Escolar Documentos
Profissional Documentos
Cultura Documentos
Im History and Pe Format
Enviado por
Remelou Garchitorena AlfelorDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Im History and Pe Format
Enviado por
Remelou Garchitorena AlfelorDireitos autorais:
Formatos disponíveis
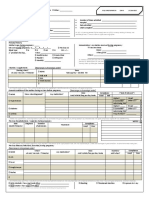
Internal Medicine History and Physical
Page 1 of 2
Chief Complaint: ____________________________________________________
Date: ________________
Time: ________________
History of Present Illness:_____________________________________________________________________
___________________________________________________________________________________________
___________________________________________________________________________________________
___________________________________________________________________________________________
___________________________________________________________________________________________
___________________________________________________________________________________________
___________________________________________________________________________________________
___________________________________________________________________________________________
Review of Systems:
General: fatigue
weight loss
fever
chills
night sweats
Eyes: visual change
pain
redness
ENT: headaches
hoarseness
sore throat
epistaxis
sinus symptoms
hearing loss
tinnitus
yes
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ] Unobtainable due to __________________________________
no
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
CV: chest pain
edema
PND
orthopnea
palpitations
claudication
Resp: cough
SOB
wheezing
hypersomnolence
GI: abdominal pain
stool changes
nausea/vomiting
diarrhea
heartburn
blood in stool
yes
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
no
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
GU: dysuria
frequency
hematuria
discharge
menstrual problems
Musc-skel: arthralgia
arthritis
joint swelling
myalgias
backpain
Heme/Lymph: bleeding
brusing
clotting
transfusions
lymph node swelling
yes
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
no
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
Endo: polyuria
polydypsia
polyphagia
heat/cold intolerance
Derm: rash
pruritis
Neuro: weakness
seizures
paresthesias
tremor
syncope
Psych: anxiety
depression
hallucinations
All/Imm: hayfever
bee sting allergy
Other ROS: ___________________________________________
[ ] All other ROS reviewed and were NORMAL.
Past Medical History:_________________________
__________________________________________
__________________________________________
__________________________________________
__________________________________________
__________________________________________
__________________________________________
__________________________________________
__________________________________________
Allergies:
Past Surgical History: ______________________
__________________________________________
__________________________________________
Family History: ____________________________
__________________________________________
__________________________________________
Social History: _____________________________
__________________________________________
Cigs [ ] No [ ] Yes Pack-yrs: _________________
EtOH [ ] No [ ] Yes Amount: __________________
Illicits [ ] No [ ] Yes Type: ____________________
Regional Medical Center at Memphis
INTERNAL MEDICINE HISTORY & PHYSICAL
PAGE 1 of 2
FORM NO. 6024.013 (Rev. 11/05)
[ ] NKDA
yes
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
no
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
[ ]
Other: ____________________
Medications: ______________________________
__________________________________________
__________________________________________
__________________________________________
__________________________________________
__________________________________________
__________________________________________
__________________________________________
__________________________________________
__________________________________________
__________________________________________
__________________________________________
__________________________________________
__________________________________________
__________________________________________
__________________________________________
__________________________________________
__________________________________________
__________________________________________
__________________________________________
__________________________________________
Addressograph/Patient ID
Internal Medicine History and Physical
Physical Exam
T _______
RR _______ BP___________ HR _______ Wt _______ (lbs) Ht _______ (in)
Page 2 of 2
BMI _______
O2 Sat _______ on _______
Eyes
[ ] nl conjunctiva & lids
ENT External
[ ] no scars, lesions, masses
Neck External [ ] no tracheal deviation
Pupils
[ ] equal, round, & reactive
Otoscopic
[ ] nl canals, tympanic membranes
Palpation
[ ] no masses or crepitus
Fundus
[ ] nl discs & vessels
Hearing
[ ] nl to finger rub
Thyroid
[ ] no megaly or tenderness
Vision
[ ] acuity & gross fields intact
Oropharynx
[ ] nl teeth, tongue, palate, pharynx
Abnormals:
Abnormals:
GI
Abnormals:
Palpation
[ ] no masses or tenderness
Resp
Skin
[ ] no rashes, lesions, ulcers
[ ] no hep/splenomegaly
Effort
[ ] nl without retractions
Auscultation
[ ] nl bowel sounds
Percussion
[ ] no dullness or hyperresonance
Chest/Breast
[ ] nl inspection & palpation
Percussion
[ ] no shifting dullness
Palpation
[ ] no fremitus
Lymph nodes
[ ] no axillary, inguinal, cervical,
Anus/rectum
[ ] no abnormality or masses
Auscultation
[ ] CTAB w/o W, R, or R
Genitourinary
[ ] nl external genitalia
[ ] heme negative stool
[ ] nl turgor
or submandibular LAD
Abnormals:
Abnormals:
[ ] nl vaginal tone, mucosa
[ ] no cervical motion tenderness
CV Palpation
[ ] PMI nondisplaced
Neuro
Auscultation
[ ] no murmur, gallop, or rub
Orientation
[ ] A&O to person, place, time
Carotids
[ ] nl intensity w/o bruit
Cranial nerves
[ ] CN II-XII intact
JVD
[ ] no jugulovenous distension
Sensory
[ ] nl sensation throughout
Pulses
[ ] 2+/= femoral & pedal pulses
Reflexes
[ ] 2+ + and symmetrical throughout
Edema
[ ] no pedal edema
Abnormals:
[ ] nl prostate size and texture
Psych
[ ] nl cognition
[ ] MMSE ___________
[ ] nl mood and affect
Abnormals:
Abnormals:
Musculoskeletal
Gait
[ ] nl penis & scrotal contents
Inspection
ROM
Strength
Upper extrem
[ ]
[ ]
[ ]
Tone ( if normal)
[ ]
Lower extrem
[ ]
[ ]
[ ]
[ ]
Abnormals:
Other:
[ ] no apparent distress
[ ] nl gait and station
X-ray:
EKG:
Other:
Assessment & Plan: _______________________________________________________________________________
_________________________________________________________________________________________________
_________________________________________________________________________________________________
_________________________________________________________________________________________________
_________________________________________________________________________________________________
_________________________________________________________________________________________________
_________________________________________________________________________________________________
_________________________________________________________________________________________________
_________________________________________________________________________________________________
Signature: _________________________________
Attending MD
[ ] Ive examined the patient.
Date: _____________________________________
[ ] Ive reviewed with housestaff and agree with the above.
Signature ____________________________ Date: ____________
Regional Medical Center at Memphis
INTERNAL MEDICINE HISTORY & PHYSICAL
PAGE 2 of 2
FORM NO. 6024.013 (Rev. 11/05)
Addressograph/Patient ID
Você também pode gostar
- PLE Reviewer Pathology Inflammation and RepairDocumento15 páginasPLE Reviewer Pathology Inflammation and RepairRemelou Garchitorena AlfelorAinda não há avaliações
- PLE Reviewer Pathology Inflammation and RepairDocumento15 páginasPLE Reviewer Pathology Inflammation and RepairRemelou Garchitorena AlfelorAinda não há avaliações
- Acute Medicine: Shock: Inadequate Tissue and Organ PerfusionDocumento3 páginasAcute Medicine: Shock: Inadequate Tissue and Organ Perfusionmyat252Ainda não há avaliações
- Pharmacology Table - GonzalesDocumento14 páginasPharmacology Table - GonzalesMark Angelo PonferradoAinda não há avaliações
- Spinal CordDocumento7 páginasSpinal CordRemelou Garchitorena AlfelorAinda não há avaliações
- MED2 5.02 Oncologic Emergencies - Dr. F. AdefuinDocumento5 páginasMED2 5.02 Oncologic Emergencies - Dr. F. AdefuinAra DiocosAinda não há avaliações
- Final Coaching 2023Documento3 páginasFinal Coaching 2023Parasaubang ButangAinda não há avaliações
- Midface Clinical Anatomy and Regional Approaches.31Documento17 páginasMidface Clinical Anatomy and Regional Approaches.31Andreas Chandra100% (3)
- PLE Review OBGYN Chap 1 Overview of ObstetricsDocumento2 páginasPLE Review OBGYN Chap 1 Overview of ObstetricsRemelou Garchitorena Alfelor100% (1)
- Trans-Out Orders: NSVD Admitting Notes Postpartum OrdersDocumento7 páginasTrans-Out Orders: NSVD Admitting Notes Postpartum OrdersDre ValdezAinda não há avaliações
- FAST ExamDocumento123 páginasFAST ExamSinisa Ristic50% (2)
- New Intern Guide Quick NotesDocumento8 páginasNew Intern Guide Quick NotesTrisAinda não há avaliações
- Obstetric FormDocumento4 páginasObstetric FormKhylamarie VillalunaAinda não há avaliações
- Pedia CardDocumento4 páginasPedia CardPatricia Kate RegalaAinda não há avaliações
- (Warding) Guideline 1 - QCGH-HISTORY - PE - GUIDELINEDocumento4 páginas(Warding) Guideline 1 - QCGH-HISTORY - PE - GUIDELINEHynne Jhea Echavez100% (1)
- Topnotch ENT Supplement Handout - UPDATED April 2017Documento15 páginasTopnotch ENT Supplement Handout - UPDATED April 2017Andrassy Twinkle AlineaAinda não há avaliações
- JI Chart OrdersDocumento4 páginasJI Chart OrdersMel BillonesAinda não há avaliações
- PLE Pathology Cell Injury, Cell Death, and AdaptationsDocumento10 páginasPLE Pathology Cell Injury, Cell Death, and AdaptationsRemelou Garchitorena AlfelorAinda não há avaliações
- Simplified Diagnostic Approach in Acute HepatitisDocumento2 páginasSimplified Diagnostic Approach in Acute HepatitisJohn Christopher LucesAinda não há avaliações
- Moonlighting GuideDocumento14 páginasMoonlighting GuideJulienneAinda não há avaliações
- The "Most Common" . According To NelsonDocumento31 páginasThe "Most Common" . According To NelsonKenneth NuñezAinda não há avaliações
- Internal MedicineDocumento83 páginasInternal MedicineSumbul PAinda não há avaliações
- OB Williams Chap 2 Maternal AnatomyDocumento7 páginasOB Williams Chap 2 Maternal AnatomyRem Alfelor0% (1)
- Diagnosing Anemia in Neonates An Evidence-Based ApproachDocumento13 páginasDiagnosing Anemia in Neonates An Evidence-Based Approacharmando salvador100% (1)
- Pedia Bacte Table 08amDocumento25 páginasPedia Bacte Table 08ampedia blue bookAinda não há avaliações
- 2 0CommDiseaseIMPTVisionDocumento3 páginas2 0CommDiseaseIMPTVisionAndrea Patricia DaquialAinda não há avaliações
- Legal Medicine and Medical Jurisprudence Comprehensive Exam ReviewerDocumento17 páginasLegal Medicine and Medical Jurisprudence Comprehensive Exam ReviewerYeshua Tura100% (1)
- Pedia - CNS Infection, Seizures, NMD (Agrava)Documento30 páginasPedia - CNS Infection, Seizures, NMD (Agrava)Ivy Grace LimAinda não há avaliações
- Topnotch Waiver Oath and Checklist April 2015 PDFDocumento2 páginasTopnotch Waiver Oath and Checklist April 2015 PDFRalph JuicoAinda não há avaliações
- OB Williams Chap 2 Maternal PhysiologyDocumento9 páginasOB Williams Chap 2 Maternal PhysiologyRem Alfelor100% (2)
- Pediatrics:: History Taking and Physical Examination of AdolescentsDocumento14 páginasPediatrics:: History Taking and Physical Examination of AdolescentsJüdith Marie Reyes BauntoAinda não há avaliações
- Pedia TicklersDocumento24 páginasPedia Ticklersjoshua espirituAinda não há avaliações
- General Surgery Tubes and DrainsDocumento4 páginasGeneral Surgery Tubes and DrainsLorenzoVasquezDatul100% (3)
- BRAIN AND SPINAL CORD TUMORS Table PDFDocumento4 páginasBRAIN AND SPINAL CORD TUMORS Table PDFRemelou Garchitorena Alfelor100% (1)
- Problem-based Approach to Gastroenterology and HepatologyNo EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisAinda não há avaliações
- GynexDocumento73 páginasGynexDominque RabastoAinda não há avaliações
- OB-GYN Patient History and PEDocumento4 páginasOB-GYN Patient History and PEAngelique TongsonAinda não há avaliações
- Prostho MCQDocumento10 páginasProstho MCQPrateek Mishra50% (8)
- Chapter 2 Maternal AnatomyDocumento9 páginasChapter 2 Maternal AnatomyRemelou Garchitorena Alfelor100% (1)
- 107 Rle Virtual Duty - Opd: Internal MedicineDocumento6 páginas107 Rle Virtual Duty - Opd: Internal MedicineGiel Margareth LindoAinda não há avaliações
- Ectopic Pregnancy William 24thDocumento44 páginasEctopic Pregnancy William 24th林昌恩Ainda não há avaliações
- SBAR ExampleDocumento13 páginasSBAR Examplejugdeep15Ainda não há avaliações
- ASADocumento3 páginasASAMelisa Malik50% (2)
- Basic Investigation of An Infertile CoupleDocumento53 páginasBasic Investigation of An Infertile CoupleRemelou Garchitorena AlfelorAinda não há avaliações
- 24 HR History 2Documento2 páginas24 HR History 2Arjun KatariaAinda não há avaliações
- Medicine OSCE - Common Diseases Ver2Documento4 páginasMedicine OSCE - Common Diseases Ver2TrisAinda não há avaliações
- Sulcus Vocalis Our Experience-DikonversiDocumento5 páginasSulcus Vocalis Our Experience-DikonversiNuni SukindarAinda não há avaliações
- Intestinal Obstruction in Pediatric PatientsDocumento25 páginasIntestinal Obstruction in Pediatric PatientsHaryo Priambodo100% (1)
- His Perfect Wife Susanne MccarthyDocumento113 páginasHis Perfect Wife Susanne Mccarthymenaal5489% (38)
- IM Cardiology Samplex All-In - LDocumento35 páginasIM Cardiology Samplex All-In - LDeepbluexAinda não há avaliações
- Minor Disorders of Newborn and Its ManagementDocumento3 páginasMinor Disorders of Newborn and Its Managementarun26198891% (11)
- 10 Medicinal Plants Approved by The DOHDocumento4 páginas10 Medicinal Plants Approved by The DOHAlyssa Jane Gaitan LauAinda não há avaliações
- Chronic Kidney Disease in PregnancyDocumento64 páginasChronic Kidney Disease in PregnancyRemelou Garchitorena AlfelorAinda não há avaliações
- Pathophysiology of AgingDocumento5 páginasPathophysiology of AgingRemelou Garchitorena AlfelorAinda não há avaliações
- History Physical FormatDocumento3 páginasHistory Physical FormatfilchibuffAinda não há avaliações
- Core Values of Family MedicineDocumento68 páginasCore Values of Family MedicineJodene Rose RojasAinda não há avaliações
- Correlative AnatomyDocumento19 páginasCorrelative AnatomyLicensed to HealAinda não há avaliações
- Ent OpdDocumento5 páginasEnt OpdRenz Marion AlemaniaAinda não há avaliações
- B - Embyrology HomologuesDocumento1 páginaB - Embyrology HomologuesS ParekhAinda não há avaliações
- Antepartum HemorrhageDocumento18 páginasAntepartum HemorrhageSanaAinda não há avaliações
- Universidad de Manila College of Nursing Community Health Survey ToolDocumento9 páginasUniversidad de Manila College of Nursing Community Health Survey Toolaina_boydonAinda não há avaliações
- PEDIA para 08AMDocumento17 páginasPEDIA para 08AMpedia blue bookAinda não há avaliações
- Small Group DiscussionDocumento3 páginasSmall Group DiscussionBea SamonteAinda não há avaliações
- CC C C: June 8, 2011 By: Santos, Edilberto DBDocumento63 páginasCC C C: June 8, 2011 By: Santos, Edilberto DBHakugeiAinda não há avaliações
- Case Presentation: NeurologyDocumento19 páginasCase Presentation: NeurologySydrex SarmientoAinda não há avaliações
- Ob-Gyn Review Part 3Documento101 páginasOb-Gyn Review Part 3filchibuffAinda não há avaliações
- Pediatric History TemplateDocumento3 páginasPediatric History TemplateJoel TamayoAinda não há avaliações
- Rabies Lay ForumDocumento40 páginasRabies Lay ForumCarlos H. AcuñaAinda não há avaliações
- TOPNOTCH Diagnostic Exam ANSWER KEY September 2018Documento20 páginasTOPNOTCH Diagnostic Exam ANSWER KEY September 2018CDAinda não há avaliações
- CPG DyslipidemiaDocumento26 páginasCPG DyslipidemiaRenzy SalumbreAinda não há avaliações
- OCHA PH - Measles OutbreakDocumento1 páginaOCHA PH - Measles OutbreakPhilippe Ceasar C. BascoAinda não há avaliações
- Shock: Rose Ann J. Raquiza-Perante Post Graduate InternDocumento53 páginasShock: Rose Ann J. Raquiza-Perante Post Graduate InternRose Ann RaquizaAinda não há avaliações
- OPD Adolescent History FormDocumento5 páginasOPD Adolescent History FormNehemiah FranciscoAinda não há avaliações
- LDTDocumento6 páginasLDTRaian SuyuAinda não há avaliações
- Bronchial Asthma: West Visayas State University Medical Center - Department of PediatricsDocumento9 páginasBronchial Asthma: West Visayas State University Medical Center - Department of PediatricsPGI Miayo, StephenAinda não há avaliações
- MicrobiologyDocumento169 páginasMicrobiologyAnnaAinda não há avaliações
- Lecture 1 - General Properties and Classification of FungiDocumento4 páginasLecture 1 - General Properties and Classification of FungiRemelou Garchitorena AlfelorAinda não há avaliações
- EBM Workshop - Chondroitin Sulfate On OsteoarthritisDocumento55 páginasEBM Workshop - Chondroitin Sulfate On OsteoarthritisFAMED RESIDENTS CESMEDAinda não há avaliações
- March 2022 Hybrid Full Course OFFICIAL Lecture Schedule - NOV-DEC UPLOADDocumento3 páginasMarch 2022 Hybrid Full Course OFFICIAL Lecture Schedule - NOV-DEC UPLOADJhon PauloAinda não há avaliações
- Chapter 727: Table 727-3 Abbreviations For Specimens inDocumento9 páginasChapter 727: Table 727-3 Abbreviations For Specimens inGab ByAinda não há avaliações
- Pediatric Tickler by RemDocumento7 páginasPediatric Tickler by RemRem AlfelorAinda não há avaliações
- History Examination of Gynecology and Obstetrics PatientsDocumento3 páginasHistory Examination of Gynecology and Obstetrics PatientsAgus WijayaAinda não há avaliações
- CASE REPORT ON Bilateral Ectopic PregnancyDocumento29 páginasCASE REPORT ON Bilateral Ectopic PregnancyRemelou Garchitorena AlfelorAinda não há avaliações
- Chapter 3 Congenital Genitourinary AbnormalitiesDocumento4 páginasChapter 3 Congenital Genitourinary AbnormalitiesRemelou Garchitorena AlfelorAinda não há avaliações
- Chap 8 Prenatal CareDocumento9 páginasChap 8 Prenatal CareRemelou Garchitorena AlfelorAinda não há avaliações
- Eclampsia in Pediatric PatientDocumento50 páginasEclampsia in Pediatric PatientRemelou Garchitorena AlfelorAinda não há avaliações
- The MediastinumDocumento61 páginasThe MediastinumRemelou Garchitorena AlfelorAinda não há avaliações
- Trans Congenital MalformationsDocumento10 páginasTrans Congenital MalformationsRemelou Garchitorena AlfelorAinda não há avaliações
- Headacheseizures Drterencio TRANSDocumento7 páginasHeadacheseizures Drterencio TRANSRemelou Garchitorena AlfelorAinda não há avaliações
- Hydrocephalus and Anomalies of The CNSDocumento26 páginasHydrocephalus and Anomalies of The CNSRemelou Garchitorena AlfelorAinda não há avaliações
- Traumatic Brain Injury: Almario G. Jabson MD Section of Neurosurgery Asian Hospital and Medical CenterDocumento38 páginasTraumatic Brain Injury: Almario G. Jabson MD Section of Neurosurgery Asian Hospital and Medical CenterRemelou Garchitorena AlfelorAinda não há avaliações
- Brain TumorsDocumento21 páginasBrain TumorsRemelou Garchitorena AlfelorAinda não há avaliações
- Eac HemaDocumento150 páginasEac HemaRemelou Garchitorena AlfelorAinda não há avaliações
- Childhood Stroke TransDocumento9 páginasChildhood Stroke TransRemelou Garchitorena AlfelorAinda não há avaliações
- Anemia, Bleeding, ThrombosisDocumento40 páginasAnemia, Bleeding, ThrombosisRemelou Garchitorena AlfelorAinda não há avaliações
- RM Name RM Name RM Name RM Name RM Name: Rem AlfelorDocumento1 páginaRM Name RM Name RM Name RM Name RM Name: Rem AlfelorRemelou Garchitorena AlfelorAinda não há avaliações
- PartogramDocumento31 páginasPartogramRemelou Garchitorena AlfelorAinda não há avaliações
- Name:: Admitting Diagnosis: Live BabyDocumento2 páginasName:: Admitting Diagnosis: Live BabyRemelou Garchitorena AlfelorAinda não há avaliações
- History and Pe Sheet ExcelDocumento12 páginasHistory and Pe Sheet ExcelRemelou Garchitorena AlfelorAinda não há avaliações
- Clerk - S CensusDocumento2 páginasClerk - S CensusRemelou Garchitorena AlfelorAinda não há avaliações
- Iron Deficiency Anemia Among Pregnant Women in Nablus District Prevalence Knowledge Attitude and Practices PDFDocumento72 páginasIron Deficiency Anemia Among Pregnant Women in Nablus District Prevalence Knowledge Attitude and Practices PDFEArl CopinaAinda não há avaliações
- 0702055522Documento577 páginas0702055522mophcvaduth1Ainda não há avaliações
- Seizures in The Preterm NeonateDocumento10 páginasSeizures in The Preterm NeonateRoosevelt Santibañez Dla TorreAinda não há avaliações
- Flyer SugiesDocumento2 páginasFlyer SugiesInomy ClaudiaAinda não há avaliações
- Surgical Site Marking Protocols and PolicyDocumento8 páginasSurgical Site Marking Protocols and PolicyashovAinda não há avaliações
- Anatomy and Pa Tho Physiology of Aqueous Production and OutflowDocumento34 páginasAnatomy and Pa Tho Physiology of Aqueous Production and OutflowChristine TanAinda não há avaliações
- Nephrolithiasis AnatomyDocumento3 páginasNephrolithiasis AnatomyKevin Ker Campaner MerillesAinda não há avaliações
- Pharmacology Iii PracticalDocumento16 páginasPharmacology Iii Practicaldoremon nobitaAinda não há avaliações
- Management of Side Effects and Complication in Medical AbortionDocumento10 páginasManagement of Side Effects and Complication in Medical AbortionmariaAinda não há avaliações
- Pedia Form Sample (Alpha)Documento3 páginasPedia Form Sample (Alpha)Rj PolvorosaAinda não há avaliações
- Esophageal Perforation: Diagnostic Work-Up and Clinical Decision-Making in The First 24 HoursDocumento7 páginasEsophageal Perforation: Diagnostic Work-Up and Clinical Decision-Making in The First 24 HourssyaifularisAinda não há avaliações
- Latihan Soal MCQ UrologiDocumento43 páginasLatihan Soal MCQ Urologidytul100% (1)
- DR AgarwalDocumento3 páginasDR AgarwalYv SantoshAinda não há avaliações
- Jurnal Internasional PDFDocumento7 páginasJurnal Internasional PDFShella GustiawatiAinda não há avaliações
- Echs EmpanelmentDocumento316 páginasEchs EmpanelmentYudhvir SawhneyAinda não há avaliações
- ETC1010 Paper 1Documento9 páginasETC1010 Paper 1wjia26Ainda não há avaliações
- DR FormsDocumento3 páginasDR FormsDianne LabisAinda não há avaliações
- Masaki - The Role of Percutaneous Nephrostomy in The Management of Obstructive Uropathy Secondary To Pelvic Malignancies at Kenyatta National HospitalDocumento48 páginasMasaki - The Role of Percutaneous Nephrostomy in The Management of Obstructive Uropathy Secondary To Pelvic Malignancies at Kenyatta National HospitalAji PatriajatiAinda não há avaliações
- Guidelines - Care of A Child Requiring Long Term VentilationDocumento30 páginasGuidelines - Care of A Child Requiring Long Term VentilationgopscharanAinda não há avaliações