Escolar Documentos
Profissional Documentos
Cultura Documentos
01 Aplastic Anaemia
Enviado por
Sreekanth MenonDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
01 Aplastic Anaemia
Enviado por
Sreekanth MenonDireitos autorais:
Formatos disponíveis
supplement to Journal of the association of physicians of india Published on 1st of every month 1st march, 2015
Aplastic Anaemia
Mammen Chandy*
Director, Tata Medical Center,
14, MAR (EW) Newtown,
Rajarhat, Kolkata 700 156,
West Bengal
aul Ehrlich, who won the Nobel Prize in
1908 was the first to describe the entity
that we know today as Aplastic Anaemia:
he described the first case in 1888, in a
young woman who died of an abrupt
illness with severe anaemia, haemorrhage,
hyperpyrexia, and a hypocellular bone
marrow. 1 One hundred and twenty six
years later we still have a diagnosis of
Idiopathic Aplastic Anaemia where
we are unable to tell a young adult who
presents with catastrophic bone marrow
failure as to why this has happened and
speculate that there could have been some
insult (drug/infection) on an underlying
genetic defect which triggered an immune
response against the hematopoietic stem
cell. Since our understanding of the
aetiology in the individual patient is
uncertain the management algorithm is
also empiric. The severity of the disease
process based on the presenting blood
counts and marrow cellularity is defined
by International Aplastic Anaemia
Study Group Criteria 2,3 but the tempo
of the disease varies with some patients
presenting with mild chronic cytopenia
and others with a rapidly fatal disease.
It is believed that the incidence of
Aplastic anaemia is around 2-3/million
population from studies in the Western
world.4 The incidence of aplastic anaemia
is higher in Asia than in the West. A large
study from Thailand, conducted with
the same methodology and some of the
same personnel as the IAAAS, found
a rate of 3.9/million for the Bangkok
metropolitan area and 5/million in the
northeast region of Khonkaen. 5 There
is no epidemiological data on the true
incidence of Aplastic Anaemia from India
and we have to depend on hospital based
statistics. If we extrapolate the data from
Aoki6 then there would be 7200 new cases
of Aplastic Anaemia every year in India.
However many of these would probably
never be even diagnosed because of the
lack of facilities in peripheral hospitals.
the prototype of a disorder where there
is failure of the DNA repair processes
in the cell. 7 Our ability to diagnose
forme frustes of this disease by new
molecular techniques is important when
a patient with Fanconi anaemia is being
taken for stem cell transplantation. The
recent understanding of the telomere
and its abnormalities which result in
a variety of genetic disorders called
telomeropathies has allowed us to
understand the molecular basis of
Dyskeratosis congenita; the other genetic
disorder which causes aplastic anaemia. 8
Telomere shortening is present even
in patients with idiopathic aplastic
anaemia and this may be the underlying
problem increasing the likelihood that
an environmental insult can trigger
the immune response against the
haematopoietic stem cell. 9
There have been rapid advances in our
understanding of the molecular biology
of the inherited bone marrow failure
syndromes with Fanconi anaemia being
Aplastic anaemia is considered in any
patient with pancytopenia and a bone
marrow aspirate and trephine biopsy
are essential to confirm the diagnosis. 11
The exact cause of haematopoietic
failure in Aplastic anaemia in the
individual patient remains obscure and
we are still left with the dilemma of
whether it is a problem with the seed (the
haematopoietic stem cell) or the soil (the
microenvironment). Drugs and exposure
to chemical agents are implicated and
there is a long list of agents capable of
damaging the marrow. In about 10% of
patients previous viral hepatitis is linked
to the development of marrow failure. 10
There is considerable evidence to suggest
that in many patients immune mediated
mechanisms are responsible for marrow
failure: these include the association
with HLA, in vitro co-culture studies of
stem cells with T lymphocytes, failure
of engraftment in syngeneic stem cell
transplants without prior conditioning,
autologous recovery after allogeneic stem
cell transplantation and the successful
outcome after administration of anti
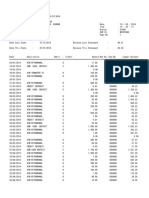
lymphocyte globulin to patients. Figure 1
illustrates the possible sequence of events
in immune mediated marrow failure.
supplement to Journal of the association of physicians of india Published on 1st of every month 1st march, 2015
Fig. 1 : The three panels above illustrate the possible sequence of events after interaction with a drug or virus with the
haematopoietic stem cell which results in an immune response which damages the haematopoietic stem cell either
directly by T cells or indirectly by cytokines or rarely antibody.
Stress testing to exclude FA is essential in all children:
tests for PNH and cytogenetic examination of the
bone marrow to exclude hypoplastic MDS is useful.
Screen for blood borne viruses is mandatory both
for the aetiology and since most patients have been
transfused.
Once a diagnosis has been established the following
treatment options are available today:
Haematopoietic stem cell transplantation
Therapy with Anti-lymphocyte (ALG) and Antithymocyte (ATG) immunoglobulin
Cyclosporine
Androgens and Danazol
The choice of the optimal therapy for the individual
patient remains empiric.
Haematopoietic stem cell transplantation if there is
a stem cell donor remains the treatment of choice for
young patient with very severe aplastic anaemia and it
is possible achieve disease free survival in the region of
85% in young patients.12,13 However many patients with
SAA in India present late, having received multiple
transfusions and are often septic: waiting for these
patients to stabilise when there are no neutrophils is
often of no use and the transplant should be performed
as quickly as possible under appropriate antimicrobial
cover.14 Logistics and resources are the most important
constraints. The use of fludarabine along with
cyclophosphamide has reduced rejection but graft
versus host disease remains a problem.15,16 ALG or ATG
would be the first line of treatment for older adults
with SAA who are not septic. The choice of the product
is important with data suggesting that horse ATG is
more effective than rabbit ATG.17 Some studies suggest
that ATGAM produced in India is comparable to the
Pfizer product but larger studies need to be done to
confirm this. 18 The exact mechanism by which ALG
and ATG work to restore haematopoiesis is unclear
since destruction of T-cells alone with monoclonal anti
T-cell antibodies is not effective. 19 Administration of
ALG/ATG to a sick aplastic anaemia patient requires
experience and adequate transfusion support and
management of infection. Response rates in the region
of 60% can be expected but some patients will have
clonal evolution to PNH and myelodysplastic (MDS)
syndrome. Cyclosporine is always administered for
3 to 6 months after ATG: however the drug can be
used as a single agent in patients with no severe
aplastic anaemia with responses in the region of
30-40%. 20 Preventing gingival hyperplasia and proper
control of drug induce hypertension is essential in
the patient with a low platelet count. The drug must
be tapered slowly if there is a response. There is an
association between HLA and cyclosporine response
and dependence. 21
There is a place for androgens in the management
of patients with non severe aplastic anaemia when
resources are limited and an occasional patient who
has failed other therapies responds to treatment. 22
Virilisation, hepatic dysfunction and premature
closure of the epiphyses in children are important
side effects. Danazol should be used in preference
to oxymethalone or stanozolol in females. There is
data that danazol may be useful in patients with
Dyskeratosis congenita. 23,24
Aplastic anaemia remains a challenging clinical
supplement to Journal of the association of physicians of india Published on 1st of every month 1st march, 2015
problem and early diagnosis and prompt institution
of the appropriate treatment for the individual
patients should be the goals for physicians in India.
The data and publications on Aplastic Anaemia from
India is limited and this issue of JAPI is an attempt to
bring together perspectives and data from different
haematologists from India.
References
1.
Ehrlich P. Ueber einem Fall von Anamie mit Bemer-kungen uber
regenerative Veranderungen des Knochenmarks. Charite-Annalen
1888;13:30109.
2.
Camitta BM, Rappeport JM, Parkman R, Nathan DG. Selection of
patients for bone marrow transplantation in severe aplastic anemia.
Blood 1975;45:355363.
3.
Bacigalupo A, Hows J, Gluckman E, Nissen C, Marsh J, Van Lint MT et
al. Bone marrow transplantation (BMT) versus immunosuppression
for the treatment of severe aplastic anaemia (SAA): a report of the
EBMT SAA working party. Br J Haematol 1988;70:177182.2.
4.
Young NS, Kaufman DW. The epidemiology of acquired aplastic
anemia. Haematologica 2008;93:489-492
5.
Issaragrisil S, Kaufman DW, Anderson T, Chansung K, Leaverton P,
Shapiro S et al. The epidemiology of aplastic anemia in Thailand.
Blood 2006;107:1299307
6.
Aoki K, Fujiki N, Shimizu H, Ohno Y: Geographic and ethnic differences
of aplastic anemia in humans, in Najean Y (ed): Medullary Aplasia.
New York, NY, Masson, 1980;79
7.
Dokal I and Vulliamy T. Inherited bone marrow failure syndromes.
Haematologica 2010;95
8.
Walne A,Dokal I. Advances in the understanding of dyskeratosis
congenita. Br J Haematol 2009;145:164-72.
9.
Calado RT, Cooper JN, Padilla-Nash HM, Sloand EM, Wu CO,
Scheinberg P et al. Short telomeres result in chromosomal instability
in hematopoietic cells and precede malignant evolution in human
aplastic anemia. Leukemia 2012;26:700707.
10. Brown KE, Tisdale J, Barrett J, Dunbar CE, Young NS. HepatitisAssociated Aplastic Anemia. N Engl J Med 1997;336:1059-1064
11. Rovo A, Tichelli A, Dufour C. Diagnosis of acquired aplastic anemia.
Bone Marrow Transplantation 2013;48:162167
12. Storb R, Leisenring W, Appelbaum FR, Buckner CD et al Long-Term
Follow-Up of Allogeneic Marrow Transplants in Patients With
Aplastic Anemia Conditioned by Cyclophosphamide Combined with
Antithymocyte Globulin. Blood 1997;89:3890-91.
13. George B, Mathews V, Viswabandya A, Lakshmi KM, Srivastava A,
Chandy M. Allogeneic hematopoietic stem cell transplantation is
superior to immunosuppressive therapy in Indian children with
aplastic anemia--a single-center analysis of 100 patients. Pediatr
Hematol Oncol 2010;27:122-31.
14. George B, Mathews V, Viswabandya A, Srivastava A, Chandy M.
Fludarabine-based reduced intensity conditioning regimens for
allogeneic hematopoietic stem cell transplantation in patients with
aplastic anemia and fungal infections. Clin Transplant 2009;23:228-32.
15. George B, Mathews V, Viswabandya A, Kavitha ML, Srivastava A,
Chandy M. Fludarabine based reduced intensity conditioning
regimens in children undergoing allogeneic stem cell transplantation
for severe aplastic anemia. Pediatr Transplant 2008;12:14-19.
16. George B, Mathews V, Viswabandya A, Kavitha ML, Srivastava A,
Chandy M. Fludarabine and cyclophosphamide based reduced
intensity conditioning (RIC) regimens reduce rejection and improve
outcome in Indian patients undergoing allogeneic stem cell
transplantation for severe aplastic anemia. Bone Marrow Transplant
2007;40:13-18.
17. Scheinberg P, Nunez O, Weinstein B, Scheinberg P, Biancotto SA,
O. Wu C, Young NS. Horse versus Rabbit Antithymocyte Globulin in
Acquired Aplastic Anemia. N Engl J Med 2011;365:430-438.
18. Chandra J, Naithani R, Ravi R et al. Antithymocyte globulin and
Cyclosporine in children with acquired aplastic anemia. Indian J
Pediatr 2008;75:229-2338.
19. Chandy M, Bradstock KF, Srivastava A, Apte S. Treatment of severe
aplastic anaemia with anti T-cell monoclonal antibody (WM48). Blood
1994;81:9.
20. Marsh J, Schrezenmeier H, Marin P, Ilhan O, Ljungman P, McCann
S et al . Prospective Randomized Multicenter Study Comparing
Cyclosporin Alone Versus the Combination of Antithymocyte Globulin
and Cyclosporin for Treatment of Patients With Non severe Aplastic
Anemia: A Report From the European Blood and Marrow Transplant
(EBMT) Severe Aplastic Anaemia Working Party. Blood 1999;93:21912195.
21. Nakao S, Takamatsu H, Chuhjo T, Ueda M, Shiobara S, Matsuda T, et al.
Identification of a specific HLA class II haplotype strongly associated
with susceptibility to cyclosporine-dependent aplastic anemia. Blood
1994;84:425761.
22. Najean Y, Pecking A, Le Danvic M. Androgen Therapy of Aplastic
Anaemia -A Prospective Study of 352 Cases. EJ Haematol 1979;22:343
356.
23. Jaime-Prez JC1, Colunga-Pedraza PR, Gmez-Ramrez CD, GutirrezAguirre CH, Cant-Rodrguez OG, Tarn-Arzaga LC, Gmez-Almaguer
D. Danazol as first-line therapy for aplastic anemia. Ann Hematol
2011;90:523-7.
24. Islam A, Rafiq S, Kirwan M, Walne A, Jamie Cavenagh, Tom Vulliamy,
Inderjeet Dokal. Haematological recovery in dyskeratosis congenita
patients treated with danazol. Br J Haematol 2013;162:854-6.
Você também pode gostar
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Prevalence of Peptic Ulcer in Patients Attending Kampala International University Teaching Hospital in Ishaka Bushenyi Municipality, UgandaDocumento10 páginasPrevalence of Peptic Ulcer in Patients Attending Kampala International University Teaching Hospital in Ishaka Bushenyi Municipality, UgandaKIU PUBLICATION AND EXTENSIONAinda não há avaliações
- SH210 5 SERVCE CD PDF Pages 1 33Documento33 páginasSH210 5 SERVCE CD PDF Pages 1 33Em sulistio87% (23)
- Shopnil Tower 45KVA EicherDocumento4 páginasShopnil Tower 45KVA EicherBrown builderAinda não há avaliações
- Go Ask Alice EssayDocumento6 páginasGo Ask Alice Essayafhbexrci100% (2)
- SMK Techno ProjectDocumento36 páginasSMK Techno Projectpraburaj619Ainda não há avaliações
- EC2 406006 001 EFE 0121 - Controgen Generator Excitation System Description - Rev - ADocumento29 páginasEC2 406006 001 EFE 0121 - Controgen Generator Excitation System Description - Rev - AAnonymous bSpP1m8j0n50% (2)
- MLT Torque Ring Field Make-Up HandbookDocumento44 páginasMLT Torque Ring Field Make-Up HandbookKolawole Adisa100% (2)
- Alternator: From Wikipedia, The Free EncyclopediaDocumento8 páginasAlternator: From Wikipedia, The Free EncyclopediaAsif Al FaisalAinda não há avaliações
- Small Signal Analysis Section 5 6Documento104 páginasSmall Signal Analysis Section 5 6fayazAinda não há avaliações
- LICDocumento82 páginasLICTinu Burmi Anand100% (2)
- Data Mining - Exercise 2Documento30 páginasData Mining - Exercise 2Kiều Trần Nguyễn DiễmAinda não há avaliações
- Business Testimony 3Documento14 páginasBusiness Testimony 3Sapan BanerjeeAinda não há avaliações
- Vodafone M2M Integrated M2M Terminals Overview BrochureDocumento4 páginasVodafone M2M Integrated M2M Terminals Overview BrochureJamie JordanAinda não há avaliações
- Tendernotice 1Documento42 páginasTendernotice 1Hanu MittalAinda não há avaliações
- Bank Statement SampleDocumento6 páginasBank Statement SampleRovern Keith Oro CuencaAinda não há avaliações
- E Nose IoTDocumento8 páginasE Nose IoTarun rajaAinda não há avaliações
- Load Sharing Strategies in Multiple Compressor Refrigeration SystemsDocumento8 páginasLoad Sharing Strategies in Multiple Compressor Refrigeration SystemsLiu YangtzeAinda não há avaliações
- Paul Milgran - A Taxonomy of Mixed Reality Visual DisplaysDocumento11 páginasPaul Milgran - A Taxonomy of Mixed Reality Visual DisplaysPresencaVirtual100% (1)
- UCAT SJT Cheat SheetDocumento3 páginasUCAT SJT Cheat Sheetmatthewgao78Ainda não há avaliações
- Palm Manual EngDocumento151 páginasPalm Manual EngwaterloveAinda não há avaliações
- Matrix of Consumer Agencies and Areas of Concern: Specific Concern Agency ConcernedDocumento4 páginasMatrix of Consumer Agencies and Areas of Concern: Specific Concern Agency ConcernedAJ SantosAinda não há avaliações
- Brief Curriculum Vitae: Specialisation: (P Ea 1. 2. 3. Statistical AnalysisDocumento67 páginasBrief Curriculum Vitae: Specialisation: (P Ea 1. 2. 3. Statistical Analysisanon_136103548Ainda não há avaliações
- Quantity DiscountDocumento22 páginasQuantity Discountkevin royAinda não há avaliações
- ACM2002D (Display 20x2)Documento12 páginasACM2002D (Display 20x2)Marcelo ArtolaAinda não há avaliações
- 950 MW Coal Fired Power Plant DesignDocumento78 páginas950 MW Coal Fired Power Plant DesignJohn Paul Coñge Ramos0% (1)
- Numerical Transformer Differential RelayDocumento2 páginasNumerical Transformer Differential RelayTariq Mohammed OmarAinda não há avaliações
- 9.admin Rosal Vs ComelecDocumento4 páginas9.admin Rosal Vs Comelecmichelle zatarainAinda não há avaliações
- Design of Flyback Transformers and Filter Inductor by Lioyd H.dixon, Jr. Slup076Documento11 páginasDesign of Flyback Transformers and Filter Inductor by Lioyd H.dixon, Jr. Slup076Burlacu AndreiAinda não há avaliações
- Accounting II SyllabusDocumento4 páginasAccounting II SyllabusRyan Busch100% (2)
- Human Resource Management by John Ivancevich PDFDocumento656 páginasHuman Resource Management by John Ivancevich PDFHaroldM.MagallanesAinda não há avaliações