Escolar Documentos
Profissional Documentos
Cultura Documentos
Permissive Hypercapnia in Extremely Low Birthweight Infants (PHELBI) : A Randomised Controlled Multicentre Trial Lancet
Enviado por
Jane LlasiTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Permissive Hypercapnia in Extremely Low Birthweight Infants (PHELBI) : A Randomised Controlled Multicentre Trial Lancet
Enviado por
Jane LlasiDireitos autorais:
Formatos disponíveis
Articles
Permissive hypercapnia in extremely low birthweight
infants (PHELBI): a randomised controlled multicentre trial
Ulrich H Thome, Orsolya Genzel-Boroviczeny, Bettina Bohnhorst, Manuel Schmid, Hans Fuchs, Oliver Rohde, Stefan Avenarius,
Hans-Georg Topf, Andrea Zimmermann, Dirk Faas, Katharina Timme, Barbara Kleinlein, Horst Buxmann, Wilfried Schenk, Prof Hugo Segerer,
Norbert Teig, Corinna Gebauer, Roland Hentschel, Matthias Heckmann, Rolf Schlsser, Jochen Peters, Rainer Rossi, Wolfgang Rascher,
Ralf Bttger, Jrgen Seidenberg, Gesine Hansen, Maria Zernickel, Gerhard Alzen, Jens Dreyhaupt, Rainer Muche, Helmut D Hummler, for the
PHELBI Study Group*
Summary
Lancet Respir Med 2015;
3: 53443
Published Online
June 16, 2015
http://dx.doi.org/10.1016/
S2213-2600(15)00204-0
See Comment page 499
*Members listed in the appendix
Division of Neonatology,
University Hospital for Children
and Adolescents, University of
Leipzig, Leipzig, Germany
(Prof U H Thome MD,
C Gebauer MD); Division of
Neonatology, Dr. von Hauner
University Childrens Hospital,
Ludwig Maximilian University
of Munich, Munich, Germany
(Prof O Genzel-Boroviczeny MD);
Division of Pediatric
Pneumology, Allergology and
Neonatology, Hannover
Medical School, Hannover,
Germany (Prof B Bohnhorst MD,
Prof G Hansen MD); Division of
Neonatology and Pediatric
Critical Care, University
Hospital for Children and
Adolescents, University of Ulm,
Ulm, Germany (M Schmid MD,
M Zernickel MSc,
Prof H D Hummler MD); Division
of Neonatology and Pediatric
Critical Care, University
Hospital for Children and
Adolescents, Albert Ludwigs
University Freiburg, Freiburg,
Germany (H Fuchs MD,
Prof R Hentschel MD); Division
of Neonatology and Pediatric
Critical Care, Elisabeth
Childrens Hospital, Klinikum
Oldenburg, Medical Campus,
Carl von Ossietzky University
of Oldenburg, Oldenburg,
Germany (O Rohde MD,
J Seidenberg MD); Hospital for
General Pediatrics and
Neonatology, Otto von
Guericke University
Magdeburg, Magdeburg,
Germany (S Avenarius MD,
R Bttger MD); Division of
Neonatology, University
Hospital for Children and
534
Background Tolerating higher partial pressure of carbon dioxide (pCO) in mechanically ventilated, extremely low
birthweight infants might reduce ventilator-induced lung injury and bronchopulmonary dysplasia. We aimed to test
the hypothesis that higher target ranges for pCO decrease the rate of bronchopulmonary dysplasia or death.
Methods In this randomised multicentre trial, we recruited infants from 16 tertiary care perinatal centres in Germany
with birthweight between 400 g and 1000 g and gestational age 2328 weeks plus 6 days, who needed endotracheal
intubation and mechanical ventilation within 24 h of birth. Infants were randomly assigned to either a high target or
control group. The high target group aimed at pCO values of 5565 mm Hg on postnatal days 13, 6070 mm Hg on
days 46, and 6575 mm Hg on days 714, and the control target at pCO 4050 mmHg on days 13, 4555 mm Hg
on days 46, and 5060 mm Hg on days 714. The primary outcome was death or moderate to severe bronchopulmonary
dysplasia, dened as need for mechanical pressure support or supplemental oxygen at 36 weeks postmenstrual age.
Cranial ultrasonograms were assessed centrally by a masked paediatric radiologist. This trial is registered with the
ISRCTN registry, number ISRCTN56143743.
Results Between March 1, 2008, and July 31, 2012, we recruited 362 patients of whom three dropped out, leaving
179 patients in the high target and 180 in the control group. The trial was stopped after an interim analysis (n=359).
The rate of bronchopulmonary dysplasia or death in the high target group (65/179 [36%]) did not dier signicantly
from the control group (54/180 [30%]; p=018). Mortality was 25 (14%) in the high target group and 19 (11%; p=032)
in the control group, grade 34 intraventricular haemorrhage was 26 (15%) and 21 (12%; p=030), and the rate of
severe retinopathy recorded was 20 (11%) and 26 (14%; p=036).
Interpretation Targeting a higher pCO did not decrease the rate of bronchopulmonary dysplasia or death in ventilated
preterm infants. The rates of mortality, intraventricular haemorrhage, and retinopathy did not dier between groups.
These results suggest that higher pCO targets than in the slightly hypercapnic control group do not confer increased
benets such as lung protection.
Funding Deutsche Forschungsgemeinschaft.
Introduction
Extremely preterm infants who survive often develop
bronchopulmonary dysplasia, which is characterised by
severely impaired alveolarisation, which in turn results
in a markedly reduced area for gas exchange.1 Infants
with bronchopulmonary dysplasia often need long-term
oxygen supplementation and frequent hospital readmissions,2 with consequent high morbidity and healthcare costs. Ventilator-induced lung injury is deemed one
of the main pathogenic factors for the development of
bronchopulmonary dysplasia and is mainly related to the
magnitude of tidal volume.3,4 Reduction of tidal volumes
might result in alveolar hypoventilation with increased
blood partial pressure of carbon dioxide (pCO), which
might be benecial.5 The intentional reduction of the
intensity of mechanical ventilation and allowing pCO
values above 45 mmHg is referred to as permissive
hypercapnia.
Increased respiratory drive through higher pCO has
been used for decades to wean infants o mechanical
ventilation. Early use of permissive hypercapnia in
newborn preterm infants from the rst day of life has
been controversial, because it might increase cerebral
perfusion, which can enhance oxygen delivery to the
brain, but also increases the risk of intracranial
haemorrhage.6 Furthermore, young rats have developed
retinopathy when exposed to very high pCO values
(roughly 100 mm Hg).7 Instead, because the susceptibility
to ventilator-induced lung injury might be highest soon
after birth,4 the reduction of tidal volumes with resultant
permissive hypercapnia could be most benecial when
applied early.
Data from some retrospective analyses suggest an
association between higher arterial pCO (PaCO) values
during the rst days of life in preterm infants and a
reduced incidence of bronchopulmonary dysplasia,8,9
www.thelancet.com/respiratory Vol 3 July 2015
Articles
Research in context
Evidence before this study
Data from animal experiments suggested that permissive
hypercapnia could be benecial for subjects requiring
mechanical ventilation because of lower tidal volumes and
additional biochemical eects. We hypothesised that such
benets might also apply to preterm infants. We searched
PubMed from 1960 until 2014 for English language articles
with the following search terms: preterm infant, permissive
hypercapnia, and minimal ventilation. We also searched the
reference lists of previous review articles. Several retrospective
analyses were inconclusive. Three randomised trials were
identied in which ventilator-dependent extremely low
birthweight infants were allocated to dierent partial pressure
of carbon dioxide (pCO) targets. Two were small and
monocentric and the third, the SAVE trial, was prematurely
terminated for reasons unrelated to the mechanical ventilation.
All three used dierent PCO targets and the pCO dierences
between the randomly allocated groups were small. None of the
trials showed reduced incidence of bronchopulmonary dysplasia
associated with permissive hypercapnia. One of the
monocentric trials reported faster weaning o mechanical
ventilation, the other, however, a worse neurodevelopmental
outcome. Investigators of the SAVE trial reported a smaller
number of infants requiring long-term mechanical ventilation
beyond a postmenstrual age of 36 weeks. Results of a metaanalysis encompassing all three trials with 334 infants were
calculated which showed trends but no signicant dierences
whereas others do not.10,11 Furthermore, ndings of a
randomised trial12 comparing two dierent tidal volume
settings in adults with acute respiratory distress syndrome
showed increased survival and decreased morbidity in
patients randomly assigned to the lower tidal volume,
who also had higher PaCO.
Several trials have assessed how strategies to avoid
mechanical ventilation can improve outcomes for
preterm infants.13 For this approach to be successful,
investigators need to accept higher than normal pCO
values, but it is not clear whether lung protection is
due more to the use of non-invasive support than to
increased pCO. In preterm infants already on mechanical ventilation, results of four previous randomised
trials1417 of permissive hypercapnia and a meta-analysis18
did not show reduced incidences of bronchopulmonary
dysplasia. However, two of these trials had small sample
sizes,14,15 and in the third with 220 infants, the PaCO
dierence between the groups was only 4 mm Hg.16 In
the fourth trial, management diered between
treatment groups in several aspects other than pCO
target ranges.17 However, no signicant increases in
adverse events, especially the rate of intracranial
haemorrhage, associated with permissive hypercapnia
were reported, and some secondary analyses of the
www.thelancet.com/respiratory Vol 3 July 2015
between the results of dierent pCO targets. In another very
large randomised trial, management diered between
treatment groups in several aspects other than pCO target
ranges.
Retrospective analyses also suggested an increased risk of
intracranial haemorrhage that was not substantiated by the
randomised trials. Animal experiments suggested an increased
risk of retinopathy of prematurity associated with severe
hypercapnia. Whether this risk also applied to human beings
was unknown.
Added value of this study
With a sample size of 359, this multicentre trial did not show
increased lung protection and improved outcomes associated
with higher pCO targets, despite lower ventilator pressures. On
the contrary, higher pCO targets were associated with an
increased incidence of bronchopulmonary dysplasia or death in
the subgroup of infants with the worst lung disease.
Furthermore, there was an unexpected increased incidence of
necrotising enterocolitis, but no increase in the incidence of
intracranial haemorrhage or retinopathy of prematurity.
Implications of all available evidence
Mildly hypercapnic pCO targets as used in the control group of
this trial and the hypercapnia group of the SAVE trial seem to be
safe and are likely to be associated with small health benets.
Higher pCO targets as used in the high target group of this trial
do not increase these benets, and might cause harm.
prematurely terminated SAVE trial17 suggest some
benecial eects.
In their eorts to improve outcome, many neonatologists
have accepted permissive hypercapnia as their standard of
care,19 despite the absence of clearly proven benecial
eects. Consideration has been given to even higher pCO
targets as being of even greater benet. Hence permissive
hypercapnia has spread in todays neonatal intensive care
without sucient supporting evidence,20 with the
optimum PaCO target range for ventilated preterm
infants still to be established. This situation led us to do a
large multicentre trial comparing two markedly dierent
PaCO target ranges in extremely low birthweight infants.
We aimed to study whether a higher pCO target range
would reduce the rate of moderate to severe
bronchopulmonary dysplasia 21 or death in extremely low
birthweight infants needing mechanical ventilation.
Furthermore, we aimed to nd out whether hypercapnia
would be most benecial to the infants requiring the most
ventilatory support.
Methods
Study design and patients
Adolescents, FriedrichAlexander University Erlangen,
Erlangen, Germany
(H-G Topf MD, W Rascher MD);
Mutter-Kind-Zentrum,
Klinikum rechts der Isar,
Technical University of Munich,
Munich, Germany
(A Zimmermann MD);
University Hospital for General
Pediatrics and Neonatology,
Justus Liebig University
Giessen, Giessen, Germany
(D Faas MD); Division of
Neonatology, Hospital for
Children and Adolescents,
Vivantes-Hospital Neuklln,
Berlin, Berlin, Germany
(K Timme MD, Prof R Rossi MD);
Hospital for Children and
Adolescents, Childrens
Hospital of the Third Order,
Munich, Germany
(B Kleinlein MD,
Prof J Peters MD); Division of
Neonatology, University
Hospital for Children and
Adolescents of the J.W. Goethe
University Frankfurt am Main,
Frankfurt am Main, Germany
(H Buxmann MD,
Prof R Schlsser MD); Hospital
for Children and Adolescents,
Central Hospital Augsburg,
Augsburg, Germany
(W Schenk MD); St. Hedwig
Hospital, University of
Regensburg, Regensburg,
Germany (Prof H Segerer MD);
Department of Neonatology
and Pediatric Intensive Care,
Katholisches Klinikum, Ruhr
University Bochum, Bochum,
Germany (N Teig MD); Division
of Neonatology and Pediatric
Critical Care, University
Hospital for Children and
Adolescents, Ernst Moritz
Arndt University Greifswald,
Greifswald, Germany
(Prof M Heckmann MD);
Division of Pediatric Radiology,
University Hospital of the
Justus Liebig University
Giessen, Giessen, Germany
(Prof G Alzen MD); and Institute
of Epidemiology and Medical
Biometry, University of Ulm,
Ulm, Germany
(J Dreyhaupt PhD, R Muche PhD)
Correspondence to:
Prof Ulrich Thome, Division of
Neonatology, Department of
Womens and Childrens
Medicine, University Hospital of
Leipzig, 04103 Leipzig, Germany
uhthome@web.de
See Online for appendix
In this randomised multicentre trial, infants were
recruited from 16 tertiary care perinatal centres in
535
Articles
1534 patients screened
430 not on assisted
ventilation
362 randomly
assigned
3 dropouts
179 high target group
411 no consent
4 chromosomal
anomaly
24 malformation
1 hydrops
14 asphyxia
40 palliative care
52 outborn
196 other
180 control target group
25 died before
36 week PMA
19 died before
36 week PMA
40 on O2 or
mechanical
support at
36 week PMA
35 on O2 or
mechanical
support at
36 week PMA
Figure 1: Trial prole
PMA=postmenstrual age. Infants not receiving invasive assisted ventilation
within 24 h of birth were not eligible for the study. Randomisation had to be
done within 12 h of intubation. The main reason for non-enrolment for some
eligible infants was that parents declined consent. Further reasons for this were
language barriers with some parents, or unavailability of parents able to give
consent within 12 h of birth.
High target
group (n=179)
Gestational age (weeks)
Birthweight (g)
256 14
713 156
Control group
(n=180)
257 13
709 153
Boys
105 (59%)
99 (55%)
Antenatal steroids (any)
162 (91%)
157 (87%)
PPROM >24 h
45 (25%)
35 (20%)
Apgar score at 5 min
7 (19)
8 (19)
Age at intubation (h)
0 (022; 21)
Intubation age 1 h
55 (31%)
0 (021; 13)
57 (32%)
Surfactant replacement
172 (96%)
175 (97%)
Total surfactant (mg/kg)
188 (65774)
183 (55829)
Methylxanthine treatment
168 (94%)
168 (94%)
Data are mean SD, median (minmax); mean, or n (%). PPROM=preterm
premature rupture of the membranes.
Table 1: Demographic data for study infants
Germany (appendix p 11). All infants who weighed 1000 g
or less at birth were screened. Inborn infants with a
gestational age of 2328 weeks plus 6 days, weighing
4001000 g and receiving endotracheal intubation and
mechanical ventilation within 24 h of birth were eligible.
Exclusion criteria were birth outside the prenatal centres
delivery ward, chromosomal anomalies, congenital
malformations requiring early surgery or otherwise
536
compromising respiratory care or outcome, hydrops
fetalis, air leaks before randomisation, severe birth
asphyxia, or a decision to provide compassionate care
only. The trial was approved by each centres institutional
review board and written informed consent was obtained
from the parents or legal guardians of all infants. The
trial was approved by the institutional review boards of
all participating centres. On-site monitoring was done by
the Interdisciplinary Centre for Clinical Trials (IZKS),
University Medical Centre, Mainz, Germany. An
independent data safety monitoring board (DSMB)
consisting of four experienced neonatologists and one
biostatistician evaluated critical safety issues as well as
the protocol amendment to enable the interim analysis
(appendix p 11). A database was programmed and all data
were entered in duplicate.
Patient allocation and masking
Infants were randomly assigned (1:1) with a secure webbased randomisation system (e-randomixer, IZKS), and
randomisation results were applied immediately. Randomisation was done by a block randomisation scheme
with variable block sizes (26) stratied by site and
birthweight (three strata: 400499 g, 500749 g,
7501000 g). It was not feasible to mask caregivers and
parents because of the many clinically indicated blood gas
determinations and ventilator adjustments required in
neonatal intensive care.
Procedures
Endotracheally intubated and mechanically ventilated
infants were randomly allocated to two dierent target
ranges of pCO. In both groups, an age-dependent pCO
increase was permitted to make weaning easier. In the
high target group (experimental intervention) the PaCO
target range was 5565 mm Hg from 13 days of life
(072 h postnatal age), 6070 mm Hg from days 46
(73144 h), and 6575 mm Hg from days 714 (145336 h).
In the control target group the PaCO target range was
4050 mm Hg from days 13 (072 h), 4555 mm Hg
from days 46 (73144h), and 5060 mm Hg from
days 714 (145336 h).
Postnatal age was counted from birth, and infants were
entered into the schedule when they were randomly
assigned. Randomisation and assignment to the
randomised target range had to be completed within 12 h
of endotracheal intubation, and was applied as long as
the infants remained intubated or until the end of day 14.
Extubation could be attempted if the PaCO was
maintained within or below the target range assigned
with a rate of less than 30 breaths per min and FiO was
less than 05. After extubation, no pCO targets were
dened by the study protocol. In the case of re-intubation
before day 14, the target range according to the
randomised group assignment and actual postnatal age
was resumed. Blood pCO was to be measured in at least
12-h intervals, or more frequently if clinically indicated or
www.thelancet.com/respiratory Vol 3 July 2015
Articles
when measurement results outside the target range
occurred. Both arterial and capillary pCO measurements
were accepted, because routine care in several of the
study centres did not include arterial line placement in
all infants, and there was consensus that arterial lines
should not routinely be left in place for 14 days. The study
protocol allowed waiving of all management restrictions
in the case of severe complications.
To minimise volutrauma, a high ventilation rate
(6080 per min) was favoured over high tidal volumes in
both groups. Initial ventilator settings comprised a rate of
6080 per min or greater, inspiratory time of 025035 s,
positive end-expiratory pressure 36 mbar, and a peak
inspiratory pressure resulting in minimal to moderate
chest rise. The rate was allowed to be decreased only if the
peak inspiratory pressure was 14 mbar or lower.
Synchronised ventilation or forms of volume control were
allowed to be used at the discretion of the clinicians in
charge of patient care. Because the administration of
sodium bicarbonate has been linked to increased lung
damage,22,23 its use was discouraged. Furthermore, we
attempted to prevent inconsistent use between the two
study groups to avoid it becoming a confounder. Therefore,
bicarbonate administration to correct a low pH in
combined acidosis was linked to the base decit rather
than the pH or pCO and allowed only if the base decit
exceeded an arbitrary level of 8 mmol/L, independent of
pH and pCO. We used high frequency ventilation only as
a rescue method. The rst dose of natural surfactant was
generally given immediately after intubation as a standard
treatment in all participating centres. However, this was
not governed by the trial protocol since intubation
occurred before enrolment. Further doses were to be
given to all enrolled infants suering from respiratory
distress syndrome and requiring at least a fraction of
inspired oxygen (FiO) of 03. Up to two additional doses
were given within 24 h if the FiO requirement exceeded
03, unless there were contraindications. Caeine was
recommended for all participating infants.
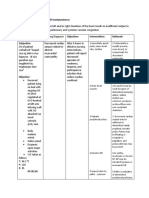
High target group
(n=179)
Control group
(n=180)
p value
65 (36%)
54 (30%)
018
Mortality to 36 weeks postmenstrual age
25 (14%)
19 (11%)
032
Moderate or severe bronchopulmonary dysplasia at
36 weeks postmenstrual age
40 (22%)
35 (19%)
044
029
Moderate or severe bronchopulmonary dysplasia or
death at 36 weeks postmenstrual age*
Death before day 28
22 (12%)
16 (9%)
O or positive pressure for 28 days
147 (82%)
150 (83%)
044
Mild bronchopulmonary dysplasia (consensus
denition)
104 (62%)
112 (63%)
026
Moderate bronchopulmonary dysplasia (consensus
denition)
18 (10%)
23 (13%)
Severe bronchopulmonary dysplasia (consensus
denition)
22 (12%)
12 (7%)
Intraventricular haemorrhage all grades
50 (28%)
55 (31%)
046
9 (5%)
8 (4%)
063
Severe intraventricular haemorrhage (grade 34)
26 (15%)
21 (12%)
030
Severe intraventricular haemorrhage (grade 34)
present on day 1 without progress
7 (4%)
3 (2%)
048
Combined death or moderate to severe
bronchopulmonary dysplasia or intraventricular
haemorrhage (grade 34)
82 (46%)
67 (37%)
009
Intraventricular haemorrhage present on day 1
without progress
Periventricular leukomalacia
16 (9%)
11 (6%)
031
Hydrocephalus internus
24 (16%)
27 (17%)
076
8 (4%)
7 (4%)
078
93 (52%)
79 (44%)
Hydrocephalus internus with shunt
Infants who received bicarbonate treatment
Bicarbonate dose cumulative over the entire hospital
stay, in infants who received bicarbonate (mmol/kg)
Extubated within the rst 14 days of life
Re-intubated within the rst 14 days of life
Days of sedative use per infant
Pulmonary interstitial emphysema
Pneumothorax
pCO targets waived in response to a severe
complication
Days pCO targets waived
Postnatal dexamethasone treatment
Cumulative dexamethasone dose (mg)
58 (05462)
63 (07380)
137 (77%)
137 (77%)
51 (29%)
51 (29%)
2 (014)
25 (014)
013
029
10
10
059
25 (14%)
32 (18%)
032
8 (5%)
13 (7%)
027
32 (18%)
26 (14%)
038
4 (110)
3 (113)
045
30 (17%)
29 (16%)
081
065 (00648)
066 (010300)
38 (22%)
Outcomes
Cumulative hydrocortisone dose (mg)
88 (06219)
The primary outcome of the trial was death or
bronchopulmonary dysplasia before 36 weeks postmenstrual age according to the physiological denition
of bronchopulmonary dysplasiaie, requiring mechanical pressure support or supplemental oxygen at
36 weeks postmenstrual age within 2 days, including
an oxygen reduction test for infants requiring less than
03 FiO (bronchopulmonary dysplasia or death).24 The
bronchopulmonary dysplasia part of this denition also
represents moderate to severe bronchopulmonary
dysplasia according to the National Institute of Child
Health and Development (NICHD) consensus definition.21 Bronchopulmonary dysplasia status was established independent of caregiver assessments by a
computer algorithm, which applied the above denition
to collected clinical data as part of the statistical analysis.
Retinopathy of prematurity
78 (47%)
78 (47%)
Severe retinopathy grade 3
20 (11%)
26 (14%)
036
Necrotising enterocolitis grade 2
20 (12%)
8 (5%)
002
www.thelancet.com/respiratory Vol 3 July 2015
50 (28%)
09
Postnatal hydrocortisone treatment
58 (0590)
017
031
092
Weight at 36 weeks postmenstrual age (g)
1943 (12003120)
2000 (10002830)
076
Weight gain to 36 weeks postmenstrual age (g)
1244 (3252384)
1250 (2002030)
059
Data are n (%) with 2 test, median with Mann-Whiney U test (minmax), unless stated otherwise. *Primary outcome
of trial, p value by group sequential analysis. One additional patient with severe bronchopulmonary dysplasia died
1 day after completing 36 postmenstrual weeks. As diagnosed by the study radiologist; high target (n=178), one
ultrasound exam missing. One infant was transferred and no follow-up cranial ultrasound scans were available.
Table 2: Overall outcome indicators
Major secondary outcomes included the severity of
bronchopulmonary dysplasia according to the consensus
denition,21 and the incidence and severity of intracranial
haemorrhage according to Papile and colleagues.25
537
Articles
600
Control target
High target
70
500
60
400
50
300
40
200
30
100
20
0
7
8
Day of life
10
11
12
13
14
mm Hg
80
Figure 2: Daily mean values of the partial pressure of carbon dioxide (pCO2) in all patients who were intubated
at the time of measurement
Error bars indicate standard deviations, lower bars indicate numbers of patients contributing data. Shaded areas
indicate the target ranges of the high target and control groups. The pCO2 values were signicantly higher in
patients randomly assigned to the high target group than in those in the control target group (linear mixed eects
regression model; p<00001), although the high target range was frequently not achieved because of the patients
own respiratory eorts. The main reason for absent data was extubation.
600
Control target
High target
735
500
730
400
725
300
720
200
715
100
710
0
pH
740
0
1
10
11
12
13
14
Day of life
Figure 3: Daily mean values of the pH in all patients who were intubated at the time of measurement
Error bars indicate standard deviations, lower bars indicate numbers of patients contributing data. The pH values
were signicantly lower in patients randomly assigned to the high target group than in those in the control target
group (linear mixed eects regression model; p<00001). The main reason for absent data was extubation.
Cranial ultrasound examinations were done on the rst
day of life, at 1214 days, and at 36 weeks postmenstrual
age and were evaluated centrally by one masked
paediatric radiologist (GA). Retinopathy of prematurity
was routinely screened for and classied according to the
International Classication.26 Necrotising enterocolitis
was diagnosed when the clinical and radiological ndings
corresponded to stage II or higher according to the
staging criteria of Bell and colleagues.27
Statistical analysis
The sample size was calculated for the test according to
a group sequential design,28 allowing earlier termination
of enrolment in case a signicant dierence was detected
during scheduled interim analyses. A pre-trial primary
538
outcome rate of death or bronchopulmonary dysplasia
incidence of 47%, showing a 20% relative reduction (from
50% to 40%) with a power of 80% and a signicance level
of 5%, using a two-sided group sequential test with two
interim analyses, required a maximum sample size of
830 patients.
Predened secondary analyses were done by tests,
Students t tests, Mann-Whitney U tests, survival analyses,
and, for repeated measures, linear mixed eects regression
models. Subgroup analyses were done to test the hypothesis
that hypercapnia is of most benet to infants at the highest
risk of poor outcomes, by analysing interactions29 with loglinear Poisson regression with robust estimation of error
variance.30 The predened subgroups were infants in the
three birthweight strata, small for gestational age infants
dened (according to published German reference data31)
as birthweight less than 10th percentile for the gestational
age, and infants with more severe lung disease (FiO >04
or mean airway pressure >10 mbar for >4 h). Sex was added
post hoc to the subgroup analyses because of its importance
as a highly relevant risk factor.32
All analyses were done on an intention-to-treat basis. A
p value of less than 005 was deemed signicant. Sample
size calculation and interim and nal analyses of the
primary outcome were done with the software East
(Cytel Software Corporation, Cambridge, MA, USA) and
Addplan (Aptiv Solutions, Reston, VA, USA). For all other
analyses, SAS software (SAS Institute, Cary, NC, USA)
was used.
Early in 2012, an amendment of the study protocol was
developed to allow for the interim analysis requested by
the review board of the funding agency. The sequential
designs boundaries had not been exceeded at that time (ie,
there were no detectable signicant dierences). The study
design was changed from a three-stage group sequential
design into a two-stage adaptive group sequential design
with one interim analysis. The amendment was approved
by the DSMB and the lead investigators responsible
institutional review board. The interim analysis was based
on 312 completed infants and carried out by an independent
statistician (BM; appendix p 10). The results were presented
to the DSMB, which recommended terminating
enrolment. The funding agencys review board concurred
with this recommendation and it was implemented by the
study coordinator.
This trial is registered with the ISRCTN registry, number
ISRCTN56143743.
Role of the funding source
The funding agencys review board requested the interim
analysis early in 2012, when it became clear that the
recruitment rate would remain below the original
projections. Apart from this request, the funding agency
had no role in data collection, analysis, and interpretation,
nor in writing the report. Access to the raw data was
limited to the data manager (MZ) and the statistician
(JD). The corresponding author (UHT) had full access to
www.thelancet.com/respiratory Vol 3 July 2015
Articles
all of the data and ultimate responsibility for submission
for publication.
www.thelancet.com/respiratory Vol 3 July 2015
Proportion of intubated infants (%)
Between March 1, 2008, and July 31, 2012, we screened
1534 infants and recruited 362, of whom three had to be
excluded: two because parental consent was withdrawn
and one after being mistakenly randomly assigned despite
meeting an exclusion criterion (malformation), leaving
359 patients (179 in the high target group, 180 in the
control group) for the intention-to-treat analysis (gure 1).
Table 1 shows baseline demographic and clinical
characteristics of the two groups.
The primary endpoint of bronchopulmonary dysplasia or
death was met in 36% of patients in the high target group
and 30% in the control group, which was not a signicant
dierence according to the Addplan analysis (table 2).
Looking separately at the components of the composite
primary outcome (ie, requirement for mechanical support
or supplemental oxygen and mortality, either at an age of
28 days or at 36 weeks postmenstrual age), there were no
signicant dierences. Comparisons of bronchopulmonary
dysplasia severity according to the consensus denition21
were also inconclusive.
Day-by-day mean values of pCO and pH diered
signicantly between study groups (gures 2 and 3).
The pCO dierence peaked at 7 mm Hg on day 4 and
the mean dierence between days 2 and 11 was
62 mm Hg. Furthermore, infants in the high target
group had signicantly lower values for peak inspiratory
pressure (appendix p 5), suggesting increased weaning
eorts in the high target group. Tidal volumes were not
measured at all centres, and no signicant dierences
were detectable (appendix p 6).
The incidence of intraventricular haemorrhage was
similar in both groups, as were the incidence of
retinopathy of prematurity, periventricular leukomalacia,
hydrocephalus, and air leaks (table 2). Infants in the high
target group had a signicantly higher rate of necrotising
enterocolitis. Weight gain was similar in both groups.
Typical for modern neonatal care, we used dierent
ventilation methods across dierent study sites (appendix
p 7); the choice of ventilation modes did not dier
signicantly between study groups. However, nal
independence from the ventilator and supplemental
oxygen was not accelerated by the high target (gures 4
and 5).
We noted no signicant interactions of risk factors with
the primary outcome of bronchopulmonary dysplasia or
death. In the predened analyses, we did not identify a
subgroup that might have beneted from the high target
(table 3). Furthermore, all interactions were nonsignicant. However, in infants with severe lung disease,
the high target was associated with a higher incidence of
bronchopulmonary dysplasia or death.
The signicantly increased incidence of necrotising
enterocolitis prompted another unplanned subgroup
High target
Control target
Censored
75
50
25
0
0
20
40
60
80
100
Day of life
Figure 4: Kaplan-Meier analysis of weaning from invasive mechanical
ventilation
There was no signicant dierence between groups (p=018, log-rank test).
Circles indicate censored datapoints. Censoring generally occurred in patients
who were still intubated on day of life 99 or in patients who died.
100
Proportion of infants
on supplemental oxygen (%)
Results
100
High target
Control target
Censored
75
50
25
0
0
20
40
60
80
100
Day of life
Figure 5: Kaplan-Meier analysis of weaning from supplemental oxygen
There was no signicant dierence between groups (p=025, log-rank test).
Circles indicate censored datapoints. Censoring generally occurred in patients
who were still on positive pressure or supplemental oxygen on day of life 99 or
in patients who died.
analysis, which showed an association between the
incidence of necrotising enterocolitis and the high target
in infants with severe lung disease (p=006) and in
infants with 500749 g birthweight (p<001; table 4).
During the follow-up, there were three additional
deaths. Of these, two of the infants (one in the high
target group, one in the control group) had been
classied for the primary outcome as having
bronchopulmonary dysplasia and died within the rst
year. The third, in the high target group, had not met
our bronchopulmonary dysplasia criteria and died at
2 years corrected age.
Discussion
The high pCO target did not reduce the primary outcome.
Our results should be interpreted in view of the protocol
specications for this trial. Infants were only eligible
539
Articles
High target group Control group
(n=179)
(n=180)
Overall
Risk ratio (95% CI) pinteraction
65 (36%)
54 (30%)
121 (090163)
400499
14/22 (64%)
10/18 (56%)
115 (068193)
500749
39/83 (47%)
32/90 (36%)
132 (092189)
7501000
12/74 (16%)
12/72 (17%)
097 (047202)
Small for gestational age
(birthweight <10th percentile)
21/35 (60%)
18/41 (44%)
137 (088212)
Appropriate for gestational age
(birthweight 10th percentile)
44/144 (31%)
36/139 (26%)
118 (081171)
Infants with severe lung disease
37/64 (58%)
29/72 (40%)
144 (101204)*
Infants without severe lung disease
28/115 (24%)
25/108 (23%)
105 (066168)
Boy
40/105 (38%)
36/99 (36%)
105 (073150)
Girl
25/74 (34%)
18/81 (22%)
152 (091255)
Groups according to birthweight (g)
074
Infants small for gestational age
062
Severe lung disease
030
Sex
024
Data are n (%). Eect of intervention according to baseline characteristics (log-linear Poisson regression with robust
estimation of error variance for bronchopulmonary dysplasia or death).*Signicantly increased risk associated with the
high target (p=004).
Table 3: Subgroup analyses for eect on moderate or severe bronchopulmonary dysplasia or death at
36 weeks postmenstrual age
High target
group
Control
group
p value
More severe lung disease
10/61 (16%)
4/68 (6%)
006
Less severe lung disease
10/113 (9%)
4/106 (4%)
012
Birthweight (g)
400499
2/21 (10%)
1/17 (6%)
039
500749
14/79 (18%)
5/89 (6%)
p<001
7501000
4/74 (5%)
2/68 (3%)
068
Data are n (%) with test.
Table 4: Subgroup analyses for necrotising enterocolitis stage 2
when they needed endotracheal intubation and invasive
mechanical ventilation because pCO control is very
limited in non-intubated infants. In combination with
increasing clinical eorts to avoid invasive mechanical
ventilation altogether,17,33,34 eligible infants were only a
minor fraction of the admitted extremely low birthweight
infants, and this markedly slowed enrolment. However,
including only intubated infants led to the selection of less
stable infants who were more likely to have pronounced
respiratory distress syndrome, and thus to a highly
relevant trial population with regard to the questions
under investigation. Enrolment, initially projected for
3 years, was terminated after the interim analysis done in
the fourth year. Several considerations played a part in this
decision. First, the interim analysis showed no benet,
and a possible trend favouring the control rather than the
high target group. This nding suggested that it was futile
to continue recruitment because a benet to the high
target group showing over the remainder of the trial had
540
become extremely unlikely. Second, proving the opposite,
a worse outcome in the high target group, would not
change current standard of care. Third, ethical concerns
were raised about the need to randomly assign hundreds
of additional patients to achieve the original sample size
with limited further scientic gain, whereas other
multicentre trials poised to test important hypotheses
were held back. Fourth, too many changes to clinical
standards can confound trial results if patient recruitment
exceeds more than 35 years.
Although the study nished prematurely, the sample
size was still higher than the sum of all three previously
published trials, in which investigators had enrolled only
intubated infants and randomly assigned them into
dierent pCO target groups.1416 Furthermore, we
recorded higher pCO dierences between groups.
Despite the preference for higher risk infants who needed
mechanical ventilation in settings in which non-invasive
support was the rule, the overall rate of bronchopulmonary
dysplasia or death was lower in our trial, perhaps because
of continuous improvements in care. However, the
results of the three previous trials, an older meta-analysis
of two of these trials,18 and this trial, were similar, showing
no dierences in the rates for primary outcome between
the study groups.
Dierent pCO targets were also used in the very large
SUPPORT trial,17 which enrolled 1316 infants and
compared a strategy favouring non-invasive continuous
positive airway pressure and an upper pCO limit of
65 mm Hg for intubation and extubation with a strategy
of using primary intubation, surfactant administration,
and an upper pCO limit of 50 mm Hg. However, there
were no lower limits for the pCO and actual pCO values
were not reported. Like previous trials of hypercapnia and
our trial, the SUPPORT trial found no dierence in the
primary outcome. However, time spent on mechanical
ventilation was shorter in the continuous positive airway
pressure and hypercapnia group, which is probably the
result of the study protocol favouring extubation to
continuous positive airway pressure in this group.
Available data suggest that the encouraging trend towards
a better outcome in the continuous positive airway
pressure group of the SUPPORT trial might be more
related to favouring continuous positive airway pressure
and avoiding mechanical ventilation13 than to favouring
hypercapnia. Nasal continuous positive airway pressure
could have intrinsic benets, which might include full
control of expiratory braking by the vocal cords and a
large leak to discharge excessive air quickly if necessary.
Several considerations led to the selection of the pCO
targets for this trial. No optimum pCO target range has
ever been dened. Data from bench research and clinical
trials in adults suggested the benecial eects of
hypercapnia and hypercapnic acidosis.5,35 In preterm
infants, secondary and subgroup analyses of the
prematurely terminated SAVE multicentre trial suggested
reduced need for prolonged mechanical ventilation was
www.thelancet.com/respiratory Vol 3 July 2015
Articles
associated with mild hypercapnia16 as compared with
normocapnia, without adverse eects. Mild hypercapnia
has since been increasingly introduced into routine care,
and discussion centred on how high to increase the pCO
goal to maximise benets. Additionally, the risk of
accidental hypocapnia fell.36 Consequently, a control
group with a normocapnic pCO target of 3545 mm Hg
seemed unethical and a mildly hypercapnic target range
was chosen. Because previous trials had been criticised
for their small pCO dierences, the high target group
was planned with much higher pCO targets to increase
the dierence in pCO between the groups, although it
was anticipated that these targets might not always be
achieved because of increased respiratory eorts by the
patients. Furthermore, we assumed that lung protection
might be increased with higher pCO goals, because
ventilator requirements and mechanical forces are
decreased, and biochemical benets of a high pCO
might depend on its concentration.37 Finally, stepwise
increases of the target ranges of both groups were
included because this was standard practice in the
participating units to help with weaning o mechanical
ventilation. We kept the planned dierence between
groups constant. Therefore, our trial is a comparison of
two dierent ranges of hypercapnia, one higher than the
other, particularly after the rst 3 days of life.
In view of these considerations, our results are
surprising. Signicantly lower ventilator pressures in the
high target group did not translate into better outcomes.
Furthermore, the most important outcomes tended to
favour the control group rather than the high target group,
arguing against the benets of a high target that might
have been missed because of the smaller-than-intended
sample size or the smaller-than-intended pCO dierence.
To explain the negative results, we hypothesised that
only infants who were extremely ill beneted from the
high target. The predened subgroup analyses had been
designed to address this hypothesis, but had low power
owing to limited sample sizes. However, our results
suggested that there was no benecial eect associated
with the high target for even the smallest infants,
consistent with subgroup analyses of the SUPPORT
trial.17 Furthermore, in infants with more severe lung
disease, the high target might have been associated with
detrimental eects, according to our data. Similarly, a
reanalysis of the SUPPORT trial showed associations
between high pCO values and adverse outcomes.38
Lung protective ventilation is a complex issue, and the
pCO is just one factor. Low ventilator pressure might be
lung protective, or lead to increased lung injury if
atelectasis formation is not prevented. However, the
most important determinant is a low tidal volume,3 and a
higher pCO might be a surrogate marker for lower tidal
volumes when other ventilatory parameters are kept
constant. As shown in experimental models,39,40 additional
lung protection can arise from the biochemical eects of
higher pCO and lower pH. On the other hand, high
www.thelancet.com/respiratory Vol 3 July 2015
pCO and corresponding low pH values might also have
harmful side-eects that outweigh any benets, and this
could explain why the high pCO target was not
associated with an improved outcome in this trial.5,41,42
Indeed, there were no pH limits, rstly because lower
pH limits for premature infants have not been dened,
and, second, the only way to correct a low pH while
maintaining hypercapnia is by bicarbonate infusion,
which itself can have negative side-eects22,23 and thus be
a possible confounder. To prevent such a confounding
eect and promote equal bicarbonate use in both study
groups, we used bicarbonate administration to correct
the pH when the base decit rather than the pH exceeded
a limit. Consequently, the varying use of bicarbonate was
not signicantly dierent between the two study groups,
but resulted in lower pH values in the high target group.
Therefore, important enzymes could have been too far
outside their optimum pH to function as needed in the
high target group, which could have, along with other
eects, impaired wound repair in injured lungs43,44 and
alveolar uid clearance45 under hypercapnic conditions.
In this case, the most severely injured lungs would be
most aected, as suggested by the respective subgroup
analysis. Similar eects of hypercapnic acidosis could
also have impaired the function of intestinal cells and
might have caused the signicantly higher rate of
necrotising enterocolitis in the high target group,
because an association between acidosis and NEC has
already been described.46 Alternatively, the diering NEC
rate might be an incidental nding because we did
several univariate analyses.
As in general neonatal care, we used dierent ventilation
modes. Most of the newer modes have not been proven to
be more benecial in rigorous large-scale clinical trials.
Additionally, the measurement of tidal volume or
synchronisation of ventilation with an in-line ow sensor
at the expense of a higher dead space, possibly increasing
the need for mechanical support, has not been shown to
reduce lung injury and lead to better outcomes in extremely
low birthweight infants. Therefore, some centres in our
study group avoided using ow sensors (appendix p 7).
The use of ow sensors did not have a signicant eect on
the outcomes of this trial (data not shown).
We noted no increases of intraventricular haemorrhage
or retinopathy of prematurity attributable to the high
target. The rate of IVH might seem high, but only the
less stable infants with the highest risk for IVH were
eligible for this trial. Severe IVH (grade 3 or 4) might
seem slightly more frequent in the high target group, but
there were already a few more cases of severe IVH
present on day 1ie, before the protocol specications
had been fully enforced. Likewise, ndings of previous
trials did not show an increased incidence of IVH
associated with permissive hypercapnia.1417,47 Data from
previous retrospective analyses had already suggested
that uctuations of pCO2 were more strongly associated
with IVH than sustained high values.48,49
541
Articles
The main limitation of this trial is probably its
premature cessation, reducing statistical power to answer
the pertinent questions. Furthermore, the pCO values
were lower than intended in the high target group, which
could be attributed either to the patients own respiratory
drive, or to insucient adherence to the protocol by the
clinicians. The signicantly lower peak inspiratory
pressure values in the high target group probably reect
the clinicians attempts to minimise ventilation and let
the pCO rise in accordance with the protocol. Clinical
decisions on choosing ventilator settings were not only
driven by pCO targets but tended to be more complex.
Looking at the collected data on ventilator settings, these
decisions did not always follow the study protocol.
However, our trial represents a pragmatic comparison of
two management strategies in daily clinical care.
In any case, all ndings should be interpreted with
appropriate caution. Previous trials also failed to fully
achieve pCO targets in the high target groups,1416 which
suggests that the target ranges in the high target group
were impossible to achieve in most infants most of the
time and probably should not be attempted either
clinically or in future studies.
In summary, we recorded no signicant dierence in
the primary outcome of bronchopulmonary dysplasia or
death between the two pCO target groups in infants
requiring intubation and mechanical ventilation. We
conclude that managing extremely low birthweight
infants with pCO targets according to the high target
group, as compared with the control group, is not
associated with improved outcomes. Moreover, the high
target might be associated with an increased incidence
of necrotising enterocolitis, and in infants with more
severe lung disease, with an increased incidence of
bronchopulmonary dysplasia or death, and therefore
cannot be recommended.
Contributors
UHT was the study coordinator and lead investigator and wrote the
grant application and institutional review board application, developed
and drafted the study protocol, co-developed the statistical analysis plan,
recruited patients, gathered data, and wrote the manuscript, and
generated gures; OG-B developed the study protocol, recruited patients,
gathered data, and edited the manuscript; BB developed the study
protocol, recruited patients, gathered data, edited the manuscript; MS,
HF, OR, SA, DF, AZ, BK, HB, WS, HS, NT, and RH developed the study
protocol, recruited patients, gathered data, and edited the manuscript;
HF developed the study protocol, recruited patients, gathered data, and
edited the manuscript; H-GT, KT, and CG recruited patients, gathered
data, and edited the manuscript; MH, RS, JP, RR, and JS developed the
study protocol, recruited patients, and edited the manuscript; WR and
GH developed the study protocol, and edited the manuscript; RB
recruited patients, gathered data, and edited the manuscript; MZ
programmed the study database, managed data and queries, entered
data into the database, and edited the manuscript; GA developed the
study protocol, analysed all cranial ultrasound exams, selected chest
radiographs, and edited the manuscript; JD developed the nal statistical
analysis plan and the protocol amendment, carried out the statistical
analyses, generated gures, and edited the manuscript; RM developed
the study protocol, initial statistical plan, sample size calculation, and
edited the manuscript; and HDH had the initial idea to do this study,
edited the grant application, developed the study protocol, recruited
patients, gathered data, and edited the manuscript.
542
Declaration of interests
We declare no competing interests.
Acknowledgments
This trial was funded by the Deutsche Forschungsgemeinschaft
(German Research Foundation, DFG, project number Th626/5-1),
which is taxpayer funded. The trial underwent extensive review by
anonymous expert reviewers before funding was approved by the
funding agencys review board. We thank the parents of our infants for
their consent and support of this project, which was given at a very
dicult time; all physicians and nurses who worked in the participating
units, many without being directly involved in this project, for their
support; and Waldemar A Carlo, Namasivayam Ambalavanan, and
Frank Pohlandt for their invaluable advice in developing the study
protocol and writing this manuscript; Sabine Schmid for entering data,
and Evelyn Killick for language editing.
References
1
Baraldi E, Filippone M. Chronic lung disease after premature birth.
N Engl J Med 2007; 357: 194655.
2
Greenough A, Alexander J, Burgess S, et al. Home oxygen status and
rehospitalisation and primary care requirements of infants with
chronic lung disease. Arch Dis Child Fetal Neonatal Ed 2002; 86: 4043.
3
Dreyfuss D, Saumon G. Ventilator-induced lung injury: lessons
from experimental studies. Am J Respir Crit Care Med 1998;
157: 294323.
4
Bjoerklund LJ, Ingimarsson J, Curstedt T, et al. Manual ventilation
with a few large breaths at birth compromises the therapeutic eect
of subsequent surfactant replacement in immature lambs.
Pediatr Res 1997; 42: 34855.
5
Curley G, Laey JG, Kavanagh BP. Bench-to-bedside review: carbon
dioxide. Crit Care 2010; 14: 220.
6
Kaiser JR, Gauss CH, Pont MM, Williams DK. Hypercapnia during
the rst 3 days of life is associated with severe intraventricular
hemorrhage in very low birth weight infants. J Perinatol 2006;
26: 27985.
7
Holmes JM, Zhang S, Leske DA, Lanier WL. Carbon dioxide-induced
retinopathy in the neonatal rat. Curr Eye Res 1998; 17: 60816.
8
Kraybill EN, Runyan DK, Bose CL, Khan JH. Risk factors for
chronic lung disease in infants with birth weights of 751 to
1000 grams. J Pediatr 1989; 115: 11520.
9
Garland JS, Buck RK, Allred EN, Leviton A. Hypocarbia before
surfactant therapy appears to increase bronchopulmonary dysplasia
risk in infants with respiratory distress syndrome.
Arch Pediatr Adolesc Med 1995; 149: 61722.
10 Van Marter LJ, Allred EN, Pagano M, et al. Do clinical markers of
barotrauma and oxygen toxicity explain interhospital variation in
rates of chronic lung disease? The Neonatology Committee for the
Developmental Network. Pediatrics 2000; 105: 1194201.
11 Subramanian S, El-Mohandes A, Dhanireddy R, Koch MA.
Association of bronchopulmonary dysplasia and hypercarbia in
ventilated infants with birth weights of 500-1,499 g.
Matern Health J 2011; 15 (suppl 1): S1726.
12 The Acute Respiratory Distress Syndrome Network. Ventilation
with lower tidal volumes as compared with traditional tidal volumes
for acute lung injury and the acute respiratory distress syndrome.
N Engl J Med 2000; 342: 130108.
13 Fischer HS, Bhrer C. Avoiding endotracheal ventilation to prevent
bronchopulmonary dysplasia: a meta-analysis. Pediatrics 2013;
132: e135160.
14 Mariani G, Cifuentes J, Carlo WA. Randomized trial of
permissive hypercapnia in preterm infants. Pediatrics 1999;
104: 108288.
15 Thome UH, Carroll WF, Wu T-J, et al. Outcome of extremely
preterm infants randomised at birth to dierent PaCO2 targets
during the rst seven days of life. Biol Neonate 2006; 90: 21825.
16 Carlo WA, Stark AR, Wright LL, et al. Minimal ventilation to
prevent bronchopulmonary dysplasia in extremely low birthweight
infants. J Pediatr 2002; 141: 37074.
17 Finer NN, Carlo WA, Walsh MC, et al. Early CPAP versus surfactant
in extremely preterm infants. N Engl J Med 2010; 362: 19709.
18 Woodgate PG, Davies MW. Permissive hypercapnia for the
prevention of morbidity and mortality in mechanically ventilated
newborn infants. Cochrane Database Syst Rev 2001; 2: CD002061.
www.thelancet.com/respiratory Vol 3 July 2015
Articles
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
Hermeto F, Bottino MN, Vaillancourt K, SantAnna GM.
Implementation of a respiratory therapist-driven protocol for
neonatal ventilation: impact on the premature population. Pediatrics
2009; 123: e90716.
Van Kaam AH, De Jaegere AP, Rimensberger PC, on behalf of the
Neovent Study Group. Incidence of hypo- and hyper-capnia in a
cross-sectional European cohort of ventilated newborn infants.
Arch Dis Child Fetal Neonatal Ed 2013; 98: F32326.
Ehrenkranz RA, Walsh MC, Vohr BR, et al. Validation of the
National Institutes of Health consensus denition of
bronchopulmonary dysplasia. Pediatrics 2005; 116: 135360.
Laey JG, Engelberts D, Kavanagh BP. Buering hypercapnic
acidosis worsens acute lung injury. Am J Respir Crit Care Med 2000;
161: 14146.
Higgins BD, Costello J, Contreras M, Hassett P, OToole D,
Laey JG. Dierential eects of buered hypercapnia versus
hypercapnic acidosis on shock and lung injury induced by systemic
sepsis. Anesthesiology 2009; 111: 131726.
Walsh MC, Wilson-Costello D, Zadell A, Newman N, Fanaro A.
Safety, reliability, and validity of a physiologic denition of
bronchopulmonary dysplasia. J Perinatol 2003; 23: 45156.
Papile LA, Burstein J, Burstein R, Koer H. Incidence and
evolution of subependymal and intraventricular hemorrhage: a
study of infants with birth weights less than 1,500 gm.
J Pediatr 1978; 92: 52934.
The International Classication of Retinopathy of Prematurity
revisited. Arch Ophthalmol 2005; 123: 99199.
Bell MJ, Ternberg JL, Feigin RD, et al. Neonatal necrotizing
enterocolitis. Therapeutic decisions based upon clinical staging.
AnnSurg 1978; 187: 17.
Pampallona S, Tsiatis AA. Group sequential designs for one-sided
and two-sided hypothesis testing with provision for early stopping
in favor of the null hypothesis. J Stat Plan Inference 1994; 42: 1935.
Wang R, Lagakos SW, Ware JH, Hunter DJ, Drazen JM. Statistics in
medicinereporting of subgroup analyses in clinical trials.
N Engl J Med 2007; 357: 218994.
Zou G. A modied poisson regression approach to prospective
studies with binary data. Am J Epidemiol 2004; 159: 70206.
Voigt M, Rochow N, Straube S, Briese V, Olbertz D, Jorch G. Birth
weight percentile charts based on daily measurements for very
preterm male and female infants at the age of 154-223 days.
J Perinat Med 2010; 38: 28995.
Jensen EA, Schmidt B. Epidemiology of bronchopulmonary
dysplasia. Birth Defects Res A Clin Mol Teratol 2014; 100: 14557.
Dargaville PA, Aiyappan A, Cornelius A, Williams C, De Paoli AG.
Preliminary evaluation of a new technique of minimally invasive
surfactant therapy. Arch Dis Child Fetal Neonatal Ed 2011; 96: F2438.
Vendettuoli V, Bellu R, Zanini R, Mosca F, Gagliardi L, for the
Italian Neonatal Network. Changes in ventilator strategies and
outcomes in preterm infants. Arch Dis Child Fetal Neonatal Ed 2014;
99: F32124.
www.thelancet.com/respiratory Vol 3 July 2015
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
Thome UH, Ambalavanan N. Permissive hypercapnia to decrease
lung injury in ventilated preterm neonates. Semin Neonatal Med 2009;
14: 2127.
Laey JG, Kavanagh BP. Hypocapnia. N Engl J Med 2002;
347: 4353.
Fuchs H, Mendler MR, Scharnbeck D, Ebsen M, Hummler HD.
Very low tidal volume ventilation with associated hypercapnia
eects on lung injury in a model for acute respiratory distress
syndrome. PloS One 2011; 6: e23816.
Ambalavanan N, Carlo WA, Wrage LA, et al. PaCO2 in Surfactant,
Positive Pressure, and Oxygenation Randomised Trial (SUPPORT).
Arch Dis Child Fetal Neonatal Ed 2014; published online Nov 25.
http://fn.bmj.com/content/early/2014/11/25/
archdischild-2014-306802.abstract.
Strand M, Ikegami M, Jobe AH. Eects of high pCO2 on ventilated
preterm lamb lungs. Pediatr Res 2003; 53: 46872.
Laey JG, Honan D, Hopkins N, Hyvelin JM, Boylan JF,
McLoughlin P. Hypercapnic acidosis attenuates endotoxin-induced
acute lung injury. Am J Respir Crit Care Med 2004; 169: 4656.
Ryu J, Heldt GP, Nguyen M, Gavrialov O, Haddad GG. Chronic
hypercapnia alters lung matrix composition in mouse pups.
J Appl Physiol 2010; 109: 20310.
Vadasz I, Hubmayr RD, Nin N, Sporn PH, Sznajder JI.
Hypercapnia: a nonpermissive environment for the lung.
Am J Respir Cell Mol Biol 2012; 46: 41721.
Doerr CH, Gajic O, Berrios JC, et al. Hypercapnic acidosis impairs
plasma membrane wound resealing in ventilator-injured lungs.
Am J Respir Crit Care Med 2005; 171: 137177.
Lang JD, Figueroa M, Sanders KD, et al. Hypercapnia via reduced
rate and tidal volume contributes to lipopolysaccharide-induced
lung injury. Am J Respir Crit Care Med 2005; 171: 14757.
Briva A, Vadasz I, Lecuona E, et al. High CO2 levels impair alveolar
epithelial function independently of pH. PLoS One 2007; 2: e1238.
Gephart SM, Spitzer AR, Eken JA, Dodd E, Halpern M,
McGrath JM. Discrimination of GutCheckNEC: a clinical risk index
for necrotizing enterocolitis. J Perinatol 2014; 34: 46875.
Hagen EW, Sadek-Badawi M, Carlton DP, Palta M. Permissive
hypercapnia and risk for brain injury and developmental
impairment. Pediatrics 2008; 122: e58389.
Fabres J, Carlo WA, Phillips V, Howard G, Ambalavanan N. Both
extremes of arterial carbon dioxide pressure and the magnitude of
uctuations in arterial carbon dioxide pressure are associated with
severe intraventricular hemorrhage in preterm infants.
Pediatrics 2007; 119: 299305.
McKee LA, Fabres J, Howard G, Peralta-Carcelen M, Carlo WA,
Ambalavanan N. PaCO2 and neurodevelopment in extremely low
birth weight infants. J Pediatr 2009; 155: 21721.
543
Comment
Arg117His-CFTR status has direct relevance to newborn
screening programmes for cystic brosis. Inclusion of
Arg117His-CFTR in screening panels leads to identication
of infants who have a very low likelihood of developing
cystic brosis lung disease, at least during childhood.
Removing the Arg117His-CFTR mutation from newborn
screening panels has been advocated.9 This position will
need to be reassessed in view of Moss and colleagues
results,6 since ivacaftor will probably play an important
part in treating Arg117His/5T-CFTR and might well be of
benet in those few patients with Arg117His/7T-CFTR
who have lung disease.
These data6 are therefore an important contribution to
the medical literature, since they provide clear support
for the treatment of patients with Arg117His-CFTR. The
results also show CFTR activity in children as well as in
adults, providing a rationale for the treatment of some
children. Whether patient-specic response to ivacaftor
can be predicted from specimens studied ex vivoeg,
nasal epithelial cells or intestinal organoidsremains
to be claried.10 Long-term studies to assess the safety
and ecacy of ivacaftor in general are also needed. In
this respect, evidence that the drug can modify the
rate of decline in lung function or the development of
structural injury will be important. Finally, the results
from Moss and colleagues study reinforce the notion of
mutation-specic treatment of CFTR dysfunctionan
important step on the road to personalised care for all
individuals with cystic brosis.
Frank J Accurso
University of Colorado and Childrens Hospital Colorado, Aurora,
CO 80045, USA
Frank.Accurso@ucdenver.edu
I have served on the Cystic Fibrosis Foundation Therapeutics, Inc./Vertex
Pharmaceuticals, Inc. Joint Development Committee since 2003. The purpose
of this committee is to improve the communication between the two groups.
I represent Cystic Fibrosis Foundation Therapeutics, Inc. in these discussions
and have no ties, nancial or otherwise, with Vertex Pharmaceuticals, Inc.
I receive reimbursement from Cystic Fibrosis Foundation Therapeutics, Inc. for
the twice a year in-person committee meetings only for plane fare, lunch, and
parking. I do not receive any remuneration from Cystic Fibrosis Foundation
Therapeutics, Inc. for time or eort. I receive no remuneration at all from
Vertex Pharmaceuticals, Inc.
1
2
3
8
9
10
Rowe SM, Miller S, Sorscher EJ. Cystic brosis. N Engl J Med 2005;
352: 19922001.
Stoltz DA, Meyerholz DK, Welsh MJ. Origins of cystic brosis lung disease.
N Engl J Med 2015; 372: 157475.
Van Goor F, Hadida S, Grootenhuis, et al. Rescue of CF airway epithelial cell
function in vitro by a CFTR potentiator, VX-770. Proc Natl Acad Sci USA
2009; 106: 1882530.
Ramsey BW, Davies J, McElvaney NG, et al. VX08-770-102 Study Group.
A CFTR potentiator in patients with cystic brosis and the G551D
mutation. N Engl J Med 2011; 365: 166372.
De Boeck K, Munck A, Walker S, et al. Ecacy and safety of ivacaftor in
patients with cystic brosis and a non-G551D gating mutation. J Cyst Fibros
2014; 13: 67480.
Moss RB, Flume PA, Elborn JS, et al, on behalf of the VX11-770-110
(KONDUCT) Study Group. Ecacy and safety of ivacaftor in patients with
cystic brosis who have an Arg117His-CFTR mutation: a double-blind,
randomised controlled trial. Lancet Respir Med 2015; 3: 52433.
Kiesewetter S, Macek M Jr, Davis C, et al. A mutation in CFTR produces
dierent phenotypes depending on chromosomal background. Nat Genet
1993; 5: 27478.
Witt DR, Schaefer C, Hallam P, et al. Cystic brosis heterozygote screening
in 5161 pregnant women. Am J Hum Genet 1996; 58: 82335.
Thauvin-Robinet C, Munck A, Huet F, et al. The very low penetrance of
cystic brosis for the R117H mutation: a reappraisal for genetic counselling
and newborn screening. J Med Genet 2009; 46: 75258.
Dekkers JF, van der Ent CK, Beekman JM. Novel opportunities for
CFTR-targeting drug development using organoids. Rare Dis 2013;
1: e27112.
Permissive hypercapnia in preterm infants: the discussion
continues
During the past decade the threshold of viability in
extremely preterm infants has shifted to the lower
gestational age of younger than 26 weeks postmenstrual
age with subsequent improved survival. As a
consequence, more of the survivors have to be treated
for typical co-morbidities of extreme prematurity such
as brochopulmonary dysplasia. The latter is associated
with extreme prematurity and ventilator-induced lung
injury. Data from small studies have suggested that
permissive hypercapnia might reduce the incidence
of lung injury, and as a result the German multicentre
PHELBI study group1 embarked on a large randomised
www.thelancet.com/respiratory Vol 3 July 2015
controlled study of 830 extremely low birthweight
infants testing two levels of partial pressures of
carbon dioxide (PCO2) during the rst 2 weeks of life.
The study was stopped prematurely after an interim
analysis of 359 (23%) of 1534 infants screened in
53 months, in which investigators noted no dierence
in the primary outcome of death or moderate to severe
bronchopulmonary dysplasia between groups.
We would like to commend the authors and the
journal for publishing the no dierence ndings as the
report contains lessons to be learned. The study included
preterm infants from 23 to 28 weeks gestation onwards.
Published Online
June 16, 2015
http://dx.doi.org/10.1016/
S2213-2600(15)00240-4
See Articles page 534
499
Roger Job/Reporters/Science Photo Library
Comment
The incidence of bronchopulmonary dysplasia is highest
in infants younger than 28 weeks and therefore this
was an appropriate target population. Of note is the
long duration of recruitment of more than 4 years.
Clinical practice might have changed during this time
especially with the increasing use of non-invasive means
of respiratory support to wean or avoid intratracheal
ventilation altogether.2 During non-invasive ventilator
support PCO2 concentrations are established by the
breathing eorts of newborn babies and clinicians are
less able to aect the concentrations directly. Future
studies will need to consider this growing group of
patients and would benet from new non-invasive
techniques such as plethysmogram analysis of pulse
oximetry traces to measure spontaneous breathing
rates together with PCO2 concentrations.3
In the PHELBI study, PCO2 target concentrations were
aimed at three increasing levels in the rst 14 days
of life.1 The study design might have inadvertently
aected the clinicians decision to ventilate newborn
babies to achieve the PCO2 targets during the study
period. It was not possible to mask the clinicians to
group allocations. After 14 days, 25% of infants were
still ventilated. In the present trend of neonatal clinical
care to wean to non-invasive ventilation as soon as
possible, many tertiary care centres would consider this
intubation rate to be high.2
The PHELBI study group targeted the lung injury
aspect of bronchopulmonary dysplasia by using low
tidal volume ventilation strategies without controlling
500
for it with volume-targeted ventilation methods that
help to reduce lung injury. Results of recent animal
studies have also shown that lung injury starts early at
resuscitation at birth and could be improved by allowing
redistribution of placental blood through delaying cord
cutting and initiating lung expansion rst.4 Findings of
the study by Polglase and colleagues4 in preterm lambs
showed a smoother transition to extrauterine life after
birth if the lambs were given ination breath with their
cord intact. This method enabled a smooth increase in
pulmonary blood ow with expansion of lung alveoli.4
Benets of redistribution of placental blood in preterm
infants such as better adaptation after birth, less need
for blood transfusion, less incidence of intraventricular
haemorrhage and necrotising enterocolitis have
been widely described and therefore have been
incorporated into international guidelines on newborn
resuscitation.58
The PHELBI study group did not collect information
about whether the recruited infants received standardised delivery room management and subsequent
stabilisation to minimise lung injury, including any
means of redistribution of placental blood before
enrolment into the study. Future studies of the
reduction of lung injury and the development of
bronchopulmonary dysplasia should include this aspect
of resuscitation of the preterm infant. This approach
would need antenatal consent to enrol the preterm
infant into the trial. Findings of a recently published
qualitative study of parents showed a positive attitude
towards enrolling their unborn preterm baby into
a randomised trial to study two dierent ways of
enhancing redistribution of placental blood at birth.9,10
Increasing data seem to suggest that the lower the
gestational age the more varying practices between
hospitals will aect the outcome of preterm infants.11
With the participation of many centres in increasingly
larger randomised controlled trials over a long time
(like the PHELBI study), accounting for comparative
eectiveness between centres (ie, alternative standards
of care, assessing outcomes important to individuals,
and incorporating varied settings and participants)
becomes an important part of outcome assessment.12
Much still needs to be learnt about lung injury and
the development of bronchopulmonary dysplasia
in extremely low birthweight infants. The pattern
of respiratory distress syndrome in these infants has
www.thelancet.com/respiratory Vol 3 July 2015
Comment
changed over the past 10 years. The introduction
of antenatal steroids has changed the incidence of
severe respiratory distress syndrome. Researchers can
now look at other preventive measures at the time of
resuscitation at birth,5 which might have more eect
than PCO2 concentrations in the rst day of life or
dierent ventilation strategies such as low volume
ventilation or patient synchronised ventilation. The
PHELBI study provides the basis for further discussions
on how to design future study protocols. Optional
antenatal consent will probably increase recruitment
in trials of extremely low birthweight infants of 23 to
28 weeks gestation.
Heike Rabe, Jose Ramon Fernandez-Alvarez
Brighton and Sussex Medical School and University Hospitals,
Academic Department of Paediatrics, Royal Alexandra Childrens
Hospital, Brighton BN2 5BE, UK
Heike.Rabe@bsuh.nhs.uk
10
We declare no competing interests.
11
Thome UH, Genzel-Boroviczeny O, Bohnhorst B, et al, for the PHELBI Study
Group. Permissive hypercapnia in extremely low birthweight infants
(PHELBI): a randomised controlled multicentre trial. Lancet Resp Med 2015;
published online June 16. http://dx.doi.org/10.1016/S22132600(15)00204-0.
12
Fernandez-Alvarez R, Gandhi RS, Amess PN, et al. Heated humidied high
ow nasal cannula versus low ow nasal cannula as weaning mode from
nasal CPAP in infants 28 weeks gestation. Eur J Pediatr 2014; 173: 9398.
Wertheim D, Olden C, Symes L, et al. Monitoring respiration in wheezy
preschool children by pulse oximetry plethysmogram analysis.
Med Biol Eng Comput 2013; 51: 96570.
Polglase GR, Dawson JA, Kluckow M, et al. Ventilation onset prior to
umbilical cord clamping (physiological-based cord clamping) improves
systemic and cerebral oxygenation in preterm lambs. PLoS One 2015;
10: e0117504.
Sweet D, Carnielli V, Greisen G, et al. European Consensus Guidelines on the
management of neonatal respiratory distress syndrome in preterm infants:
2010 Update. Neonatology 2010; 97: 40217.
The American College of Obstetricians and Gynecologists. Committee on
Obstetric Practice. Timing of umbilical cord clamping after birth.
Obstet Gynecol 2012; 120: 152226.
The National Institute for Health and Care Excellence. Intrapartum care:
care of healthy women and their babies during childbirth. December, 2014.
http://www.nice.org.uk/guidance/cg190 (accessed Feb 25, 2015).
WHO. Every Newborn: an action plan to end preventable deaths.
http://www.everynewborn.org/Documents/Full-action-plan-EN.pdf
(accessed March 10, 2015).
Ayers S, Sawyers A, During C, et al. Parents report positive experiences
about enrolling babies in a cord-related trial before birth. Acta Pediatr 2015;
104: e164e170.
Rabe H, Jewison A, Fernandez Alvarez R, et al. Milking compared with
delayed cord clamping to increase placental transfusion in preterm
neonates. A randomized controlled trial. Obstet & Gynecol 2011;
117: 20511.
Rysavy MA, Li L, Bell EF, et al. Between-hospital variation in treatment and
outcomes in extremely preterm Infants. New Engl J Med 2015;
372: 180111.
Lagatta J, Uhing M, Panepinto J. Comparative eectiveness and practice
variation in neonatal care. Clin Perinatol 2014; 41: 83345.
About 510% of patients on mechanical ventilation
will have persistent respiratory failure necessitating
prolonged mechanical ventilation.1 This condition is part
of the larger syndrome of chronic critical illness, in which
critically ill patients have continuing organ failures
leading to protracted periods of organ support.2 Both
prolonged mechanical ventilation and chronic critical
illness are important public health problems. In the
USA, for example, more than 380 000 individuals are
estimated to have chronic critical illness every year, with
costs exceeding US$50 billion annually.3
A meta-analysis of studies reporting clinical outcomes
in prolonged mechanical ventilation published in
The Lancet Respiratory Medicine further highlights the
challenges posed by these patients.4 Emily Damuth and
colleagues4 systematically reviewed 124 studies from
16 dierent countries worldwide, with sobering results.
Pooled mortality at hospital discharge was 26%, 57% of
www.thelancet.com/respiratory Vol 3 July 2015
patients were liberated from mechanical ventilation by
the end of their hospital stay, and 22% of patients were
discharged home. Perhaps most concerning was that
59% of patients were dead at 1 year.
These ndings should serve as a wake-up call to
clinicians, hospital administrators, and health policy
makers involved in the care of patients with prolonged
mechanical ventilation. Eorts are urgently needed
to increase liberation rates and improve survival.
Unfortunately, the way to proceed in this area is not
at all clear. Despite the increasing recognition of
the immense clinical and nancial burden chronic
critical illness puts on health systems, evidence-based
strategies to guide clinical care in this population
are lacking. This situation is the real wake-up call
not that outcomes must be improved, but that how
to improve them is simply not known. Immediate,
targeted research is needed to ll this knowledge gap
Jade/Blend Images/Corbis
Improving outcomes in prolonged mechanical ventilation:
a road map
Published Online
May 21, 2015
http://dx.doi.org/10.1016/
S2213-2600(15)00205-2
See Articles page 544
501
Você também pode gostar
- 1997 Inhaled Nitric Oxide in Full-Term and Nearly Full-TermDocumento8 páginas1997 Inhaled Nitric Oxide in Full-Term and Nearly Full-TermRick RoxAinda não há avaliações
- Articulos BronquiolitisDocumento18 páginasArticulos BronquiolitisLaura López Del Castillo LalydelcaAinda não há avaliações
- Evidence Support and Guidelines For Using Heated, Humidified, High-Flow Nasal Cannulae in NeonatologyDocumento13 páginasEvidence Support and Guidelines For Using Heated, Humidified, High-Flow Nasal Cannulae in NeonatologylilyAinda não há avaliações
- High Flow Oxygen Therapy V Standard Care in InfantsDocumento5 páginasHigh Flow Oxygen Therapy V Standard Care in InfantsJaque ArandaAinda não há avaliações
- Bubble CPAP Vs Ventilatory CPAPDocumento9 páginasBubble CPAP Vs Ventilatory CPAPRyan Rahman OesmanAinda não há avaliações
- Early View: A Randomised Trial of High-Flow Nasal Cannula in Infants With Moderate BronchiolitisDocumento28 páginasEarly View: A Randomised Trial of High-Flow Nasal Cannula in Infants With Moderate BronchiolitisutamiprakosoAinda não há avaliações
- HFN Literatur Rivew PDFDocumento12 páginasHFN Literatur Rivew PDFutamiprakosoAinda não há avaliações
- 2024 - Appnoeic Oxygenation During Paediatric Tracheal Intubation A Systematic Review and Meta AnalysisDocumento15 páginas2024 - Appnoeic Oxygenation During Paediatric Tracheal Intubation A Systematic Review and Meta AnalysisPamela Mamani FloresAinda não há avaliações
- S177 FullDocumento4 páginasS177 FullCalvin AffendyAinda não há avaliações
- Hemorragia PulmonarDocumento11 páginasHemorragia PulmonarFer45Ainda não há avaliações
- A Randomized Trial of High-Flow Oxygen Therapy in Infants With BronchiolitisDocumento11 páginasA Randomized Trial of High-Flow Oxygen Therapy in Infants With BronchiolitisErwin YanthoAinda não há avaliações
- Las Nebulizaciones Con Solucion Salina HipertonicaDocumento6 páginasLas Nebulizaciones Con Solucion Salina HipertonicaAlisson De Berduccy TroncosoAinda não há avaliações
- Effectiveness of Airway ClearanceDocumento7 páginasEffectiveness of Airway ClearanceNelly Lutfieta SariAinda não há avaliações
- Ajrcccm 2004Documento9 páginasAjrcccm 2004kichilla1Ainda não há avaliações
- Artigo Ana e Frederico 2021Documento10 páginasArtigo Ana e Frederico 2021CarolinaAinda não há avaliações
- Crit Care Med.: Krause@kkl200.ukl - Uni-Freiburg - de Back To TopDocumento11 páginasCrit Care Med.: Krause@kkl200.ukl - Uni-Freiburg - de Back To TopTharshini_Indr_6713Ainda não há avaliações
- Rhinopharyngeal Retrograde Clearance Induces Less Respiratory Effort and Fewer Adverse Effects in Comparison With Nasopharyngeal Aspiration in Infants With Acute Viral BronchiolitisDocumento7 páginasRhinopharyngeal Retrograde Clearance Induces Less Respiratory Effort and Fewer Adverse Effects in Comparison With Nasopharyngeal Aspiration in Infants With Acute Viral Bronchiolitismariane bezerraAinda não há avaliações
- Rclutamiento VAFO Pre Surfactante PTDocumento7 páginasRclutamiento VAFO Pre Surfactante PTGustavo Carhuamaca RoblesAinda não há avaliações
- Therapeutic Strategies For Pediatric Bronchiolitis: Expert Review of Respiratory MedicineDocumento25 páginasTherapeutic Strategies For Pediatric Bronchiolitis: Expert Review of Respiratory MedicineBastian MedinaAinda não há avaliações
- Klebsiella PDFDocumento4 páginasKlebsiella PDFOscarEduardoAinda não há avaliações
- Articulo ViernesDocumento6 páginasArticulo Viernesvelf5Ainda não há avaliações
- The Role of High-Frequency Ventilation in Neonates: Evidence-Based RecommendationsDocumento16 páginasThe Role of High-Frequency Ventilation in Neonates: Evidence-Based RecommendationsSiska LesnussaAinda não há avaliações
- Weaning Oxygen in Infants With Bronchopulmonary DysplasiaDocumento26 páginasWeaning Oxygen in Infants With Bronchopulmonary DysplasiaJHONATAN MATA ARANDAAinda não há avaliações
- AnalitikDocumento17 páginasAnalitikwecytriaAinda não há avaliações
- Bronquilitis Pdiatrics 2010Documento10 páginasBronquilitis Pdiatrics 2010thorin8Ainda não há avaliações
- Oxygen Saturation and Outcomes in Preterm InfantsDocumento17 páginasOxygen Saturation and Outcomes in Preterm InfantsSav GaAinda não há avaliações
- Oxygen Therapy and Monitoring in Newborn Infants: Editorial CommentDocumento2 páginasOxygen Therapy and Monitoring in Newborn Infants: Editorial CommentZuna QaziAinda não há avaliações
- Acute Respiratory Distress Syndrome: Children's Hospital of MichiganDocumento58 páginasAcute Respiratory Distress Syndrome: Children's Hospital of MichiganMuhammad Darwis100% (1)
- Journal Reading-Critical AppraisalDocumento28 páginasJournal Reading-Critical AppraisalHanifah RahmaniaAinda não há avaliações
- Impact of Immunoglobulin E and Airway Obstruction On BronchiectasisDocumento7 páginasImpact of Immunoglobulin E and Airway Obstruction On BronchiectasisRichie Irvanto CiandraAinda não há avaliações
- Chest Physiotherapy in Mechanically Ventilated Children A ReviewDocumento10 páginasChest Physiotherapy in Mechanically Ventilated Children A Reviewmrizki_1Ainda não há avaliações
- Management and Treatment Guidelines For Sepsis in Pediatric PatientsDocumento9 páginasManagement and Treatment Guidelines For Sepsis in Pediatric PatientsIhsan PutraAinda não há avaliações
- Pediatrics 2013 Kapadia E1488 96Documento11 páginasPediatrics 2013 Kapadia E1488 96M Aprial DarmawanAinda não há avaliações
- Accepted Manuscript: Paediatric Respiratory ReviewsDocumento16 páginasAccepted Manuscript: Paediatric Respiratory ReviewsAlvaro Guillen CerpaAinda não há avaliações
- Epinephrine and Dexamethasone in Children With BronchiolitisDocumento11 páginasEpinephrine and Dexamethasone in Children With BronchiolitisAdelina Wahyuni LubisAinda não há avaliações
- Annotated-J Siny 2019 101070Documento7 páginasAnnotated-J Siny 2019 101070Andre Faustino QuispeAinda não há avaliações
- The Use of Sildenafil in Persistent Pulmonary Hypertension of The Newborn PDFDocumento6 páginasThe Use of Sildenafil in Persistent Pulmonary Hypertension of The Newborn PDFmaciasdrAinda não há avaliações
- Acuterespiratorydistress Syndrome: Ventilator Management and Rescue TherapiesDocumento16 páginasAcuterespiratorydistress Syndrome: Ventilator Management and Rescue TherapiessamuelAinda não há avaliações
- Fluid Management in Association With Neonatal SurgeryDocumento3 páginasFluid Management in Association With Neonatal SurgeryGunduz AgaAinda não há avaliações
- 10 1016@j Ijporl 2020 110139Documento28 páginas10 1016@j Ijporl 2020 110139Gregoria choque floresAinda não há avaliações
- Shukla 2019Documento17 páginasShukla 2019Stheffany Allison Maldonado BravoAinda não há avaliações
- Lung Protective Mechanical Ventilation StrategiesDocumento4 páginasLung Protective Mechanical Ventilation StrategiesAnne Julia AgustinAinda não há avaliações
- CHEST Nov 2005Documento183 páginasCHEST Nov 2005rizjkuramaAinda não há avaliações
- The Efficacy of Nebulized Salbutamol, Magnesium Sulfate, and Salbutamol/magnesium Sulfate Combination in Moderate BronchiolitisDocumento4 páginasThe Efficacy of Nebulized Salbutamol, Magnesium Sulfate, and Salbutamol/magnesium Sulfate Combination in Moderate BronchiolitisgraciaAinda não há avaliações
- Pediatrics 2014 Polin 156 63 PDFDocumento11 páginasPediatrics 2014 Polin 156 63 PDFdediraihanAinda não há avaliações
- Case PresentationDocumento34 páginasCase PresentationPhilbert Russell Del ValleAinda não há avaliações
- VM PediatrikDocumento13 páginasVM PediatrikWayan SupiartaAinda não há avaliações
- Solucion A en BronquiolitisDocumento6 páginasSolucion A en BronquiolitisLuis Sanchez CarranzaAinda não há avaliações
- HT PedDocumento18 páginasHT PedLina María CañónAinda não há avaliações
- 2211-Article Text-8778-10260-10-20230620Documento8 páginas2211-Article Text-8778-10260-10-20230620IdmAinda não há avaliações
- IJP Volume 6 Issue 11 Pages 8507-8516Documento10 páginasIJP Volume 6 Issue 11 Pages 8507-8516Marda LinaAinda não há avaliações
- Original: DOI 10.1007/s00134-016-4617-8Documento8 páginasOriginal: DOI 10.1007/s00134-016-4617-8qvc.regulatory 2Ainda não há avaliações
- Postnatal Hydrocortisone For Preventing or Treating Bronchopulmonary Dysplasia in Preterm Infants: A Systematic ReviewDocumento7 páginasPostnatal Hydrocortisone For Preventing or Treating Bronchopulmonary Dysplasia in Preterm Infants: A Systematic ReviewAldy RinaldiAinda não há avaliações
- Clinical StudyDocumento7 páginasClinical StudyJonathan MarkAinda não há avaliações
- Journal ReadingDocumento5 páginasJournal ReadingRoma WestAinda não há avaliações
- Ppul 24811Documento5 páginasPpul 24811rizki romadaniAinda não há avaliações
- Clinical Study of Bronchial Asthma in Children Aged 5 To 12 Years With Special Reference To Peak Expiratory Flow RateDocumento6 páginasClinical Study of Bronchial Asthma in Children Aged 5 To 12 Years With Special Reference To Peak Expiratory Flow Rateturky hadiAinda não há avaliações
- Recommendation 1ADocumento26 páginasRecommendation 1Asyahrizon thomasAinda não há avaliações
- Inhaled Hypertonic Saline Safe, Effective in Infants With CFDocumento3 páginasInhaled Hypertonic Saline Safe, Effective in Infants With CFnaxo128Ainda não há avaliações
- Infection and Tumorigenesis of Biomaterials by Smit Prajapati-200280103028 and Yukta Dodia - 200280103052Documento18 páginasInfection and Tumorigenesis of Biomaterials by Smit Prajapati-200280103028 and Yukta Dodia - 200280103052Yukta DodiaAinda não há avaliações
- Dr. Adarsh Chandra Swami - Anaesthesia Doctor in Mohali - Fortis HealthcareDocumento1 páginaDr. Adarsh Chandra Swami - Anaesthesia Doctor in Mohali - Fortis Healthcarej01scottAinda não há avaliações
- Oxford GastroenterologyDocumento673 páginasOxford Gastroenterologymymamym100% (1)
- सञ्चयकर्ता स्वास्थ्योपचार योजना सञ्चालन कार्यविधि, २०७७-50e1Documento13 páginasसञ्चयकर्ता स्वास्थ्योपचार योजना सञ्चालन कार्यविधि, २०७७-50e1crystalconsultancy22Ainda não há avaliações
- Brochure Biology & Medicine 03 2022 - CompressedDocumento40 páginasBrochure Biology & Medicine 03 2022 - CompressedMerida Bertrand Alex PodgaAinda não há avaliações
- Northwestern Lifestyle Medicine QuestionnaireDocumento9 páginasNorthwestern Lifestyle Medicine QuestionnaireAndrew HuaAinda não há avaliações
- Vision Ans MissionDocumento11 páginasVision Ans MissionValarmathiAinda não há avaliações
- MEdication ErrorsDocumento6 páginasMEdication ErrorsBeaCeeAinda não há avaliações
- Mrs. Manisha Chichani 29032023 064453 PMDocumento1 páginaMrs. Manisha Chichani 29032023 064453 PMManisha ChichaniAinda não há avaliações
- Gwen Watego (New)Documento3 páginasGwen Watego (New)Duan Tian0% (1)
- Nicaragua Reflection PaperDocumento3 páginasNicaragua Reflection Paperapi-487254609Ainda não há avaliações
- Legal Medicine: Legal Medicine (2011) Antonio Rebosa, LL.B, M.DDocumento6 páginasLegal Medicine: Legal Medicine (2011) Antonio Rebosa, LL.B, M.DarciblueAinda não há avaliações
- Dip HIV Man (SA) Regulations 24-1-2017Documento9 páginasDip HIV Man (SA) Regulations 24-1-2017matentenAinda não há avaliações
- 01 - Pharmacotherapy Pearls For Emergency Neurological Life Support PDFDocumento26 páginas01 - Pharmacotherapy Pearls For Emergency Neurological Life Support PDFawinsyAinda não há avaliações
- Is It Okay To Drink Alcohol On Steroids - Google SearchDocumento1 páginaIs It Okay To Drink Alcohol On Steroids - Google SearchEsin SyurmeliAinda não há avaliações
- Perioperative Hemodynamic MonitoringDocumento9 páginasPerioperative Hemodynamic MonitoringjayezmenonAinda não há avaliações
- Medical Intensive Care UnitDocumento120 páginasMedical Intensive Care Unithaaronminalang100% (6)
- Health Education For Patients With Urinary CathetersDocumento2 páginasHealth Education For Patients With Urinary CathetersTriXie SorrillaAinda não há avaliações
- Tumors of The Orbit by Dr. Jonathan Del Prado 082708Documento3 páginasTumors of The Orbit by Dr. Jonathan Del Prado 082708CitrusAinda não há avaliações
- Jimma University: Institute of Health Faculty of Health Science School of PharmacyDocumento69 páginasJimma University: Institute of Health Faculty of Health Science School of PharmacyMaህAinda não há avaliações
- A Guide To Clinical Case Study and Its PresentationDocumento13 páginasA Guide To Clinical Case Study and Its PresentationVince Troy AquinoAinda não há avaliações
- Linhart Continuing Dental Education ProgramDocumento2 páginasLinhart Continuing Dental Education ProgramnallatmAinda não há avaliações
- Four Big Pollution Diseases of Japan - Wikipedia, The Free Encyclopedia PDFDocumento6 páginasFour Big Pollution Diseases of Japan - Wikipedia, The Free Encyclopedia PDFudayngAinda não há avaliações
- Nutrition Month 2011: Isulong Ang Breastfeeding - Tama, Sapat at Eksklusibo! (Tsek) ProgramDocumento22 páginasNutrition Month 2011: Isulong Ang Breastfeeding - Tama, Sapat at Eksklusibo! (Tsek) Programセル ZhelAinda não há avaliações
- Primary Lesion: Abdul Rashid Bin Tharek Group 90Documento27 páginasPrimary Lesion: Abdul Rashid Bin Tharek Group 90rashidAinda não há avaliações
- NEET-SS UrologyDocumento59 páginasNEET-SS Urologyadi100% (1)
- Kudori Therapy - Updated 9th Dec17Documento32 páginasKudori Therapy - Updated 9th Dec17Manickavasagam RengarajuAinda não há avaliações
- CHF NCPDocumento8 páginasCHF NCPZy Hallasgo100% (1)
- Konsensus IBDDocumento15 páginasKonsensus IBDTaufikAinda não há avaliações
- Determinants of HealthDocumento29 páginasDeterminants of HealthMayom Mabuong92% (12)
- The Age of Magical Overthinking: Notes on Modern IrrationalityNo EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityNota: 4 de 5 estrelas4/5 (24)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNo EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNota: 4.5 de 5 estrelas4.5/5 (42)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsAinda não há avaliações
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNo EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNota: 5 de 5 estrelas5/5 (80)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNo EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNota: 5 de 5 estrelas5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNo EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNota: 4.5 de 5 estrelas4.5/5 (266)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNota: 2 de 5 estrelas2/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossNo EverandThe Obesity Code: Unlocking the Secrets of Weight LossNota: 4 de 5 estrelas4/5 (5)
- Why We Die: The New Science of Aging and the Quest for ImmortalityNo EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityNota: 4 de 5 estrelas4/5 (3)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningNo EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningNota: 4 de 5 estrelas4/5 (3)
- Gut: the new and revised Sunday Times bestsellerNo EverandGut: the new and revised Sunday Times bestsellerNota: 4 de 5 estrelas4/5 (392)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.No EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Nota: 4.5 de 5 estrelas4.5/5 (110)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNo EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNota: 3.5 de 5 estrelas3.5/5 (3)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNo EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNota: 5 de 5 estrelas5/5 (1)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisNo EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisNota: 3.5 de 5 estrelas3.5/5 (2)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsNo EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsNota: 4.5 de 5 estrelas4.5/5 (169)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessNo EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessNota: 4.5 de 5 estrelas4.5/5 (328)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisNo EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisNota: 4 de 5 estrelas4/5 (1)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisNo EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisNota: 4 de 5 estrelas4/5 (9)
- 12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosNo Everand12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosNota: 4.5 de 5 estrelas4.5/5 (207)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryNo EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryNota: 4 de 5 estrelas4/5 (44)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeNo EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeNota: 4.5 de 5 estrelas4.5/5 (253)