Escolar Documentos
Profissional Documentos
Cultura Documentos
1 285 1 PB
Enviado por
Vmiguel LcastilloTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
1 285 1 PB
Enviado por
Vmiguel LcastilloDireitos autorais:
Formatos disponíveis
Original Article
A Study of Antibiotics Self-Medication at Primary
Health Care Centers in Shiraz, Southern Iran
Mehrdad Askarian1,
Mohsen Hosseingholizadeh
Mahani2,
Mina Danaei3,
Mohsen Momeni2
1
Department of Community
Medicine, Medicinal & Natural Products
Chemistry Research Center,
Shiraz University of Medical Sciences,
Shiraz, Iran;
2
Student Research Center,
Shiraz University of Medical Sciences,
Shiraz, Iran;
3
Department of Community Medicine,
Shiraz University of Medical Sciences,
Shiraz, Iran
Correspondence:
Mehrdad Askarian, M.D., M.P.H.,
Professor of Community Medicine,
Department of Community Medicine,
Shiraz University of Medical Sciences,
P. O. Box: 71345-1737, Shiraz, Iran
Tel: +98-917-1125577
Fax: +98-711-2354431
Email: askariam@sums.ac.ir
Received: 2 January 2013
Revised: 4 March 2013
Accepted: 16 May 2013
Abstract
Background: Nowadays, self-medication of therapeutic agents is
of global concern particularly in developing and underdeveloped
countries. Some studies conducted in Iran showed that the
frequency of self-medication was significant.
Objective: This research was conducted to estimate the
prevalence of arbitrary use of antibiotics in Shiraz community
with special interest in its determinant factors.
Methods: This cross-sectional study was conducted in Shiraz, in
2009. Approximately 710 out of all patients referred to all health
care centers in Shiraz were selected to fill out a questionnaire
containing 23 questions divided into two parts. The frequency of
self-medication according to demographic factors was described
and the association between independent variables and selfmedication was analyzed.
Results: The frequency of self-medication in this study was
44.5% and the request to prescribe antibiotics by the patients
was 53.5%. Amoxicillin was the most widely used drug by
the participants. There was a significant association between
age and gender with self-medication. The frequent cause for
self-medication was common cold. Approximately, 74.4% of
the participants reported their previous experience as the main
reason for self-medication.
Conclusion: The results of this survey demonstrated the
high frequency of self-medication in Shiraz. Socio-cultural
determinants are the etiologic factors for self-medication.
Policy makers are recommended to provide community-wide
educational programs to make people aware about the adverse
effects of self-medication. There was a significant association
between age, gender and education with self-medication and
governments could pay more attention to these factors for
designing the interventional programs.
Please cite this article as: Askarian M, Hosseingholizadeh Mahani M, Danaei
M, Momeni M. A Study of Antibiotics Self-Medication at Primary Health Care
Centers in Shiraz, Southern Iran. J Health Sci Surveillance Sys. 2013;1(1):1-5.
Keywords: Self-medication; Antibiotics; Prevalence; Iran
Introduction
Nowadays, self-medication of therapeutic agents
is a global concern particularly in developing and
underdeveloped countries.1 Self-medication with
antibiotics is defined as the use of antibiotics to
treat disorders without physicians prescription and
clinical indication. The reuse of prescribed drugs for
J Health Sci Surveillance Sys July 2013; Vol 1; No 1
recurrent sign and symptoms and chronic disorders
is also included in this definition.1, 2 Improper and
incomplete use of drugs can affect the community
as well as individuals. Adverse effects of antibiotics
and allergic reactions are very common and
might threaten the patients life. Self-medication
in infectious diseases can increase the antibiotic
resistance and its following complications.2-4
1
Askarian M, Hosseingholizadeh Mahani M, Danaei M, Momeni M
Poverty and lack of insurance are the two
main factors associated with self-medication,
prominently in the low income countries. Many
diagnostic and therapeutic procedures have
dramatic costs and the price of many legal drugs
is extremely high, leading to the patients selfmedication.5,6 Physical access to health care
services and the patients residence (urban
or rural) are important in both developed and
developing countries.6,7
Generally, some patients administer the
previously-effective and acceptable prescribed
drugs for their new disease with the same sign and
symptoms or their recurrent or chronic diseases.
The drugs prescribed for the previous disease
and left out in the household are the common
source for many self-medication therapies. 3, 8, 9
Lack of regulation and enforcement, availability of
over-the-counter antibiotics, and high prevalence
of communicable and infectious diseases are
noticeable in developing countries.1
Few studies have been conducted in Iran on
this important issue, showing that the frequency
of self-medication is significant.9-12 Analgesic and
antibiotic drugs were the most frequently used
drugs requested by patients as over-the-counter
drug in pharmacies, respectively.9, 12 To the best
of our knowledge, there is no study carried out in
Shiraz about the frequency of self-administration
of antibiotics and its determinants especially as
a population-based study. This research was
conducted to estimate the prevalence of arbitrary
use of antibiotics in Shiraz community focusing
on its determinant factors.
Materials and Methods
This cross-sectional study was conducted in Shiraz,
2009 where there are 71 government and private
healthcare centers. Based on the sample size
formula, 710 out of all patients referred to all health
care centers in Shiraz were selected during one
month. The first ten patients in each center were
selected using convenience sampling to answer
the questionnaires. Oral informed consent was
obtained from the participants. If the patient did not
accept to participate in this study, we selected the
next patient until our sample size was completed.
Patients older than 18years old who were able
to visit the physician independently and use the
drugs were included in this study. Disabled or
dependent patients were excluded. The authors
helped the participants with low literacy to fill out
the questionnaire.
The self-reported questionnaire was designed
by authors. The validity of the questionnaire
was checked by expert opinion. Some expert
professors in medical field and some expert
2
professors in pharmacotherapy were consulted
to improve the validity of the questionnaire. The
reliability analysis (-Cronbach= 0.8) showed that
the questionnaire was reliable. The questionnaire
contained 23 questions divided into two parts.
Firstly, the participants were asked about their
demographic characteristics (age, gender, marital
status, job, family number, family income, and their
level of education). The participants educational
level considering the number of years that they
spent in education (<12 year, 12 year, 13-16 year, 17
year) was categorized. Moreover, if the participants,
their family members or their near friends jobs
were health-related (health care workers, nurses,
etc.), they were asked in three separate questions.
The status of the patients insurance was asked.
If the participants answered yes to the questions
about self-medication or requested the doctors to
prescribe antibiotics for them, the second part of
the questionnaire was filled out.
The kind of illness (diarrhea, common cold,
urinary tract infection, toothache, etc.), the person
suggesting the participants to administer antibiotics
(family members, friends, pharmaceutics, etc.),
the resource of drug provision (drugstore, family
members, friends, storage drugs at home, etc.),
the cause of self-medication (distant location,
lack of willingness to pay, inability to pay, crowded
clinics, etc.), the name of antibiotics used, the
source of the information about the method of
antibiotic consumption (family members, friends,
pharmaceutics, the brochure of the drug, etc.),
the type of antibiotics (pill, capsule, syrup,
injection, etc.), and the period that the participants
continued their self-medication (until the cure of
illness and recovery) were all included in the
second part of the questionnaire. The patients
request from physicians to prescribe a specific
antibiotic and its determinants were studied in
this survey.
The participants that did not answer more
than two questions were excluded from the study.
The frequency of self-medication according to
demographic factors was described and the
association between independent variables
and self-medication was analyzed using Chisquared test. To determine the predictors of
self-medication, multivariable logistic regression
analyses were performed using SPSS, version 15.
The statistical significance level was considered
as less than 0.05.
Results
Seven hundred and ten patients participated in this
study. Of self-completed questionnaires, 667 had
eligible criteria for analyzing the data (response
rate: 93.9%). The frequency of self-medication in
J Health Sci Surveillance Sys July 2013; Vol 1; No 1
Antibiotics self-medication in Shiraz
the previous year of the study was 44.5% (297
subjects) among the participants and the request
to prescribe antibiotics by the patients was 53.5%
(349 cases).
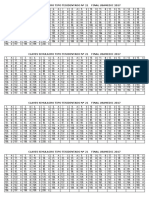
Table 1 shows the association between
demographic factors and other independent
variables in this study and the self-medication
behavior. Among different independent variables,
there was only a significant association between
age and gender with self-medication. Age was
significantly related to the patients request for
antibiotics to be prescribed by the physician but other
variables did not reveal any significant correlation.
The frequent causes for self-medication
were common cold (62.8%), sore throat (45.1%),
toothache (22.9%), rhinorrhea (16.5%), urinary
tract infection (14.5%), otitis media (7.4%),
diarrhea (4.7%) and other disorders (10.1%),
respectively.
Participants who reported their previous
experience as the main reason for self-medication
comprised 74.4% of all. Some of the participants
(11.7%) consulted with their family members
or friends and 8% of them with pharmacies
suggesting them to administer antibiotics. Overall,
213 (71.7%) of the participants prepared their drug
from drugstores. Approximately, 107 cases (36%)
took the medication from the storage of drugs
at home and 10 (3.3%) patients prepared drugs
from their family and friends. The participants
explained that their self-medication behavior
was due to previous experience on the efficacy of
treatment (41%), inability to access the physician
(30.9%), inability to pay for the expenses (21.8%),
and lack of willingness to pay (16%).
216 participants (72.5%) reported taking
antibiotics until recovery and 81(27.5%) cases
reported continuous treatment until the completion
of antibiotics therapy. Amoxicillin was the most
widely used drug by the participants (63.7%).
Ampicillin (19.9%), cephalexin (19%), penicillin
(16.7%), cotrimoxazole (6.9%), and ciprofloxacin
(5.2%) were the most frequently used drugs by
the participants, respectively.
The results from logistic regression analysis
did not show any statistically significant
association between independent variables and
self-medication of antibiotics.
Discussion
The results of this survey demonstrated the high
frequency (45.5%) of self-medication in Shiraz. The
results of the studies in Iran and other developing
countries including southern and eastern
Mediterranean countries are consistent with those
of this study.10-14 Compared to other countries, the
frequency of self-medication in this country is high
and noticeable. In European countries, it was lower
than that in Iran and the prevalence range was
Table 1: The association between independent variables and self-medication and request of antibiotics from physicians
Self-medication
Request of antibiotics from physician
Yes N (%)
No N (%)
P value
Yes N (%)
No N (%)
P value
Age (years)
0.033
0.007
18-23
43(45.7)
51(54.3)
41(45.1)
50(54.9)
24-29
92(52.3)
84(47.7)
101(59.1)
70(40.9)
30-35
49(38.9)
77(61.1)
66(53.2)
58(46.8)
36-41
38(51.4)
36(48.6)
50(67.6)
24(32.4)
>41
63(37.7)
104(62.3)
75(46.3)
87(53.7)
Gender
0.025
0.135
Female
138(40.1)
206(59.9)
187(56.3)
145(43.7)
Male
156(48.8)
164(51.2)
160(50.5)
157(49.5)
Marital status
0.343
0.862
Married
206(43.7)
265(56.3)
253(54.4)
Single
83(45.9)
98(54.1)
88(51.2)
84(48.8)
Divorced
2(100)
0(0.0)
1(50)
1(50)
Widow
2(66.7)
1(33.3)
2(66.7)
1(33.3)
Job
0.8
0.422
Related to medicine
21(45.7)
25(54.3)
22(48.9)
23(51.1)
Unrelated to medicine
237(47.4)
263(52.6)
269(55.1)
219(44.9)
Education (years)
0.074
0.887
<12
52(40.3)
77(59.7)
67(53.6)
58(46.4)
12
111(41.1)
159(58.9)
138(52.3)
126(47.7)
13-16
110(52.6)
99(47.4)
114(55.3)
92(44.7)
44
11(36.7)
19(63.3)
17(56.7)
13(43.3)
Health Insurance
0.605
0.887
Yes
259(44.3)
326(55.7)
310(53.9)
265(46.1)
No
38(46.3)
44(53.7)
39(50.6)
38(49.4)
J Health Sci Surveillance Sys July 2013; Vol 1; No 1
Askarian M, Hosseingholizadeh Mahani M, Danaei M, Momeni M
0.1-37% in Cyprus and Lebanon, respectively.13
According to this study, more than two thirds
of the participants provided their drug from
drugstores. Lack of strict rules and regulations
on drug distribution and insufficient monitoring
and evaluation can account for the existing
status. The strong regulatory systems with
penalties are needed to reduce this problem.
Pharmacists should be prevented from delivering
non-prescribed drugs to the clients. Previously
prescribed antibiotics stored at homes were
the other main resource. These results were
in the same line as other studies in European,
American and Asian countries.3, 8Other studies
in Iran showed that drug storage was frequent
among Iranians.12 Perhaps, the dose of antibiotics
prescribed by physicians was more than that
actually needed. The patients did not complete
their treatment course, or the patients referred
to more than one physician for their symptoms.
Therefore, the drugs are stored in their homes.
But in some European countries with convenient
access to antibiotics, self-medication is less
frequent than in Iran. Socio-cultural determinants
are the etiologic factors for self-medication.3
In this study, approximately half of the
participants prescribed antibiotics for themselves
according to their diagnosis. These data showed
that the patients did not have enough knowledge
about the adverse effects of antibiotics and the
indication for antibiotic therapies. Governments
take measures to hold training programs to change
the patients knowledge, attitude, belief and
practice. Access to the physician was the other
important factor associated with self-medication.
Some studies showed the relationship between
the distance from health care center and selfmedication.6, 7
Upper respiratory tract symptoms including
common cold, sore throat, and rhinorrhea were
the most frequent reasons for self-medication in
this study and amoxicillin and ampicillin were the
most frequently prescribed drugs. Other studies
demonstrated similar results and respiratory
symptoms were the most frequent reasons for
antibiotic administration.13 Researchers should take
action to improve the patients knowledge about
viral respiratory symptoms and signs, the proper
use of antibiotics, and the antibiotic side-effects.
There was a significant association between
age, gender and education with self-medication.
These findings are similar to those of other
studies conducted in European countries and
Jordan, indicating that the high level of education
and younger ages were associated with selfmedication.8, 13 Probably, the educated patients
had a higher level of self-esteem and elder people
were more cautious. Other studies demonstrated
4
consistent and inconsistent information.15-18
The results of the regression analysis in this
study did not show any significant relationship
between these factors and self-medication.
There is a need to conduct further studies with
more independent variables to assess selfmedication determinants. Policy makers should
hold community-wide educational programs to
make people aware about the adverse effects
of self-medication. This study was self-reported;
so many factors including social desirability bias
or recall bias might have confounded the results.
Further observational studies are suggested to
solve this problem.
Conclusion
This study dealt with non-recommended use of
antibiotics through self-medication in Shiraz. This
situation may reflect the trends in Iran. The results
of this study highlight the importance of communitywide and professional education programs to
improve the misuse of antibiotics. Policymakers
should make more stringent laws and have more
control over the supply of drugs in pharmacies.
Acknowledgments
This article is the result of a research project that
was funded by The Vice-Chancellor for Research
at Shiraz University of Medical Sciences and
performed by Mohsen Hosseingholizadeh
Mahani in partial fulfillment of the requirements
for certification as a general physician at Shiraz
University of Medical Sciences in Shiraz, Iran. We
thank all primary care center attendants for their
kind cooperation.
Conflict of Interest: None declared
References
1 Donkor ES, Tetteh-Quarcoo PB, Nartey
P, Agyeman IO. Self-Medication Practices
with Antibiotics among Tertiary Level
Students in Accra, Ghana: A CrossSectional Study. International Journal of
Environmental Research and Public Health.
2012;9(10):3519-29.
2 Muras M, Krajewski J, Nocun M, GodyckiCwirko M. A survey of patient behaviours and
beliefs regarding antibiotic self-medication for
respiratory tract infections in Poland. Arch
Med Sci. 2012;1-4.
3 Grigoryan L, Haaijer-Ruskamp FM, Burgerhof
JGM, Mechtler R, Deschepper R, TambicAndrasevic A, et al. Self-medication with
antimicrobial drugs in Europe. Emerging
J Health Sci Surveillance Sys July 2013; Vol 1; No 1
Antibiotics self-medication in Shiraz
infectious diseases. 2006;12(3):452.
4 Poole K. Overcoming antimicrobial resistance
by targeting resistance mechanisms.
Journal of pharmacy and pharmacology.
2001;53(3):283-94.
5 Okeke IN, Lamikanra A, Edelman R.
Socioeconomic and behavioral factors leading
to acquired bacterial resistance to antibiotics
in developing countries. Emerging infectious
diseases. 1999;5(1):18.
6 Shankar P, Partha P, Shenoy N. Selfmedication and non-doctor prescription
practices in Pokhara valley, Western Nepal:
a questionnaire-based study. BMC Family
Practice. 2002;3(1):17.
7 Edwards DJ, Richman PB, Bradley K, Eskin
B, Mandell M. Parental use and misuse of
antibiotics: are there differences in urban vs.
suburban settings? Academic emergency
medicine: official journal of the Society for
Academic Emergency Medicine. 2002;9(1):22.
8 Al-Azzam SI, Al-Husein BA, Alzoubi F,
Masadeh MM, Al-Horani MAS. Self-medication
with antibiotics in Jordanian population.
International journal of occupational medicine
and environmental health. 2007;20(4):373-80.
9 Sahebi L, Seydi A, AMINI S, Mousa Khani
M. Self-Medication Status among referring
patients to Tabriz pharmacies. Pharmaceutical
Sciences. 2009; 14(4): 174-81.
10 Sarahroodi S, Arzi A, Sawalha A,
Ashtarinezhad A. Antibiotics self-medication
among southern iranian university students.
International Journal of Pharmacology.
2010;6(1):48-52.
11 Sarahroodi S, Arzi A. Self medication with
J Health Sci Surveillance Sys July 2013; Vol 1; No 1
12
13
14
15
16
17
18
antibiotics, is it a problem among Iranian
college students in Tehran. J Biol Sci.
2009;9(8):829-32.
Sahebi L, Vahidi RG. Self-medication and
storage of drugs at home among the clients
of drugstores in Tabriz. Current Drug Safety.
2009;4(2):107-12.
Scicluna EA, Borg MA, Gr D, Rasslan O,
Taher I, Redjeb SB, et al. Self-medication
with antibiotics in the ambulatory care setting
within the Euro-Mediterranean region; results
from the ARMed project. Journal of infection
and public health. 2009;2(4):189-97.
Zargarzadeh AH, Minaeiyan M, Torabi A.
Prescription and nonprescription drug use
in isfahan, Iran: An observational, crosssectional study. Current Therapeutic
Research. 2008;69(1):76-87.
Pan H, Cui B, Zhang D, Farrar J, Law F,
Ba-Thein W. Prior Knowledge, Older Age,
and Higher Allowance Are Risk Factors
for Self-Medication with Antibiotics among
University Students in Southern China. PloS
one. 2012;7(7):e41314.
Shamsi M, Tajik R, Mohammadbegee A.
Effect of education based on Health Belief
Model on self-medication in mothers referring
to health centers of Arak. Arak Medical
University Journal. 2009;12(3):57-66.
Puczynski MS, Gonzalez J, OKeefe JP. Selftreatment with antibiotics. Ann Emerg Med.
1987;16(12):1359-61.
Bi P, Tong S, Parton KA. Family selfmedication and antibiotics abuse for children
and juveniles in a Chinese city. Social science
& medicine. 2000;50(10):1445-50.
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- 19 Claves STR Nº19 Final Usamedic 2017 Print PDFDocumento1 página19 Claves STR Nº19 Final Usamedic 2017 Print PDFVmiguel LcastilloAinda não há avaliações
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- 21 Claves STR #21 Final Usamedic 2017 PDFDocumento1 página21 Claves STR #21 Final Usamedic 2017 PDFVmiguel LcastilloAinda não há avaliações
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Diabetology & Metabolic Syndrome: Post-Transplant Diabetes MellitusDocumento4 páginasDiabetology & Metabolic Syndrome: Post-Transplant Diabetes MellitusVmiguel LcastilloAinda não há avaliações
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (894)
- 1 s2.0 S2212267213005182 MainDocumento9 páginas1 s2.0 S2212267213005182 MainVmiguel LcastilloAinda não há avaliações
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Predictores de CorioDocumento12 páginasPredictores de CorioVmiguel LcastilloAinda não há avaliações
- Nri 3341Documento14 páginasNri 3341Vmiguel LcastilloAinda não há avaliações
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Ranking General 2do Sim NacionalDocumento13 páginasRanking General 2do Sim NacionalVmiguel LcastilloAinda não há avaliações
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Asma - NelsonDocumento22 páginasAsma - NelsonVmiguel LcastilloAinda não há avaliações
- Respuesta in MuneDocumento23 páginasRespuesta in MuneVmiguel LcastilloAinda não há avaliações
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- Itu en DiabetesDocumento6 páginasItu en DiabetesVmiguel LcastilloAinda não há avaliações
- International Journal of Surgery Case ReportsDocumento4 páginasInternational Journal of Surgery Case ReportsVmiguel LcastilloAinda não há avaliações
- Antitumor Effects of Octreotide LAR, A Somatostatin AnalogDocumento2 páginasAntitumor Effects of Octreotide LAR, A Somatostatin AnalogVmiguel LcastilloAinda não há avaliações
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Journal of Pediatric Surgery: Wendy K. Fujioka, Robert A. CowlesDocumento3 páginasJournal of Pediatric Surgery: Wendy K. Fujioka, Robert A. CowlesVmiguel LcastilloAinda não há avaliações
- Team 13BDocumento13 páginasTeam 13BVmiguel LcastilloAinda não há avaliações
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Suicidality and Depression Disparities Between Sexual Minority and Heterosexual YouthDocumento9 páginasSuicidality and Depression Disparities Between Sexual Minority and Heterosexual YouthVmiguel LcastilloAinda não há avaliações
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- PNTD 0001819Documento12 páginasPNTD 0001819Vmiguel LcastilloAinda não há avaliações
- Upper GI BleedingDocumento24 páginasUpper GI BleedingRosalía Arroyo FloresAinda não há avaliações
- Self-Medication in Older Urban Mexicans: An Observational, Descriptive, Cross-Sectional StudyDocumento2 páginasSelf-Medication in Older Urban Mexicans: An Observational, Descriptive, Cross-Sectional StudyVmiguel LcastilloAinda não há avaliações
- Automedicación en Brasil)Documento7 páginasAutomedicación en Brasil)Vmiguel LcastilloAinda não há avaliações
- P 44Documento10 páginasP 44hannediantaAinda não há avaliações
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Antibioticos para Vias Respiratorias AltasDocumento12 páginasAntibioticos para Vias Respiratorias AltasVmiguel LcastilloAinda não há avaliações
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- Embriologia Del Sistema Urogenital y Anomalias CongenitasDocumento42 páginasEmbriologia Del Sistema Urogenital y Anomalias CongenitasVmiguel LcastilloAinda não há avaliações
- Ti41 04Documento0 páginaTi41 04Vmiguel LcastilloAinda não há avaliações
- Quiste Pancreatico - Revisión - Colegio Americano de CirugiaDocumento9 páginasQuiste Pancreatico - Revisión - Colegio Americano de CirugiaVmiguel LcastilloAinda não há avaliações
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Vacunación Contra Malaria - RevisiónDocumento3 páginasVacunación Contra Malaria - RevisiónVmiguel LcastilloAinda não há avaliações
- Prevención de Eventos Tromboembólicos en Cirugía GinecológicaDocumento13 páginasPrevención de Eventos Tromboembólicos en Cirugía GinecológicaVmiguel LcastilloAinda não há avaliações
- Prediction Clinical Profile To Distinguish Between Systolic and Diastolic Heart Failure in Hospitalized PatientsDocumento6 páginasPrediction Clinical Profile To Distinguish Between Systolic and Diastolic Heart Failure in Hospitalized PatientsVmiguel LcastilloAinda não há avaliações
- JNC 8 PDFDocumento14 páginasJNC 8 PDFAlan NophalAinda não há avaliações
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Isicem 2021Documento90 páginasIsicem 2021labbeneAinda não há avaliações
- DAFTAR PUSTAKA Serologi Dan ImunologiDocumento2 páginasDAFTAR PUSTAKA Serologi Dan ImunologiSari Anggun NAinda não há avaliações
- Information and Resources For Effective Self-Management of Problem Substance UseDocumento52 páginasInformation and Resources For Effective Self-Management of Problem Substance Useedmidler100% (1)
- Erectile DysfunctionDocumento31 páginasErectile Dysfunctionrahuldtc100% (1)
- Laminectomy Definition: Spine Surgery to Relieve Pressure on Spinal Cord or NervesDocumento9 páginasLaminectomy Definition: Spine Surgery to Relieve Pressure on Spinal Cord or NervesEdmarie AmistadAinda não há avaliações
- ICICI Lombard General Insurance Company LimitedDocumento22 páginasICICI Lombard General Insurance Company LimitedAmit BansalAinda não há avaliações
- Fellowship Course 3 Program v1Documento15 páginasFellowship Course 3 Program v1Joice RumondangAinda não há avaliações
- FNCPDocumento3 páginasFNCPLander VirayAinda não há avaliações
- Dental Caries IndexDocumento35 páginasDental Caries Indexdr parveen bathla100% (1)
- CostipitationDocumento4 páginasCostipitationashmi akberAinda não há avaliações
- Coverage Midterm Examination 2021 Drug and Vice ControlDocumento4 páginasCoverage Midterm Examination 2021 Drug and Vice ControlTaga Phase 7Ainda não há avaliações
- Front Matter 2021Documento18 páginasFront Matter 2021Евгений ПанковецAinda não há avaliações
- Name of DrugDocumento6 páginasName of DrugKathleen ColinioAinda não há avaliações
- Gen EpidemiologyDocumento88 páginasGen EpidemiologyShibu Sebastian100% (1)
- Microbiology of Clostridium Tetani and Wound ClassificationDocumento3 páginasMicrobiology of Clostridium Tetani and Wound ClassificationAZIZAH ARDINALAinda não há avaliações
- Semana 3 Enf (2) InglesDocumento22 páginasSemana 3 Enf (2) InglesROMERO BARBOZA KIARA ESTHEFANYAinda não há avaliações
- 113 - JCI Mock Survey QuestionDocumento4 páginas113 - JCI Mock Survey QuestionMohamad Attia100% (1)
- Schedule FinalDocumento2 páginasSchedule Finalapi-360816970Ainda não há avaliações
- AIIMS Dental PG November 2009 Solved Question Paper PDFDocumento16 páginasAIIMS Dental PG November 2009 Solved Question Paper PDFDr-Amit PandeyaAinda não há avaliações
- Create PDFDocumento10 páginasCreate PDFAthanasia SergouniotiAinda não há avaliações
- Kumar Fong's Prescription WorksheetDocumento2 páginasKumar Fong's Prescription WorksheetKumar fongAinda não há avaliações
- Anorexia Nerviosa y Trastornos Del Espectro Autista Investigacion Guiada de Endofenotipos Cognitivos SocialesDocumento31 páginasAnorexia Nerviosa y Trastornos Del Espectro Autista Investigacion Guiada de Endofenotipos Cognitivos SocialesCarito Hernandez RodriguezAinda não há avaliações
- Dimension EXL 200/EXL With LM Integrated Chemistry Systems: Global Test MenuDocumento2 páginasDimension EXL 200/EXL With LM Integrated Chemistry Systems: Global Test MenuGuneyden GuneydenAinda não há avaliações
- Dapa-CKD - Applying Clinical Evidence To Clinical PracticeDocumento45 páginasDapa-CKD - Applying Clinical Evidence To Clinical Practicedevikumar kelkarAinda não há avaliações
- Association Between Mir Let-7g Gene Expression and The Risk of Cervical Cancer in Human Papilloma Virus-Infected PatientsDocumento8 páginasAssociation Between Mir Let-7g Gene Expression and The Risk of Cervical Cancer in Human Papilloma Virus-Infected PatientsGICELAAinda não há avaliações
- Halozyme Therapeutics, Inc. 2009 Investor Day PresentationDocumento88 páginasHalozyme Therapeutics, Inc. 2009 Investor Day Presentationsstrumello7395Ainda não há avaliações
- MCQ Bleeding Disorders 2nd Year2021Documento6 páginasMCQ Bleeding Disorders 2nd Year2021sherif mamdoohAinda não há avaliações
- Biosensors 12 00985 v2Documento30 páginasBiosensors 12 00985 v2aqsa javedAinda não há avaliações
- Ejsr 72 3 04Documento9 páginasEjsr 72 3 04Khalifa BakkarAinda não há avaliações
- Ayurved TerminologiesDocumento30 páginasAyurved TerminologiesVipul RaichuraAinda não há avaliações