Escolar Documentos
Profissional Documentos
Cultura Documentos
Discapacidad Intelectual DSM
Enviado por
Pamela HernandezDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Discapacidad Intelectual DSM
Enviado por
Pamela HernandezDireitos autorais:
Formatos disponíveis
INTELLECTUAL AND DEVELOPMENTAL DISABILITIES
AAIDD
2014, Vol. 52, No. 3, 165174
DOI: 10.1352/1934-9556-52.3.165
To ID or Not to ID? Changes in Classification Rates of
Intellectual Disability Using DSM-5
Aimilia Papazoglou, Lisa A. Jacobson, Marie McCabe, Walter Kaufmann, and T. Andrew Zabel
Abstract
The Diagnostic and Statistical Manual of Mental DisordersFifth Edition (DSM-5) diagnostic criteria
for intellectual disability (ID) include a change to the definition of adaptive impairment. New
criteria require impairment in one adaptive domain rather than two or more skill areas. The authors
examined the diagnostic implications of using a popular adaptive skill inventory, the Adaptive
Behavior Assessment SystemSecond Edition, with 884 clinically referred children (ages 616).
One hundred sixty-six children met DSM-IV-TR criteria for ID; significantly fewer (n 5 151,
p 5 .001) met ID criteria under DSM-5 (9% decrease). Implementation of DSM-5 criteria for ID
may substantively change the rate of ID diagnosis. These findings highlight the need for a
combination of psychometric assessment and clinical judgment when implementing the adaptive
deficits component of the DSM-5 criteria for ID diagnosis.
Key Words: adaptive functioning; intellectual disability; mental retardation; DSM-IV; prevalence
The diagnosis of intellectual disability (ID; formerly
known as mental retardation) is characterized by
concurrent deficits in intellectual and adaptive
functioning, with onset prior to adulthood. Prevalence rates for ID are generally estimated to be 1% of
the population, with higher rates in middle and lowincome countries (Maulik, Mascarenhas, Mathers,
Dua, & Saxena, 2011). In the United States, this
amounts to approximately 3 million people (Larson
et al., 2001), with more than 543,000 children (ages
621) identified by the public school system as having
some level of ID (U.S. Department of Education,
2007). A diagnosis of ID has a number of important
implications, including eligibility for supports such as
academic services, residential placement, vocational
support, and Social Security Disability, as well as
ineligibility for capital punishment.
The definition of ID has undergone many
revisions. Initially, ID referred only to impairments
in intellectual functioning; however, in 1959,
impairments in age-appropriate day-to-day functioning (adaptive functioning) formally became part of
the definition (Heber, 1959, 1961). More recent
diagnostic formulations of ID have maintained the
requirements for deficits in both intellectual ability
and adaptive functioning. In the Diagnostic and
Statistical Manual of Mental DisordersFourth Edition
A. Papazoglou et al.
(Text Revision; DSM-IV-TR), the intellectual
impairment component of the diagnosis of ID
was defined as significantly subaverage intellectual
functioning: an IQ of approximately 70 or below
(American Psychiatric Association, 2000, p. 49).
Based largely upon the definition of adaptive
functioning proposed by the American Association
of Intellectual and Developmental Disabilities
(AAIDD, formerly known as the American Association on Mental Retardation; Luckasson et al.,
1992), DSM-IV-TR defined adaptive functioning
deficits as concurrent impairments (e.g., performance approximately 2 standard deviations [SD]
below the mean) in at least two theoretically derived
adaptive skill areas (i.e., communication, self-care,
home living, social/interpersonal skills, use of community resources, self-direction, functional academic
skills, work, leisure, health, and safety; American
Psychiatric Association, 2000). Of note, there is
some debate about whether there are 10 or 11
adaptive skill areas depending on whether or not
health and safety are considered distinct skill areas.
Subsequently, broader factors or adaptive domains
composed of these individual adaptive skill areas
were described (e.g., Greenspan, 1999; Harrison &
Oakland, 2003; Luckasson et al., 2002; Thompson,
McGrew, & Bruininks, 1999). These three broad
165
INTELLECTUAL AND DEVELOPMENTAL DISABILITIES
2014, Vol. 52, No. 3, 165174
domains (i.e., Conceptual, Social, Practical) have
since been incorporated into the AAIDD description of adaptive functioning (Luckasson et al., 2002;
Schalock et al., 2010).
The fifth edition of the DSM (DSM-5; American
Psychiatric Association, 2013) includes a change in
the name of the disorder, a revision of the diagnostic
criteria, and changes in the severity specifiers.
Consistent with the AAIDDs and the international
communitys shift from the term mental retardation to
intellectual disability, DSM-5 uses the term intellectual
disability coupled with the term intellectual developmental disorder (to be consistent with International
Classification of Diseases, 11th Edition). As was the case
with DSM-IV, DSM-5 diagnostic criteria for ID
specify evidence of intellectual and adaptive impairment during the developmental period. DSM-5
criteria pertaining to intellectual impairment are
similar to those of DSM-IV and stipulate deficits in
general mental abilities such as reasoning, problemsolving, planning, abstract thinking, judgment, academic learning, and learning from experience,
defined as an IQ of approximately # 70 (6 5 points
for error; American Psychiatric Association, 2013,
p. 37). The DSM-5 criteria pertaining to deficits in
adaptive functioning, however, have been more
significantly modified. Specifically, adaptive impairment is defined as follows (American Psychiatric
Association, 2013):
Deficits that result in failure to meet
developmental and sociocultural standards for
personal independence and social responsibility (p. 33).[The criterion] is met when at
least one domain of adaptive functioning
conceptual, social, or practicalis sufficiently
impaired that ongoing support is needed in
order for the person to perform adequately in
one or more life settings at school, work, home
or in the community. (p. 38)
In contrast to DSM-IV, which stipulated impairments in two or more skill areas, DSM-5 criteria
denote impairment in one or more superordinate
domains of adaptive functioning (e.g., Conceptual,
Social, Practical).
DSM-5 also redefines how ID severity is
determined. DSM-IV-TR defined severity on the
basis of IQ test scores (mild, moderate, severe,
or profound). These same levels of severity are
retained; however, in DSM-5 the various levels of
severity are defined on the basis of adaptive
166
AAIDD
DOI: 10.1352/1934-9556-52.3.165
functioning, and not IQ scores, because it is
adaptive functioning that determines the level of
supports required. Moreover IQ measures are less
valid in the lower end of the IQ range (American
Psychiatric Association, 2013, p. 33).
For diagnostic purposes under DSM-5, deficits
in adaptive functioning are still established by way
of clinical evaluation and administration of psychometrically sound measures, such as questionnaires that elicit observer or informant ratings of an
individuals typical level of independent functioning (McCarver & Campbell, 1987). Of note,
however, DSM-5 provides a table offering additional guidance for determining severity of adaptive
impairment (i.e., mild, moderate, severe, and
profound) within Conceptual, Social, and Practical
domains. This table is intended to assist in
determination of severity of adaptive impairment,
although no specific guidance is given regarding the
use of test scores for the determination of severity
specifiers (e.g., the mild range of ID is not defined
by a test score range). Clinicians are encouraged to
use both clinic evaluation and individualized,
culturally appropriate, psychometrically sound measures (American Psychiatric Association, 2013,
p. 37), and to use clinical judgment when interpreting scores from these measures.
One such standardized observerinformant
report instrument is the Adaptive Behavior Assessment SystemSecond Edition (ABAS-II; Harrison
& Oakland, 2003), which is a commonly used
measure of adaptive functioning on which a
caregiver rates the individuals level of independent
functioning on multiple items across skill areas.
The parent form is used for children ages 521 years
and provides estimates of the childs functioning
across 9 skill areas (or 10 skill areas if he or she is
employed). Scale composition of the first edition of
the ABAS (Harrison & Oakland, 2000) was
substantively influenced by the definition of
adaptive functioning proposed by the AAIDD and
others (e.g., Luckasson et al., 1992; Thompson
et al., 1999), as well as the diagnostic criteria in
DSM-IV. The skill areas were maintained in the
publication of the second edition (ABAS-II;
Harrison & Oakland, 2003), but in keeping with
the existing body of research (e.g., Greenspan,
1999; Harrison & Oakland, 2003; Luckasson et al.,
2002; Thompson et al., 1999) and the revised ID
conceptualization proposed by the AAIDD, these
skill areas were further organized into three broad
adaptive skill domains: Conceptual, Practical, and
Intellectual Disability and DSM-5
INTELLECTUAL AND DEVELOPMENTAL DISABILITIES
AAIDD
2014, Vol. 52, No. 3, 165174
Social. The ABAS-II domains have increased
relevance with the publication of DSM-5, as they
map onto the new adaptive domain model
presented in DSM-5. Of note, the ABAS-II
groupings of the individual skill areas into domain
scales were modeled on theoretical foundations
based in earlier research, and were not based on
exploratory factor loadings. Subsequently, confirmatory factor analysis of the ABAS-II has yielded
only modest support for this three-factor model
(Wei, Oakland, & Algina, 2008), and there is
evidence to suggest that the most parsimonious fit
to the data is a one-factor solution (Harrison &
Oakland, 2003). To date, there has been little
research on the appropriateness of the 9 and 10 skill
area factors.
The aim of this study was to examine the
potential impact of the DSM-5 diagnostic criteria
on classification rates of ID. There is the potential
for a gray zone in which individuals meet ID
criteria under the DSM-IV-TR criteria (i.e., impairment in two or more skill areas) but not under
DSM-5 criteria (i.e., impairment in one or more
domains), particularly when psychometric measures
such as the ABAS-II are used as the primary means
to quantify deficits in adaptive functioning. For
instance, under the ABAS-II factor structure,
individuals with skill deficits in home living and
self-care might still qualify for ID, as both of these
skills are grouped under the Practical domain
factor. In contrast, an individual with skill deficits
in social skills and functional communication
might not, as these skill areas are grouped into
different domain factors. Clarification of a possible
diagnostic drift in ID diagnoses is valuable, as the
implications for the educational (i.e., eligibility for
special education services), social (i.e., eligibility
for entitlement services and funding), and legal
(i.e., capital punishment decisions) systems may be
profound. To this end, we examined ID classification rates using a psychometric definition of
impairment as two or more skill areas (DSM-IVTR criteria) and one domain area (DSM-5 criteria),
with adaptive impairment defined as standardized
scores $ 2 SD below the mean. Given persistent
questions about the factor structure of the ABASII, we hypothesized that, when compared with
classification rates of ID using DSM-IV-TR criteria,
diagnosis based on psychometrically defined impairment in one domain (DSM-5 criteria) has the
potential to result in significantly fewer children
meeting criteria for ID.
A. Papazoglou et al.
DOI: 10.1352/1934-9556-52.3.165
Methods
Participants
For the purposes of this study, de-identified patient
records from the clinical database of the Department of Neuropsychology at the Kennedy Krieger
Institute, a large medical institute serving youth
with developmental disabilities in the mid-Atlantic
region, were reviewed. Data are routinely entered
into this database by department clinicians via the
electronic health record, and are securely maintained by the information systems department.
After approval by the Johns Hopkins Hospital
institutional review board, a limited dataset was
constructed of patients between the ages of 6 and
16 years for whom valid scores on both intellectual
(e.g., Wechsler Intelligence Scales for Children
Fourth Edition, WISC-IV; Wechsler, 2003) and
adaptive (e.g., ABAS-II; Harrison & Oakland,
2003) measures were available. The final sample
included 884 children (mean age 5 10.49, SD 5
2.80; 67% male), for whom records included
WISC-IV and ABAS-II scores, age at time of
assessment, ethnicity, and sex. All patients included in the dataset had been referred for outpatient
neuropsychological assessment. Of these 884 children and adolescents, 203 had a Full Scale IQ
(FSIQ) that was $ 2 SD below the mean (FSIQ #
70), representing 23% of the total clinically
referred sample.
Measures
ABAS-II. The ABAS-II is a parent-report
questionnaire assessing whether an individual
independently displays the functional skills necessary for age-appropriate daily living. The ABAS-II
divides adaptive functioning into nine skill areas,
which are subsumed under three theoretically
derived domains: the Conceptual Domain (Communication, Functional Academics, and Self-Direction skill areas), Social Domain (Leisure and
Social skill areas), and Practical Domain (Community Use, Home Living, Health and Safety, and
Self-Care skill areas). A 10th skill area, Work skills,
can be administered to older adolescents and young
adults who are employed, but it was not included in
this study given the age range of the sample. The
nine primary skill areas can be used to generate a
General Adaptive Composite (GAC). As noted in
the test manual (Harrison & Oakland, 2003), the
ABAS-II GAC has strong internal consistency
(a 5 .98) as do the domain (a 5 .86.93) and skill
167
INTELLECTUAL AND DEVELOPMENTAL DISABILITIES
AAIDD
2014, Vol. 52, No. 3, 165174
area scores (a 5 .95.97). Stability over time (M 5
12 days, SD 5 10 days) is strong (GAC corrected
testretest reliability r 5 .93, domain corrected
testretest r 5 .89.93, skill area corrected test
retest r 5 .84.92). The ABAS-II also has
demonstrated adequate validity in a sample of
children with ID (e.g., mean GAC scores in a group
of 41 individuals between the ages of 5 and 21
diagnosed with ID, of unspecified severity, was
equal to 63.7, mean skill area scaled scores ranged
from 3.7 to 5.5). Of note, 82.93% of these
individuals with ID had two or more individual
skill area scores that fell at or below 22 SD, while
80.49% of these same individuals had one or more
adaptive domain scores that fell at or below 22 SD
based on caregiver report. Because the sample is
described as unspecified, there is no way to
examine these data at various levels of intellectual
impairment (e.g., mild versus moderate intellectual
ability). However, although statistical significance
was not reported, there was a trend toward a higher
percentage of impaired skill area scores reported for
individuals with mild ID in the validity data for the
teacher version of the ABAS-II. Specifically, of the
66 individuals with mild ID who were rated by their
teachers on the ABAS-II, 75.76% had two or more
individual skill areas scores that fell at or below 22
SD, while only 60.61% of these same individuals
had one or more adaptive domain scores that fell at
or below 22 SD (Harrison & Oakland, 2003).
Two other commonly used measures of adaptive functioning are the Vineland Adaptive Behavior Scales, Second Edition (VABS-II; Sparrow,
Cicchetti, & Balla, 2005) and the Scales of
Independent Behavior, Revised (SIB-R; Bruininks,
Woodcock, Weatherman, & Hill, 1996). Correlations between the ABAS-II GAC and VABS-II
Adaptive Behavior Composite were moderately
high (r 5 .78), with correlations at the subdomain/skill area level mostly falling in the 0.50
range. Correlations between the ABAS-II GAC
parent version and the Early Development Form of
the SIB-R Broad Independence Score were low (r
5 .18), while the correlation between the ABAS-II
GAC teacher-version and the Short Form of the
SIB-R Broad Independence Score were stronger
(r 5 .59).
WISC-IV. The WISC-IV is a widely accepted
measure of intellectual ability with adequate
psychometric properties for identifying children
with ID. The WISC-IV provides a global intellectual estimate, the FSIQ. The FSIQ has shown
168
DOI: 10.1352/1934-9556-52.3.165
excellent internal reliability and stability over time
(e.g., internal consistency estimates [split-half]
yield an FSIQ r 5 .97; corrected testretest r 5
.93). The WISC-IV FSIQ also has demonstrated
adequate validity for use with this population
(Wechsler, 2003).
Experimental Design
First, we examined the pattern of associations
between measures of intellectual and adaptive skill
areas. Next, the total number of children who met
strict DSM-IV-TR criteria for ID was identified
(i.e., WISC-IV FSIQ # 70, with two or more skill
areas on the ABAS-II # scaled score of 4). The
total number of children who met the psychometrically defined DSM-5 criteria was then calculated
(i.e., WISC-IV FSIQ # 70, with one or more
domains on the ABAS-II # 70). The McNemar
test was used to compare the differences in the
proportion of individuals classified as ID based on
the changing criteria for adaptive impairment.
Results
Of the 203 children with FSIQ # 70, 166 met
DSM-IV-TR criteria for adaptive impairment, that
is, impairment in two or more skill areas. On the
basis of DSM-5 criteria for adaptive impairment
(i.e., impairment in one or more adaptive domains),
151 children met criteria for ID. This represents a
net loss of 15 children. Sixteen children met DSMIV-TR criteria but not DSM-5 criteria, and one
child met DSM-5 criteria but did not meet DSMIV-TR criteria. This net difference of 15 children
represents a statistically significant 9% decrease in
the number of children who met criteria for ID
under DSM-5 as compared to DSM-IV-TR (McNemar test x2 5 122.02, p 5 .001). Mean scores on
the ABAS-II and WISC-IV for the children who
meet DSM-IV-TR and DSM-5 criteria for adaptive
impairment are presented in Table 1.
In the total clinically referred sample (N 5
884), there was a broad range of correlations
between FSIQ and individual skill areas on the
ABAS-II. The strongest correlations were noted
between FSIQ and the ABAS-II Functional
Academics (r 5 .56, p , .001) and Communication (r 5 .39, p , .001) skill area scales. All of the
remaining seven ABAS-II skill area scales also were
significantly correlated with FSIQ (p , .001), with
correlations ranging from r 5 .13 to r 5 .32. Each
of the composite domain scales of the ABAS-II was
Intellectual Disability and DSM-5
INTELLECTUAL AND DEVELOPMENTAL DISABILITIES
AAIDD
2014, Vol. 52, No. 3, 165174
DOI: 10.1352/1934-9556-52.3.165
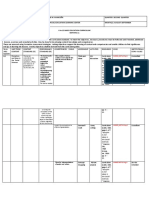
Table 1
Descriptive Statistics
Variable
Age in years
Percent male
Percent White: African American:
Other: Unknown
WISC-IV FSIQ
ABAS-II GAC
ABAS-II Conceptual
ABAS-II Social
ABAS-II Practical
All children with
FSIQ # 70
(n 5 203)
DSM-IV: FSIQ and
two skill areas impaired
(n 5 166)
DSM-5: FSIQ and
one domain impaired
(n 5 151)
11.32 (2.73)
66
11.35 (2.69)
67
11.38 (2.71)
68
37: 42: 6: 15
60.25 (7.79)
66.22 (15.21)
68.88 (13.74)
74.82 (15.63)
66.22 (15.22)
38: 41: 7: 14
59.49 (8.06)
61.10 (10.67)
64.82 (10.42)
70.36 (12.44)
60.43 (15.27)
40: 38: 7: 15
59.15 (8.21)
59.28 (9.23)
63.15 (9.30)
68.58 (11.10)
58.20 (14.26)
Note. Standard deviations are presented in parentheses. ABAS-II and WISC-IV scores are presented as standard
scores.
significantly correlated with FSIQ (all p , .001),
with the strongest correlations noted with the
Conceptual domain (r 5 .48) as compared to the
Social (r 5 .31) and Practical (r 5 .32) domains. In
children with FSIQ # 70, the frequency of
impaired scores (i.e., scaled score # 4) on the
ABAS-II skill area scales was as follows: Home
Living (70%), Self-Direction (68%), Social (66%),
Functional Academics (58%), Self-Care (56%),
Community Use (51%), Communication (46%),
Health and Safety (45%), and Leisure (35%). In
this group, impaired domain scores (standard scores
# 70) were most frequently found on the
Conceptual (62%) and Practical (62%) composites
and were less frequently observed on the Social
composite (48%).
Data on the 17 children whose status changed
with the shift to DSM-5 criteria are presented in
Table 2. Bold font is used to denote children who
were impaired in ABAS-II skill areas. The one
child who met DSM-5, but not DSM-IV, criteria
was impaired on the Conceptual domain and had a
single area of skill area impairment (Communication), with three other skill areas in the borderlineimpaired range. Of the 16 children who met DSMIV, but not DSM-5, criteria, 100% had a FSIQ of
# 70, 25% had a Verbal Comprehension Index of
# 70, 38% had a Perceptual Reasoning Index of
# 70, 81% had a Working Memory Index of # 70,
and 88% had a Processing Speed Index of # 70.
The majority of these children had two skill areas
impaired (69%), with 19% impaired on three skill
areas, and 12% impaired on four skill areas. Home
A. Papazoglou et al.
Living was most likely to be impaired (56%),
followed by Communication (38%), Functional
Academics (38%), Self-Care (31%), Social (31%),
Self-Direction (19%), Community Use (19%), and
Health & Safety (12%). No children were impaired
on Leisure.
Discussion
This study sought to investigate any potential
impact on the rates of ID classification when an
existing and widely used adaptive functioning
measure (ABAS-II) was used to psychometrically
determine deficits in adaptive functioning based on
implementation of the new DSM-5 ID criteria. The
DSM-5s use of adaptive impairment to quantify
severity of ID highlights a renewed emphasis on
adaptive functioning in this condition. There is
concern, however, that the diagnostic change from
adaptive skill deficits to adaptive domain deficits
might make the diagnosis more restrictive due to
instrumentation and measurement issues, particularly when psychometric measures are used as the
primary means to quantify deficits in adaptive
functioning. We hypothesized that, when using the
ABAS-II to psychometrically quantify adaptive
impairment, fewer children would qualify for an
ID diagnosis when DSM-5 criteria were implemented (relative to DSM-IV). This was supported, as we
identified a potential 9% decline in the number of
children who met criteria for DSM-5 as compared
with DSM-IV-TR in our large clinical sample. Of
note, the children excluded by DSM-5 ID criteria
had milder degrees of adaptive impairment,
169
170
67
65
54
67
68
56
59
70
70
56
64
61
60
52
69
55
13.75
13.17
14.58
14.33
8.75
12.58
11.42
8.5
11.42
8.42
10.67
7.92
7.42
8.42
12.67
13.08
89
83
73
79
69
75
79
73
89
59
79
75
65
57
77
77
57
73
75
57
73
88
55
57
71
73
73
61
73
71
61
86
51
59
75
79
82
88
69
85
84
77
84
76
85
80
82
69
70
82
78
Does not meet ID criteria for DSM-IV, but does meet criteria for DSM-5
67
84
87
2
7
5
6
Meet criteria for ID on DSM-IV-TR but not on DSM-5
72
90
79
6
6
5
5
75
90
82
9
8
6
5
78
97
81
7
7
6
3
91
100
83
10
11
9
3
72
81
75
6
8
1
2
86
92
87
8
6
4
3
87
93
82
13
7
4
4
88
72
79
9
7
7
4
72
105
86
7
10
6
1
81
96
72
3
6
5
2
80
97
87
4
10
6
4
83
87
85
3
2
9
11
81
72
95
4
9
7
8
75
72
78
3
7
3
6
72
78
78
2
4
4
6
80
93
82
9
1
4
8
7
10
11
10
6
11
9
6
7
3
9
7
11
4
5
7
11
6
8
10
10
7
7
8
5
12
8
10
10
6
5
9
6
2
3
4
3
4
8
6
6
11
8
8
7
7
5
6
10
4
1
9
6
6
9
5
7
2
9
8
5
5
8
9
5
9
7
9
11
5
9
10
4
10
10
9
4
3
4
2
11
Health
Communi- Functional Home and
Self- Self-Dication Use Academics Living Safety Leisure Care rection Social
2014, Vol. 52, No. 3, 165174
Note. Boldface indicates children with impairment on the same skill area of the ABAS-II. WISC-IV and ABAS-II GAC and domain scores are presented as
standard scores, ABAS-II skill area scores are presented as scaled scores. Abbreviation: VCI, Verbal Comprehension Index; PRI, Perceptual Reasoning
Index.
50
10.92
Age WISC-IV
ABAS-II
Commu(years) FSIQ
VCI PRI GAC Conceptual Social Practical nication
Table 2
Standardized Scores on the ABAS-II and WISC-IV for Children Whose ID Diagnostic Classification Changes With the Implementation of DSM-5 Criteria
INTELLECTUAL AND DEVELOPMENTAL DISABILITIES
DOI: 10.1352/1934-9556-52.3.165
AAIDD
Intellectual Disability and DSM-5
INTELLECTUAL AND DEVELOPMENTAL DISABILITIES
2014, Vol. 52, No. 3, 165174
although their profiles still indicated a high level of
adaptive and intellectual impairment. Given the
relatively mild nature of their adaptive impairment,
it is unclear whether these children and adolescents
would have been identified with ID during the
DSM-IV-TR era, even though their IQ and ABASII scores were consistent with the diagnostic
criteria. As such, these data are of somewhat
limited value in anticipating the true impact of
DSM-5 on rates of ID. What these data do
highlight, however, is the need for clinical
judgment when interpreting these scores, rather
than a strict reliance upon scores from the current
psychometric scale compositions.
When adaptive impairment is psychometrically
defined using ABAS-II scores, the children in our
sample who would be left out of an ID diagnosis
by the impaired domain criterion still show
compelling evidence of intellectual and adaptive
skill impairment. Among the children left out of
the DSM-5 ID classification, their various combinations of adaptive skill area deficits tended to load
onto different domains (rather than a single
domain), resulting in domain level scores that were
above a standard score of 70 in spite of the presence
of impairment in multiple skill areas. For instance,
a child with skill area deficits in Communication,
Social skills, and Community Use may experience
significant adaptive impairment, even though each
of these skill areas is grouped onto separate ABASII domains and these composite scores may fall
within normal limits. Analysis of adaptive functioning in the 16 children who would be excluded
from an ID diagnosis based on DSM-5 criteria
revealed that Home Living was the most commonly
impaired skill area, followed by Communication,
Functional Academics, Self-Care, and Social skills.
These skill areas span all three of the ABAS-II
adaptive domains, and highlight the manner in
which significant skill area deficits may be hidden
by grossly intact domain scores.
Given the common assumption that intellectual deficits contribute to deficits in adaptive skills
in youths with ID, it is not unexpected that
intellectual and adaptive functioning would be
significantly correlated. From a measurement
perspective, however, it remains unclear whether
a low score in an adaptive area that is highly
correlated with IQ constitutes a distinct area of
adaptive deficit related to IQ rather than simply a
multimethod approach to measuring the same
construct. This has, in fact, been a criticism of
A. Papazoglou et al.
AAIDD
DOI: 10.1352/1934-9556-52.3.165
the formulation of the diagnosis of ID in the past,
as Greenspan (2006) and others have proposed
that the Conceptual composite of the ABAS-II
and its constituent skill area scales may measure
much the same construct as an IQ test (i.e.,
conceptual or academic intelligence). Indeed, in
our sample of children with a FSIQ of # 70, IQ
was most highly correlated with the Conceptual
domain (r 5 .30, p , .001), with smaller, albeit
still significant, correlations with the Practical
(r 5 .27, p , .001) and Social (r 5 .18, p , .001)
domains. As noted, the degree of variation in
correlation between IQ and adaptive domain
scores not only raises a concern regarding multimethod assessment of the same construct (e.g., IQ
and Conceptual adaptive functioning), but also
raises a question as to the relatedness of IQ and
adaptive functioning in general. While each
ABAS-II adaptive domain was significantly correlated with IQ, the varying degrees of correlation
between IQ and the three adaptive domains brings
into question the idea of a direct relationship,
which is presumed in the ID diagnosis (i.e., To
meet diagnostic criteria for intellectual disability,
the deficits in adaptive functioning must be
directly related to the intellectual impairments,
American Psychiatric Association, 2013, p. 38).
Future conceptualizations of ID may benefit
from further shifting the diagnostic emphasis to
deficits in adaptive functioning, as this might better
define a subgroup of individuals who are highly
vulnerable to exploitation or injury and require
additional protections (regardless of IQ). Barkley
and colleagues have proposed the concept of
adaptive disability, in which deficits in adaptive
functioning are associated with behavioral factors
(e.g., conduct problems, inattention, aggression)
within the context of broadly intact intelligence
(Barkley et al., 2002; Shelton et al., 1998). Other
recent work has identified relatively distinct
cognitivebehavioral clusters associated with deficits in adaptive functioning, with IQ representing
only one of many variables thought to contribute to
deficits in adaptive functioning (Papazoglou, Jacobson, & Zabel, 2013a). We propose that future
DSM revisions consider the evidence for the
concept of an adaptive disability in which deficits
in adaptive functioning are the primary diagnostic
feature, with associated specifiers to qualify presumed etiologies (e.g., with intellectual deficits,
with executive functioning deficits, with affective
dysregulation, etc.).
171
INTELLECTUAL AND DEVELOPMENTAL DISABILITIES
2014, Vol. 52, No. 3, 165174
In closing, we strongly recommend that
discussion concerning the impact of new DSM-5
ID diagnostic criteria include discussion of practical
assessment issues that may occur when new
diagnostic criteria are implemented using existing
test instruments such as the ABAS-II. First,
although existing adaptive skill instruments have
been shown to be reliable, it is very important that
the underlying construction of the tests be considered when they are applied to new diagnostic
formulations. As noted earlier, the domain factor
structure of the ABAS-II was organized on the basis
of theoretical foundations, and the model then
underwent confirmatory factor analysis. Although
this is an appropriate method for test construction,
it may not capture the strongest factor loadings or
provide information about other potential arrangements of the scales. Subsequently, individual
adaptive skill area deficits may be somewhat
silenced in the larger factor model. As such, the
diagnostic utility of existing adaptive skill instruments such as ABAS-II should be explored before
presuming that they are equally valid under both
DSM-IV-TR and DSM-5 conditions, and clinical
judgment should continue to be emphasized in the
diagnostic process to help minimize possible
psychometric measurement issues. Moreover, agreement between different measures should be explored, as quantification of deficits in adaptive
functioning can vary considerably between instruments (Papazoglou, Jacobson, & Zabel, 2013b) and
further complicate the diagnostic picture. To
mitigate the potential impact of these issues,
DSM-5 recommends that the clinician use multiple
sources of information as well as clinical judgment
when establishing whether an individual presents
with significant deficits in adaptive behavior.
In addition, we recommend that the appropriateness of content from current adaptive skill
instruments be reviewed, particularly given the
renewed emphasis placed on adaptive impairment
in the DSM-5 ID diagnostic formulation. Due to the
pace of accommodative technology, the definition of
an adaptive deficit is likely to continue to change
rapidly. Although the advent of GPS guidance
systems, text-to-speech software, smart phones,
electronic cueing devices, and other technologies
has created exciting new habilitation opportunities,
the speed with which these devices become available
outpaces the more time-intensive process necessary
for the development and standardization of adaptive
skill measures. This dilemma will likely continue,
172
AAIDD
DOI: 10.1352/1934-9556-52.3.165
creating a disparity between the reality of the
individuals situation (e.g., ability to use a smart
phone and access the Internet) and the content of
the latest version of a standardized adaptive skill
instrument (e.g., ability to use a pay phone and read
a newspaper). Lack of items reflecting an individuals
ability to use technologies such as a smart phone, a
computer, and the Internet creates both face validity
and content validity questions, particularly as these
types of technologies continue to become normal,
necessary components of daily living rather than
accommodative technologies or interventions. This
is a particularly salient dilemma for the ABAS-II,
which contains the same item content from the
original ABAS, which was developed prior to the
collection of standardization data between December 1998 and December 1999.
Although these findings have important implications for clinical practice and policy, this study
has several limitations. All children were clinically
referred, so results may not be consistent with
potential findings in a nonreferred population,
although it is worth noting that the decisionmaking process regarding classification of ID is
inherently a clinical one. More specifically, however, the Kennedy Krieger Institute is an internationally recognized center of excellence for children
with developmental disabilities, thus the population
of children referred for evaluation here may be more
significantly impaired than those for whom ID
classification decisions are made in other settings
(e.g., local school special education decisions). If this
is indeed the case, the measurement issues raised
concerning the ABAS-II skill area and adaptive
domain scores may be overrepresented or underrepresented. More research is needed regarding the
factor structure of the ABAS-II and whether the 9
and 10 skill areas and three domains represent
appropriate factor groupings of the ABAS-II items.
Research to date has shown only modest support for
the three domains (Wei et al., 2008), and there are
limited data on the 9-and-10 factor solutions. No
data were available regarding whether clinicians
actually made a diagnosis of ID for all 166 children
who met formal DSM-IV-TR criteria, and, to our
knowledge, there are no published data examining
how consistently clinicians adhered to DSM-IV-TR
diagnostic criteria when making a diagnosis of ID.
Nevertheless, these findings suggest a risk of fewer ID
diagnoses when existing adaptive functioning instruments are used as the primary means by which to
implement DSM-5 criteria for adaptive impairment.
Intellectual Disability and DSM-5
INTELLECTUAL AND DEVELOPMENTAL DISABILITIES
2014, Vol. 52, No. 3, 165174
References
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders
(4th ed., text rev). Arlington, VA: Author.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders
(5th ed.). Washington, DC: Author.
Barkley, R. A., Shelton, T. L., Crosswait, C.,
Moorehouse, M., Fletcher, K., Barrett, S., &
Metevia, L. (2002). Preschool children with
disruptive behavior: Three-year outcome as a
function of adaptive disability. Developmental
Psychopathology, 14, 4567.
Bruininks, R. H., Woodcock, R. W., Weatherman,
R. F., & Hill, B. K. (1996). Scales of Independent
Behavior-Revised. Chicago, IL: Riverside Publishing.
Greenspan, S. (1999). A contextualist perspective
on adaptive behavior. In R. L. Schalock (Ed.),
Adaptive behavior and its measurement: Implications for the field of mental retardation (pp. 61
80). Washington, DC: American Association
on Mental Retardation.
Greenspan, S. (2006). Mental retardation in the real
world: Why the AAMR definition is not there
yet. In H. N. Switzky & S. Greenspan (Eds.),
What is mental retardation? Ideas for an evolving
disability in the 21st century (pp. 167185).
Washington DC: American Association on
Intellectual and Developmental Disabilities.
Harrison, P., & Oakland, T. (2000). Adaptive
behavior assessment system. San Antonio, TX:
The Psychological Corporation.
Harrison, P., & Oakland, T. (2003). Adaptive
behavior assessment system (2nd ed.). San
Antonio, TX: The Psychological Corporation.
Heber, R. (1959). A manual on terminology and
classification in mental retardation: A monograph supplement. American Journal of Mental
Deficiency (Monograph Supplement), 64, 1111.
Heber, R. (1961). A manual on terminology and
classification in mental retardation (rev. ed.).
Washington, DC: American Association on
Mental Deficiency.
Larson, S. A., Lakin, K. C., Anderson, L., Kwak, N.,
Lee, J. H., & Anderson, D. (2001). Prevalence
of mental retardation and developmental disabilities: Estimates from 1994/1995 National
Health Survey Disability Supplement. American
Journal of Mental Retardation, 106, 231252.
Luckasson, R., Borthwick-Duffy, S., Buntinx,
W. H. E., Coulter, D. L., Craig, E. M., Reeve,
A. Papazoglou et al.
AAIDD
DOI: 10.1352/1934-9556-52.3.165
A.,Tasse, M. J. (2002). Mental retardation:
Definition, classification, and systems of supports
(10th ed.). Washington, DC: American Association on Mental Retardation.
Luckasson, R., Coulter, D. L., Polloway, E. A.,
Reiss, S., Schalock, R. L., Snell, M. E.,Stark,
J. A. (1992). Mental retardation: Definition,
classification, and systems of supports (9th ed.).
Washington, DC: American Association on
Mental Retardation.
Maulik, P. K., Mascarenhas, M. N., Mathers, C. D.,
Dua, T., & Saxena, S. (2011). Prevalence of
intellectual disability: A meta-analysis of
population-based studies. Research in Developmental Disabilities, 32, 419436.
McCarver, R. B., & Campbell, V. A. (1987). Future
developments in the concept and application
of adaptive behavior. Journal of Special Education, 21, 197207.
Papazoglou, A., Jacobson, L., & Zabel, T. A.
(2013a). More than intelligence: Distinct
cognitive/behavioral clusters linked to adaptive
dysfunction in children. Journal of the International Neuropsychological Society, 19, 189197.
Papazoglou, A., Jacobson, L. A., & Zabel, T. A.
(2013b). Sensitivity of the BASC-2 Adaptive
Skills Composite in detecting adaptive impairment in a clinically referred sample of children
and adolescents. The Clinical Neuropsychologist,
27, 386395.
Schalock, R. L., Borthwick-Duffy, S. A., Bradley,
V. J., Buntix, W. H. E., Coulter, D. L., Craig,
E. M.,Yeager, M. H. (2010). Intellectual
disability: Definition, classification, and systems
of supports (11th ed.).Washington, DC: American Association on Mental Retardation.
Shelton, T. L., Barkley, R. A., Crosswait, C.,
Moorehouse, M., Fletcher, K., Barrett, S., &
Metevia, L. (1998). Psychiatric and psychological morbidity as a function of adaptive
disability in preschool children with aggressive
and hyperactive-impulsive inattentive behavior. Journal of Abnormal Child Psychology, 26,
475494.
Sparrow, S. S., Cicchetti, D. V., & Balla, D. A.
(2005). Vineland Adaptive Behavior Scales (2nd
ed.). Circle Pines, MN: American Guidance
Service, Inc.
Thompson, J. R., McGrew, K. S., & Bruininks,
R. H. (1999). Adaptive and maladaptive behavior: Functional and structural characteristics.
In R.L. Schalock (Ed.), Adaptive behavior and its
173
INTELLECTUAL AND DEVELOPMENTAL DISABILITIES
2014, Vol. 52, No. 3, 165174
measurement: Implications for the field of mental
retardation (pp. 1542). Washington, DC:
American Association on Mental Retardation.
U.S. Department of Education. (2007). 29th annual
report to Congress on the implementation of the
Individuals with Disabilities Education Act, 2007
(Vol. 1). Washington, DC: Author.
Wechsler, D. (2003). WISC-IV technical and
interpretive manual. San Antonio, TX: The
Psychological Association.
Wei, Y., Oakland, T., & Algina, J. (2008).
Multigroup confirmatory factor analysis for
the Adaptive Behavior Assessment System-II
Parent Form, Ages 521. American Journal of
Mental Retardation, 113, 178186.
174
AAIDD
DOI: 10.1352/1934-9556-52.3.165
Received 7/6/2013, accepted 10/2/2013.
Authors:
Aimilia Papazoglou, Childrens Healthcare of
Atlanta; Lisa A. Jacobson, Kennedy Krieger
Institute; Marie McCabe, Saratoga Springs, NY;
Walter Kaufmann, Boston Childrens Hospital;
T. Andrew Zabel, Kennedy Krieger Institute.
Correspondence concerning this article should be
addressed to Aimilia Papazoglou, Childrens Healthcare of Atlanta, Neuropsychology, Suite 180, 5455
Meridian Mark Road, Atlanta, GA 30342 (e-mail:
emily.papazoglou@choa.org).
Intellectual Disability and DSM-5
Você também pode gostar
- New Terminology For Mental Retardation in DSM-5 and ICD-11: EditorialDocumento3 páginasNew Terminology For Mental Retardation in DSM-5 and ICD-11: EditorialLupita LeyvaAinda não há avaliações
- Development and Standardization of The Diagnostic Adaptive Behavior Scale: Application of Item Response Theory To The Assessment of Adaptive BehaviorDocumento16 páginasDevelopment and Standardization of The Diagnostic Adaptive Behavior Scale: Application of Item Response Theory To The Assessment of Adaptive BehaviorCarolina MoraesAinda não há avaliações
- The Relation Between Intellectual Functioning and Adaptive Behavior in The Diagnosis of Intellectual DisabilityDocumento10 páginasThe Relation Between Intellectual Functioning and Adaptive Behavior in The Diagnosis of Intellectual DisabilityCristinaAinda não há avaliações
- Practical - 1: Changes Made in The Classificafatory System From DSM - Iv To DSM - VDocumento5 páginasPractical - 1: Changes Made in The Classificafatory System From DSM - Iv To DSM - VRakesh KumarAinda não há avaliações
- APA - DSM 5 Intellectual Disability PDFDocumento2 páginasAPA - DSM 5 Intellectual Disability PDFEmil Mari FollosoAinda não há avaliações
- TEXTO INGLES 2021pdfDocumento10 páginasTEXTO INGLES 2021pdfLaura RamirezAinda não há avaliações
- Borderline Intellectual Functioning: A Systematic Literature ReviewDocumento28 páginasBorderline Intellectual Functioning: A Systematic Literature ReviewlbburgessAinda não há avaliações
- DSM 5 Intellectual Disability Fact SheetDocumento2 páginasDSM 5 Intellectual Disability Fact Sheetapi-242024640Ainda não há avaliações
- DSM 5 Intellectual Disability Fact SheetDocumento2 páginasDSM 5 Intellectual Disability Fact SheetMelissa Ortega MaguiñaAinda não há avaliações
- Intellectual Disability Fact Sheet PDFDocumento2 páginasIntellectual Disability Fact Sheet PDFAle M. Martinez100% (2)
- Leichsenring 2019Documento14 páginasLeichsenring 2019Ekatterina DavilaAinda não há avaliações
- Oltmanns & Widiger in Press PiCDDocumento54 páginasOltmanns & Widiger in Press PiCDDaniel KoffmanAinda não há avaliações
- Mental RetarditionDocumento14 páginasMental RetarditionDenvergerard Tamondong100% (1)
- Adaptive Behavior Assessment - Tasse (2009)Documento10 páginasAdaptive Behavior Assessment - Tasse (2009)Karen Steele50% (2)
- Personality Disorder Intro SampleDocumento17 páginasPersonality Disorder Intro SampleCess NardoAinda não há avaliações
- Personality Inventory For DSM-5 (PID-5) in Clinical Versus Nonclinical Individuals: Generalizability of Psychometric FeaturesDocumento12 páginasPersonality Inventory For DSM-5 (PID-5) in Clinical Versus Nonclinical Individuals: Generalizability of Psychometric FeaturesJasmine BurgosAinda não há avaliações
- Critically Evaluate The Difference Between DSM 4 and DSM 5EVFDocumento3 páginasCritically Evaluate The Difference Between DSM 4 and DSM 5EVFNaganajita ChongthamAinda não há avaliações
- DSM 5 - DSM 5Documento7 páginasDSM 5 - DSM 5Roxana ClsAinda não há avaliações
- PSY403 - Ivon Sagita - 1Documento8 páginasPSY403 - Ivon Sagita - 1Muhammad Isnaeni Rizqi WijayaAinda não há avaliações
- DSM5-Reflexion in AutismDocumento7 páginasDSM5-Reflexion in AutismBianca NuberAinda não há avaliações
- Clinical Characteristics of Intellectual Disabilities - Mental Disorders and Disabilities Among Low-Income Children - NCBI BookshelfDocumento6 páginasClinical Characteristics of Intellectual Disabilities - Mental Disorders and Disabilities Among Low-Income Children - NCBI BookshelfArhatya MarsasinaAinda não há avaliações
- CAARS ReviewDocumento7 páginasCAARS ReviewRAMSES REZA RENDONAinda não há avaliações
- Review of Cognitive Characteristics of Autism Spectrum DisorderDocumento14 páginasReview of Cognitive Characteristics of Autism Spectrum DisorderKarel GuevaraAinda não há avaliações
- Le FaivreDocumento7 páginasLe FaivreOtra PersonaAinda não há avaliações
- Beda DSM IV Vs DSM 5Documento19 páginasBeda DSM IV Vs DSM 5strioagung06Ainda não há avaliações
- Opinions of People Who Self-Identify With Autism and Asperger's On DSM-5 CriteriaDocumento11 páginasOpinions of People Who Self-Identify With Autism and Asperger's On DSM-5 CriteriaAndrés SánchezAinda não há avaliações
- A Study of Co-Morbidity in Mental RetardationDocumento9 páginasA Study of Co-Morbidity in Mental RetardationijhrmimsAinda não há avaliações
- Psychodynamic Diagnostic Manual 2nd Edition PDDocumento3 páginasPsychodynamic Diagnostic Manual 2nd Edition PDgustiAinda não há avaliações
- Psychometric Properties of The Personality Inventory For Dsm-5 in A Romanian Community SampleDocumento18 páginasPsychometric Properties of The Personality Inventory For Dsm-5 in A Romanian Community SampleDianaStanciuAinda não há avaliações
- WAISIV LDSQ AuthorDocumento19 páginasWAISIV LDSQ AuthorSudarshana DasguptaAinda não há avaliações
- Cicero,+0210 1696 2021 0052 0003 0029 0036Documento8 páginasCicero,+0210 1696 2021 0052 0003 0029 0036Alba subiñas poloAinda não há avaliações
- Intellectual DevelopmentalDocumento29 páginasIntellectual DevelopmentalAnne de AndradeAinda não há avaliações
- Pauta Discapacidad N&ADocumento29 páginasPauta Discapacidad N&APedro Y. LuyoAinda não há avaliações
- Berghuis Et Al., GAPD CP&P 2012Documento14 páginasBerghuis Et Al., GAPD CP&P 2012Feras ZidiAinda não há avaliações
- ABAS Manual Chapter 1 PDFDocumento14 páginasABAS Manual Chapter 1 PDFTeodora Rusu100% (2)
- Intelligence Measures As Diagnostic Tools For Children With SpecificDocumento6 páginasIntelligence Measures As Diagnostic Tools For Children With Specificjulicosita19Ainda não há avaliações
- For Immediate Release Commentary Takes Issue With Criticism of New Autism DefinitionDocumento2 páginasFor Immediate Release Commentary Takes Issue With Criticism of New Autism DefinitionElyssa DurantAinda não há avaliações
- A Five-Factor Measure of Obsessive-Compulsive Personality Traits PDFDocumento38 páginasA Five-Factor Measure of Obsessive-Compulsive Personality Traits PDFRANJINI.C 20PSY042Ainda não há avaliações
- Personality DisordersDocumento5 páginasPersonality DisordersFabianAinda não há avaliações
- Schema Therapy Conceptualization of Personality Functioning and Traits in ICD-11 and DSM-5Documento13 páginasSchema Therapy Conceptualization of Personality Functioning and Traits in ICD-11 and DSM-5benoitmonchotteAinda não há avaliações
- 10.1.1.627.9556 Millon PDFDocumento12 páginas10.1.1.627.9556 Millon PDFGERMAN ANDRES BARON BONILLA100% (1)
- Foley-Nicpon 2017Documento13 páginasFoley-Nicpon 2017Jennifer TanAinda não há avaliações
- Diagnosis and Treatment of Mental Disorders: An IntroductionNo EverandDiagnosis and Treatment of Mental Disorders: An IntroductionAinda não há avaliações
- The Five-Factor Personality Inventory For ICD-11 - A Facet-Level Assessment of The ICD-11 Trait ModelDocumento38 páginasThe Five-Factor Personality Inventory For ICD-11 - A Facet-Level Assessment of The ICD-11 Trait Modeld55v9x8846Ainda não há avaliações
- An Overview of The DSM-5 Alternative Model of Personality DisordersDocumento7 páginasAn Overview of The DSM-5 Alternative Model of Personality DisordersJosé Ignacio SáezAinda não há avaliações
- Intellectual Development DisordersDocumento9 páginasIntellectual Development DisordersCindy Van WykAinda não há avaliações
- Dale Et Al (2021) WISC-V and AutismDocumento17 páginasDale Et Al (2021) WISC-V and Autismliliana temudo romãoAinda não há avaliações
- A Comparison of WISC-IV and WISC-V VerbalDocumento12 páginasA Comparison of WISC-IV and WISC-V VerbalKarel GuevaraAinda não há avaliações
- Beyond The DSM-IV Assumptions, Alternatives, and Alterations PDFDocumento10 páginasBeyond The DSM-IV Assumptions, Alternatives, and Alterations PDFMira BurovaAinda não há avaliações
- The Psychodynamic Diagnostic Manual Version 2 (PDM-2) : Assessing Patients For Improved Clinical Practice and ResearchDocumento25 páginasThe Psychodynamic Diagnostic Manual Version 2 (PDM-2) : Assessing Patients For Improved Clinical Practice and ResearchSilvia R. AcostaAinda não há avaliações
- Skodol Et Al 2011 Part IIDocumento18 páginasSkodol Et Al 2011 Part IIssanagavAinda não há avaliações
- The Effect of Response Bias On The Personality Inventory For DSMDocumento5 páginasThe Effect of Response Bias On The Personality Inventory For DSMОксана ГриневичAinda não há avaliações
- Adhd MakaleDocumento11 páginasAdhd MakaleNESLİHAN ORALAinda não há avaliações
- CHP 3A10.1007 2F978 1 4419 0234 4 - 8Documento17 páginasCHP 3A10.1007 2F978 1 4419 0234 4 - 8astrimentariAinda não há avaliações
- NIH Public AccessDocumento20 páginasNIH Public AccessMyriam PaquetteAinda não há avaliações
- Subtypes of Psychopathology in Children Referred For Neuropsychological AssessmentDocumento15 páginasSubtypes of Psychopathology in Children Referred For Neuropsychological Assessmentdrake2932Ainda não há avaliações
- Dsm-5 and Autism Spectrum Disorders (Asds) : An Opportunity For Identifying Asd SubtypesDocumento6 páginasDsm-5 and Autism Spectrum Disorders (Asds) : An Opportunity For Identifying Asd SubtypesLuis SeixasAinda não há avaliações
- Research Final Paper-Brenna SchulteDocumento15 páginasResearch Final Paper-Brenna Schulteapi-610116630Ainda não há avaliações
- Neo Ffi DissertationDocumento5 páginasNeo Ffi DissertationWriteMyPaperUK100% (1)
- Chapter 10Documento5 páginasChapter 10Lorie Jane UngabAinda não há avaliações
- D Example-VIT (M, WO)Documento8 páginasD Example-VIT (M, WO)Anonymous q084Nx6FUAinda não há avaliações
- FILE - 20200610 - 183606 - Constructive AlignmentDocumento19 páginasFILE - 20200610 - 183606 - Constructive AlignmentThanh ThanhAinda não há avaliações
- Celie Case StudyDocumento7 páginasCelie Case Studyapi-491868957Ainda não há avaliações
- Problem StatementDocumento2 páginasProblem Statementikx pxndaAinda não há avaliações
- Artigo - Pildes, S. and Moon, K. A. I Didn - T Know You Felt That Way - The Practice of Client-Centered Couple and Family TherapyDocumento10 páginasArtigo - Pildes, S. and Moon, K. A. I Didn - T Know You Felt That Way - The Practice of Client-Centered Couple and Family TherapyGabriel RochaAinda não há avaliações
- 20th Century War PoetryDocumento3 páginas20th Century War Poetryapi-350339852Ainda não há avaliações
- Nielsen, T.Documento10 páginasNielsen, T.Amanda MunizAinda não há avaliações
- MPDF PDFDocumento3 páginasMPDF PDFP'ken ZeeAinda não há avaliações
- Visit ReportDocumento2 páginasVisit ReportGirish Pal100% (3)
- Human Resource ManagementDocumento14 páginasHuman Resource ManagementPuneet BansalAinda não há avaliações
- Creativity FrameworkDocumento18 páginasCreativity FrameworkAshkan AhmadiAinda não há avaliações
- DLL Food-Processing-Sugar-ConcentrationDocumento7 páginasDLL Food-Processing-Sugar-ConcentrationErma Jalem71% (7)
- Types of StressorsDocumento4 páginasTypes of StressorsIceyYamahaAinda não há avaliações
- Competency Based HRM ModuleDocumento4 páginasCompetency Based HRM ModuleErlene LinsanganAinda não há avaliações
- Humss 7 Cur Map Q2Documento7 páginasHumss 7 Cur Map Q2Martie AvancenaAinda não há avaliações
- Rethinking Procrastination: Positive Effects of "Active" Procrastination Behavior On Attitudes and PerformanceDocumento22 páginasRethinking Procrastination: Positive Effects of "Active" Procrastination Behavior On Attitudes and PerformanceJuniii OktavianiAinda não há avaliações
- SAMHSA Psychological Response AidDocumento2 páginasSAMHSA Psychological Response AidAiszellnutAinda não há avaliações
- Maslach Leiter Burnout Stress Concepts Cognition Emotionand BehaviorDocumento5 páginasMaslach Leiter Burnout Stress Concepts Cognition Emotionand BehaviorMOHD SHAHRIZAL CHE JAMEL100% (1)
- Learner Progress Report Card: Name: Tisha Nair Grade: Vii Eins Roll No: 19Documento4 páginasLearner Progress Report Card: Name: Tisha Nair Grade: Vii Eins Roll No: 19Tisha NairAinda não há avaliações
- Mackenzie, G. (2018) - Building Resilience Among Children and Youth With ADHDDocumento18 páginasMackenzie, G. (2018) - Building Resilience Among Children and Youth With ADHDjuanAinda não há avaliações
- Background of The Study FinalDocumento8 páginasBackground of The Study FinalBIEN RUVIC MANEROAinda não há avaliações
- SOSC1960 Discovering Mind and Behavior: Wednesdays & Fridays 1:30 - 2:50 PMDocumento30 páginasSOSC1960 Discovering Mind and Behavior: Wednesdays & Fridays 1:30 - 2:50 PMericlaw02Ainda não há avaliações
- 5043 AssignmentDocumento6 páginas5043 AssignmentFoo Siew YokeAinda não há avaliações
- wk1 Assignment - ch2 Theories of Development Deema Othman 2Documento2 páginaswk1 Assignment - ch2 Theories of Development Deema Othman 2api-385327442Ainda não há avaliações
- Abu Dhabi and Dubai 2020 MFDocumento1 páginaAbu Dhabi and Dubai 2020 MFYaryna Telenko de OvelarAinda não há avaliações
- Summary 2 - PhobiaDocumento2 páginasSummary 2 - PhobiaAmutha Ammu0% (1)
- Soccer Block PlanDocumento2 páginasSoccer Block Planapi-237645751Ainda não há avaliações
- SHS DAILY LESSON LOG (DLL) TEMPLATE (By Ms. Gie Serrano)Documento3 páginasSHS DAILY LESSON LOG (DLL) TEMPLATE (By Ms. Gie Serrano)Irah Rendor SasaAinda não há avaliações
- The 16-Item Maladaptive Daydreaming Scale (MDS-16)Documento3 páginasThe 16-Item Maladaptive Daydreaming Scale (MDS-16)Diogo Desiderati100% (2)