Escolar Documentos
Profissional Documentos
Cultura Documentos
3493 12829 1 PB
Enviado por
Adythya DhenyTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
3493 12829 1 PB
Enviado por
Adythya DhenyDireitos autorais:
Formatos disponíveis
Associated risk factors with ante-partum
intra-uterine fetal death
Lamia A. Shaaban, SBOBGYN,
SBOBGYN MBBS, Rihab A. Al-Saleh, ABOBGYN
ABOBGYN, MBBS,
Buthina M. Alwa, SBOBGYN, MBBS, Rajaa M. Al-Raddadi
Al-Raddadi, M
MBBS, ABCM.
ABSTRACT
Objective: To determine ante-partum maternal risk factors
for intrauterine fetal death.
Methods: We carried out a case control retrospective
study, at the Maternity and Childrens Hospital, Jeddah,
Kingdom of Saudi Arabia. We included all pregnant women
diagnosed as singleton intra-uterine fetal death in the third
trimester with fetal weight of 1500 gm and more, admitted
to the hospital over a 2-year (2001-2002) period (study
group). We examined the following risk factors: diabetes,
hypertension, abruptio-placenta, age, gestational age,
parity, trauma, sepsis, booking, chromosomal abnormality,
previous history of intra-uterine fetal death (IUFD) and
intra-uterine growth restriction (IUGR). We compared
the results to those pregnant women with live pregnancy
admitted before and after each case (control group).
Results: There were 157 cases of singleton IUFD during
that period. The intra-uterine fetal death rate was 10.1
per 1000 deliveries. In 28% of the cases, we could not
determine the associated risk factors. Among cases there
nte-partum intrauterine fetal death (IUFD) is a
major cause of perinatal death.1 A population
based analysis by Cotzias et al2 estimated the risk
of unexplained IUFD at or beyond 38 weeks to be
one in 730 singleton pregnancies. Late fetal deaths
currently comprise at least half of all perinatal deaths
and more than one third of total fetal and infant deaths
were 57.3% (odds ratio [OR] 2.4 95% condence interval
[CI] 1.4-4) lacking antenatal care, cord accident in 56.6%
(OR 5.1% 95 CI 2.7-9.5), 29.3% (OR 5.5 95% CI 2.4-12.6)
hypertension, 26.1% (OR 12.9 95% CI 5.5-30.6) diabetes,
IUGR in 24.8% (OR 1.73% 95% CI 1.1-2.7), 14% (OR
23.4% 95% CI 4.6-119.3) abruption-placenta, and previous
history of IUFD in 8.3% (OR 7.01 95% CI 2.1-23.6). Other
risk factors found were age between 20-30 years in 51.6%,
gestational age between 37-41 weeks in 58.6%, parity
between 0-5 in 77.1%, and chromosomal abnormality in
5.7% (OR 0.91% 95% CI 0.91-0.99).
Conclusion: The identied risk factors for IUFD in our
community appear preventable. We should pay attention to
health education with emphasis on antenatal care and the
benets of regular clinic attendance. Patients compliance
is important in reducing most of these preventable fetal
deaths.
Saudi Med J 2006; Vol. 27 (1): 76-79
in Europe and North America.2 Despite the evident
importance of stillbirth as both a clinical and public
health problem, little attention has focused specically
on the epidemiology of fetal death separately from
neonatal or infant death.2 In the developing countries,
the bulk of intrauterine deaths are intrapartum and
attributed commonly to the avoidable factors.3 In
From the Department of Obstetric and Gynecology (Shaaban, Al-Saleh, Alwa), Maternity and Childrens Hospital, and the Department of Primary
Health Care (Al-Raddadi), Primary Health Care Directorate, Jeddah, Kingdom of Saudi Arabia.
Received 30th April 2005. Accepted for publication in nal form 12th November 2005.
Address correspondence and reprint request to: Dr. Lamia A. Shaaban, Obstetrics and Gynecology Specialist, Maternity and Childrens Hospital, PO
Box 13877, Jeddah 21414, Kingdom of Saudi Arabia. Tel. +966 (2) 6673818/6670508. Fax. +966 (2) 6613667. E-mail: lmlm63@hotmail.com.
76
Ante-partum intra-uterine fetal death ... Shaaban et al
contrast, stillbirth in developed countries is largely
ante-partum with no apparent cause.3 Many fetal
deaths can be attributed to maternal disorders, such
as diabetes or hypertensive disease, to fetal pathology
such as congenital anomalies, severe fetal growth
restriction (FGR) or cord accident, and to placental
pathology such as abruptio placenta.4 For the purpose
of our study, we dened IUFD as delivery of a dead
fetus weighing 1500 gm or more. The IUFD rate is
the number of IUFD per 1000 deliveries. This study
attempts to determine associated maternal and fetal
risk factors to IUFD.
Methods. A case control retrospective study, in the
Maternity and Childrens Hospital, Jeddah, Kingdom
of Saudi Arabia included all pregnant women admitted
to the hospital with a diagnosis of singleton IUFD at
the third trimester with a fetal weight of 1500 gm and
more. Multiple pregnancy and intra-partum IUFD
were excluded. The control group was all pregnant
women admitted to the hospital with a singleton live
birth before and after each case. A questionnaire was
structured, completed by reviewing the patient, and
the missing data obtained from the le of the patient.
As a hospital policy, the neonatologist examines
all IUFD. No autopsy was performed on any of the
infants. The data were entered and analyzed using the
Statistical Package for Social Sciences version 10.
Continuous variables were summarized as means and
standard deviation (SD), and categorical variables by
frequency and percentage. Multiple logistic regression
was used to assess the relation between IUFD and all
risk factors.
Results. Total number of deliveries was 16562,
with 157 cases of IUFD in that period, giving a rate
of 10.1 per 1000 deliveries. In 28% of the cases, the
associated risk factors could not be determined. The
mean maternal age was 30.3 6.5 for cases, and 28.4
6.4 for control, which is not signicant. Table 1
shows the risk factors among cases and control with
multiple logistic regression. Fetal trauma, hydrops,
placental weight, fetal presentation and sex, color of
the liquor, length of the cord and sepsis were found
not signicant among both group.
Discussion. The incidence of IUFD is variable
among different centers.3,5-9 Even locally, the incidence
is variable in different regions of the country. Maternal
conditions such as poorly controlled diabetes mellitus,
hypertension either chronic or pre-eclampsia were
more associated with poor outcome,1,3,6,7,9,10 also in
accordance with other studies.3,5,6,9,10 These problems
can be controlled to some extent if a good antenatal
care service is provided. A past history of IUFD
was more common in our cases. This may indicate
some sub clinical genetic or chromosomal problems,
which can recur in future pregnancies. The role of
bad obstetric history was variable in the literature.1,8,11
It was noticed to most affected women in their 3rd
Table 1 - Characteristic of the study group.
Number of patients (%)
Risk factors
Cases
Diabetes mellitus
Hypertension
Abruptio-placenta
Un-booked
Cord accident
Congenital anomaly
Parity
(0-5)
(6-10)
(>10)
Gestational age
(27-31)
(32-36)
(37-41)
(>41)
Intrauterine growth restriction
Previous IUFD
Age
(<20)
(20-30)
(31-40)
(>40)
IUFD
Control
41
46
22
90
47
9
(26.1)
(29.3)
(14)
(57.3)
(56.6)
(5.7)
10
15
2
130
36
0
(3.2)
(4.8)
(0.6)
(41.4)
(43.4)
0
0.000
0.000
0.000
0.001
0.000
0.000
121
34
2
(77.1)
(21.7)
(1.3)
268
44
2
(85.4)
(14)
(0.6)
0.08
16
41
92
8
39
13
(10.2)
(26.1)
(58.6)
(5.1)
(24.8)
(8.3)
3
22
275
14
50
6
(1)
(7.)
(87.6)
(4.5)
(16)
(1.9)
0.000
7
81
61
8
(4.5)
(51.6)
(38.9)
(5.1)
19
202
82
11
(6.1)
(64.3)
(26.1)
(3.5)
0.023
0.022
0.001
OR
CI 95%
12.9
5.5
23.4
2.4
5.1
5.5-30.6
2.4-12.6
4.6-119.3
1.4-4
2.7-9.5
7.01
2.1-23.6
OR - odd ratio, CI - condence interval, IUFD - ante-partum intrauterine fetal death
www.smj.org.sa
Saudi Med J 2006; Vol. 27 (1)
77
Ante-partum intra-uterine fetal death ... Shaaban et al
decade, indicating that most of the affected cases are
relatively young. However, this differs in comparison
to the western community, where the problem was
in elderly women.6,11 This can be explained to some
extent by better antenatal care services for which
high-risk conditions were picked up and treated early.
The effect of nulliparity was variable in different
studies.10 Our results showed risk to be higher in
low parity women, compared to the Abha and Hofuf
group, where grand multiparous women had a higher
incidence of IUFD.3,9
The availability of antenatal care is the corner
stone for identifying high-risk cases and therefore for
providing specialized care, and eventually to reduce
complications. Absence of antenatal care was more
prevalent in IUFD cases, in accordance with other
studies.8,9 It was interesting to nd that most of our
IUFD cases have some associated problem, and only
28% were unexplained. This observation warrants
detailed multi-center studies to look for a causative
relationship, if any. In the literature, the incidence of
unexplained IUFD is much higher, although autopsy
is practiced in some centers.1,4,5,8,12
The difference in placental weight in cases
and control was almost negligible. It may indicate
absence of a co-relationship between function of
placenta and its actual size. Congenital malformation
is a known risk factor for IUFD and neonatal death. It
is well documented that there are some defects, which
cannot be detected by routine antenatal ultrasound,
and are discovered at delivery.12 The incidence of
congenital anomaly was higher in the Abha and
Hofuf group when compared to ours.3,9 However,
regression analysis did not support this nding in
our work. Intra uterine growth retardation is a known
associated complication for a number of congenital
and chromosomal disorders. It was more prevalent
in cases compared to control. A bias may have taken
place because the gestational age given to IUFD cases
is the date of delivery not the actual date of death.6,8,12
In the Abha study, it was interesting to notice that
most of the affected cases were of more than 2500 gm
indicating that they were appropriate for gestational
age.
Acute incidents such as abruption and cord accident
were more common in IUFD cases. That would
explain the loss of healthy fetuses in utero.1 It was
noticed that most of our fetuses were lost at 37 weeks
and beyond. It may indicate that uterine conditions
become hostile at that phase. It is recommended to
apply closer surveillance at 37 weeks and beyond,
so that fetuses will not be lost at that critical period.7
78
Saudi Med J 2006; Vol. 27 (1)
www.smj.org.sa
The critical peak at which fetuses were lost is variable
in the literature.1,3,7,9,10,11,13 This may indicate the
predisposing pathology for IUFD in our unit different
compared to others.
In conclusion, the associated risk factors in our
community seem to be preventable. We should
pay attention to health education with emphasis on
antenatal care and the benet of regular attendance.
Patient compliance is important in reducing most of
these preventable fetal losses.
Acknowledgment. We would like to thank the Department
of Obstetrics and Gynecology and the Record Department,
Maternity and Childrens Hospital, Jeddah, Saudi Arabia for
helping us do this study; Special thanks to Dr. Rajaa for her great
help and for Dr. Nasser Mustafa Khbaz for the translation. In
addition, we thank Dr. Fredrick Makoha (Consultant Obstetrics
and Gynecology in MCH), and Dr. Ezzeldin Ibrahim (Chairman,
Department of Oncology, Deputy Executive Director, King Faisal
Specialist Hospital and Research Center, Jeddah) for reviewing
our research.
References
1. Shankar M, Navti O, Amu O, Konjel JC. Assessment of still
birth risk and associated risk factors in a tertiary hospital. J
Obstet Gynaecol 2002; 22: 34-38.
2. Cotzias CS, Paterson-Brown S, Fisk MN. Prospective of
unexplained stillbirth in singleton pregnancies at term:
Population based analysis. BMJ 1999; 319:287-288.
3. Archibong EI, Sobande AA, Asindi AA. Antenatal intrauterine
fetal death; A prospective study in a tertiary hospital in
Western Saudi Arabia. J Obstet Gynaecol
Gynaecol2003; 23: 170-173.
4. Huang DY, Usher RH, Kramer MS, Yang H, Morin L, Fretts
RC. Determinants of unexplained ante-partum fetal death. J
Obstet Gynaecol 2000; 95: 215-221.
5. Rasmussen S, Albrechtsen S, Irgens LM, Dalaker K,
Martmann-Moe H, Vlatkovic L, et al. Unexplained antepartum fetal death in Norway, 1985-97. Diagnostic validation
and some epidemiology aspects. Acta Obstet Gynecol 2003;
82: 109-115.
6. Ratmond EG, Cnattingius S, Kiely JL. Effects of maternal
age parity and smoking on the risk of stillbirth. Br J Obstet
Gynaecol 1994; 101: 301-306.
7. Smulian JC, Ananth CV, Vintzileos AM, Scorza, Knuppel
RA, et al. Fetal death in the United States. Inuence of high
risk conditions and implication for management. Obstet
Gynecol 2002; 100: 1183-11891.
8. Maleckiene L, Nadisauskiene R, Bergstrom S. Socioeconomic,
demographic and obstetric risk for late fetal deaths of
unknown etiology in Lithuania: A case-referent study. Acta
Obstet Gynecol Scand 2001; 80: 321-325.
9. Ogbonna BN, Sumra S, Zeyadha E, Bakhurji E. A review of
late fetal deaths in Alhassa: A retrospective study. Ann Saudi
Med 1989; 9: 561-565.
Ante-partum intra-uterine fetal death ... Shaaban et al
10. Copper RL, Goldenberg RL, DuBard MB, Davis RO. Risk
factors for fetal deaths in white black and Hispanic women.
Collaborative Group on Preterm Birth Prevention. Obstet
Gynecol 1994; 84: 490-495.
11. Froen JF, Arnestad M, Frey K, Vege A, Saugstad OD,
Stray-Pedersen B, et al. Risk factors for sudden intrauterine
un-explained fetal death: Epidemiologic characteristics of
singleton cases in Oslo, Norway, 1986-1995: Am J Obstet
Gynecol 2001; 184:649-702.
12. Incarpi MH, Miller DA, Samodi R, Settlage RH, Goodwin
TM. Stillbirth evaluation: What tests are needed? AMJ
Obstet Gynecol 1998; 178:1121-1125.
13. Alberman E, Blatchley N, Botting B, Schuman J, Dunn
A. Medical causes on stillbirth certicates in England and
Wales: Distribution and results of Hierarchal classications
tested by the ofce for National statistics. BJOG 1997; 104:
1043-1049.
www.smj.org.sa
Saudi Med J 2006; Vol. 27 (1)
79
Você também pode gostar
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Female Reproductive OrgansDocumento42 páginasFemale Reproductive Organsaliyah nerz83% (6)
- Uterine FibroidsDocumento21 páginasUterine FibroidsPrasun BiswasAinda não há avaliações
- Nursing Care Plan For Ineffective Breastfeeding NCPDocumento4 páginasNursing Care Plan For Ineffective Breastfeeding NCPderic76% (46)
- Obstetrical Nursing BUBBLE SHE Assessment - Postpartum NCPDocumento3 páginasObstetrical Nursing BUBBLE SHE Assessment - Postpartum NCPFranz goAinda não há avaliações
- Endometrial HyperplasiaDocumento21 páginasEndometrial Hyperplasianautilus81Ainda não há avaliações
- Post Partum Hemorrhage (PPH)Documento77 páginasPost Partum Hemorrhage (PPH)Aparna LaxmanAinda não há avaliações
- Science 5 DLP 3 - PubertyDocumento8 páginasScience 5 DLP 3 - PubertyMark Cua100% (4)
- Family Planning - A Global Handbook For Providers PDFDocumento460 páginasFamily Planning - A Global Handbook For Providers PDFJemie Dagadas100% (1)
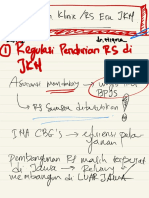
- Seminar Pembangunan Klinik - Rs Era JKNDocumento13 páginasSeminar Pembangunan Klinik - Rs Era JKNAdythya DhenyAinda não há avaliações
- Update 14 - EPI-WIN - COVID19Documento17 páginasUpdate 14 - EPI-WIN - COVID19Adythya DhenyAinda não há avaliações
- # 4 Kreativitas Dan InovasiDocumento95 páginas# 4 Kreativitas Dan InovasiAdythya DhenyAinda não há avaliações
- SdfisadpufiDocumento1 páginaSdfisadpufiAdythya DhenyAinda não há avaliações
- Duty Report Alul Anemia Gravis CA MammaeDocumento5 páginasDuty Report Alul Anemia Gravis CA MammaeAdythya DhenyAinda não há avaliações
- Jadwal Stase IntermediateDocumento2 páginasJadwal Stase IntermediateAdythya DhenyAinda não há avaliações
- W9eqvs 3Documento2 páginasW9eqvs 3Adythya DhenyAinda não há avaliações
- Modul 4Documento12 páginasModul 4ImaIkrimahAinda não há avaliações
- LEGAL MEDICINE: VIRGINITY AND DEFLORATIONDocumento17 páginasLEGAL MEDICINE: VIRGINITY AND DEFLORATIONAllan Jay Manoddom EbelanAinda não há avaliações
- Knowledge of nursing students on polycystic ovarian syndromeDocumento80 páginasKnowledge of nursing students on polycystic ovarian syndromeDiksh JindeAinda não há avaliações
- Factors Associated with Severe Postpartum HemorrhageDocumento27 páginasFactors Associated with Severe Postpartum HemorrhageCory Monica MarpaungAinda não há avaliações
- Recapturing The Art of Therapeutic Breast Massage During BreastfeedingDocumento4 páginasRecapturing The Art of Therapeutic Breast Massage During BreastfeedingwladjaAinda não há avaliações
- Pi Is 0015028208033050Documento17 páginasPi Is 0015028208033050Annisa YutamiAinda não há avaliações
- Jurnal Kuda 1Documento21 páginasJurnal Kuda 1Yulistia FadhilahAinda não há avaliações
- CertificatesDocumento13 páginasCertificatesbkmurthy78100% (1)
- Mauritius MNCH HandbookDocumento66 páginasMauritius MNCH Handbooknevin KhedooAinda não há avaliações
- Ob - Operative ObstetricsDocumento224 páginasOb - Operative Obstetricsapi-385605133% (3)
- Form F Registration RecordDocumento2 páginasForm F Registration RecordArchit ChampanekarAinda não há avaliações
- A Complete Vaginal Discharge Color GuideDocumento3 páginasA Complete Vaginal Discharge Color GuideAmna SerafAinda não há avaliações
- Ajibola Swep PresentationDocumento15 páginasAjibola Swep PresentationBabatunde AjibolaAinda não há avaliações
- Everything You Need to Know About the Menstrual CycleDocumento16 páginasEverything You Need to Know About the Menstrual CycleCoxnxkAinda não há avaliações
- Anatomi Reproduksi WanitaDocumento23 páginasAnatomi Reproduksi WanitaocepAinda não há avaliações
- Real Sex: A Safe Sex Guide For TeensDocumento9 páginasReal Sex: A Safe Sex Guide For TeensLilly CrumpAinda não há avaliações
- M. Preterm and Postterm - NewDocumento92 páginasM. Preterm and Postterm - NewTry Ariditya UtomoAinda não há avaliações
- Keywords: Fetal Distress, Cesarean Section, Artificial Rupture of Membrane, Placenta Abruption, Syphilis in Pregnancy Case SummaryDocumento38 páginasKeywords: Fetal Distress, Cesarean Section, Artificial Rupture of Membrane, Placenta Abruption, Syphilis in Pregnancy Case SummaryooijinshengAinda não há avaliações
- Metformin Use in Women With Polycystic Ovary Syndrome: Neil P. JohnsonDocumento6 páginasMetformin Use in Women With Polycystic Ovary Syndrome: Neil P. JohnsonanyAinda não há avaliações
- Preterm LaborDocumento41 páginasPreterm LaborAdistri Kim100% (3)
- Step-by-Step Approach For Nerve-Sparing Reduction ClitoroplastyDocumento1 páginaStep-by-Step Approach For Nerve-Sparing Reduction ClitoroplastyKevin YonathanAinda não há avaliações
- Preterm Labour and PROMDocumento25 páginasPreterm Labour and PROMNinaAinda não há avaliações
- Delivery of TwinsDocumento25 páginasDelivery of TwinsCakraEkkyAinda não há avaliações