Escolar Documentos
Profissional Documentos
Cultura Documentos
[60]
Enviado por
Vashish RamrechaDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
[60]
Enviado por
Vashish RamrechaDireitos autorais:
Formatos disponíveis
Artificial Organs
30(12):929948, Blackwell Publishing, Inc.
2006, Copyright the Authors
Journal compilation 2006, International Center for Artificial Organs and Transplantation
Numerical Simulation of Cardiovascular Dynamics
With Left Heart Failure and In-series Pulsatile
Ventricular Assist Device
Yubing Shi and Theodosios Korakianitis
Department of Engineering, Queen Mary University of London, London, UK
Abstract: This article presents a numerical model for
investigations of the human cardiovascular circulation
system response, where the function of the impaired left
ventricle is augmented by the pumping action of a pulsatile
ventricular assist device (VAD) connected in series to the
native heart. The numerical model includes a module for
detailed heart valve dynamics, which helps to improve the
accuracy of simulation in studying the pulsatile type VAD
designs. Simulation results show that, for the case with left
ventricular (LV) failure, the VAD support successfully
compensates the impaired cardiovascular response, and
greatly reduces the after-load of the diseased ventricle, thus
assisting possible recovery of the ventricle from the diseased condition. The effects of these conditions on pulmonary circulation are also shown. To investigate the effect of
different pumping-activation functions (VAD motion profiles) on the cardiovascular response, three different VAD
motion profiles are investigated. The numerical results
suggest that Hermitian type motion profiles (smooth
curves skewed toward early systole) have the advantage of
requiring minimum power to the VAD, and producing the
minimum after-load to the left ventricle, minimum ventricular wall stress, and minimum ventricular work to the
diseased ventricle; while sawtooth type motions need
slightly more power input, and induce slightly increased
aortic pressure in diastole, thus improving coronary
perfusion. Key Words: Numerical simulationCardiovascular dynamicsHeart failureVentricular dysfunctionPulsatileVentricular assist deviceHeart valve
dynamics.
Since their first surgical implantation in the 1960s,
ventricular assist devices (VADs) have greatly
helped in the treatment of heart failure, either as a
bridge to transplantation, or as a bridge to recovery,
while lately there is also mention of permanent
implantation (destination therapy) (1). Two kinds of
VADs are available for clinical usage now: the impeller pump types (which usually provide continuous
blood flow); and the displacement pump types (which
usually provide pulsatile blood flow). The impeller
pump type VADs have the advantage of producing
relatively larger volume rate of flows with lower pressures, while for relatively lower volume rate of flows
and higher-pressure applications the displacement
pump type of VADs are generally more suitable (1).
Additionally, the impeller pumps operate at higher
revolutions per minute and are thus limited by the
cavitation threshold and the maximum allowable
shear rates (1), while the displacement pumps are
larger, operate at lower reciprocations per minute,
and need relatively more complex control systems for
proper function. In recent years some researchers
also proposed the application of pulsatile impeller
pumps, producing the pulsatile flow by varying either
the rotating speed of the pump or the axial placement
of the impeller in its casing in a heart cycle (2,3). The
advantages and the disadvantages of the pulsatile and
nonpulsatile effects have been intensively discussed.
In supporting nonpulsatile perfusion, Saito et al. (4)
investigated the hepatic and renal function and
plasma renin levels in 15 healthy sheep under chronic
nonpulsatile circulation support, concluded that
neither functional nor histologic changes were
observed in major end organs, and stated that the
nonpulsatile devices can be used safely for long-term
support. Also Chow et al. (5) used near-infrared
Received March 2006; revised April 2006.
Address correspondence and reprint requests to Dr. Theodosios
Korakianitis (a.k.a. Theodosios Alexander), Department of Engineering, Queen Mary University of London, London E14NS, UK.
E-mail: t.alexander@qmul.ac.uk
929
930
Y. SHI AND T. KORAKIANITIS
spectroscopy to examine the relationship between
pump flow rate and cerebral hemodynamics during
pulsatile and nonpulsatile cardiopulmonary bypass in
40 patients, and concluded that pulsatile flow does
not increase cerebral blood flow or alter hemoglobin
concentration during cardiopulmonary bypass in
children. Recently, more pro-pulsatile perfusion evidence has been published. Sezai et al. (6) examined
the major organ function under the pulsatile and
nonpulsatile support by observing various physiological changes during 3-hour biventricular-assisted
circulation after acute myocardial infarction model in
pigs. They concluded that pulsatile pumping produced superior circulation in the kidney and liver,
and microcirculation at the cell level was superior as
well in early treatment of acute heart failure. Results
of other researchers also support similar conclusions
(7). In an invited editorial (8), ndar reviewed the
various aspects of this dispute, confirmed the advantages of pulsatile over nonpulsatile perfusion, and
also revealed that pulsatile roller pumps can not be
guaranteed to generate more hemodynamic energy
when compared with nonpulsatile pumps, concluding
that in order to achieve the full advantages of pulsatile perfusion physiological pulsatile pumps are
necessary.
In the past decades enormous numerical and
experimental investigations have been carried out
to improve VAD designs. As an economical and versatile tool in scientific research, numerical simulation has been extensively applied in the design and
analysis of VADs. The published articles on these
numerical simulation works can be classified into
two groups: those concentrated on developing the
numerical models, and those on the application of
the developed model to investigate the hemodynamic response in the cardiovascular system under
the support of various VADs. The current research
studies the interaction between the native cardiovascular system and pulsatile VADs. This article presents a detailed numerical model for the system
dynamics and belongs to the first group of studies.
Future articles will use these models to study
various cases of system response under physiological and pathological conditions with various VAD
designs, and these articles will belong to the second
group of studies.
Previous numerical studies of cardiovascular
dynamics under VAD assist concentrated on analyzing the system response and optimization of the
VAD design, so that most of these studies used relatively simple cardiovascular system models. In a
hierarchical series of articles Verkerke et al. (9)
coupled a cardiovascular system model, including
Artif Organs, Vol. 30, No. 12, 2006
the systemic circulation and the coronary circulation, and a pulsatile catheter pump type VAD
model, to study the influence of the VAD on the
native cardiovascular system. Other researchers
(2,10) simplified the cardiovascular system into a
Windkessel model or a Westkessel model combined
with the left heart, while some researchers developed complete cardiovascular system models
including both the systemic and pulmonary circulation (3,7,1113). From the point of view of accuracy,
the complete cardiovascular system model as well
as the complete VAD model are necessary in the
numerical simulation.
Among the above numerical models, some
studied the interaction between the native cardiovascular system and the nonpulsatile, impeller-type
VADs (3,13), some studied the impeller-type VADs
but changed the rotating speed of the impeller in
the heart cycle to produce pulsatile type VAD
action (2,3), and some investigated the assisting
action of the intra-aortic balloon pump or of displacement type pulsatile VADs (7,912). ndar (8)
suggested that physiological pulsatile pumps
provide the best hemodynamic VAD support
mechanism. To date the dynamic interaction of pulsatile and nonpulsatile rotary-type VADs with the
cardiovascular system has been systematically investigated with both numerical and experimental
studies, while for the physiological pulsatile type
VADs, only the traditional intra-aortic balloon
pump has been extensively studied with numerical
investigations (10,12) as well as experimental study
(14). Numerical study of other displacement type
VADs involve complex dynamic characteristics
(7,9,11) and thus received less attention, but due to
their special hemodynamic advantage they still need
further investigation.
The present article presents numerical models of
the cardiovascular system and of physiological type
pulsatile VADs, and investigates the interaction of
reciprocating valve pulsatile VADs with the native
cardiovascular system. Atrial contraction and heart
valve dynamics, which affect and contribute to the
pulsatility of the physiological flow, are specially considered in the model. Various types of prototype
models for reciprocating valve VADs can be found in
the literature (e.g., [15,16]). In these designs any type
of prosthetic heart valve (monoleaflet, bileaflet,
PTFE membrane, bioprosthetic, etc.) is mounted on
an annular magnet, and it is moved in a reciprocating
motion along the length of the VAD. The prosthetic
valve is closed and acts as a piston pump in one
direction of motion along the length of the VAD,
while it opens to let flow through the valve in the
CARDIAC DYNAMICS WITH PULSATILE VAD
931
(a)
(b)
(c)
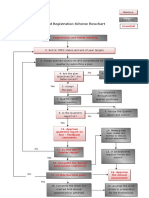
FIG. 1. Illustration of the simulation model. (a) Schematic of the native circulation system; (b) schematic of the reciprocating valve pump
type VAD; (c) illustration of typical forces acting on a heart valve leaflet.
reverse direction of motion along the length of
the VAD. Although both devices can be installed in
the traditional in-parallel configuration (in which the
VAD inlet is in the left ventricular (LV) apex, and the
VAD outlet is in the aorta), the designers of the
VADs mentioned above recommend the in-series
configuration (in which the VAD replaces a small
portion of the ascending aorta, as shown in Fig. 1a,b).
This in-series pulsatile VAD application closely
couples the VADs pumping action with the remaining contractile ability of the diseased ventricle, thus
achieving improved pumping efficiency, and may also
assist the recovery of the diseased ventricle. Thus, the
in-series configuration takes advantage of the work
of the native diseased ventricle, and in this way the
power consumption of the VAD is minimized. Also
the aiding function of the VAD can be increased if
necessary, decreased in the case of partial recovery of
the native ventricle, or stopped in case of full recovery (16). With these advantages in-series application
of these reciprocating valve types of VAD are good
prospects for clinical applications.
Artif Organs, Vol. 30, No. 12, 2006
932
Y. SHI AND T. KORAKIANITIS
MATERIALS AND METHODS
Model of the native cardiovascular system
A schematic of the native circulation system is
illustrated in Fig. 1a. The system is modeled in three
main parts: heart, systemic circulation loop, and pulmonary circulation loop. The heart is modeled as a
four-chamber pump with variable elastance and
four heart valves that control the blood flow direction. The systemic and pulmonary circulation loops
are each separated into aortic sinus/pulmonary
artery sinus, artery, arteriole, capillary and vein segments. In every segment the individual component
is modeled by considering the local resistance to
blood flow, elasticity of blood vessels, and inertia of
blood. The combined effect of venule, vein and vena
cava is modeled as the vein segment. The artery
segment represents the general characteristics of
both the main and smaller arteries. The aortic
sinus is separated from the artery to facilitate estimation of pressure response in the aortic arch. The
following models, figures, and equations include
repeating symbols. Definitions of all the symbols are
included in the nomenclature, while the values and
dimensions of the variables are included in the
tables.
Heart chambers
In modeling the heart, basic chamber characteristics are described with the pressure-volume relation
with the widely used Suga et al.s variable elastance
model (17), in which the chamber pressure is
described as a linear function of the chamber volume
and the chamber elastance. The chamber volume is
decided by the flow-rate difference between the inlet
and the outlet of the chamber, while the chamber
elastance varies in a heart cycle representing the
action of the heart muscle.
Take the left ventricle for example. The instantaneous volume change in the left ventricle is equal to
the flow-rate difference between mitral and aortic
valves:
dVlv
= Qmi Qao
dt
(1)
The time-varying ventricle elastance is a function
of the characteristic elastance (Elv,s and Elv,d) and an
activation function elv(t):
elv ( t ) = Elv,d +
Artif Organs, Vol. 30, No. 12, 2006
Elv,s Elv,d
elv ( t )
2
(2)
The activation function elv(t) describes the contraction and the relaxation changes in the ventricular
muscle. A commonly used activation function is
adopted:
1 cos t
Ts1
t Ts1
elv ( t ) = 1 + cos
Ts2 Ts1
: 0 t < Ts1
: Ts1 t < Ts2
(3)
: Ts2 t < T
The pressure in the left ventricle is then derived
from the instantaneous volume and elastance values
in the ventricle:
Plv = Plv,0 + elv (Vlv Vlv,0 )
(4)
The model for the right ventricle is similar to that
for the left side, except the values of parameters are
different. Modeling of the left and right atria are
similar to that for the ventricles, but with different
maximum and minimum chamber elastances and different activation function for the elastance change.
The activation functions for the left and right atria,
era(t) = ela(t), are set as:
t Tpwb
ela ( t ) = 1 cos
2
Tpww
: 0 t < Tpwb
: Tpwb t < Tpwb + Tpww
: Tpwb + Tpww t < T
(5)
Blood circulation loops
In modeling the various components of systemic circulation, depending on detailed local flow conditions,
the frictional loss, elastance, and blood inertia are
modeled as resistance, compliance, and inductance
effects, following the classical idea of electric-fluid
analog. The native systemic circulation loop is
divided into five parts: aortic sinus, artery, arterioles,
capillary, and vein. The artery is quite elastic, and the
flow is pulsatile in this segment, so that all the resistance, compliance, and inductance effects must be
considered. The aortic sinus has the similar characteristics as the artery segment, but in the simulation this
segment is greatly affected by the VAD, and thus, the
inertial and resistance effects is combined into the
consideration of the VAD dynamics. The arterioles
and capillaries are dominated by the resistance effect.
Veins function to collect and store blood, thus resistance and compliance effects are considered in the
vein model.
CARDIAC DYNAMICS WITH PULSATILE VAD
Pressure and flow-rate oscillations are experienced
in the aortic sinus due to the local tissue elastance
and result in important flow features related to coronary flow. The pressure is governed by:
dPsas Qao Qsas
=
dt
Csas
(6)
The pressure and flow-rate changes in the artery
are similar to that in the aortic sinus. As arterioles
and capillaries are both considered as pure resistance
units, their effects are integrated with the artery as
resistance units. Thus, the pressure equation is:
dPsat Qsas Qsat
=
dt
Csat
(7)
and the flow-rate equation is:
dQsat Psas Psvn ( Rsat + Rsar + Rscp ) Qsat
=
dt
Lsat
(8)
The systemic vein is modeled as a compliance combined with a resistance. In the vein the pressure is:
dPsvn Qsat Qsvn
=
dt
Csvn
(9)
and the flow rate is governed by:
Qsvn =
Psvn Pra
Rsvn
(10)
The pulmonary loop model is similar to that of the
systemic loop, with different values for system
parameters. Also as in the segment of the pulmonary
artery sinus all the resistance, compliance, and inertial effects are considered.
Heart valve
In the native heart there are four heart valves:
mitral, aortic, tricuspid, and pulmonary. In the reciprocating valve type of pulsatile VAD described above
the additional prosthetic-valve assists in the pumping
action and becomes part of the dynamic system.
Although the native and the prosthetic valves have
different geometries, their dynamic mechanisms of
operation are similar, so their basic heart valve model
is identical, but different values are adopted in the
parameters of the model to reflect the differences
among the individual valves.
In the physical system heart valve dynamics are
dominated by the bloodleaflet interaction effect
(18,19). Full description of this effect needs detailed
933
three-dimensional distributed-parameter modeling of
the pulsatile flow field around the valve and the valveleaflet deformation/motion (such as with computational fluid dynamics (CFD) studies). Previous studies
on the bloodleaflet interaction effect (18,19) are
mostly case specific, and cannot be used for overall
dynamic modeling of the whole cardiovascular system
as illustrated in Fig. 1a. As a novel contribution, this
article makes a compromise between the detailed
three-dimensional study and the simplified diode-like
description of the valve, using a concentratedparameter method to describe the bloodleaflet interaction effect. For this modeling purpose, the heart
valve is simplified as follows: a nominal leaflet opening
angle is used as an average of the variation of angular
position in the different parts of the elastic leaflet; the
detailed pressure and velocity distributions in the
valve are rounded and replaced with the averaged
pressure and flow rate before and after the valve. The
nominal leaflet opening angle is calculated by solving
the governing differential equation for the leaflet
dynamics, which takes into account the contribution
of the blood flow, while the corresponding leaflet
motion also drives the local pressure and flow-rate
changes around the valve. This concentratedparameter model of the bloodleaflet interaction
effect is less detailed than three-dimensional distributed parameter studies, but is an advancement over
the diode models, and it satisfies the need of the
present article to model the overall cardiovascular
system.
In the current model the basic pressure-flow relation in the aortic valve is described with an orifice
model:
CQao ARao Plv Psas
Qao =
CQao ARao Psas Plv
: Plv Psas
: Plv Psas
(11)
while the valve opening ARao is a function of the
angular position of the valve leaflets, as illustrated in
Fig. 1c:
ARao =
2
(1 cos )2
[ rao(1 cos )]
=
2
(1 cos max )2
[ rao(1 cos max )]
(12)
In Eq. 12, q is the leaflet opening angle. Zero (0
degrees) for q corresponds to the fully closed leaflet
position, and the maximum opening angle corresponds to the fully open leaflet position. q is computed by considering the various factors that affect
the leaflet motion. These include: the moment due to
the pressure difference across the valve; the moment
generated by the shear stress on the leaflet due to
Artif Organs, Vol. 30, No. 12, 2006
934
Y. SHI AND T. KORAKIANITIS
fluid flow; the moment produced by the frictional
force; and the moment generated by the vortex
near the valve leaflet surface, as shown in Fig. 1c.
Based on the CFD results of Hart et al. (18) and Shi
et al. (19), the shear stress force is much smaller than
the pressure force acting on the leaflet, so the shear
stress acted on the valve is neglected. The effect of
the vortex in the heart valve is an open question and
its contribution is still under investigation. Some
researchers proposed that the vortices influence the
valve closing process (20), but this argument needs
further validation, and it is the subject of future
investigations. Thus, in this article the vortex effect is
also neglected. Based on these considerations the following governing equation for the aortic leaflet
motion is derived:
Iao
d2
d
(13)
= kp,ao ( Plv Psas ) Aao cos kf,ao
dt 2
dt
The number of coefficients is minimized by substituting Kp,ao = kp,aoAao/Iao and Kf,ao = kf,ao/Iao:
d2
d
= K p,ao ( Plv Psas ) cos K f,ao
2
dt
dt
A dx + CQ AR
vad
vad
vad dt
: Psas Psat
Psas Psat
Qvad =
Avad dx + CQvad ARvad
dt
: Psas < Psat
Psat Psas
(14)
Model of Pulsatile VAD pumping action
and motion
Traditional pulsatile VADs such as the aortic
balloon pump and in-parallel installations of pneumatic diaphragm pumps have been applied in clinical
practice for many years, and numerous analyses have
been carried out to study their performance. The
model in this article concentrates on the in-series
action of reciprocating valve pulsatile-type VADs.
These have various different implementations as
illustrated by Larson et al. (15) and Korakianitis and
Grandia (16). These different implementations have
different driving mechanisms and control strategies,
which are beyond the scope of this article. As the
emphasis of the present article is on the fluid
dynamic interaction of the VAD and the native
cardiovascular system, the motion profile of the
pumping action is directly used in the current study.
Figure 1b illustrates the schematic of the reciprocating pump. Any type of prosthetic heart valve
(15)
When the VAD motion is properly designed flow
in the VAD chamber is continuous, so that:
Qvad = Qsas
The consideration of valve dynamics helps to
describe the regurgitant flow in the valve, thus
improving the accuracy of the simulation. Modeling
of the remaining three native heart valves, and of the
prosthetic valve in the VAD is implemented in the
same way, except the values of model parameters are
different.
Artif Organs, Vol. 30, No. 12, 2006
(leaflet, membrane, bioprosthetic, or other) is
mounted on an annular magnet inside a cylinder. In
the in-series configuration the length of the cylinder
replaces a portion of the length of the ascending
aorta. The annular magnet and valve assembly is
moved in a reciprocal fashion along the length of the
cylinder (via external electromagnetic coils [15] and
via an external magnet [16]). In either case the flow
through the prosthetic valve of the VAD can be
modeled by:
(16)
Motion of the pumping action is specified by the
VAD control algorithm. To have maximum VAD
working efficiency and minimum impact to the physiological function of the native cardiovascular system,
the pumping motion must be carefully designed. In
the current research, three pumping motion profiles,
illustrated in Fig. 2a, are examined, and their effects
on the native cardiovascular response are evaluated.
Figure 2b shows the three corresponding velocity
profiles. For easy comparison the electrocardiograph
(ECG) signal is shown in Fig. 2 and the characteristic
instances of 0, Ttwe, and T are specially marked with
dash-dot lines. (Comparisons of timing of these
motion profiles with later system-response figures
can be made with the ECG trace.)
The first motion profile is the sawtooth profile
adopted by Larson et al. (15):
X vad t
: 0 t Ttwe
Ttwe
x (t ) =
X vad X vad ( t Ttwe ) : Ttwe < t < T
T Ttwe
(17)
This motion profile is quite straightforward and
easy to implement in both the numerical model and
motion control algorithm. The general motion trend
also conforms to the ventricular motion, thus it helps
to reach a reasonable efficiency. However, in this
motion profile the VAD motion is not smooth (discontinuity in velocity and acceleration) at instants 0
CARDIAC DYNAMICS WITH PULSATILE VAD
(a)
935
(b)
FIG. 2. Pumping action profiles of the left ventricular assist device (LVAD). (a) Motion profiles of the LVAD; (b) velocity profiles of the
LVAD.
and Ttwe. This affects the system response, and also
increases the instantaneous system power requirement around these points. To improve the situation,
we propose two further motion profiles. First, we
propose the use of two segments of sine wave to
replace the sawtooth function (as shown in Fig. 2a).
With the sinusoidal profiles the slope of the motion
profile (the velocity) at instances 0 and Ttwe is specified to be 0 m/s:
X vad
2
x (t ) =
X vad
2
t
1 cos
Ttwe
: 0 t Ttwe
( t Ttwe )
1 + cos
T Ttwe
: Ttwe < t < T
(18)
The sine wave motion profile smooths the VAD
motion, and thus helps to lower the power requirement in the VAD specification. However, in the early
systole part of ventricular contraction of the native
healthy system the ventricular pressure increases
almost exponentially. In order to produce a similar
pressure response from the combined action of the
diseased heart and VAD pumping motion, we
propose a displacement profile that increases faster
than the sine wave in the early part of time between
t = 0 and t = Ttwe. In order to achieve this we propose
for the motion profile the Hermitian function
described below (and illustrated in Fig. 2a). There are
many types of Hermitian profiles that could be used,
but for the purposes of this article the displacement
and velocity in the motion of the VAD are specified
at time instants t = 0 s and t = Ttwe s. In addition, we
specify the position and slope of the motion profile at
an intermediate instant between t = 0 s and t = Ttwe s,
so that at t = Tr s the displacement is Xr m and the
velocity is Sr m/s. The return (nonpumping) motion
profile from Ttwe s to T s is the same as the sine wave.
Thus, the proposed two-segment Hermitian motion
of the pumping part of the profile for the VAD
becomes:
X 1 2 t Tr + S ( t T )
r
r
r
Tr
2
t
0 t Tr
T
r
t Tr
X r 1 2 T T +
r
twe
x (t ) =
2
S ( t T ) t Ttwe + X
vad
r
r
Tr Ttwe
2
t Ttwe t Tr
Tr < t Ttwe
1
Ttwe Tr Ttwe Tr
X vad
( t Ttwe )
1 + cos
Ttwe < t < T
T Ttwe
2
(19)
System parameters
In this work, most of hemodynamic variables used in
the numerical model of the cardiovascular system are
assigned values by referring to published materials.
Most researchers used variable elastance model to
describe the heart dynamics. By referring to parameter selection in Ursino (21) and Lu et al. (22) in the
current research, chamber elastance values are
assigned as shown in Table 1. Parameter settings as
shown in Table 2 for systemic and pulmonary loops
are based on the works of Ursino (21) and Lu et al.
(22). In modeling heart valve dynamics, coefficients
for valve motion equations are selected through
Artif Organs, Vol. 30, No. 12, 2006
936
Y. SHI AND T. KORAKIANITIS
TABLE 1. Parameters for the heart
Parameter
Value
Parameter
Value
Unit
CQao
CQmi
Elv,s
Elv,d
Plv,0
Vlv,0
Ela,max
Ela,min
Pla,0
Vla,0
350
400
2.5
0.1
1.
5.
0.25
0.15
1.
4.
CQpo
CQti
Erv,s
Erv,d
Prv,0
Vrv,0
Era,max
Era,min
Pra,0
Vra,0
350
400
1.15
0.1
1.
10
0.25
0.15
1.
4.
mL/(s mm Hg0.5)
mL/(s mm Hg0.5)
mm Hg/mL
mm Hg/mL
mm Hg
mL
mm Hg/mL
mm Hg/mL
mm Hg
mL
numerical experiments to find the optimal parameter
combinations that produce near physiological valve
motion process as described in literature of De Hart
et al. (18) and of Shi et al. (19), as shown in Table 3.
Other parameters such as systolic duration, beginning
instance and duration of the P wave in the ECG signal,
and the time step of simulation, etc., were chosen
based on general knowledge in physiological textbooks (23). Table 4 shows values for these parameters.
In assigning values to the VAD motion, the sectional
area of the cylinder is decided based on the human
aortic geometry and the VAD design, and the
maximum piston displacement is chosen based on the
normal stroke volume and the piston head area.
RESULTS
Based on the mathematical models described
above, a program is developed in C language to simu-
late the dynamic changes in the cardiovascular
system under various healthy, diseased, and VADsupported conditions. In the study, first, the normal
values are assigned to the cardiovascular variables to
reveal the physiological response in healthy condition; next, the LV characteristics are changed to simulate the pathological condition of LV failure. Based
on the LV failure condition, the reciprocating valve
pump as VAD with three kinds of motion profiles is
individually coupled with the diseased cardiovascular
model to study the dynamic response of the native
diseased cardiovascular system under VAD support.
Based on these results, important physiological variables such as pressure in the left atrium and the pulmonary vein, and some characteristic variables, such
as the power requirement for the VAD, and LV wall
stress, etc., are compared, to investigate the effect of
different motion profile design on the cardiovascular
TABLE 2. Parameters for the blood vessels
Parameter
Csas
Rsas
Lsas
Csat
Rsat
Lsat
Rsar
Rscp
Rsvn
Csvn
Vlv0
Value
Parameter
Value
Unit
0.08
0.003
0.000062
1.6
0.05
0.0017
0.5
0.52
0.075
20.5
800
Cpas
Rpas
Lpas
Cpat
Rpat
Lpat
Rpar
Rpcp
Rpvn
Cpvn
Vrv0
0.18
0.002
0.000052
3.8
0.01
0.0017
0.05
0.25
0.006
20.5
500
mL/mm Hg
mm Hg s/mL
mm Hg s2/mL
mL/mm Hg
mm Hg s/mL
mm Hg s2/mL
mm Hg s/mL
mm Hg s/mL
mm Hg s/mL
mL/mm Hg
mL
TABLE 3. Parameters for variable valve opening model
Parameter
Value
Parameter
Value
Unit
Kp,ao
Kf,ao
Kp,mi
Kf,mi
Kp,vad
Kf,vad
5500
50
6000
40
3500
25
Kp,po
Kf,po
Kp,ti
Kf,ti
5000
60
5800
45
rad/(s2 mm Hg)
L/s
rad/(s2 mm Hg)
L/s
rad/(s2 mm Hg)
L/s
Artif Organs, Vol. 30, No. 12, 2006
CARDIAC DYNAMICS WITH PULSATILE VAD
TABLE 4. Additional parameters
Parameter
Avad
DT
Elvf
T
Ts
Tpwb
Tpww
Tr
Ts1
Ts2
Ttwb
Ttwe
Ttww
Xvad
Xr
Value
0.0008
0.0001
0.5
1.
0.3
0.92
0.09
0.28
0.3
0.45
0.22
0.42
0.2
0.11
0.0605
Unit
2
m
s
mm Hg/mL
s
s
s
s
s
s
s
s
s
s
m
m
response. The heart period is chosen to be 1 s in the
simulation (60 beats per minute). In the simulation,
the system often reaches periodic solution after four
to five heart cycles of calculation. The converged
solution in the period from 10 to 11 s is chosen in
every simulated case for comparison of results. For
reference, the ECG signal is shown in some of the
figures, to facilitate comparison and illustration of the
timing in the cardiac cycle, and with the pumping
motion profiles in Fig. 2.
This article introduces the numerical model developed and presents some elementary results on the
hemodynamic response in the cardiovascular system
in the healthy, diseased, and assisted conditions. Only
representative baseline healthy and diseased conditions, with and without VAD support, are presented
in this article. The in-depth exploration of the effect
of each type of VAD on the cardiovascular system is
the topic of future works.
Response in healthy conditions
First, the simulation is carried out to simulate the
cardiovascular response under healthy conditions.
For this purpose the normal physiological values are
adopted in the model, and the VAD model is deactivated in the global model. Figure 3 shows the simulation results for pressure, flow rate, and volume
changes in the systemic and pulmonary circulation
loops under the healthy condition. In Fig. 3 it is
observed that these simulation results agree well with
the typical drawings for cardiovascular response
shown in textbooks such as Textbook of Medical
Physiology (23). The LV pressure is in the range of
0120 mm Hg, and the aortic pressure changes
between 80 and 120 mm Hg. Periodic peak flows exist
in the mitral and aortic flows, with average flow rate
of about 5 L/min. The LV volume change is approxi-
937
mately from 50 mL to 120 mL, with a stroke volume
of 70 mL. In the pulmonary circulation the cardiovascular response also matches the description in the
physiological textbooks. Accompanying the heart
valve closing motion in end systolic and diastolic
phases, there are reverse flows in the four valves,
which suggests the advantage of the current valve
dynamics model over previous simpler models.
Response with LV failure
To simulate the pathological condition of LV
failure, the value of the maximum elastance in the
left ventricle is changed from the normal value
of 2.5 mm Hg/mL to the much impaired value of
0.5 mm Hg/mL. Figure 4 illustrates the simulation
results for pressure, flow rate, and volume changes in
the systemic and pulmonary circulations under the
LV failure condition, which agrees with representative diseased heart results described by Guyton (23).
(Comparison between healthy response, diseased
response, and diseased response aided with three different VAD pumping profiles is also shown in Fig. 8.)
Generally, the cardiovascular response in the LV
failure condition follows the same trend as that in the
healthy condition, but the values for the physiological
variables change greatly. In Fig. 4a it is observed
that, under the LV failure condition, the aortic pressure range is reduced from the normal value of
80120 mm Hg to the current 4668 mm Hg, and the
peak systolic LV pressure is reduced from the normal value of 120 mm Hg to the current value of
68 mm Hg. This greatly impaired perfusion condition
will adversely affect the function of important organs
in the cerebral, renal, and hepatic subsystems. Also in
Fig. 4a,d, it is observed that pressures in the left
atrium and the pulmonary vein are elevated to about
14 mm Hg, almost increased 50% from the normal
value of about 9 mm Hg. The LV failure situation
simulated here is a mild case. When the LV failure
develops further, and the pressure of the pulmonary
vein is elevated to above 18 mm Hg, pulmonary
edema will manifest itself and serious consequence of
pulmonary failure will follow (23). In the flow-rate
response of Fig. 4b,e it is illustrated that peak flow
rates across the mitral and aortic valves are reduced
to about 60% of the normal healthy values. At the
same time, although there is no great change in the
peak flow rates in the tricuspid and pulmonary valves,
the flow rates drop faster from the peak. In the
volume response of Fig. 4c,f, it is observed that there
are prominent changes to all four chamber volumes
in the heart. (The computed volumes of the heart
chambers in the model are affected by the combined
effect of the equations in the numerical model, Eqs.
Artif Organs, Vol. 30, No. 12, 2006
938
Y. SHI AND T. KORAKIANITIS
(a)
(d)
(b)
(e)
(c)
(f)
FIG. 3. System response with cardiovascular model in healthy conditions. (a) Pressure, left heart; (b) flow rate, left heart; (c) volume, left
heart; (d) pressure, right heart; (e) flow rate, right heart; (f) volume, right heart.
114, and particularly by Eqs. 14.) The LV volume
varies between 139 mL and 192 mL, greatly elevated
from the normal healthy range of 50130 mL in the
healthy condition, and with a corresponding decrease
in the difference between the minimum and
maximum volumes. (The ventricular maximum to
minimum volume difference is slightly larger than the
ejected blood volume per heart beat, due to regurArtif Organs, Vol. 30, No. 12, 2006
gitant flows in the valves. In the physiological case
with heart failure, the heart rate would increase
accordingly to make up for lost volume pumped per
beat to maintain the total cardiac output required.)
The left atrial volume is also increased, from the
normal range of 4068 mL in the healthy condition,
to the current range of 5787 mL. These changes
suggest that the ventricular volume difference has
CARDIAC DYNAMICS WITH PULSATILE VAD
(a)
(d)
(b)
(e)
(c)
(f)
939
FIG. 4. System response of cardiovascular model with left ventricular failure. (a) Pressure, left heart; (b) flow rate, left heart; (c) volume,
left heart; (d) pressure, right heart; (e) flow rate, right heart; (f) volume, right heart.
been reduced from the normal 80 mL to the current
value of 53 mL, with corresponding decrease in
cardiac output, while at the same time prominent left
heart dilation has developed. Accompanying the dilation in the left heart, there is great volume reduction
in the right ventricle and atrium. These pathological
changes in the cardiovascular response need to be
remedied by medical intervention.
Response with pulsatile left ventricular assist device
(LVAD) support
To simulate the cardiovascular response in LV
failure condition with VAD support, the three VAD
motion profiles described by Eqs. 1719 are applied
to activate the reciprocating valve pump (LVAD) in
the numerical model. Figure 2a shows the three
motion profiles with the ECG signal as timing referArtif Organs, Vol. 30, No. 12, 2006
940
Y. SHI AND T. KORAKIANITIS
(a)
(d)
(b)
(e)
(c)
(f)
FIG. 5. System response with left ventricular failure and sawtooth type left ventricular assist device motion. (a) Pressure, left heart; (b)
flow rate, left heart; (c) volume, left heart; (d) pressure, right heart; (e) flow rate, right heart; (f) volume, right heart.
ence, and Fig. 2b shows the corresponding velocity
changes associated with the three motion profiles.
Figures 57 show the corresponding changes of pressure, flow rate, and volume with LV failure condition
assisted by the LVAD pumping action, operated
under these three motion profiles. Figure 8 compares
some important physiological variables, including
Artif Organs, Vol. 30, No. 12, 2006
pressures in the left atrium, left ventricle, systemic
artery, pulmonary vein, etc., and the pressure-volume
loop under the conditions of healthy, LV failure, and
LV failure assisted by LVAD. Figure 9a compares the
ideal power requirement of LVAD with different
motion profiles, and Fig. 9b illustrates the corresponding estimated LV wall stress changes.
CARDIAC DYNAMICS WITH PULSATILE VAD
(a)
(d)
(b)
(e)
(c)
(f)
941
FIG. 6. System response with left ventricular failure and sine type left ventricular assist device motion. (a) Pressure, left heart; (b) flow
rate, left heart; (c) volume, left heart; (d) pressure, right heart; (e) flow rate, right heart; (f) volume, right heart.
Comparing Figs. 57 with Figs. 3 and 4 illustrates
that LVAD assistance greatly improves the cardiac
function, and compensates the impaired cardiovascular response to almost match that in the normal
healthy condition. As shown in Figs. 57 parts (a)
and (d), the systemic arterial pressure under LVAD
support with the three different motion profiles
returns to the normal range of 80120 mm Hg, and
the pressures in the left atrium and the pulmonary
vein drop back to the normal value of about
9 mm Hg. The greatly dilated left heart chambers in
the LV failure situation are satisfactorily remedied,
as shown in part (c) of Figs. 57, and the compensated volume responses in the VAD assistance condition match that in the normal healthy condition of
Fig. 3c. (Here, the computed volumes of the heart
Artif Organs, Vol. 30, No. 12, 2006
942
Y. SHI AND T. KORAKIANITIS
(a)
(d)
(b)
(e)
(c)
(f)
FIG. 7. System response with left ventricular failure and Hermitian type ventricular assist device motion. (a) Pressure, left heart; (b) flow
rate, left heart; (c) volume, left heart; (d) pressure, right heart; (e) flow rate, right heart; (f) volume, right heart.
chambers in the model are affected by the combined effect of the equations in the numerical
model, Eqs. 119, and particularly by Eqs. 14.) The
shape of the aortic flow-rate response in the LVAD
assist condition, as shown in parts (b) of Figs. 57,
becomes smoother and is different from that of
Fig. 3b in the healthy condition. Nevertheless, the
volume changes as discussed above suggest that the
cardiac output is not impaired by the change in
Artif Organs, Vol. 30, No. 12, 2006
aortic flow. Besides successful compensation of
pressure and volume response discussed above,
other aspects of pressure, flow rate, and volume
response almost duplicate the native response in the
healthy condition. This suggests that under the three
motion profiles studied, from the theoretical point
of view, the reciprocating valve pump is a suitable
choice for LVAD support under the LV failure
condition.
CARDIAC DYNAMICS WITH PULSATILE VAD
(a)
(d)
(b)
(e)
(c)
(f)
943
FIG. 8. Comparison of cardiovascular system response under various conditions. (a) Left atrial pressure; (b) left ventricular pressure; (c)
pressure in ventricular assist device inlet; (d) pressure in systemic artery; (e) pressure in pulmonary vein; (f) pressure-volume loops.
To investigate the effect of different pumping
motion profiles on the cardiovascular response, the
characteristic variables of LVAD function are compared, as illustrated in Figs. 8 and 9. From Fig. 8a,e, it
is observed that LVAD assistance with any of the
three motion profiles can bring the elevated left atrial
and pulmonary vein pressures in LV failure back to
normal value of below 10 mm Hg. In terms of flow
rates and volumes in the cardiovascular system, the
difference among the three LVAD motion profiles is
minor. Among the three motion profiles, the Hermitian type motion induces the lowest peak LV pressure
(Fig. 8b). LV failure causes the peak LV pressure to
drop from the normal value of about 120 mm Hg to
Artif Organs, Vol. 30, No. 12, 2006
944
Y. SHI AND T. KORAKIANITIS
(a)
(b)
FIG. 9. Estimation of ventricular assist device (LVAD) characteristic variables. (a) Estimation of LVAD ideal power requirement; (b)
estimation of left ventricular wall stress.
68 mm Hg in the diseased condition. With LVAD
support the cardiac output is increased to normal
levels, while the left ventricle is working at a reduced
rate. Figure 8b illustrates that LV pressure can
remain lower while the LVAD support maintains
arterial pressure to normal levels (Fig. 8d). Some
clinical studies suggest that this opportunity to rest
may assist the diseased ventricle to regenerate.
Figure 8c illustrates that the pressure in the aortic
root (ventricular after-load), which is the same as the
pressure at the inlet to the LVAD, is greatly reduced
in the systolic phase, while it returns to normal levels
in the diastolic phase (the after-load in diastole helps
coronary perfusion). Among the three motion profiles, the Hermitian type motion produces the lowest
after-load to the diseased ventricle in the systolic
phase, and the after-load is reduced to about onefourth of that in the healthy condition and about one
half of that in the diseased condition. In terms of
ventricular after-load, the Hermitian type motion is
more beneficial for the recovery of the diseased
ventricle. The after-load returns to the normal value
in different stages of the diastolic phase, with the
sawtooth type motion restoring the after-load the
earliest, in early diastole. Thus, the sawtooth type
VAD motion is more helpful in promoting coronary
perfusion. From Fig. 8d it is observed that the application of LVAD generally restores the systemic
artery pressure, from the much impaired value in the
LV failure case, back to the normal range. Among the
three motion profiles, the Hermitian type motion
produced the smoothest pressure variation, and the
sawtooth type motion causes the highest systemic
artery pressure among the three. Figure 8f illustrates
the pressure-volume loops of the left ventricle under
the various conditions. The area enclosed inside the
Artif Organs, Vol. 30, No. 12, 2006
pressure-volume loop is the work performed by the
ventricle. From this it is estimated that ventricle
work, from maximum to minimum value, is for the
healthy state, diseased state, sawtooth, sine, and Hermitian profiles, respectively. Figure 9 compares the
LVAD ideal power requirement and the LV wall
stress changes in a heart cycle under the different
conditions. The ideal LVAD power requirement is
estimated from the power difference downstream
and upstream of the LVAD:
P = Psas Qsas Psat Qsat
(20)
Figure 9a shows that generally the three motion
profiles require similar power input, and the mean
power requirements in all the three cases are estimated to be below 2 W. For most of the heart cycle
the instantaneous power requirement is below 1 W
for all three motion profiles, while the sawtooth type
motion produces a peak power requirement of about
4 W. The peak power requirement occurs immediately before the QRS complex in the ECG wave; and
oscillations in instantaneous power requirement
occur soon after the end of the T wave in the ECG
signal, both of which correspond to changes in the
direction of motion of the VAD. The Hermitian type
motion produces two peak power requirements in
the heart cycle, one (of about 1.6 W in amplitude)
during the QRS complex, corresponding to the
pumping phase of the VAD; and a second (of about
the same amplitude) corresponding to the retreating
motion of the VAD. The sine type motion produces
the smoothest power requirement. Of course this
power requirement estimation is based purely on
hemodynamic response, and this does not include the
CARDIAC DYNAMICS WITH PULSATILE VAD
effects of other important factors such as electromagnetic LVAD efficiency, driving mechanism efficiency,
etc.
In Fig. 9b the LV wall stress is estimated based on
Laplaces theory for thin-wall shell structure (24).
The left ventricle is assumed to be a near spherical
shell, thus, the wall stress is approximately:
Plv Dlv2
4w (w + Dlv )
(21)
with the wall thickness to be w = 10 mm at peak
systole (2). The LV wall stress generally follows the
same trend as that of the LV pressure shown in
Fig. 8b. VAD assistance greatly reduces the wall
stress in the diseased ventricle, thus is beneficial for
the ventricle recovery from the diseased condition.
The Hermitian type motion produces the lowest wall
stress, and the sine type motion the highest.
DISCUSSION
This article presents numerical models for the
human cardiovascular system and for physiologically
pulsatile type VADs, and studies and compares the
predicted dynamic response of the human cardiovascular system under three conditions: healthy, LV
failure, and LV failure assisted by an LVAD. The
focus of the article is on presenting the numerical
model developed and predicting the hemodynamic
characteristics of the interaction between the native
cardiovascular system and the VAD under representative baseline conditions of healthy, diseased, and
diseased with VAD support. The cardiovascular
model includes the four heart chambers and their
activation, the systemic and pulmonary circulation
loops, and improved models for the four native heart
valves (predicting regurgitant valve flow). The VAD
model includes a realistic description of the pulsatile
pumping action and regurgitant flow generated by a
prosthetic valve, which acts as a pumping piston, but
is generic to all such pumping devices present in the
literature, as the model does not depend on the powering or control mechanism for the VAD. Detailed
consideration of the VAD control and driving mechanism varies with different implementations, such as
in the design of Larson et al. (15) (which uses an
electric-coil driving mechanism), and the design
of Korakianitis and Grandia (16) (which uses a
magnetic-hydraulic driving mechanism driven in turn
by an electric coil in order to fit within the constraints
of the human body). In either case, the detailed VAD
powering and control system are beyond the scope of
the current work.
945
As shown in Fig. 3 the healthy cardiovascular
system model accurately predicts left and right heart
pressures, heart chamber volumes, and flow rates.
For instance the LV pressure is between 80 and
120 mm Hg, the mean flow rates through the mitral
valve is 5 L/min, corresponding to 0.17 m/s for valve
size of 25 mm. The improved valve model predicts
regurgitant calve flows and pressure fluctuations
after aortic and pulmonary valve closure. (The pressure fluctuations are present in both aortic and pulmonary valve closure, but they are more prominently
shown on the pulmonary-side pressure plot as the
overall pressure is lower on the right heart.) The
volumes of the four chambers of the heart are also
accurately predicted.
The diseased system response under the condition
of LV failure is shown in Fig. 4. This condition is
simulated by a reduction in the maximum elastance
of the left ventricle. The numerical model again accurately predicts the reduction in pressures on the
left side of the heart, the increase in left heart
volumes, and the increased after-load on pulmonary
circulation.
Three different LVAD motion profiles (and corresponding pumping action profiles) are studied in this
article. The pumping action is effected by a prosthetic
valve which is placed to replace a portion of the
ascending aorta. The fluid dynamic model for this
valve is similar to the model used for the native heart
valves, and thus includes the effects of regurgitant
flows. The displacement and velocity profiles of the
pumping action are shown in Fig. 2. The response of
the diseased system (LV failure) as aided by the
LVAD is shown in Figs. 59. The results show that the
reciprocating valve VAD satisfactorily supports the
failing heart by restoring important physiological
variables to their values under healthy normal conditions, such as pressures in the pulmonary vein and
the aorta, the volume of the diseased ventricle
chamber, etc. This preliminary study shows that the
reciprocating valve VAD needs an ideal power consumption of about 1 W, with peak values in the region
of 24 W. Although this power estimation did not
consider the VAD pumping efficiency, the preliminary result is promising. Even if one takes into
consideration electromagnetic and fluid dynamic
losses in the operation of the VAD, these levels of
power consumption indicate that the reciprocating
prosthetic-valve type of pump has great potential in
energy conservation when compared with other
mainstream pulsatile VADs currently in the market.
By comparing the results for the three motion profiles, it is observed that Hermitian type VAD motion
as proposed in the current article helps to reach miniArtif Organs, Vol. 30, No. 12, 2006
946
Y. SHI AND T. KORAKIANITIS
mized ventricular wall stress, while the sine type
VAD motion helps to minimize the VAD power
requirement. These two types of VAD motion also
help to minimize the ventricular work. Minimizing
the ventricular work in the diseased ventricle helps
to unload the chamber and promote its recovery
process in bridge to recovery applications. The sawtooth type VAD motion produces slightly higher
ventricular wall stress and requires slightly more ventricular work, but at the same time it induces slightly
increased arterial pressure in diastole, thus aiding
coronary perfusion. In this sense the sawtooth type
VAD motion assists the ventricular recovery process
from another aspect. From these preliminary results
it is hard to judge which motion profile is superior.
There is evidence from the group of Papaioannou
et al. (25) that the lower the aortic compliance, the
greater the performance of the intra-aortic balloon
pumping. Also the detailed VAD driving and control
mechanism (electromagnetic, hydroelectromagnetic,
etc.) will affect the VAD efficiency and VAD power
requirement, thus the efficiencies of these different
implementations of the reciprocating valve VAD
need to be compared. For in-depth comparisons,
further investigation of the system response under
various conditions must be conducted, including different pathological situations like heart rate changes,
variation of aortic compliance and different seriousness of heart failure. These are the subject of future
investigations.
The ongoing discussion of pulsatile/nonpulsatile
perfusion has an enormous impact on VAD
development. ndar (8) reviewed the published
works and concluded that pulsatile perfusion is indispensable for normal function of the end organs. Thus,
in this article the action of a new design of prostheticvalve type VAD on an improved cardiovascular
model is presented and studied. This preliminary
work indicates that the powering requirement of the
prosthetic-valve type of pulsatile VAD is promising,
and that further research on these designs is
warranted. Several other researchers also worked on
numerical studies of the effect of pulsatile VADs on
the native cardiovascular system. Drzewiecki et al.
(7) studied the effect of an atrio-aortic pneumatically
driven VAD on the native cardiovascular system.
Both the systemic and the pulmonary loops were
included in the cardiovascular model, which was used
to evaluate the system response of mean aortic pressure, LV oxygen consumption, and stroke volume
changes with different time delay in VAD motion
timing. Barnea et al. (12) analyzed the effect of the
intra-aortic balloon pump VAD on a complete cardiovascular model, and studied the changing of inflaArtif Organs, Vol. 30, No. 12, 2006
tion and deflation times on the various cardiovascular
parameters of cardiac oxygen availability and consumption, mean diastolic pressure, peak systolic pressure, etc. Verkerke et al. (9) presented a combined
model of the cardiovascular system that includes the
systemic circulation, coronary circulation, and a pulsatile catheter type VAD. The model was used to
simulate the changes of LV and aortic pressures, and
coronary flow under three conditions of healthy,
heart infarction, and heart infarction with VAD
assist. De Lazzari et al. (11) constructed a combined
model of a pneumatic LVAD and an open-loop
circuit description of the systemic circulation, and
evaluated the changes of cardiac flow, pressurevolume area and cardiac mechanical efficiency with
different atrial and arterial pressures in the openloop circuit. These previous studies concentrated on
the analysis of the VAD effect and optimization of
VAD motion, and the numerical models used were
not the focus of the work presented. As a contrast in
the present article the emphasis is on the presentation of the improved cardiovascular model and the
introduction of the model for the new type of VAD.
In-depth analysis of VAD performance and VAD
motion optimization will be the topic of the next
stage of the work presented in this article.
Previous experimental studies of pulsatile VAD
performance (such as [14]) have revealed that the
timing in the pulsatile VAD motion has direct influence on VAD efficiency. In these studies the heart
valve opening and closure were often used as reference instances for VAD motion design. Nevertheless,
even in those studies with complete cardiovascular
system models (3,7,1113), the important feature of
detailed heart valve dynamics was not considered. In
these earlier studies the heart valves were mostly
described as an on/off diode combined with a resistance component. Such heart valve models neglect
the valve motion processes and therefore produce
inaccurate valve motion sequences. For pulsatile type
VADs, the valve motion is crucial to the effectiveness
of the motion profile designs, and thus to the VAD
optimization process. The current article presents an
improved numerical model, which includes the complete cardiovascular model and also detailed description of the heart valve dynamics, providing a better
platform for numerical study of pulsatile type VAD
performance. In addition, the present model can be
coupled with more-elaborate models of local circulations (renal, cerebral, etc.).
CONCLUSIONS
This article introduces numerical models for the
human cardiovascular system and for prosthetic-
CARDIAC DYNAMICS WITH PULSATILE VAD
valve pulsatile type VADs. Detailed heart valve
dynamics were considered in the modeling process,
which helps to improve the accuracy of simulation in
studying the pulsatile type VAD designs. The article
also compares the predicted dynamic response of the
human cardiovascular system under three conditions:
healthy, LV failure, and LV failure assisted by a
prosthetic-valve pulsatile LVAD, under three different motion profiles. The three motion profiles studied
are sawtooth, sine, and Hermitian. With the LVAD
support, the impaired cardiovascular response in the
LV failure condition is successfully compensated, and
the after-load of the diseased ventricle and of the
pulmonary-side circulation are greatly reduced, thus
helping the recovery of the ventricle from the diseased condition. It is found that the Hermitian type
pumping motion has the advantage of requiring
minimum power, and produces the minimum afterload, ventricular wall stress, and ventricular work to
the diseased ventricle. The sawtooth type pumping
motion needs slightly more power input, but induces
slightly increased artery pressure in diastole, thus
improving coronary perfusion.
Nomenclature
A = sectional area
C = compliance
CQ = flow coefficient
DT = time step
E, e = elastance
I = inertial moment of rotating
K, k = coefficient
L = inertance
M = mass
P = pressure
Q = flow rate
R = resistance
T = time; heart period
V = volume, velocity
X = stroke, displacement
w = wall thickness
q = rotating angle of valve leaflet, ventricular wall
stress
Subscripts
0 = initial value; offset value; value for unstressed
condition
ao = aortic valve
d = diastolic phase
e = elastance action
ea = elastance of atrium
ev = elastance of ventricle
f = frictional action
la = left atrium
947
lv = left ventricle
lvf = left ventricular failure
max = maximum value
min = minimum value
mi = mitral valve
p = effect of pressure force
par = pulmonary arterioles
pas = pulmonary artery sinus
pat = pulmonary artery
pcp = pulmonary capillary
po = pulmonary valve
pvn = pulmonary vein
pwb = beginning of P wave
pww = duration of P wave
r = a specified intermediate instant in early systole
ra = right atrium
rv = right ventricle
s = systolic phase
s1 = peak of systolic phase
s2 = end of systolic phase
sar = systemic arterioles
sas = systemic aortic sinus
sat = systemic artery
scp = systemic capillary
svn = systemic vein
ti = tricuspid valve
twb = beginning of T wave
twe = end of T wave
tww = duration of T wave
vad = ventricular assist device
REFERENCES
1. Reul HM, Akdis M. Blood pumps for circulation support.
Perfusion 2000;15:295311.
2. Vandenberghe S, Segers P, Meyns B, Verdonck P. Unloading
effect of a rotary blood pump assessed by mathematical
modeling. Artif Organs 2003;27:1094101.
3. Pekkan K, Frakes D, de Zelicourt D, Lucas CW, Parks WJ,
Yoganathan AP. Coupling pediatric ventricle assist devices to
the fontan circulation: simulation with a lumped-parameter
model. ASAIO J 2005;51:61828.
4. Saito S, Westaby S, Piggot D, et al. End-organ function during
chronic nonpulsatile circulation. Ann Thorac Surg 2002;74:
10805.
5. Chow G, Roberts IG, Edwards AD, et al. The relation between
pump flow rate and pulsatility on cerebral hemodynamics
during pediatric cardiopulmonary bypass. J Thorac Cardiovasc
Surg 1997;114:56877.
6. Sezai A, Shiono M, Orime Y, et al. Major organ function under
mechanical support: comparative studies of pulsatile and nonpulsatile circulation. Artif Organs 1999;23:2805.
7. Drzewiecki GM, Pilla J, Welkowitz W. Design and control
of the atrio-aortic left ventricular assist device based on o2
consumption. IEEE Trans Biomed Eng 1990;37:12837.
8. ndar A. Myths and truths of pulsatile and nonpulsatile perfusion during acute and chronic cardisc support. Artif Organs
2004;28:43943.
9. Verkerke GJ, Geertsema AA, Mihaylov D, Blanksma PK,
Rakhorst G. Numerical simulation of the influence of a left
Artif Organs, Vol. 30, No. 12, 2006
948
10.
11.
12.
13.
14.
15.
16.
17.
Y. SHI AND T. KORAKIANITIS
ventricular assist device on the cardiovascular system. Int J
Artif Organs 2000;23:76573.
Nitta S, Yoshizawa M, Yambe T, Tanaka M, Takeda H. A less
invasive emax estimation method for weaning from cardiac
assistance. IEEE Trans Biomed Eng 1995;42:116573.
De Lazzari C, Mimmo FR, Tosti G, Ambrosi D. A desk-top
computer model of the circulatory system for heart assistance
simulation: effect of an LVAD on energetic relationships
inside the left ventricle. Med Eng Phys 1994;16:97103.
Barnea O, Moore TW, Dubin S, Jaron D. Cardiac energy considerations during intraaortic balloon pumping. IEEE Trans
Biomed Eng 1990;17:17081.
Vollkron M, Shima H, Huber L, Wieselthaler G. Interaction of
the cardiovascular system with an implanted rotary assist
device: simulation study with a refined computer model. Artif
Organs 2002;26:34959.
Barnea O, Smith BT, Dubin S, Moore TW, Jaron D. Optimal
controller for intraaortic balloon pumping. IEEE Trans
Biomed Eng 1992;39:62934.
Larson CO, Smith JS, Chapman JH, et al. Reciprocating
pumps and linear motor arrangement. Patent No.: US
5,879,375, United States Patent, March 9 1999.
Korakianitis T, Grandia L. Optimized pulsatile flow ventricular assistance device and total artificial heart. Patent No.: US
6,632,169, United States Patent, October 14, 2003.
Suga H, Sagawa K, Shoukas AA. Load independence of the
instantaneous pressure-volume ratio of the canine left ven-
Artif Organs, Vol. 30, No. 12, 2006
18.
19.
20.
21.
22.
23.
24.
25.
tricle and effects of epinephrine and heart rate on the ratio.
Circ Res 1973;XXXII:31422.
De Hart J, Paters GWM, Schreurs PJG, Baaijens FPT. A
three-dimensional computational analysis of fluidstructure
interaction in the aortic valve. J Biomech 2003;36:10312.
Shi YB, Zhao Y, Yeo JH, Hwang NHC. Numerical simulation
of opening process in a bileaflet mechanical heart valve under
pulsatile flow condition. J Heart Valve Dis 2003;12:24556.
Bellhouse BJ. The fluid mechanics of heart valves. In: Bergel
DH, eds, Cardiovascular Fluid Dynamics, Vol. 1, Chapter 8.
London: Academic Press, 1972;26185.
Ursino M. A mathematical model of the carotid baroregulation in pulsating conditions. IEEE Trans Biomed Eng 1999;46:
38292.
Lu K, Clark JW, GhorBel FH, Ware DL, Bidani A. A human
cardiopulmonary system model applied to the analysis of the
valsalva maneuver. Am J Physiol (Heart Circ Physiol) 2001;
281:H266179.
Guyton AC. Textbook of Medical Physiology. Philadelphia:
W.B. Saunders Company, 1986.
Fung YC. Biodynamics: Circulation. New York: SpringerVerlag, 1984.
Papaioannou TG, Mathioulakis DS, Stamatelopoulos KS, et al.
New aspects on the role of blood pressure and arterial stiffness
in mechanical assistance by intra-aortic balloon pump: in-vitro
data and their application in clinical practice. Artif Organs
2004;28:71727.
Você também pode gostar
- Piping FormulaeDocumento9 páginasPiping FormulaeVashish RamrechaAinda não há avaliações
- Steel Beam BS 5950Documento17 páginasSteel Beam BS 5950Vashish RamrechaAinda não há avaliações
- Max Allowable Pressure of Pipes and Pipellines CER 04022013 1 (V. S. Kumar Unprotected)Documento106 páginasMax Allowable Pressure of Pipes and Pipellines CER 04022013 1 (V. S. Kumar Unprotected)Vashish Ramrecha100% (1)
- In-Text: (Nickerson and Buist, 2008) Bibliography: Nickerson, D. and Buist, M. (2008) - Practical Application of Cellml 1.1: The IntegrationDocumento1 páginaIn-Text: (Nickerson and Buist, 2008) Bibliography: Nickerson, D. and Buist, M. (2008) - Practical Application of Cellml 1.1: The IntegrationVashish RamrechaAinda não há avaliações
- ISA SymbolsDocumento1 páginaISA SymbolsmustafasandikciAinda não há avaliações
- Roll 2015Documento26 páginasRoll 2015Vashish RamrechaAinda não há avaliações
- Gantt ChartDocumento6 páginasGantt ChartVashish RamrechaAinda não há avaliações
- CH-4 Shells Under External PressureDocumento64 páginasCH-4 Shells Under External PressureVashish RamrechaAinda não há avaliações
- Legacy ECSA ProfEng Appform TESDocumento1 páginaLegacy ECSA ProfEng Appform TESVashish RamrechaAinda não há avaliações
- Steel Cals SimpleDocumento53 páginasSteel Cals SimpleVashish RamrechaAinda não há avaliações
- E C S A: DeclarationDocumento1 páginaE C S A: DeclarationVashish RamrechaAinda não há avaliações
- The Gurney Flap: A Case Study: 1.1 Issues in Wing DesignDocumento9 páginasThe Gurney Flap: A Case Study: 1.1 Issues in Wing DesignVashish RamrechaAinda não há avaliações
- SRS Flowchart of ProcessDocumento1 páginaSRS Flowchart of ProcessVashish RamrechaAinda não há avaliações
- Formula Sheet 2007Documento3 páginasFormula Sheet 2007Vashish RamrechaAinda não há avaliações
- Development of A SemiDocumento4 páginasDevelopment of A SemiVashish RamrechaAinda não há avaliações
- 4.2d - 4.6bDocumento21 páginas4.2d - 4.6bVashish RamrechaAinda não há avaliações
- Nations Cup TimetableDocumento60 páginasNations Cup TimetableVashish RamrechaAinda não há avaliações
- Pressure-Volume Loops: Feasible For The Evaluation of Right Ventricular Function in An Experimental Model of Acute Pulmonary Regurgitation?Documento6 páginasPressure-Volume Loops: Feasible For The Evaluation of Right Ventricular Function in An Experimental Model of Acute Pulmonary Regurgitation?Vashish RamrechaAinda não há avaliações
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)