BI) for the duration of follow-up.
Thus, we calculated the proportion difference in BI
reduction between the ROM and the multidrug therapy
groups. We calculated the difference in mean BI at baseline
and at 2 years in the ROM group (DR = Rb ) R2); the
proportion difference was then calculated as PR = DR Rb.
Similarly, the proportion difference was calculated for the
multidrug therapy group (PM). The overall difference in
proportion between the ROM and the multidrug therapy
group was calculated as PR ) PM. We also calculated the
95% confidence intervals for this difference. The estimates
from the two multibacillary studies were pooled using the
fixed effects approach (Cooper & Hedges 1994; Shams
et al. 2010). We did not pool the data from ROM only
studies; these were just described in the text and tables.
The studies were also assessed for heterogeneity by using
the chi-square test with degrees of freedom equal the
number of studies that were combined in the meta-analysis
minus one. We planned to use the random effects model if
the studies were found to be heterogeneous. We also
assessed the quality of trials by criteria suggested by Jadad
et al. (1996); the trials are scored on the basis of description of randomisation, blinding and withdrawals.
Publication bias
We assessed publication bias because of the reluctance of
authors and editors to publish smaller studies or those with
2011 Blackwell Publishing Ltd
results closer to a null effect (Song et al. 2000) by using a
funnel plot; ln RR for each of the individual studies was
plotted against its SE. Further, publication bias was
evaluated using Beggs (Begg & Mazumdar 1994) and
Eggers tests (Egger et al. 1997). We used Stata version 10
(StataCorp, College Station, TX, USA) for these tests and
the Forest plot.
Results
Search results: included and excluded studies
We reviewed 257 citations identified from all the four data
bases. Details of the search are provided in Figure 1. After
excluding the duplicate citations and studies that were not
directly relevant to this meta-analysis, we assessed 27
potential studies in detail. Of these, we excluded 13
studies: eight were additional reports of included studies
(Babu et al. 1997; Ganapati et al. 1999; Pai et al. 1999;
Gupte 2000; Martelli et al. 2000; Costa et al. 2001;
Emmanuel & Gupte 2005; National Institute of Epidemiology 2005); two studies did not discuss response to ROM
therapy (Revankar et al. 2002; Sousa et al. 2007); one
study was on contacts of leprosy patients who used ROM
used as chemoprophylaxis (Oo et al. 2008); one study used
ROM along with the Convit vaccine (Majumder et al.
2000); and one study had initially compared ROM therapy
with a combination of ofloxacin and minocycline for a
week followed by standard multidrug therapy in all
patients (Ji et al. 1998).
Thus, we included 14 studies for the review: six studies
comparing ROM therapy with multidrug therapies
(Single-lesion Multicentre Trial Group 1997; 23 Lesion
Multicentre Trial Group 2001; Deshmukh et al. 2003;
Villahermosa et al. 2004; Gupte 2006a; Ura et al. 2007)
and eight studies that observed the improvement only in
ROM therapy (there was no comparison group) (Mane
et al. 1997; Ebenezer & Job 1999; Revankar et al. 1999;
Shinde et al. 2000; Shukla et al. 2002; Martelli et al. 2003;
Gupte 2006b; Alam et al. 2007).
Comparison studies (ROM vs. MDT)
Of the six comparison studies, four were conducted in
paucibacillary leprosy patients (Single-lesion Multicentre
Trial Group 1997; 23 Lesion Multicentre Trial Group
2001; Deshmukh et al. 2003; Gupte 2006a) and two
were conducted in multibacillary leprosy patients
(Villahermosa et al. 2004; Ura et al. 2007). The former
four studies used a single dose of ROM, whereas the latter
two studies used multiple doses. All four paucibacillary
leprosy studies were conducted in India. Of these, only one
study (Deshmukh et al. 2003) found a higher proportion of
1543
Tropical Medicine and International Health
volume 16 no 12 pp 15411551 december 2011
M. S. Setia et al. ROM therapy in leprosy: a systematic review and meta-analysis
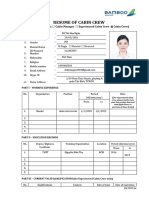
Figure 1 Figure showing the data
abstraction procedure for the present
meta-analysis.
improvement in the ROM group than in the standard
multidrug therapy. The two studies in multibacillary
leprosy patients found that multidrug therapy was slightly
more effective in reducing the bacillary index, although the
difference was not statistically significant. No life-threatening side effects were reported in either of the groups; nor
did there appear to be a preponderance of side effects in
either of the groups. Reversal reactions and erythema
nodosum leprosum reactions were reported in both.
Although one study found similar numbers of reactions in
both the study (ROM) and the control (MDT-MB) groups
(Villahermosa et al. 2004), another (Single-lesion Multicentre Trial Group 1997) found that the ROM group had
double the number of reaction cases as the MDT-PB group.
Interestingly, although the former study provided detailed
information on reactions (Tables S1), the numbers of
1544
patients in both groups were too small to make any useful
conclusions. The other MDT-MB study by Ura et al.
(2007) did not give any detailed information on the
reactions. One study in paucibacillary leprosy patients,
however, found that the relapse rate was twice as high in
the ROM group as in the control group (multidrug
therapy) (Gupte 2006a). Tables S1 provides further details
on each study.
ROM only studies
Of the eight studies in the ROM only group, five were
conducted in India (Ebenezer & Job 1999; Revankar et al.
1999; Shinde et al. 2000; Shukla et al. 2002; Gupte 2006b)
and one each was conducted in Brazil (Martelli et al. 2003),
Bangladesh (Alam et al. 2007) and Senegal (Mane et al.
2011 Blackwell Publishing Ltd
Tropical Medicine and International Health
volume 16 no 12 pp 15411551 december 2011
M. S. Setia et al. ROM therapy in leprosy: a systematic review and meta-analysis
1997). All but one (Mane et al. 1997) were in paucibacillary
leprosy patients. The effects in these studies were measured
by various criteria: clearance of lesions, disappearance of
patches or reduction in granulomas on histopathology.
Overall, the range of clearance (as defined by the individual
authors) for single-dose ROM therapy in paucibacillary
leprosy patients varied from 44% in the study by Shukla
et al. (2002) and 99% in the study by Revankar et al.
(1999). Mane et al. (1997) had treated paucibacillary
patients with monthly doses of ROM for 6 months; they
reported that about 25% of these patients had complete
clearing of lesions and in the remaining subjects these lesions
were reduced significantly. Although the majority of the
reports did not mention side effects, Mane et al. (1997),
who did specifically mention side effects, did not find any
clinical toxic effect of the medications. The highest rate of
relapse was 6 1000 person years in the study by Revankar
et al. (1999); however, this figure included delayed clinical
problems in relapses. Interestingly, Martelli et al. (2003)
from Brazil found that individuals who were positive for
Mycobacterium leprae confirmed by PCR were more likely
to report neural aggression. Further details on each study
are provided in Tables S2.
Summary estimates and publication bias
We calculated the RRs in four studies (Single-lesion Multicentre Trial Group 1997; 23 Lesion Multicentre Trial
Group 2001; Deshmukh et al. 2003; Gupte 2006a) that
compared single-dose ROM therapy to multidrug therapy in
paucibacillary leprosy patients. The summary estimate of
these RRs using the fixed effects model was 0.91 (95% CI:
0.860.97). No statistically significant heterogeneity was
observed in these studies; hence, the random effects model
was not used. Figure 2a shows a Forest plot of individual
estimates and the combined estimate in the Forest Plot.
There was no apparent publication bias as determined with
Beggs Funnel Plot (Figure 2b). The test for publication bias
was not statistically significant by both Beggs and Eggers
methods. Two studies (Villahermosa et al. 2004; Ura et al.
2007) assessed the effect of multiple doses of ROM therapy
in multibacillary patients. The combined proportion difference for the reduction in bacillary index in the ROM
group compared with the multidrug therapy group in these
multibacillary leprosy patients was )4% (95% CI: )31% to
23%). Both studies were statistically homogenous; hence,
the random effects model was not used.
Figure 2 (a) Forest plot of the
paucibacillary leprosy studies included in
the meta-analysis. The black dots are the
point estimates for each study and the
horizontal lines around it are the confidence
intervals. The box represents the size given
to each study in the fixed effects model
(mentioned as % Weights). The dashed line
is the combined estimate. The diamond
represents the confidence interval of the
summary estimate. (b) Funnel plot of all the
included studies in the meta-analysis
(assessing the publication bias).
2011 Blackwell Publishing Ltd
1545
Tropical Medicine and International Health
volume 16 no 12 pp 15411551 december 2011
M. S. Setia et al. ROM therapy in leprosy: a systematic review and meta-analysis
Sensitivity analysis
We performed sensitivity analyses on our results. For
instance, we had included data from a WHO report (Gupte
2006a) on the effect of ROM therapy (compared with data
from articles published in peer reviewed journals) in
paucibacillary leprosy patients in the meta-analysis. After
excluding this WHO report, we found that the summary
estimate changed slightly (RR: 0.87, 95% CI: 0.790.96),
even though this difference was not statistically significant
(P = 0.44). In one of the paucibacillary leprosy studies
(Deshmukh et al. 2003), we used the number of patients
that had clinically improved (compared with complete
clearance in other studies). The summary estimate after
excluding this study was nearly similar to the overall
estimate (RR: 0.91, 95% CI: 0.860.97).
Discussion
The present systematic review and meta-analysis present
information on the role of ROM therapy in the treatment
of leprosy. Of the studies included for the systematic
review, six compared ROM therapy to the multidrug
therapy and eight studied the effectiveness of ROM
therapy alone. The combined estimate for single-dose
ROM vs. multidrug therapy in paucibacillary leprosy
patients suggested that ROM was less effective that
multidrug therapy in these patients (RR: 0.91, 95% CI:
0.860.97). However, the combined estimate for multiple
doses of ROM vs. multidrug therapy in multibacillary
leprosy patients (proportion change: )4%, 95% CI: )31%
to 23%) did not provide enough information to substantially conclude on the efficacy of multidose ROM therapy
in multibacillary leprosy and additional studies with ROM
therapy in multibacillary therapy are needed. No major
side effects were reported in either the ROM or the MDT
treatment groups.
Even though the ROM regimen was recommended only
in 1997, many previous clinical and animal studies had
suggested the utility of these medications in leprosy.
Indeed, some studies in the 1970s demonstrated the
bactericidal effect of rifampicin on Mycobacterium leprae.
Rees et al. (1970) demonstrated that rifampicin inhibited
the growth of Mycobacterium leprae in mice; this
inhibition was seen in both dapsone sensitive and resistant
bacilli. In the same study, rifampicin in a dose
600 mg day was effective in treating lepromatous
patients. Subsequent studies in humans and animal
models confirmed the role of rifampicin in treating
leprosy. (Shepard et al. 1971, 1972, 1974; Levy et al.
1976). Ji et al. (1992, 1996) initially reported that
rifampicin was highly bactericidal even in a single dose
1546
and in a subsequent study found rifampicin to be highly
bactericidal compared with other regimens including
newer drugs. Unsurprisingly, rifampicin was thus included
in the multidrug therapy regimen for leprosy. However, it
was only in the latter half of 1980s that reports on the
bactericidal effects of the other two drugs (ofloxacin and
minocycline) were discussed in literature; these reports
included both animal studies and studies of clinical cases
of leprosy (Saito et al. 1986; Gelber 1987; Pattyn 1987;
Grosset et al. 1988, 1990; Leysen et al.1989; Franzblau
& White 1990; Gelber et al. 1992, 1994). In 1998, Ji
et al. reported that although both combinations ofloxacin and minocycline & rifampicin, ofloxacin and minocycline were bactericidal, the former was less so than
the latter in lepromatous patients. Hence, these animal
and clinical studies demonstrated the role of these three
drugs in the treatment of leprosy; subsequently, clinical
studies were conducted to assess the efficacy of this combination in various forms of leprosy. However, Katoch
(1998) had reservations about the use of ROM in leprosy;
he argued that as Mycobacterium leprae does not multiply
simultaneously, the use of these regimens may not have a
convincing enough microbiological rationale for the use
of these regimens.
As seen in our review, the two main groups of studies
that formed a part of the existing literature were as
follows: those comparing ROM therapy to multidrug
therapy and those that had simply evaluated the efficacy of
ROM therapy in treatment of leprosy patients. Interestingly, even though WHO guidelines recommend ROM
therapy for single-lesion paucibacillary leprosy
patients (World Health Organization 2010d), these studies had used ROM in such patients (even with more than
one patch) and in multibacillary leprosy patients; thus,
they are useful to understand the role of this therapy in
different forms of leprosy. As observed in our metaanalysis, single-dose ROM therapy was less protective
than the WHO multidrug therapy in paucibacillary leprosy
patients. In all of these studies, patients in the ROM group
received only a single dose of ROM therapy even though
the number of lesions varied from 1 to 5 among these
patients. In contrast to this, all multibacillary leprosy
patients received monthly doses of ROM therapy for
24 months; this was the same time period for which the
control group received WHO multidrug therapy. As such,
we found that the combined proportion change of bacillary index was )4% (95% CI: )31% to 25%). The
confidence intervals were too broad, and sufficient increase
in statistical power was not achieved in multibacillary
leprosy. Hence, there are insufficient data to conclude on
the efficacy of multidose ROM therapy in multibacillary
leprosy, and additional studies with ROM therapy in
2011 Blackwell Publishing Ltd
Tropical Medicine and International Health
volume 16 no 12 pp 15411551 december 2011
M. S. Setia et al. ROM therapy in leprosy: a systematic review and meta-analysis
multibacillary leprosy are required. It appears that multiple doses of ROM therapy are as effective as multidrug
therapy compared with single dose; we have to highlight,
however, that these two different types of doses were used
in different types of leprosy.
The other group of studies, i.e., those that included
only the ROM therapy group, also showed a clinical
improvement in the patients, although the proportion
varied across different studies. All but one study had used
ROM as a single-dose therapy for treatment of paucibacillary leprosy patients. The study by Mane et al. (1997)
from Senegal had used multiple doses of ROM once a
month for 6 months in paucibacillary leprosy patients and
for 24 months in multibacillary patients and found
good clinical response among these paucibacillary leprosy
patients. Revankar et al. (1999) used single-dose therapy
in both single-lesion and multilesional (two to five lesions)
paucibacillary leprosy patients; they reported nearly
similar clinical outcomes in both these groups. Interestingly, one study (Alam et al. 2007) in this group had a
long average follow-up of 6.3 years (as reported to us by
one of the co-authors of the study), and the authors
reported a high relapse rate (5.09 per 1000 person years).
Even though this study did not include comparison
groups, the findings are useful to understand the clinical
outcomes in leprosy patients and for the design of future
studies.
ROM therapy has its own advantages; it is administered
as single dose (or multiple doses every month) and may
lead to better patient compliance, an issue that has been
highlighted as one problem of the WHO multidrug therapy
regimen (Gautam 2009). Another socially relevant
advantage discussed by Villahermosa et al. (2004) is the
pigmentation because of clofazimine in the multidrug
therapy. They suggest that as none of the medications in
the ROM therapy will cause the type of pigmentation
associated with clofazimine, ROM will help maintain the
anonymity of these patients. Indeed, this was also highlighted by a WHO report on treatment of leprosy (WHO
1998). Even though individually each of these medications
rifampicin, ofloxacin, and minocycline may have side
effects including some very severe ones (Halkin 1988; Ji
et al. 1993, 1994; Vijayakumaran et al. 1997; WHO 1998;
Namisato & Ogawa 2000), severe reactions were not
observed in the included studies.
Another important aspect of leprosy therapy is the rate
of relapses in treated patients. Although relapses were not
mentioned in some of the included studies, many had
evaluated these in their study populations. The study with
a relatively longer average follow-up period reported a
relapse rate of 5.09 per 1000 person years (Alam et al.
2007). Others have reported that paucibacillary patients
2011 Blackwell Publishing Ltd
with 25 lesions and treated with ROM were twice as
likely to have a relapse compared with those that were
treated with WHO multidrug therapy. Thus, this appears
to be one shortcoming of ROM therapy. However, as
Lockwood and Kumar (2004) pointed out, we need longterm studies (follow-up of 10 years or more) for a better
understanding of these phenomena. Finally, cost is another
important factor to be considered when recommending
this treatment. Villahermosa et al. (2004) reported that
ROM is more expensive than the WHO multidrug therapy
for a similar duration of treatment, at least in the
Philippines. This trend may be expected in other countries
as well.
As with other reviews and meta-analyses, the present
study also has its limitations. Heterogeneity among studies
is an important limitation in most meta-analyses. As such,
different study sites and populations, varying study designs
and procedures, and differences in measurements of
clinical outcomes (complete clearance vs. clinical
improvement) may lead to heterogeneity between the
subjects. The type of medication used (for example, if
generic versions vs. proprietary versions of the drugs are
used in these studies) may also contribute to the heterogeneity. This heterogeneity can be accounted for by using
the random effects models as described by DerSimonian
and Laird (1986). In our meta-analysis, we did not find any
statistical heterogeneity between the paucibacillary leprosy
studies or the multibacillary leprosy studies; thus, we
restricted our analyses to fixed effect models only. There
was, however, heterogeneity in the paucibacillary leprosy
study populations. Even though they were all paucibacillary leprosy patients, the number of lesions varied across
these studies. Furthermore, some studies had reported
complete clearance whereas another had just reported
clinical improvement.
Another important limitation of such analyses is the
potential publication bias because of the reluctance of
authors and editors to publish smaller studies or those with
results closer to a null effect. (Song et al. 2000) We did not
find evidence of publication bias in the funnel plot; there
was no apparent asymmetry in the distribution of the four
studies in this plot. Similarly, in the corresponding
statistical tests, we did not find any evidence of publication
bias. However, only four studies were available to assess
this bias.
Another important limitation to be considered in the
present analysis is the bias in each of the individual studies.
Although some of the paucibacillary leprosy trials had
randomised treatment allocations, the methods of randomisation were not clearly specified in three of these trials
(Single-lesion Multicentre Trial Group 1997; Deshmukh
et al. 2003; Gupte 2006a) Furthermore, double blinding
1547
Tropical Medicine and International Health
volume 16 no 12 pp 15411551 december 2011
M. S. Setia et al. ROM therapy in leprosy: a systematic review and meta-analysis
was not clearly defined in the manuscripts of these trials. In
such cases, the recorded outcomes may be biased depending on whether the clinical observer favours or not the new
therapy. In multibacillary leprosy cases, even if the
treatment allocation is double blinded, skin pigmentation
because of clofazimine in the WHO multidrug therapy
regimen may provide information on the type of treatment
the study participant is receiving. Thus, blinding may be
even more complicated in these cases. Because we calculated unadjusted RRs from the raw data provided in the
manuscripts, we did not adjust for some of the demographic characteristics of the study participants (such as
age and sex) in our analyses. However, this may be less of a
problem in case of randomised trials. Indeed, in all of the
four paucibacillary trials for which we calculated RRs
using data from the manuscripts, the authors had mentioned that the two groups (ROM and multidrug therapy)
were similar on intake.
Despite these limitations, our review is a new contribution to the existing literature on leprosy treatment. The
summary estimate of all the included paucibacillary leprosy
trials suggests that single-dose ROM therapy is not as
effective as WHO multidrug therapy in treatment of
paucibacillary leprosy patients. However, there are insufficient data to conclude on the efficacy of multidose ROM
therapy in multibacillary leprosy, and additional studies
with ROM therapy in multibacillary leprosy are needed.
Even though in general there were no apparent increases in
reactions, relapses or side effects in the ROM groups
compared with the multidrug therapy groups, the followup periods were relatively short in most of these studies
(a duration of 10 years of follow-up may be important as
suggested by Lockwood and Kumar (2004). Thus, with the
existing literature, there is limited evidence that single-dose
ROM therapy can be a useful alternative to WHO
multidrug therapy in paucibacillary leprosy patients. It is
worthwhile to reiterate that some of the paucibacillary
leprosy patients in the present group of studies also had
multiple lesions; thus, there was heterogeneity in these
subjects as far as the number of lesions was concerned.
Finally, multiple doses may be considered as another
alternative even for paucibacillary leprosy patients and
randomised controlled trials of this therapy may be useful
to understand its contribution in the treatment and control
of leprosy.
Acknowledgements
MSS was funded by CIHR-IHSPR Fellowship and CIHRRRSPQ Public Health Training Programme for his
doctoral studies at McGill University.
1548
References
Alam K, Butlin CR, Pahan D, Kumar S & Chowdhury (2007)
Long-term follow-up of ROM treated cases. Leprosy Review
78, 160.
Altman DG & Bland JM (2003) Interaction revisited: the
difference between two estimates. BMJ 326, 219.
Babu GR, Edward VK, Gupte MD et al. (1997) Efficacy of singledose multidrug therapy for the treatment of single-lesion
paucibacillary leprosy. Leprosy Review 68, 341349.
Begg CB & Mazumdar M (1994) Operating characteristics of a
rank correlation test for publication bias. Biometrics 50,
10881101.
Cooper H & Hedges L (1994) The Handbook of Research
Synthesis. Russell Sage Foundation, New York, NY.
Costa MB, Cavalcanti Neto PF, Martelli CM et al. (2001) Distinct
histopathological patterns in single lesion leprosy patients treated with single dose therapy (ROM) in the Brazilian Multicentric Study. International Journal of Leprosy and Other
Mycobacterial Diseases 69, 177186.
DerSimonian R & Laird N (1986) Meta-analysis in clinical trials.
Controlled Clinical Trials 7, 177188.
Deshmukh AR, Dhurat RS & Jerajani HR (2003) A comparative
clinicopathological study of single dose ROM in paucibacillary
leprosy patients with 1-3 skin lesions. Indian Journal of Leprosy
75, 209217.
Ebenezer GJ & Job CK (1999) Histopathological activity in
paucibacillary leprosy patients after ROM therapy. International Journal of Leprosy and Other Mycobacterial Diseases 67,
409413.
Egger M, Davey Smith G, Schneider M & Minder C (1997) Bias in
meta-analysis detected by a simple, graphical test. British
Medical Journal 315, 629634.
Emmanuel M & Gupte MD (2005) Lesional characteristics and
histopathology in paucibacillary leprosy patients with 2 or 3
skin lesions: comparison between ROM and PB-MDT regimens.
Indian Journal of Leprosy 77, 1925.
Fine P & Dockrell H (1991) Leprosy vaccines. Vaccine 9,
291293.
Franzblau SG & White KE (1990) Comparative in vitro activities
of 20 fluoroquinolones against Mycobacterium leprae. Antimicrobial Agents and Chemotherapy 34, 229231.
Ganapati R, Revankar CR, Pai VV & Kingsley S (1999) Singledose treatment for paucibacillary leprosy; feasibility of longterm follow up. International Journal of Leprosy and Other
Mycobacterial Diseases 67, 308309.
Gautam VP (2009) Treatment of leprosy in India. Journal of
Postgraduate Medicine 55, 220224.
Gelber RH (1987) Activity of minocycline in Mycobacterium
leprae-infected mice. Journal of Infectious Diseases 156,
236239.
Gelber RH, Fukuda K, Byrd S et al. (1992) A clinical trial of
minocycline in lepromatous leprosy. BMJ 304, 9192.
Gelber RH, Murray LP, Siu P, Tsang M & Rea TH (1994) Efficacy
of minocycline in single dose and at 100 mg twice daily for
2011 Blackwell Publishing Ltd
Tropical Medicine and International Health
volume 16 no 12 pp 15411551 december 2011
M. S. Setia et al. ROM therapy in leprosy: a systematic review and meta-analysis
lepromatous leprosy. International Journal of Leprosy and
Other Mycobacterial Diseases 62, 568573.
Greenland S (1987) Quantitative methods in the review of
epidemiologic literature. Epidemiologic Reviews, 9, 130.
Grosset JH, Guelpa-Lauras CC, Perani EG & Beoletto C (1988)
Activity of ofloxacin against Mycobacterium leprae in the
mouse. International Journal of Leprosy and Other Mycobacterial Diseases 56, 259264.
Grosset JH, Ji BH, Guelpa-Lauras CC, Perani EG & NDeli LN
(1990) Clinical trial of pefloxacin and ofloxacin in the treatment
of lepromatous leprosy. International Journal of Leprosy and
Other Mycobacterial Diseases 58, 281295.
Gupte MD (1991) Vaccines against leprosy. Indian Journal of
Leprosy 63, 342349.
Gupte MD (2000) Field trials of a single dose of the combination
rifampicinofloxacin-minocycline (ROM) for the treatment of
paucibacillary leprosy. Leprosy Review 71(Suppl), S77S80.
Gupte MD (2006a) Clinical Trials for Treatment of PB Leprosy
Patients with Single Dose of Rifampicin, Ofloxacin and Minocycline (ROM): Final Report Effectiveness of Single Dose
ROM in Paucibacillary Leprosy Patients with 2-5 Skin Lesions.
World Health Organization, New Delhi, India.
Gupte MD (2006b) Clinical Trials for Treatment of PB Leprosy
Patients with Single Dose of Rifampicin, Ofloxacin and Minocycline (ROM): Final Report Relapse Rates in Single-lesion
Paucibacillary Leprosy Cases Treated with Single-dose ROM.
World Health Organization, New Delhi, India.
Halkin H (1988) Adverse effects of the fluoroquinolones. Reviews
of Infectious Diseases 10(Suppl 1), S258S261.
Jadad AR, Moore RA, Carroll D et al. (1996) Assessing the quality
of reports of randomized clinical trials: is blinding necessary?
Controlled Clinical Trials 17, 112.
Ji B (1998) Why multidrug therapy for multibacillary leprosy can
be shortened to 12 months. Leprosy Review 69, 106109.
Ji B, Perani EG, Petinon C & Grosset JH (1992) Bactericidal
activities of single or multiple doses of various combinations of
new antileprosy drugs and or rifampin against M. leprae in
mice. International Journal of Leprosy and Other Mycobacterial
Diseases 60, 556561.
Ji B, Jamet P, Perani EG, Bobin P & Grosset JH (1993) Powerful
bactericidal activities of clarithromycin and minocycline against
Mycobacterium leprae in lepromatous leprosy. Journal of
Infectious Diseases 168, 188190.
Ji B, Perani EG, Petinom C, NDeli L & Grosset JH (1994) Clinical
trial of ofloxacin alone and in combination with dapsone plus
clofazimine for treatment of lepromatous leprosy. Antimicrobial
Agents and Chemotherapy 38, 662667.
Ji B, Perani EG, Petinom C & Grosset JH (1996) Bactericidal
activities of combinations of new drugs against Mycobacterium
leprae in nude mice. Antimicrobial Agents and Chemotherapy
40, 393399.
Ji B, Sow S, Perani E, Lienhardt C, Diderot V & Grosset J (1998)
Bactericidal activity of a single-dose combination of ofloxacin
plus minocycline, with or without rifampin, against Mycobacterium leprae in mice and in lepromatous patients. Antimicrobial Agents and Chemotherapy 42, 11151120.
2011 Blackwell Publishing Ltd
Katoch VM (1998) Is there a microbiological rationale for singledose treatment of leprosy? Leprosy Review 69, 25.
2-3 Lesion Multicentre Trial Group (2001) A comparative trial
of single dose chemotherapy in paucibacillary leprosy patients
with two to three skin lesions. Indian Journal of Leprosy 73,
131143.
Levy L, Shepard CC & Fasal P (1976) The bactericidal effect of
rifampicin on M. leprae in man: a) single doses of 600, 900 and
1200 mg; and b) daily doses of 300 mg. International Journal
of Leprosy and Other Mycobacterial Diseases 44, 183187.
Leysen DC, Haemers A & Pattyn SR (1989) Mycobacteria and the
new quinolones. Antimicrobial Agents and Chemotherapy 33,
15.
Lockwood DN (1997) Rifampicin minocycline and ofloxacin
(ROM) for single lesions what is the evidence? Leprosy
Review 68, 299300.
Lockwood DN & Kumar B (2004) Treatment of leprosy. BMJ
328, 14471448.
Majumder V, Saha B, Hajra SK, Biswas SK & Saha K (2000)
Efficacy of single-dose ROM therapy plus low-dose convit
vaccine as an adjuvant for treatment of paucibacillary leprosy
patients with a single skin lesion. International Journal of
Leprosy and Other Mycobacterial Diseases 68, 283290.
Mane I, Cartel J-L & Grosset J-H (1997) Field trial on efficacy of
supervised monthly dose of 600 mg rifampin, 400 mg ofloxacin
and 100 mg minocycline for the treatment of leprosy; first
results. International Journal of Leprosy 65, 224229.
Martelli CM, Stefani MM, Gomes MK et al. (2000) Single lesion
paucibacillary leprosy: baseline profile of the Brazilian Multicenter Cohort Study. International Journal of Leprosy and
Other Mycobacterial Diseases 68, 247257.
Martelli CMT, Stefani MMA, Gillis TP et al. (2003) Final Report
No.60 -Leprosy: Brazils leprosy research and control efforts
enhanced. http://www.who.int/tdrold/research/finalreps/
no60.htm (accessed 22 September 2009).
Meima A, Smith WC, van Oortmarssen GJ, Richardus JH &
Habbema JD (2004) The future incidence of leprosy: a scenario
analysis. Bulletin of the World Health Organization 82, 373380.
Namisato M & Ogawa H (2000) Serious side effects of rifampin
on the course of WHO MDT: a case report. International
Journal of Leprosy and Other Mycobacterial Diseases 68,
277282.
National Institute of Epidemiology (2005) Leprosy Studies. 2026.
http://www.icmr.nic.in/annual/2004-05/nie/leprosy.pdf.
Oo KN, Yin NN, Han TT, Wai KT, Myint K & Gyi MM (2008)
Serological response to chemoprophylaxis in extended contacts
in leprosy a randomized controlled trial. Nihon Hansenbyo
Gakkai Zasshi 77, 310.
Pai VV, Bulchand HO, Revankar CR & Ganapati R (1999) Singledose treatment for paucibacillary leprosy; clinical problems and
management. International Journal of Leprosy and Other
Mycobacterial Diseases 67, 310312.
Pattyn SR (1987) Activity of ofloxacin and pefloxacin against
Mycobacterium leprae in mice. Antimicrobial Agents and
Chemotherapy 31, 671672.
1549
Tropical Medicine and International Health
volume 16 no 12 pp 15411551 december 2011
M. S. Setia et al. ROM therapy in leprosy: a systematic review and meta-analysis
Rees RJ, Pearson JM & Waters MF (1970) Experimental and
clinical studies on rifampicin in treatment of leprosy. British
Medical Journal 1, 8992.
Revankar CR, Pai VV, Samy MSA & Ganapati R (1999) Singledose treatment for paucibacillary leprosy; field implications [4].
International Journal of Leprosy and Other Mycobacterial
Diseases 67, 312314.
Revankar CR, Bulchand HO, Pai VV & Ganapati R (2002) Singledose ROM treatment for multilesion paucibacillary leprosy
further observations. International Journal of Leprosy and
Other Mycobacterial Diseases 70, 3738.
Saito H, Tomioka H & Nagashima K (1986) In vitro and in vivo
activities of ofloxacin against Mycobacterium leprae infection
induced in mice. International Journal of Leprosy and Other
Mycobacterial Diseases 54, 560562.
Schuring RP, Richardus JH, Pahan D & Oskam L (2009)
Protective effect of the combination BCG vaccination and
rifampicin prophylaxis in leprosy prevention. Vaccine 27,
71257128.
Sehgal VN, Sardana K & Dogra S (2008) The imperatives of
leprosy treatment in the pre-and post-global leprosy elimination
era: appraisal of changing the scenario to current status. The
Journal of Dermatological Treatment 19, 8291.
Setia MS, Steinmaus C, Ho CS & Rutherford GW (2006) The role
of BCG in prevention of leprosy: a meta-analysis. The Lancet
Infectious Diseases 6, 162170.
Shams T, Setia MS, Hemmings R, McCusker J, Sewitch M &
Ciampi A (2010) Efficacy of black cohosh-containing preparations on menopausal symptoms: a meta-analysis. Alternative
Therapies in Health and Medicine 16, 3644.
Shepard CC, Walker LL, Van Landingham M & Redus MA
(1971) Kinetic testing of drugs against Mycobacterium leprae
in mice. Activity of cephaloridine, rifampin, streptovaricin,
vadrine, and viomycin. American Journal of Tropical Medicine
and Hygiene 20, 616620.
Shepard CC, Levy L & Fasal P (1972) Rapid bactericidal effect
of rifampin on Mycobacterium leprae. American Journal of
Tropical Medicine and Hygiene 21, 446449.
Shepard CC, Levy L & Fasal P (1974) Further experience with the
rapid bactericidal effect of rifampin on Mycobacterium leprae.
American Journal of Tropical Medicine and Hygiene 23,
11201124.
Shinde A, Khopkar U & Pai VV (2000) Single-dose treatment for
single lesion leprosy; histopathological observations [4].
International Journal of Leprosy and Other Mycobacterial
Diseases 68, 328330.
Shukla P, Miranda MS, Prabhudesai R & Rege VL (2002) Single
dose ROM therapy in Goa. Indian Journal of Leprosy 74,
169172.
Single-lesion Multicentre Trial Group (1997) Efficacy of single
dose multidrug therapy for the treatment of single-lesion
paucibacillary leprosy. Single-lesion Multicentre Trial Group.
Indian Journal of Leprosy 69, 121129.
Song F, Eastwood AJ, Gilbody S, Duley L & Sutton AJ (2000)
Publication and related biases. Health Technology Assessment
4, 1115.
1550
Sousa AL, Stefani MM, Pereira GA et al. (2007) Mycobacterium
leprae DNA associated with type 1 reactions in single lesion
paucibacillary leprosy treated with single dose rifampin, ofloxacin, and minocycline. American Journal of Tropical Medicine
and Hygiene 77, 829833.
Stanford JL (1994) The history and future of vaccination and
immunotherapy for leprosy. Tropical and Geographical
Medicine 46, 93107.
Talwar GP (1985) Vaccines against leprosy. Asian Pacific Journal
of Allergy and Immunology 3, 137139.
Ura S, Diorio SM, Carreira BG et al. (2007) Estudo terapeutico
comparando a associacao de Rifampicina, Ofloxacina e Minociclina com a associacao Rifampicina, Clofazimina e Dapsona
em pacientes com Hansenase multibacilar. Hansenologica
Internationalis 32, 5765.
Vijayakumaran P, Manimozhi N, Jesudasan K, Arunthathi S,
Jacob M & Samuel P (1997) Leucocytopenia after
rifampicin and ofloxacin therapy in leprosy. Leprosy Review
68, 1015.
Villahermosa LG, Fajardo TT Jr, Abalos RM et al. (2004)
Parallel assessment of 24 monthly doses of rifampin, ofloxacin,
and minocycline versus two years of World Health
Organization multi-drug therapy for multi-bacillary leprosy.
American Journal of Tropical Medicine and Hygiene 70,
197200.
Visschedijk J, van de Broek J, Eggens H, Lever P, van Beers S &
Klatser P (2000) Mycobacterium leprae millennium resistant!
Leprosy control on the threshold of a new era. Tropical
Medicine and International Health 5, 388399.
World Health Assembly (1991) Elimination of Leprosy:
resolution of the 44th World Health Assembly. World Health
Assembly.
World Health Organization (1982) Chemotherapy of Leprosy for
Control Programmes (No. 675). World Health Organization.
World Health Organization (1998) WHO Expert Committee on
Leprosy (1997). World Health Organization, Geneva.
World Health Organization (2010a) Global leprosy situation.
Weekly epidemiological record. http://www.who.int/wer/2010/
wer8535.pdf (accessed 19 October 2010).
World Health Organization (2010b) Leprosy elimination. http://
www.who.int/lep/en/index.html (accessed 19 October 2010).
World Health Organization (2010c) WHO Multidrug therapy
(MDT). http://www.who.int/lep/mdt/en/ (accessed 20 October
2010).
World Health Organization (2010d) WHO recommended MDT
regimens. http://www.who.int/lep/mdt/regimens/en/index.html
(accessed 20 October 2010).
Supporting Information
Additional Supporting Information may be found in the
online version of this article:
Table S1. Publication details, Inclusion exclusion criteria, description of study population, findings, side
effects reactions relapses and other characteristics of the
2011 Blackwell Publishing Ltd
Tropical Medicine and International Health
volume 16 no 12 pp 15411551 december 2011
M. S. Setia et al. ROM therapy in leprosy: a systematic review and meta-analysis
studies that compared ROM therapy with standard WHO
therapy.
Table S2. Description (place of study, study population
and treatment, outcomes and relapses) of the observational
studies using ROM therapy in the treatment of leprosy.
Please note: Wiley-Blackwell are not responsible for the
content or functionality of any supporting materials
supplied by the authors. Any queries (other than missing
material) should be directed to the corresponding author
for the article.
Corresponding Author Maninder Singh Setia, Consultant Dermatologist and Epidemiologist, Karanam Consultancy,
Ground Floor-66, Hi Life P M Road, Santacruz West Mumbai - 400 054, India. E-mail: maninder.setia@karanamconsultancy.in
2011 Blackwell Publishing Ltd
1551
Você também pode gostar
- Nej Mo A 1213096Documento9 páginasNej Mo A 1213096Lidya ChristyAinda não há avaliações
- HE PJKDocumento26 páginasHE PJKLidya ChristyAinda não há avaliações
- Drug and Multidrug Resistance Among Mycobacterium Leprae Isolates From Brazilian Relapsed Leprosy PatientsDocumento6 páginasDrug and Multidrug Resistance Among Mycobacterium Leprae Isolates From Brazilian Relapsed Leprosy PatientsLidya ChristyAinda não há avaliações
- Diagnosis Dan Pengobatan Reaksi Kusta Di Layanan Terpadu - Perspektif Pasien Di NepalDocumento1 páginaDiagnosis Dan Pengobatan Reaksi Kusta Di Layanan Terpadu - Perspektif Pasien Di NepalBernad NauliAinda não há avaliações
- Temporal Adverse Effects in Leprosy Saudi Patients Receiving Multi Drug Therapy 2161 1459-3-141Documento4 páginasTemporal Adverse Effects in Leprosy Saudi Patients Receiving Multi Drug Therapy 2161 1459-3-141Lidya ChristyAinda não há avaliações
- Dengue Guideline DengueDocumento33 páginasDengue Guideline DenguedrkkdbAinda não há avaliações
- Traumatic Brain Injury - Epidemiology, Classification, and PathophysiologyDocumento12 páginasTraumatic Brain Injury - Epidemiology, Classification, and PathophysiologyLidya ChristyAinda não há avaliações
- 08-04-15 Data MH Jan 2012 - Jan 2015Documento15 páginas08-04-15 Data MH Jan 2012 - Jan 2015Lidya ChristyAinda não há avaliações
- Is There A Role For Rifampicin, Ofloxacin and Minocycline (ROM) Therapy in The Treatment of Leprosy? Systematic Review and Meta-AnalysisDocumento11 páginasIs There A Role For Rifampicin, Ofloxacin and Minocycline (ROM) Therapy in The Treatment of Leprosy? Systematic Review and Meta-AnalysisLidya ChristyAinda não há avaliações
- Morning Report 21-5Documento14 páginasMorning Report 21-5Lidya ChristyAinda não há avaliações
- Morning Report 21-5Documento14 páginasMorning Report 21-5Lidya ChristyAinda não há avaliações
- Case Report Negative Rusell Body GastritisDocumento3 páginasCase Report Negative Rusell Body GastritisLidya ChristyAinda não há avaliações
- 1471 2334 13 456Documento8 páginas1471 2334 13 456Lidya ChristyAinda não há avaliações
- Spontaneous Intracerebral Hemorrhage - Treatment and PrognosisDocumento22 páginasSpontaneous Intracerebral Hemorrhage - Treatment and PrognosisLidya ChristyAinda não há avaliações
- Traumatic Brain Injury - Epidemiology, Classification, and PathophysiologyDocumento12 páginasTraumatic Brain Injury - Epidemiology, Classification, and PathophysiologyLidya ChristyAinda não há avaliações
- ACME Quote-Word 2003Documento4 páginasACME Quote-Word 2003Mutmainnah AGAinda não há avaliações
- Risk Factors For Severe Acute Lower Respiratory Tract Infection in Under-Five ChildrenDocumento10 páginasRisk Factors For Severe Acute Lower Respiratory Tract Infection in Under-Five ChildrenLidya ChristyAinda não há avaliações
- Overview of The Management of Epilepsy in AdultsDocumento29 páginasOverview of The Management of Epilepsy in AdultsLidya ChristyAinda não há avaliações
- Management of Acute Severe Traumatic Brain InjuryDocumento24 páginasManagement of Acute Severe Traumatic Brain InjuryLidya ChristyAinda não há avaliações
- Journal - Pone.0105785 AMI&ACIDocumento9 páginasJournal - Pone.0105785 AMI&ACILidya ChristyAinda não há avaliações
- What Is EdemaDocumento3 páginasWhat Is EdemaLidya ChristyAinda não há avaliações
- Design PPT (K)Documento20 páginasDesign PPT (K)Lidya ChristyAinda não há avaliações
- Spontaneous Intracerebral Hemorrhage - Treatment and PrognosisDocumento22 páginasSpontaneous Intracerebral Hemorrhage - Treatment and PrognosisLidya ChristyAinda não há avaliações
- Journal - Pone.0105785 AMI&ACIDocumento9 páginasJournal - Pone.0105785 AMI&ACILidya ChristyAinda não há avaliações
- Risk Factors For Severe Acute Lower Respiratory Tract Infection in Under-Five ChildrenDocumento10 páginasRisk Factors For Severe Acute Lower Respiratory Tract Infection in Under-Five ChildrenLidya ChristyAinda não há avaliações
- How Breast Milk Protects NewbornsDocumento4 páginasHow Breast Milk Protects NewbornsDennis HerreraAinda não há avaliações
- Cover Kasus 4-ForENSIKDocumento1 páginaCover Kasus 4-ForENSIKTri AriyaniAinda não há avaliações
- What Is EdemaDocumento3 páginasWhat Is EdemaLidya ChristyAinda não há avaliações
- Patofisiologi Ulkus VarikosumDocumento5 páginasPatofisiologi Ulkus VarikosumLidya ChristyAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (120)
- Tea CaffeineDocumento3 páginasTea CaffeinedigitaltextAinda não há avaliações
- Reflective Functioning: A ReviewDocumento11 páginasReflective Functioning: A ReviewNeilermind100% (1)
- Intravenous TherapyDocumento30 páginasIntravenous TherapyKoass14 2012Ainda não há avaliações
- LT 2 Members: Raazia Jalil, Ali Amjad & Ali Raza: Project 2 Doctors InterviewDocumento3 páginasLT 2 Members: Raazia Jalil, Ali Amjad & Ali Raza: Project 2 Doctors InterviewfatimaAinda não há avaliações
- ARTICLE - DR.S R PHATAK. Kinjal Dave - 4th BHMCDocumento2 páginasARTICLE - DR.S R PHATAK. Kinjal Dave - 4th BHMCᎧᎷ ᎴᏗᏉᏋAinda não há avaliações
- Biokimia NeurupsikiatriDocumento40 páginasBiokimia Neurupsikiatrisuyudi kimikoAinda não há avaliações
- Hospital PharmacyDocumento13 páginasHospital PharmacySridivya SrihariAinda não há avaliações
- Diabetic RetinopathyDocumento18 páginasDiabetic Retinopathymohelshiekh100% (3)
- Nursing Information SystemDocumento20 páginasNursing Information SystemShahad Hakimuddin100% (1)
- Instructions For Use CA 153Documento12 páginasInstructions For Use CA 153Benjamin MannAinda não há avaliações
- History of Physiological Psychology PDFDocumento14 páginasHistory of Physiological Psychology PDFYusril Abdan Nur100% (1)
- Prob PDFDocumento12 páginasProb PDFwallace120Ainda não há avaliações
- 4 2Documento39 páginas4 2Anonymous GWPdocUtAinda não há avaliações
- Nomina Anatomica VeterinariaDocumento177 páginasNomina Anatomica VeterinariaAnđelka PopovićAinda não há avaliações
- Multicare MC in ManualDocumento28 páginasMulticare MC in ManualTom TamponAinda não há avaliações
- Neuromuscular Blocking DrugsDocumento3 páginasNeuromuscular Blocking DrugsYogi drAinda não há avaliações
- Bacteriological Quality of Street Vended Food PanipuriDocumento5 páginasBacteriological Quality of Street Vended Food PanipuriYus EfendiAinda não há avaliações
- Congenital HypothyroidismDocumento36 páginasCongenital HypothyroidismRandi DwiyantoAinda não há avaliações
- Family Case Study On The Billones Family 1Documento63 páginasFamily Case Study On The Billones Family 1Ivy Mae DecenaAinda não há avaliações
- Application Technique Traction PDFDocumento25 páginasApplication Technique Traction PDFAZOZ 19Ainda não há avaliações
- Application Form 1Documento3 páginasApplication Form 1thienndhAinda não há avaliações
- Ground Floor PlanDocumento1 páginaGround Floor PlanjrsourisAinda não há avaliações
- Suprapubic Prostatectomy HinmanDocumento9 páginasSuprapubic Prostatectomy HinmanputriAinda não há avaliações
- 220200320sathiya PrakashDocumento95 páginas220200320sathiya Prakashpriya selvaraj100% (1)
- GUY Et Al 1994 - Regulation of Colostrum Formation in Beef and Dairy CowsDocumento6 páginasGUY Et Al 1994 - Regulation of Colostrum Formation in Beef and Dairy CowsMonique IndAinda não há avaliações
- Good Opinion Essay TopicsDocumento4 páginasGood Opinion Essay Topicsmywofod1nud2100% (2)
- Komposisi z350Documento9 páginasKomposisi z350muchlis fauziAinda não há avaliações
- Lumbar PunctureDocumento4 páginasLumbar Puncturerupali gahalianAinda não há avaliações
- Interpretation of MriDocumento12 páginasInterpretation of Mrijimitkapadia100% (1)
- Fullsize SBAR Report SheetDocumento1 páginaFullsize SBAR Report SheetShane LambertAinda não há avaliações