Escolar Documentos
Profissional Documentos
Cultura Documentos
Integrated Management of Neonatal & Childhood Illness (Imnci)
Enviado por
J Ta Ra0 notas0% acharam este documento útil (0 voto)
32 visualizações5 páginasThe IMNCI strategy aims to reduce infant and child mortality in India by providing an integrated approach to managing the most common illnesses in children under 5 years old. It focuses on improving case management skills of health staff, strengthening the overall health system, and promoting better family/community health practices. The core of the strategy is integrated case management using evidence-based clinical guidelines. Sick children are assessed and classified by color according to their symptoms and treatment needs. This may indicate urgent referral, specific treatments, or home management. The goal is to ensure children receive the right treatment through improved practices at health facilities, in the community, and at home.
Descrição original:
nursing education
Título original
genetic counselling
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
DOCX, PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoThe IMNCI strategy aims to reduce infant and child mortality in India by providing an integrated approach to managing the most common illnesses in children under 5 years old. It focuses on improving case management skills of health staff, strengthening the overall health system, and promoting better family/community health practices. The core of the strategy is integrated case management using evidence-based clinical guidelines. Sick children are assessed and classified by color according to their symptoms and treatment needs. This may indicate urgent referral, specific treatments, or home management. The goal is to ensure children receive the right treatment through improved practices at health facilities, in the community, and at home.
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato DOCX, PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
32 visualizações5 páginasIntegrated Management of Neonatal & Childhood Illness (Imnci)
Enviado por
J Ta RaThe IMNCI strategy aims to reduce infant and child mortality in India by providing an integrated approach to managing the most common illnesses in children under 5 years old. It focuses on improving case management skills of health staff, strengthening the overall health system, and promoting better family/community health practices. The core of the strategy is integrated case management using evidence-based clinical guidelines. Sick children are assessed and classified by color according to their symptoms and treatment needs. This may indicate urgent referral, specific treatments, or home management. The goal is to ensure children receive the right treatment through improved practices at health facilities, in the community, and at home.
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato DOCX, PDF, TXT ou leia online no Scribd
Você está na página 1de 5
INTEGRATED MANAGEMENT OF NEONATAL &
CHILDHOOD ILLNESS (IMNCI)
Introduction
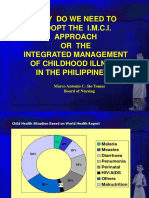
In India, common illness in children under 3 years of age includes fever
(27%), acute respiratory inspections (17%), diarrhea (13%) and
malnutrition (43%) and often in combination. Infant Mortality Rate
continuous to be high at 68/1000 live births and Under Five Mortality
Rate at 95/1000 live births per year. Neonatal mortality contributes to
over 64% of infant deaths and most of these deaths occur during the first
week of life. Mortality rate in the second month of life is also higher
than at later ages. Any health program that aims at reducing Infant
Mortality Rate needs to address mortality in the first two months of
Life, particularly in the first week of life.
An evidence-based syndromic approach can be used to
determine the:
1. Health problem(s) the child may have,
2. Severity of the child's condition, and
3, actions that can be taken to care for the child (e.g.. refer the child
immediately, manage with available resources, or manage at home).
IMNCI Promotes
1 Adjustment of interventions to the capacity of the health system.
2. Active involvement of family members and the community in the
health care process.
Components of the integrated Approach
The IMNCI strategy includes both preventive and curative interventions
that aim to improve practices in health facilities, the health system and at
home. At the core of the strategy is integrated case management of the
most common neonatal and childhood problems with a focus on the
most common causes of death.
The strategy includes three main components:
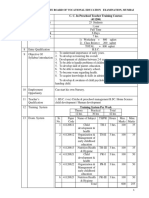
I. Improvements in the case-management skills of health staff through
the provision of locally- adapted guidelines on Integrated Management
of Neonatal and Childhood Illness and activities to promote their use.
2. Improvements in the overall health system required for effective
management of neonatal and childhood illness.
3. Improvements in family and community health care practices.
Principles of Integrated Care
Depending on a child's age, various clinical signs and symptoms differ
in their degree of reliability y and diagnostic value and importance.
The IMNCI guidelines are based on the following principles:
1. All sick young infants up to 2 months of age must be assessed for
possible bacterial infection/jaundice". Then they must be routinely
assessed for the "diarrhea".
2. All sick children age 2 months up to 5 years must be examined for
"general danger signs" which indicate the need for immediate referral or
admission to a hospital. They must then be routinely assessed for major
symptoms: cough or difficult breathing, diarrhea, fever and ear
problems.
3. All sick young infants and children 2 months up to 5 years must also
be routinely assessed for nutritional and immunization status, feeding
problems, and other potential problems.
4. Only a limited number of carefully selected clinical signs are used,
based on evidence of their sensitivity and specificity to detect disease.
5. These signs were selected considering the conditions and realities offacilities. Health facilities.
6. A combination of individual signs leads to an infant's or a child's
classification(s) rather than a diagnosis. Classification(s) indicate the
severity of condition(s). They call for specific actions based on whether
the infant or child:
Should be urgently referred to a higher level of care (Pink colour).
requires specific treatments (such as antibiotics or anti-malarial
treatment) (Yellow colour)
May be safely managed at home (Green colour).
The classifications are colour coded: "pink" suggests hospital
referral or admission,. "Yellow" indicates initiation of specific
treatment, and "green" calls for home management.
7. The IMNCI guidelines address most, but not all, of the major reasons
a sick infant is child is brought to a clinic. An infant or child returning
with chronic problems or less common illness may require special care.
The guidelines do not describe the management trauma or other acute
emergencies due to accidents or injuries. they do not cover care at birth.
IMNCI Case management process
The overall case management process is memorized in figure.
For all sick children age up to 5 years who are brought to a first
level health facility
Access the child: check for danger signs (or possible bacterial
infection/jaundice).ask about main symptoms reported, access
further. Check nutrition and immunization status. Check for other
problems
Classify the childs illness: use a colour coded triage system to
classify the childs main symptoms and his or her nutrition or
feeding status.
If urgent referral is needed and possible /If not urgent referral is
needed and possible.
Identify urgent pre-referral treatment(s) needed for the childs
classification./identify treatment: needs for the childs
classification: identify specific medical treatments and/or advice
Treat the child-give urgent pre-referral treatment(s) needed / treat
the child- give the first dose of oral drugs in the clinic and/or
advice the childs care taker. Teach the care taker how to give oral
drugs and how to treat local infections at home. if needed, given
immunization.
Refer the child: explains to the childs care taker the need for
referral, calm the care takers fears and help resolve any problem.
While referral note. give instructions and supplies needed to take
care for the child on the way to the hospital./counsel the mother :
assess the childs feeding , including breast feeding practices and
solve feeding problems, if present advice about feeding and fluids
during illness and about
when to return to a health
facility.counsel the mother about her own health.
Follow up care: give follow up care when childs return to the
clinic and if necessary reassess the child for new problems.
Outpatient health facility
1. Assessment of health.
2. Classification and identification of treatment.
3. Referral. Treatment or counseling of the childs care taker
(depending on the classification(s) identified).
4. Follow up care.
Referral Health Facility
1. Emergency triage assessment and treatment (ETAT).
2. Diagnosis. Treatment and monitoring of patient progress.
Appropriate Home Management
1. Teaching mothers or other care takers how to give oral drugs and treat
local infections at home.
2. Counselling mothers or other care takers about food (feeding
recommendations, feeding problems), fluids. When to return to the
health facility and the mother's own health.
Você também pode gostar
- IMNCIDocumento31 páginasIMNCIJaya Prabha100% (2)
- IMCIDocumento85 páginasIMCIPiao Liang JingAinda não há avaliações
- Integrated Management of Childhood IllnessDocumento8 páginasIntegrated Management of Childhood IllnessSehar162Ainda não há avaliações
- CHN 211 Week 8 PPT - Integrated Management of Childhood IllnessDocumento82 páginasCHN 211 Week 8 PPT - Integrated Management of Childhood IllnessMark Angelo Berdejo100% (1)
- Seminar On IMNCI (Autosaved)Documento17 páginasSeminar On IMNCI (Autosaved)CM-A-12-Aditya Bhopalbade100% (1)
- Integrated Management On Childhood Imci ReportDocumento29 páginasIntegrated Management On Childhood Imci ReportvernaAinda não há avaliações
- IMCI Integrated Management of Childhood IllnessDocumento24 páginasIMCI Integrated Management of Childhood Illnesssimplyme_tin13100% (1)
- IMCI - Integrated Management of Childhood IllnessDocumento11 páginasIMCI - Integrated Management of Childhood IllnessIvy100% (2)
- WHO - IMCI-Integrated Management of Childhood IllnessDocumento60 páginasWHO - IMCI-Integrated Management of Childhood Illnesseric100% (1)
- IMCI LectureDocumento34 páginasIMCI LectureRomana LatowedAinda não há avaliações
- IMNCIDocumento10 páginasIMNCIUday KumarAinda não há avaliações
- Report of Inservice EducationDocumento35 páginasReport of Inservice EducationAkansha JohnAinda não há avaliações
- IMCImoduleDocumento13 páginasIMCImoduleWynjoy NebresAinda não há avaliações
- Integrated Management of Childhood Illness (IMCI) PDFDocumento7 páginasIntegrated Management of Childhood Illness (IMCI) PDFLOVELY ANN GIGANTEAinda não há avaliações
- Imci 1Documento90 páginasImci 1Miguel VergelAinda não há avaliações
- IMNCI Training Module 1-9Documento356 páginasIMNCI Training Module 1-9smbawasaini50% (4)
- Imci, Diseases With TreatmentDocumento54 páginasImci, Diseases With TreatmentBernadeth Tolentino LimonAinda não há avaliações
- Integrated Management of Childhood Illness (IMCI) A Strategy, An ApproachDocumento23 páginasIntegrated Management of Childhood Illness (IMCI) A Strategy, An ApproachMarjo FegideroAinda não há avaliações
- IMNCI Integrated Management of Newborn and Childhood IllnessDocumento11 páginasIMNCI Integrated Management of Newborn and Childhood IllnessPriyaAinda não há avaliações
- 7091371954mod 1 INTRODUCTION RDocumento16 páginas7091371954mod 1 INTRODUCTION RJEEJAAinda não há avaliações
- IMCIDocumento35 páginasIMCIharutoshippuden0Ainda não há avaliações
- Integrated Management of Childhood IllnessDocumento22 páginasIntegrated Management of Childhood Illnessstelmar_16Ainda não há avaliações
- Integrated Management of Childhood IllnessDocumento148 páginasIntegrated Management of Childhood IllnessMichael CrisologoAinda não há avaliações
- Imnci: (Principles and Strategies)Documento15 páginasImnci: (Principles and Strategies)Dhanunjay Kalvakuri NaiduAinda não há avaliações
- CHN211 Week 8 WORD - Integrated Management of Childhood IllnessDocumento28 páginasCHN211 Week 8 WORD - Integrated Management of Childhood IllnessYrah Elaine SanchezAinda não há avaliações
- Integrated Management of Childhood IllnessDocumento5 páginasIntegrated Management of Childhood Illnessjulieyauder624Ainda não há avaliações
- IMNCI Part - IDocumento72 páginasIMNCI Part - IKedir AhmedAinda não há avaliações
- Integrated Management of Childhood IllnessesDocumento5 páginasIntegrated Management of Childhood IllnessesPamela Joy Rico UnayAinda não há avaliações
- Integrated Management of Childhood IllnessesDocumento27 páginasIntegrated Management of Childhood IllnessesJoeYeshitellaAinda não há avaliações
- MCN Lecture NotesDocumento52 páginasMCN Lecture NotesJHYANE KYLA TRILLESAinda não há avaliações
- IMCI Nov 2009Documento141 páginasIMCI Nov 2009togononkaye100% (1)
- Integrated Management of Childhood IllnessDocumento5 páginasIntegrated Management of Childhood IllnessheartianeAinda não há avaliações
- Pediatric Revieer PrelimsDocumento3 páginasPediatric Revieer PrelimsJada GonzalesAinda não há avaliações
- 3 Year Paediatric Assignment One: Department NursingDocumento12 páginas3 Year Paediatric Assignment One: Department NursingmekdesAinda não há avaliações
- Integrated Management On Childhood IllnessDocumento3 páginasIntegrated Management On Childhood IllnessAbeer AguamAinda não há avaliações
- IMCI Orientation Powerpoint PresentationDocumento45 páginasIMCI Orientation Powerpoint Presentationboynegro100% (18)
- IMCI Lecture For NCM 104semisDocumento171 páginasIMCI Lecture For NCM 104semisKathleen Joy G. TadleAinda não há avaliações
- Final Adaptation Sick Young Infant Module PDFDocumento76 páginasFinal Adaptation Sick Young Infant Module PDFAngelica AmandoAinda não há avaliações
- Integrated Management of Childhood Illness (IMCI) : An OverviewDocumento54 páginasIntegrated Management of Childhood Illness (IMCI) : An Overviewmonmon50% (2)
- IMCI#1Documento89 páginasIMCI#1Rosechelle Baggao Siupan-ElarcoAinda não há avaliações
- EPI - AND - IMCI - Docx Filename - UTF-8''EPI AND IMCIDocumento14 páginasEPI - AND - IMCI - Docx Filename - UTF-8''EPI AND IMCIYvonne Carmel Aguilar SunigaAinda não há avaliações
- IMCIDocumento24 páginasIMCISaniAinda não há avaliações
- IMCI - ContentDocumento13 páginasIMCI - ContentMarianne Daphne GuevarraAinda não há avaliações
- Module 1 Introduction Nov 2011Documento16 páginasModule 1 Introduction Nov 2011samuelAinda não há avaliações
- IMCI (Integrated Management of Childhood Illness)Documento4 páginasIMCI (Integrated Management of Childhood Illness)Jane BautistaAinda não há avaliações
- Integrated Management of Childhood Illness (IMCI) : BackgroundDocumento10 páginasIntegrated Management of Childhood Illness (IMCI) : BackgroundMarianne Tajanlangit BebitAinda não há avaliações
- K - 39 Well ChildDocumento27 páginasK - 39 Well ChildVinanda Maria AlexandraAinda não há avaliações
- Integrated Management of Childhood IllnessDocumento83 páginasIntegrated Management of Childhood Illnessjava_biscocho1229Ainda não há avaliações
- Pediatrics: Demlie Z. (BSC, MSC)Documento62 páginasPediatrics: Demlie Z. (BSC, MSC)Abel EthioAinda não há avaliações
- Guidelines On Severe Acute Malnutrition MangementDocumento4 páginasGuidelines On Severe Acute Malnutrition MangementVandanaAinda não há avaliações
- IMCIDocumento15 páginasIMCISandy JusiAinda não há avaliações
- Communicable Diseases Summary A Guide For School Health Services Personnel Child Care Providers and Youth CampsDocumento36 páginasCommunicable Diseases Summary A Guide For School Health Services Personnel Child Care Providers and Youth CampsBalqees MohammedAinda não há avaliações
- IMCI Basic Pedia 2015 PPTDocumento77 páginasIMCI Basic Pedia 2015 PPTCharles DoradoAinda não há avaliações
- Under Fives ClinicDocumento4 páginasUnder Fives ClinicJyoti SidhuAinda não há avaliações
- Integrated Management of Childhood Illness (Imci)Documento19 páginasIntegrated Management of Childhood Illness (Imci)M•A•R•V•E•LAinda não há avaliações
- The Integrated Management of Childhood IllnessesDocumento32 páginasThe Integrated Management of Childhood IllnessesKrishna PhulpagarAinda não há avaliações
- Field TripsDocumento4 páginasField TripsJ Ta Ra100% (1)
- Curriculum EvaluationDocumento5 páginasCurriculum EvaluationJ Ta RaAinda não há avaliações
- Welcome: N.K.LathaDocumento17 páginasWelcome: N.K.LathaJ Ta RaAinda não há avaliações
- Collaboration Issues Within and Outside NursingDocumento9 páginasCollaboration Issues Within and Outside NursingJ Ta RaAinda não há avaliações
- Definition of Seminar TechniquesDocumento1 páginaDefinition of Seminar TechniquesJ Ta RaAinda não há avaliações
- Essay Type QuestionsDocumento3 páginasEssay Type QuestionsJ Ta Ra100% (1)
- Roles in Seminar TechniqueDocumento3 páginasRoles in Seminar TechniqueJ Ta Ra100% (1)
- Workshop TechniqueDocumento1 páginaWorkshop TechniqueJ Ta RaAinda não há avaliações
- Paplau, AbdellahDocumento41 páginasPaplau, AbdellahJ Ta RaAinda não há avaliações
- Acute Inflammation, Cell Derived and Plasma Protein Derived Mediators, MorphologyDocumento66 páginasAcute Inflammation, Cell Derived and Plasma Protein Derived Mediators, MorphologyJ Ta RaAinda não há avaliações
- Cold SpongingDocumento13 páginasCold SpongingJ Ta Ra83% (6)
- PHILODocumento33 páginasPHILOJ Ta RaAinda não há avaliações
- Allen, J - Coping With Catch-22s of Depression, (2002)Documento42 páginasAllen, J - Coping With Catch-22s of Depression, (2002)Ola AlansaryAinda não há avaliações
- Week 13-14 Part 1Documento3 páginasWeek 13-14 Part 1Loren Joy S. SulayaoAinda não há avaliações
- Guidelines For Acute Care of The Neonate 22eDocumento181 páginasGuidelines For Acute Care of The Neonate 22eKatherin J.Ainda não há avaliações
- Development of A Complementary Feeding Manual For BangladeshDocumento83 páginasDevelopment of A Complementary Feeding Manual For Bangladeshنوبوني يززونAinda não há avaliações
- 107 RLE Group 5 1F Newborn Delivery Final OutputDocumento79 páginas107 RLE Group 5 1F Newborn Delivery Final OutputJr CaniaAinda não há avaliações
- Mammals: Feeding Their Babies Since The Beginning of Time!Documento41 páginasMammals: Feeding Their Babies Since The Beginning of Time!Wiji AstutiAinda não há avaliações
- NLE Practice Exam With AnswersDocumento43 páginasNLE Practice Exam With AnswersSuzette Rae TateAinda não há avaliações
- Susanna Isaacs ElmhirstDocumento14 páginasSusanna Isaacs Elmhirstkarine botelhoAinda não há avaliações
- Clinical Guideline: Enteral Feeding - Iron Supplementation: Neonatal Clinical Oversight GroupDocumento12 páginasClinical Guideline: Enteral Feeding - Iron Supplementation: Neonatal Clinical Oversight GroupStphn WllngtnAinda não há avaliações
- Nipissing Developmental Screen 2 MonthDocumento2 páginasNipissing Developmental Screen 2 Monthg_kravaritisAinda não há avaliações
- Calculation of KcalDocumento13 páginasCalculation of KcalMichael WilliamsAinda não há avaliações
- Asuhan PrenatalDocumento25 páginasAsuhan PrenatalRifqiyah Al-ManshurAinda não há avaliações
- Breast Care ProcedureDocumento3 páginasBreast Care ProcedureDaniel AdlawonAinda não há avaliações
- Characteristics OFA NewbornDocumento14 páginasCharacteristics OFA NewbornhemihemaAinda não há avaliações
- Infant Care and Feeding Post TestDocumento4 páginasInfant Care and Feeding Post TestFely B. Balgoa93% (30)
- Cup FeedingDocumento2 páginasCup FeedingEaster Soma HageAinda não há avaliações
- Nursing Care Plan For Ineffective Breastfeeding NCPDocumento4 páginasNursing Care Plan For Ineffective Breastfeeding NCPderic76% (46)
- Module 9 Eng Health PDFDocumento80 páginasModule 9 Eng Health PDFVivica MorenoAinda não há avaliações
- Imitation and Other Minds MeltzoffDocumento29 páginasImitation and Other Minds MeltzoffDiego Abraham Morales TapiaAinda não há avaliações
- 6241Documento17 páginas6241miltodiavoloAinda não há avaliações
- D4 InfanciaDocumento3 páginasD4 InfanciaPedroPocasAinda não há avaliações
- Developmental AssessmentDocumento3 páginasDevelopmental Assessmentsarguss14Ainda não há avaliações
- Natural Pregnancy and ParentingDocumento70 páginasNatural Pregnancy and ParentingAmela SabicAinda não há avaliações
- Pre School Teacher Training Course. 1Documento19 páginasPre School Teacher Training Course. 1MithileshAinda não há avaliações
- Browne 2011Documento11 páginasBrowne 2011Gisele Elise MeninAinda não há avaliações
- KMC ProjectDocumento2 páginasKMC ProjectNadiya RashidAinda não há avaliações
- Reference Range Values For Pediatric Care-2nd PDFDocumento202 páginasReference Range Values For Pediatric Care-2nd PDFIvan Veriswan67% (3)
- Rubin's TheoryDocumento3 páginasRubin's TheoryBeerna Grande50% (2)
- Prado Random FactsDocumento377 páginasPrado Random Factsjkrix100% (2)
- Epidemiology Assignment 2Documento10 páginasEpidemiology Assignment 2Melissa Monique Peart-YatesAinda não há avaliações
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNo EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNota: 4 de 5 estrelas4/5 (404)
- The Age of Magical Overthinking: Notes on Modern IrrationalityNo EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityNota: 4 de 5 estrelas4/5 (34)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNo EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNota: 5 de 5 estrelas5/5 (4)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)No EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Nota: 3 de 5 estrelas3/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNo EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNota: 4 de 5 estrelas4/5 (4)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNo EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNota: 4.5 de 5 estrelas4.5/5 (82)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeNo EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeNota: 4.5 de 5 estrelas4.5/5 (254)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsNo EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsNota: 4.5 de 5 estrelas4.5/5 (170)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsAinda não há avaliações
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNota: 2 de 5 estrelas2/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNo EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNota: 4.5 de 5 estrelas4.5/5 (44)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNo EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNota: 5 de 5 estrelas5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNo EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNota: 4.5 de 5 estrelas4.5/5 (266)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesNo EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesNota: 4.5 de 5 estrelas4.5/5 (1412)
- The Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeNo EverandThe Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeNota: 4.5 de 5 estrelas4.5/5 (2)
- The Obesity Code: Unlocking the Secrets of Weight LossNo EverandThe Obesity Code: Unlocking the Secrets of Weight LossNota: 4 de 5 estrelas4/5 (6)
- To Explain the World: The Discovery of Modern ScienceNo EverandTo Explain the World: The Discovery of Modern ScienceNota: 3.5 de 5 estrelas3.5/5 (51)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.No EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Nota: 4.5 de 5 estrelas4.5/5 (110)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisNo EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisNota: 3.5 de 5 estrelas3.5/5 (2)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsAinda não há avaliações
- Hearts of Darkness: Serial Killers, The Behavioral Science Unit, and My Life as a Woman in the FBINo EverandHearts of Darkness: Serial Killers, The Behavioral Science Unit, and My Life as a Woman in the FBINota: 4 de 5 estrelas4/5 (20)
- Why We Die: The New Science of Aging and the Quest for ImmortalityNo EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityNota: 4.5 de 5 estrelas4.5/5 (6)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryNo EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryNota: 4 de 5 estrelas4/5 (46)