Escolar Documentos
Profissional Documentos
Cultura Documentos
Algorithms 08 00395
Enviado por
venkayammaDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Algorithms 08 00395
Enviado por
venkayammaDireitos autorais:
Formatos disponíveis
Algorithms 2015, 8, 395-406; doi:10.
3390/a8030395
OPEN ACCESS
algorithms
ISSN 1999-4893
www.mdpi.com/journal/algorithms
Review
Algorithms for Computerized Fetal Heart Rate Diagnosis with
Direct Reporting
Kazuo Maeda 1,*, Yasuaki Noguchi 2, Masaji Utsu 3 and Takashi Nagassawa 4
1
Department of Obstetrics and Gynecology (Emeritus), Tottori University Medical School, 3-125,
Nadamachi, Yonago, Tottoriken 683-0835, Japan
Department of Applied Physics, National Defence Academy, Yokosuka, 239-0811 Japan;
E-Mail: noguchiy@nda.ac.jp
Department of Obstetrics and Gynecology, Seirei Mikatahara Hospital, Hamamatsu 433-8558,
Japan; E-Mail: utsu-og@sis.seirei.or.jp
Department of Information Technology, TOITU Ltd., Tokyo144-0033, Japan;
E-Mail: nagasawa@toitu.co.jp
* Author to whom correspondence should be addressed; E-Mail: maedak@mocha.ocn.ne.jp;
Tel./Fax: +81-859-22-6856.
Academic Editor: Tak-Wah Lam
Received: 28 May 2015 / Accepted: 15 June 2015 / Published: 29 June 2015
Abstract: Aims: Since pattern classification of fetal heart rate (FHR) was subjective and
enlarged interobserver difference, objective FHR analysis was achieved with computerized
FHR diagnosis. Methods: The computer algorithm was composed of an experts knowledge
system, including FHR analysis and FHR score calculation, and also of an objective artificial
neural network system with software. In addition, a FHR frequency spectrum was studied to
detect ominous sinusoidal FHR and the loss of baseline variability related to fetal brain
damage. The algorithms were installed in a central-computerized automatic FHR monitoring
system, which gave the diagnosis rapidly and directly to the attending doctor. Results:
Clinically perinatal mortality decreased significantly and no cerebral palsy developed after
introduction of the centralized system. Conclusion: The automatic multichannel FHR
monitoring system improved the monitoring, increased the objectivity of FHR diagnosis and
promoted clinical results.
Algorithms 2015, 8
396
Keywords: fetus; heart rate; fetal movement; experts knowledge system; artificial neural
network system; frequency analysis; algorithm
1. Introduction
Fetal heart rate (FHR) and uterine contractions were continuously traced with a cardiotocogram
(CTG), and the recorded chart was visually classified into various patterns; then, abnormal FHR patterns
were individually assessed in each case, where the diagnosis was subjective and enlarged inter-observer
difference, and therefore various problems developed in the CTG diagnosis. In addition, visual FHR
pattern diagnosis was unable to apply computerized diagnosis because of no logical criteria, e.g., no lag
time of late deceleration was reported by Hon [1]. Later, Chik et al. [2] estimated it to be 20 or more
seconds. Therefore, FHR diagnosis was computerized to quantitatively analyze FHR changes in an
experts knowledge system, artificial neural network analysis, and FHR frequency spectrum analysis [37].
Meanwhile, our recent studies on fetal movements with actocardiogram (ACG) [8] solved several CTG
problems, e.g., a physiologic sinusoidal FHR was unable to differentiate a fatal pathologic sinusoidal
condition with CTG, while they were separated when a physiologic sinusoidal condition was developed
by fetal periodic respiratory or mouthing movements in the ACG [9]. Artificial birth was recommended
before the loss of variability, because FHR variability is the response of the fetal brain to minor fetal
movements, and its loss will mean fetal brain damage preceding cerebral palsy [1012].
Maeda et al. reported computerized FHR diagnosis using a minicomputer in 1980, on the FHR
analysis and FHR score calculation with quantified FHR data, challenging the objective FHR
diagnosis [3,4], and furthermore reported artificial neural network computer diagnosis of FHR in 1998,
calculating probabilities to be normal, suspicious and pathologic to the outcome of the fetus [5].
Pathologic ominous sinusoidal FHR was diagnosed using an actocardiogram [9] and also by the
computer using frequency spectral analysis [6]. The loss of FHR variability was detected with the
experts knowledge system [3,4] and the frequency spectoral computer system [7]. Chudek et al.
analyzed FHR using the computer in fetal heart rate fractal analysis in 2004 [13], Dawes et al. studied
FHR changes and its variability in pregnancy and labor [14], Georgieva et al. studied FHR in labor in
2011 [15], Jezewski et al. analyzed FHR using the neural network approach in 2007 [16], and
Signorini et al. studied FHR using signal processing and wearable technology in 2014 [17].
FHR monitoring was confused by subjective FHR pattern diagnosis in the past and solved by
quantitative studies as follows.
1.1. Bradycardia
There was severe fetal bradycardia in a fetal cardiac sick sinus case, where reactive acceleration was
present against fetal movements, and the A/B ratio was high in the ACG, resulting in a healthy neonate
without asphyxia [18]. Since the acceleration was responsive to excitation of the healthy fetal brain to
fetal movement, this demonstrated healthy fetal state. As the bradycardia has a positive response to low
PaO2, there is no sign of hypoxic fetal brain damage.
Algorithms 2015, 8
397
1.2. Transient FHR Decrease (Deceleration)
1.2.1. Variable Deceleration
Mild to variable deceleration was the vagal reflex to umbilical cord compression, but not transient
hypoxia, while a severely variable condition was hypoxia in the past, namely, a variable deceleration
was thought to be vagal reflex and another was hypoxia in the past. The author estimated the nadir FHR
to be at PaO2 level at present.
1.2.2. Uniform Deceleration (Late decelerations)
Its lag time was 20 or more sec [1], but Hon reported no lag time in his pattern definition. Its outcome
was reported to be ominous, however, Apgar was 9 in a case of late deceleration, where the A/B ratio of
acceleration was >1 in ACG. Although late deceleration was ominous even though it was shallow
according to Hon, shallow deceleration would be recognized when the baseline variability was lost,
which might cause an ominous outcome. Although late deceleration was caused by placental
insufficiency by Hon, false positive results were experienced in clinical cases to bring confusion in the
pattern diagnosis.
1.3. Transient FHR Increase (Acceleration)
Its disappearance from fetal movement (non-reactive FHR) was the first FHR sign in fetal hypoxia,
i.e., hypoxia suppresses mid-brain function, which develops acceleration by the stimulation of fetal
movement burst, while baseline variability is preserved until severely advanced hypoxia [12].
1.4. The Loss of FHR Variability
FHR baseline variability will develop as the response of the mid-brain to minor fetal movements, and
finally disappeared in the severe hypoxia possibly due to fetal brain damage. It is recommended,
therefore, to perform rapid delivery before the loss of variability to reduce cerebral palsy, instead of
cesarean section after the loss of variability [1012]. As decreased variability, the loss of acceleration,
severe NRFS, and a high hypoxia index would precede the loss of variability, rapid delivery should be
performed according the appearance of these signs.
1.5. Sinusoidal FHR
Although true fatal pathologic sinusoidal FHR and a benign favorable physiologic sinusoidal
condition should be differentiated, the two sinusoidal conditions could not be differentiated with CTG.
Fortunately, periodic fetal movements in fetal periodic respiration or mouth movements developed
physiologic sinusoidal (Figure 1) [9], but no fetal movement was associated to the pathologic one in
ACG. Thus, two sinusoidal FHR cases were collected to find the difference of frequency spectrum
between two sinusoidal HR only using fetal heart rate, then they were quantitatively diagnosed with
computer in clinical automatic FHR diagnosis in the present paper [6].
Algorithms 2015, 8
398
7S
delay
Envelop of periodic fetal respiratory
Figure 1. The most upper line is a benign physiologic sinusoidal fetal heart rate (FHR),
which synchronizes to the envelope of periodic fetal respiratory movements of the second
and third lines recorded by actocardiogram (ACG). Since the outcome of physiologic
sinusoidal FHR was favorable, it should be separated from pathologic fatal sinusoidal FHR;
however, it was unable to be analyzed by CTG, while it was able as above using the
ACG [9], where FHR change was parallel to the height of fetal movement spikes. Since
frequency spectrum of both sinusoidal FHR diagnosed by ACG were characteristic,
pathologic sinusoidal FHR was diagnosed using the frequency spectrum in computer
analysis. Outcome probability was 100% pathologic after input of the presence of pathologic
sinusoidal FHR into educated neural network computer.
2. Methods
Personal data of the patient and the phone number of attending doctor were registered at the top of
the FHR along with contraction data, which were transferred to the computer center through a telemetry
or local area network (LAN). The computer input was composed of an 100 channels time sharing system
to handle the data of multiple births. After A to D conversion every 5 min, 150 data items were
continuously obtained in FHR and contraction. Actocardiogram data will be handled in the future.
Original data was saved in a large external memory to be reproduced on demand.
3. Experts Knowledge System
Computer processing was started from the calculation of baseline FHR, FHR accelerations, FHR
decelerations, FHR variability, and differentiation of late/early and variable decelerations. An objective
FHR score was determined using values of FHR deceleration elements, baseline FHR, and
acceleration [4]. Our FHR analyzing algorithms were composed of FHR curve analysis and FHR score
calculation. Fetal outcome probability was estimated by the neural network system using FHR
parameters, diagnosis of pathologic sinusoidal FHR and the loss of FHR variability. No CTG chart was
traced but original signals are saved in a large memory and the CTG chart is output as the computer hard
Algorithms 2015, 8
399
copy on demand. Summary of the fetal monitoring was saved in the computer memory and patient
record, as well as sent to the attending doctor or any responsible department.
3.1. Detection of FHR Baseline
FHR and contraction curves were sampled four times per 1 s and averaged at 2 s, constructing two
data groups of each 150 data in 5 min. The number of FHR data was counted every 20 bpm steps, and
the average of FHR data in the step of maximal number of FHR data was determined as the baseline
FHR in 5 min. Acceleration was determined, if its amplitude was 15 or more bpm and the duration was
15 or more sec above the upper reference line, which was the sum of baseline FHR and half mean FHR
variation. Deceleration (dip) was determined if the FHR decreased more than 15 bpm than the lower
reference line and longer than 15 s. The number of accelerations and decelerations were counted
in 5 min.
3.2. Late and Variable Decelerations
It was determined to be late deceleration if the DIP SHAPE value (dip area / [the dip duration dip
amplitude]) was <0.5, where the lag time between FHR nadir and contraction peak was >20 s, and the
sum of each FHR data difference (dip variability) <60 bpm, and the dip number was >contraction
number-1 in 15 min. A variable deceleration was determined, if the DIP SHAPE was >0.6, and dip
variability >60 bpm in a dip [3].
3.3. FHR Score
Baseline FHR and decelerations were quantitatively analyzed in 5 min, and the following data were
utilized to calculate the FHR score: baseline FHR (bpm), dip duration (min), dip amplitude (bpm), nadir
FHR (bpm), recovery time (sec) to return baseline, lag time (bpm), and the presence of acceleration. The
work looks complicated in visual analysis, but it was easy in computer analysis (Figure 2) [3].
Figure 2. Quantified analysis of FHR changes for computerized experts knowledge
system [3]. Each deceleration was analyzed if there were multiple decelerations in 5 min,
where sum of the scores of all decelerations were the FHR score in 5 min. The items of above
analysis was evaluated by the evaluation score determined by the percentage of low Apgar
score lower than 7, i.e., it was four points when low Apgar appeared in 100% of that FHR
change, three points if low Apgar was 70%, two points for 40% and one point for 20%
(Table 1). A statistician allowed the evaluation as a goodness score. The sum of evaluation
scores in 5 min was the FHR score.
Algorithms 2015, 8
400
Fetal state was abnormal if the FHR score was 1019, and highly abnormal if the score was 20 or
more. The FHR score was comprehensive evaluation of fetal status [11].
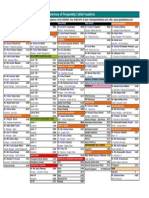
Table 1. Evaluation scores to be given each FHR abnormalities [4].
FHR Abnormality
Baseline FHR 160-180 or 130-110
>180 or <110
Deceleration duration > 60 s
nadir heart rate < 100 bpm
amplitude > 50 bpm
lag time > 40 s
recovery time > 40 s
no acceleration
W-shape without variability
Apgar <7 (%)
28
71
71
37
50
71
63
45
100
Evaluation Score
1
3
3
2
2
3
3
2
4
Sum of all evaluation scores was FHR score.
The FHR score in the first stage of labor (X) correlated to 1 min Apgar score (Y) and umbilical arterial
blood pH (Z). Regression equations were;
Y = 9.361 0.335X, R2 = 0.84, p < 0.05
Z = 7.31 0.01X, R2 = 0.85, p = 0.024 [4].
As expected Apgar score = 4 (severe asphyxia) and pH = 7.16, if FHR score was 15 according to
regression equations, rapid delivery will be indicated to avoid fetal or neonatal compromise if the FHR
score was high [4].
The down-hill amplitudes (bpm) of each long term variability were measured and averaged. The
averaged variability <5 bpm was reported as reduced variability, and <1 bpm was loss of variability.
Frequency spectrum analysis also detected the loss of variability [7].
4. Artificial Neural Network Analysis
Since artificial neural network analysis was more objective than the experts knowledge system, it
was added to our computerized FHR diagnosis to confirm the results obtained using the FHR score in
the experts knowledge system.
The network software of Noguchi, composed of 40 units in the input layer, 30 units in the intermediate
layer, three units in the output layer and a back-propagation system, was trained with eight FHR data
including baseline FHR, the presence of sinusoidal FHR [3,7], variability amplitude, number of
decelerations, its duration, nadir heart rate, recovery time to baseline, lag time from contraction peak, and
fetal outcome (normal = 1, suspicious = 2, pathologic = 3), for 10,000 times until the output outcome was
correct in the internal check. Eight FHR data were utilized to economize the time of computer diagnosis
instead to use total FHR data. Educated software was installed in the diagnostic computer, where eight
new FHR data of parturient women were input into the trained network for the diagnosis. The neural
computer output was the percentage of fetal outcome probability to be normal, suspicious and
pathologic. The results were compared to the FHR score, where both results were coincided [5]. New
Algorithms 2015, 8
401
cases of known outcome were analyzed with the network system, where the clinical outcome of the
fetuses coincided to the output of neural computer [5].
5. Frequency Spectrum Analysis of FHR
5.1. Materials and Methods
Although physiologic sinusoidal FHR was separated from pathologic one by the synchronization of
periodically changing fetal movements in actocardiogram [9], frequency spectrum of FHR trace was
studied in the present report, instead of the use of actocardiogram, because only FHR data was handled
in our computer diagnosis [6].
Nine cases of pathologic sinusoidal FHR were diagnosed by clinical conditions and ACG, including
an anemic Rh-incompatibility, 3 feto-maternal transfusions, an anemic Parbo B-19 infection and
4 NRFS, which were used as pathologic sinusoidal cases, and 12 control cases where 7 were clinically
benign by ACG confirmed physiologic sinusoidal FHR and 5 normal FHR. Both groups were compared
using the frequency spectrum parameters [6].
5.2. Results and Conclusion of Sinusoidal FHR Diagnosis
The ratio of the area under 0.03125 to 0.1 Hz, which was common low frequency area in the heart
rate frequency spectrum analysis, to the area under total spectrum (La/Ta) of pathologic sinusoidal FHR
was >39% and also the peak power spectrum density (PPSD) was >300 bpm2/Hz, while the two
parameters showed lower values in the control cases.
Thus, it was concluded that it was pathologic sinusoidal FHR, when both La/Ta > 39% and PPSD
>300 bpm2/Hz, and it was physiologic pseudo-sinusoidal FHR, when one or both parameter values were
lower than the above values [6].
5.3. The Loss of Variability
The experts system computer diagnosed the loss of long term variability when the mean amplitude
of LTV was <1 bpm. In addition, the loss of variability was diagnosed, if the La/Ta ratio < 15% and
PPSD < 60 bpm2/Hz, in the frequency spectrum analysis of FHR baseline [7].
Since FHR variability developed by the response of fetal brain to minor fetal movements, the loss of
FHR variability could be the sign of general damage of fetal brain. Thus, it would be recommended to
perform rapid delivery, such as a cesarean section, before the loss of variability to reduce cerebral
palsy [1012], instead of cesarean section after the loss of variability. It was important, therefore, to
alarm the states before the loss of variability, which would be reduced variability <5 bpm, severe
bradycardia, severe late decelerations lasting >15 min, repeated severe variable decelerations, prolonged
deceleration >2 min, loss of acceleration, high hypoxia index (sum of <110 bpm bradycardia
duration (min) 100/nadir bradycardia) tentatively as 2024 [12].
There will be institutions, which performed cesarean section by the signs before the loss of variability
listed here with the purpose to improve perinatal state, and experienced the reduction of CP. That was
natural according to the theory in the present report.
Algorithms 2015, 8
402
6. Central Computerized Automatic Fetal Monitoring System (TOITU Central Station Monitor
MF-7400A20W) (Tokyo) [19]
6.1. Data Input
FHR and uterine contraction signals were transferred by the local area network or radio wave
telemetry to the central computer system, where the 100 channel time sharing system accepts multiple
case signals in a non-fault computer system, preparing many simultaneous deliveries. There was no FHR
chart recorder, instead original data are saved in a large memory to replay the FHR curve and output its
hard copy on demand. The phone number of attending doctor was memorized in the data to inform the doctor
of analyzed results.
6.2. Computer Processing
The central computer program was composed of an experts knowledge system to determine the FHR
score and detect FHR elements, and an artificial neural network system to output outcome probabilities
to be normal, suspicious and pathologic. FHR frequency spectrum analysis reported the diagnosis of
pathologic sinusoidal FHR and the loss of variability.
6.3. Direct Report to Attending Doctor
Pathologic results obtained by the computer system were immediately and directly reported to the
attending doctor, responsible departments and on the electronic patient record, to perform various
treatments for the prevention of fetal compromise, by cellular phone, PC or similar mobile data terminal
using registered address at the input of fetal data. The contents of direct information are listed in
Table 2.
Table 2. Direct information items of fetal abnormalities to attending doctor.
Bradycardia < 110, tachycardia > 180 (bpm) #,
Reduced FHR variability < 5 bpm #
The loss of variability #
Pathologic sinusoidal FHR #
Loss of acceleration
Severe variable deceleration #
Prolonged deceleration>2 min #
Late decelerations > 15 min #
FHR score >10 #
Pathologic outcome probability >30% #
A/B ratio (sum of acceleration duration ratio/fetal movement burst duration) < 1.0 *
#
nonreassuring fetal state (NRFS); * Future actocardiographic data.
6.4. Clinical Improvements by the Use of Centralized Computer System
Perinatal mortality was significantly reduced compared to the previous computer system without a
rapid and direct reporting system, and no cerebral palsy developed, using the central fetal monitoring
Algorithms 2015, 8
403
computer system of the present report, at Seirei Mikatahara hospital (Table 3) [19]. Computerized FHR
monitoring was useful not only for the convenience of attending doctor but also for the objective and
rapid detection of fetal abnormality, to prevent fetal demise and cerebral palsy caused by fetal brain
damage in the pregnancy and labor.
Table 3. Improved clinical results compared to the previous computer system [18].
20092011
Present system with direct
alarm
1,767
significant reduction - 1.1
0
19962009
Previous central system
Number of births
Perinatal mortality*
Cerebral palsy rate in 1000 births
10,346
5.5 1.0**
* Perinatal mortality in 19962009: 6.74.2 in Japan [20]; ** Cerebral palsy in Tottori, Japan after wide use
of CTG: 1.0/1000 births [21].
6.5. Computerized Diagnosis of Actocardiogram
The actocardiographic fetal movement spike signal data of normal pregnancy were introduced into a
computer and fetal active, intermediate and resting states were automatically determined using the spike
handling algorithm (Figure 3), where the undeterminable result was intermediate fetal state [21].
Figure 3. The algorithm to automatically define fetal behavioral states into active and resting
states. Undeterminable state was intermediate fetal state [22].
Fetal behavioral states were unstable in the periods before 34 weeks of gestation, and stabilized after
36 weeks in the computerized analysis using fetal movement signals (Figure 3). Fetal hiccupping,
non-reactive FHR (no acceleration against fetal movement), physiologic and pathologic sinusoidal FHR,
Algorithms 2015, 8
404
abnormal fetal behavior, etc., will be automatically detected by the automatic actocardiographic signal
analysis in the future.
The percentages of three behavioral states were calculated in four pregnancy periods at 2629,
3033, 3437 and 3841 gestational weeks. As the percentages of active fetal states were gradually
reduced and that of the resting fetal states increased during 2636 weeks, and the percentage was stable
in 3741 weeks, fetal behavioral development would be complete at 37 weeks in normal pregnancy
(Figure 4) [21].
Figure 4. Fetal behavioral states obtained by computer analysis at four pregnancy periods
using the algorithm of Figure 3. Fetal behavioral development would be complete in
37 weeks of pregnancy [22].
7. Discussion and Conclusion
FHR diagnosis were objectivity achieved by quantitative analysis of fetal heart rate using FHR score
and automated evaluation. Parallel processing of neural network computer diagnosis of the probability
of fetal outcome confirmed diagnostic accuracy of FHR score, and frequency spectrum analysis
diagnosed pathologic sinusoidal FHR and the loss of variability, in addition rapid and direct reporting
system enhanced monitoring utility. Comprehensive FHR evaluation was obtained by automated
diagnosis. Perinatal mortality was reduced and no cerebral palsy developed after introduction of the
automatic centralized computer with direct and rapid reporting system at Seirei Mikatahara hospital,
which was also capable of simultaneously monitoring multiple labor cases with a large time sharing
system, which is attractive and useful in busy obstetric institutions handling a large number of births.
The time used to visually monitor the fetal CTG in the labor is economized even in small obstetric
clinics. In addition, the precision of analysis and no exhaustion will be advantages of computerized
monitoring.
Acknowledgments
The first author expresses sincere gratitude to contributions ofco-authors and the efforts of TOITU to
develop the cenral computer.
Algorithms 2015, 8
405
Author Contributions
Maeda K contributed the manuscript, quantified objective analysis of FHR curve, creation of
actocardiogram, of which application on the diagnosis of physiologic sinusoidal pattern, frequency
spectrum of FHR curve, computer analysis of fetal behavior with actocardiogram.
Noguchi Y created the soft wear of artificial neural network analysis, its application for the FHR, the
training of the neural network, and theneural network FH diagnosis.
Utsu M set the central computer system in his hospital, actual diagnosis of the fetus in the labor, and
the statistics on the effect of the new computer system.
Nagasawa T conducted the creation of central computer system, introduced frequency spectrum
analysis, the diagnosis of ominous sinusoidal FHR and the loss of FHR variability with the spectrums.
Conflicts of Interest
The authors declare no conflict of interest.
References
1.
2.
Hon, E.H. An Atlas of Fetal Heart Rate Patterns; Harty Press: New Haven, CT, USA, 1968.
Chik, L.; Rosen, M.G.; Hirsch, V.J. An analysis of lag time and variability of fetal heart rate
measurements. Am. J. Obstet. Gynecol. 1974, 118, 237242.
3. Maeda, K.; Arima, T.; Tatsumura, T. Computer-Aided fetal heart rate analysis and automatic fetal
distress diagnosis during labor and pregnancy utilizing external technique in fetal monitoring.
MEDINFO 1980, 80, 12141218.
4. Maeda, K.; Noguchi, Y.; Matsumoto, F.; Nagasawa, T. Quantitative fetal heart rate evaluation
without pattern classification: FHR score and artificial neural network analysis. In Text Book of
Perinatal Medicine, 2nd ed.; Kurjak, A., Chervenak, F.A., Eds.; Informa: Londone, UK, 2006;
pp. 14871495.
5. Maeda, K.; Utsu, M.; Makio, A.; Serizawa, M.; Noguchi, Y.; Hamada, T.; Mariko, K.;
Matsumoto, F. Neural network computer analysis of fetal heart rate. J. Matern. Fetal Invest. 1998,
8, 163171.
6. Maeda, K.; Nagsawa, T. Automatic computerized diagnosis of fetal sinusoidal heart rate.
Fetal Diag. Ther. 2005, 20, 328333.
7. Maeda, K.; Nagasawa, T. Loss of FHR variability diagnosed by frequency analysis. J. Perinat. Med.
2010, 38, 7782.
8. Maeda, K. Studies on new ultrasonic Doppler fetal actograoh and continuous recording of fetal
movement. Acta Obstet. Gynecol. Jpn. 1984, 36, 280288.
9. Ito, T.; Maeda, K.; Takahashi, H.; Nagata, N.; Nakajima, K.; Terakawa, N. Differentiation between
physiologic and pathologic sinusoidal FHR pattern by fetal actocardiogram. J. Perinat. Med. 1994,
22, 3948.
10. Maeda, K. Origin of the long-term variability and acceleration of FHR studied for the prevention of
cerebral palsy in fetal hypoxia and general insults. J. Perinat. Med. 2013, doi:11.1515/jpm-2013-0134.
Algorithms 2015, 8
406
11. Maeda, K. Actocardiographic analysis of fetal hypoxia detected by the bradycardia, loss
of fetal heart rate acceleration and long term variability. J. Health Med. Inform. 2013, 4, 118122.
12. Maeda, K. Modalities of fetal evaluation to detect fetal compromise prior to the development of
significant neurological damage. J. Obstet. Gynecol. Res. 2014, doi:10.1111/jog.12481.
13. Chudek, V.; Anden, J.; Mallat, S.; Abry, P.; Doret, M. Scattering transform for intrapartum fetal
heart rate variability fractal analysis: a case control study. IEEE Trans. Biomed. Eng. 2014, 61,
11001108.
14. Dawes, G.S.; Lobb, M.; Moulden, M.; Redman, C.W.; Wheeler, T. Antenatal cardiotocogram
quality and interpretation using computers. BJOG 2014, 121, 28.
15. Georgieva, A.; Pavne, S.J.; Moulden, M.; Redman, C.W. Computerized fetal hearte rate analysis in
labor: detection of intervals with un-assignable baseline. Physiol. Meas. 2011, 32, 15491560.
16. Jezewski, M.; Wrobel, J.; Czabanski, R.; Horoba, K. Analysis of extracted cardiotocobraphic signal
features to imptove automated prediction of fetal outcome. Biocybern. Biomed. Engineer. 2010, 30,
2947
17. Signorini, M.G.; Fanelli, A.; Magenes, G. Monitoring fetal heart rate during pregnancy
contributions from advanced signal processing and wearable technology. Comput. Math. Methods
Med. 2014, 2014, 707581.
18. Maeda, K.; Iwabe, T.; Yoshida, S.; Ito, T.; Minagawa, Y.; Morokuma, S.; Pooh, R.K.; Fuchiwaki, T.
Detailed multigrade evaluation of fetal disorders with the quantified actocardiogram. J. Perinat.
Med. 2009, 37, 392396.
19. Maeda, K.; Utsu, M.; Noguchi, Y.; Matsumoto, F.; Nagasawa, T. Central computerized automatic fetal
heart rate diagnosis with a rapid and direct alarm system. Open Med. Devices J. 2012, 4, 2833.
20. Kamitani, K. Maternal and Child Health Status in Japan; Boshi Hoken Jigyodan: Tokyo, Janpan,
2011; pp. 2223.
21. Takeshita, K.; Ando, Y.; Ohtani, K.; Takashima, S. Cerebral palsy in Tottori, Japan.
Neuroepidemiology 1989, 8, 184192.
22. Maeda, K.; Tatsumura, M.; Utsu, M. Analysis of fetal movements by Doppler actocardiogram and
fetal B-mode imaging. Clin. Perinatol. 1999, 26, 829851.
2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article
distributed under the terms and conditions of the Creative Commons Attribution license
(http://creativecommons.org/licenses/by/4.0/).
Você também pode gostar
- Business Startup Practical Plan PDFDocumento70 páginasBusiness Startup Practical Plan PDFShaji Viswanathan. Mcom, MBA (U.K)Ainda não há avaliações
- Life Overseas 7 ThesisDocumento20 páginasLife Overseas 7 ThesisRene Jr MalangAinda não há avaliações
- Canada's Health Care SystemDocumento11 páginasCanada's Health Care SystemHuffy27100% (2)
- Intra-Operative Monitoring: A Comprehensive ApproachNo EverandIntra-Operative Monitoring: A Comprehensive ApproachAinda não há avaliações
- Fundamentals of Fast SwimmingDocumento9 páginasFundamentals of Fast SwimmingTorcay Ulucay100% (1)
- Rachel Lindsay - Man of IceDocumento170 páginasRachel Lindsay - Man of Icemistytom2883% (30)
- Farid Jafarov ENG Project FinanceDocumento27 páginasFarid Jafarov ENG Project FinanceSky walkingAinda não há avaliações
- Uterine Artery Malformation1Documento9 páginasUterine Artery Malformation1venkayammaAinda não há avaliações
- Revision Notes For The Mrcog Part 1 Oxford Specialty Training Revision Texts PDF Downloaddocx PDFDocumento2 páginasRevision Notes For The Mrcog Part 1 Oxford Specialty Training Revision Texts PDF Downloaddocx PDFvenkayamma0% (3)
- UMR Introduction 2023Documento110 páginasUMR Introduction 2023tu reves mon filsAinda não há avaliações
- NCMA 217 - Newborn Assessment Ma'am JhalDocumento5 páginasNCMA 217 - Newborn Assessment Ma'am JhalMariah Blez BognotAinda não há avaliações
- Allium CepaDocumento90 páginasAllium CepaYosr Ahmed100% (3)
- Activity No 1 - Hydrocyanic AcidDocumento4 páginasActivity No 1 - Hydrocyanic Acidpharmaebooks100% (2)
- CTG HaDocumento15 páginasCTG HaNabila SaribanunAinda não há avaliações
- Fetal MonitoringDocumento9 páginasFetal MonitoringfadlydrAinda não há avaliações
- Sensors 20 04139Documento15 páginasSensors 20 04139soo chiAinda não há avaliações
- Zuva MuzachimDocumento6 páginasZuva MuzachimZuva MuzachimAinda não há avaliações
- 12Documento15 páginas12Jolly EddzAinda não há avaliações
- Cerebrospinal Fluid and Blood Biomarkers of Status Epilepticus - 2020Documento40 páginasCerebrospinal Fluid and Blood Biomarkers of Status Epilepticus - 2020Reny Wane Vieira dos SantosAinda não há avaliações
- Monitorización de La Fibrilación AuricularDocumento15 páginasMonitorización de La Fibrilación AuricularDaniel MuñozAinda não há avaliações
- Acad Emerg Med 2004 p1193Documento5 páginasAcad Emerg Med 2004 p1193Handris SupriadiAinda não há avaliações
- Monitoreo 2012 PDFDocumento19 páginasMonitoreo 2012 PDFDiego A. Cuadros TorresAinda não há avaliações
- Caveats of Longitudinal Automated Hippocampal Volumetry in Alzheimer's DiseaseDocumento22 páginasCaveats of Longitudinal Automated Hippocampal Volumetry in Alzheimer's Diseasedess101Ainda não há avaliações
- Quan Et Al. 2022 - Frequency-Specific Changes of Amplitude of Low-Frequency Fluctuations in Patients With Acute Basal Ganglia Ischemic StrokeDocumento10 páginasQuan Et Al. 2022 - Frequency-Specific Changes of Amplitude of Low-Frequency Fluctuations in Patients With Acute Basal Ganglia Ischemic StrokeJ ChenAinda não há avaliações
- Jurnal 16 - An Internet-Based Tool For Pediatric Cardiac Disease Diagnosis Using Intelligent PhonocardiographyDocumento5 páginasJurnal 16 - An Internet-Based Tool For Pediatric Cardiac Disease Diagnosis Using Intelligent PhonocardiographyAngela Erti Suci RosariAinda não há avaliações
- Rulebased Algorithm For Intrapartum Cardiotocograph Pattern Features Extraction and ClassificationDocumento13 páginasRulebased Algorithm For Intrapartum Cardiotocograph Pattern Features Extraction and ClassificationdianaAinda não há avaliações
- 2021 Full-2Documento5 páginas2021 Full-2Argtim RexhepiAinda não há avaliações
- Prediction of Fetal State From The Cardiotocogram Recordings Using Adaptive Neuro-Fuzzy Inference SystemsDocumento7 páginasPrediction of Fetal State From The Cardiotocogram Recordings Using Adaptive Neuro-Fuzzy Inference SystemsguptaAinda não há avaliações
- 16Documento9 páginas16Jolly EddzAinda não há avaliações
- Pulse Rate Variability Is Not A Surrogate For Heart Rate VariabilityDocumento7 páginasPulse Rate Variability Is Not A Surrogate For Heart Rate VariabilityFiras ZakAinda não há avaliações
- Rajiv Gandhi University of Health Sciences - Karnataka Bangalore Annexure II: Proforma For Registration of Subject For DissertationDocumento14 páginasRajiv Gandhi University of Health Sciences - Karnataka Bangalore Annexure II: Proforma For Registration of Subject For DissertationvenkayammaAinda não há avaliações
- Eeg and EcgDocumento12 páginasEeg and EcgsitvijayAinda não há avaliações
- Fetal MonitoringDocumento14 páginasFetal MonitoringRobinson BrenesAinda não há avaliações
- Transthoracic Echocardiography For Cardiopulmonary Monitoring in Intensive Care (FATE)Documento9 páginasTransthoracic Echocardiography For Cardiopulmonary Monitoring in Intensive Care (FATE)Anish H DaveAinda não há avaliações
- Review - Prediction of ESDocumento9 páginasReview - Prediction of ESRenukaAinda não há avaliações
- Hodnett Et Al 2015 Clinical Anatomy 2Documento7 páginasHodnett Et Al 2015 Clinical Anatomy 2ChrissAinda não há avaliações
- EANM Procedure Guideline For Brain Perfusion SPECT PDFDocumento10 páginasEANM Procedure Guideline For Brain Perfusion SPECT PDFAulia HudaAinda não há avaliações
- CTG FigoDocumento12 páginasCTG FigoIuliaCoropetchi0% (1)
- Fetal ECG for Improving Intrapartum MonitoringDocumento5 páginasFetal ECG for Improving Intrapartum MonitoringmariakjaimesAinda não há avaliações
- 2017.JCSM - Sharma.HRPO Screening For OSA in CHF InpatientsDocumento6 páginas2017.JCSM - Sharma.HRPO Screening For OSA in CHF Inpatientslion5835Ainda não há avaliações
- High-Frequency Oscillations in The Normal Human BrainDocumento12 páginasHigh-Frequency Oscillations in The Normal Human BrainCindy Tatiana NMAinda não há avaliações
- JCSM 14 9 1495Documento7 páginasJCSM 14 9 1495Bagus Tri WahyudiAinda não há avaliações
- Monitoring Atrial Fibrillation Using PPG Signals and A SmartphoneDocumento16 páginasMonitoring Atrial Fibrillation Using PPG Signals and A SmartphoneCarlos Daniel Valencia RincónAinda não há avaliações
- 1809 6891 Cab 19 E49000Documento12 páginas1809 6891 Cab 19 E49000FADASDADSAinda não há avaliações
- Engineering Applications of Artificial Intelligence: Shing-Hong Liu, Kang-Ming Chang, Tsu-Hsun FuDocumento10 páginasEngineering Applications of Artificial Intelligence: Shing-Hong Liu, Kang-Ming Chang, Tsu-Hsun FuGabriel CscAinda não há avaliações
- Clinical Outcomes of Neonatal Hypoxic Ischemic Encephalopathy Evaluated With Diffusion-Weighted Magnetic Resonance ImagingDocumento6 páginasClinical Outcomes of Neonatal Hypoxic Ischemic Encephalopathy Evaluated With Diffusion-Weighted Magnetic Resonance ImagingDrsandy SandyAinda não há avaliações
- HarP The EADC ADNI Harmonized Protocol For Manual Hippocampal Segmentation. A Standard of Reference From A Global Working GroupnnDocumento13 páginasHarP The EADC ADNI Harmonized Protocol For Manual Hippocampal Segmentation. A Standard of Reference From A Global Working GroupnnValeria AlzateAinda não há avaliações
- Chest 147 1 132Documento8 páginasChest 147 1 132Timothy Eduard A. SupitAinda não há avaliações
- Ambulatory Elaphic MonitoDocumento3 páginasAmbulatory Elaphic Monitocap tainAinda não há avaliações
- A88 Nirs PdaDocumento9 páginasA88 Nirs PdaFahri OvalıAinda não há avaliações
- Diagnosis of Idiopathic Normal Pressure Hydrocephalus Is Supported by MRI-based Scheme: A Prospective Cohort StudyDocumento11 páginasDiagnosis of Idiopathic Normal Pressure Hydrocephalus Is Supported by MRI-based Scheme: A Prospective Cohort StudyDini NanamiAinda não há avaliações
- AI and Sonographer Cardiac AssessmentDocumento9 páginasAI and Sonographer Cardiac AssessmentAndré Muniz de MouraAinda não há avaliações
- BioRadio - WirelessECG PDFDocumento13 páginasBioRadio - WirelessECG PDFsastrakusumawijayaAinda não há avaliações
- Hung Et Al-2009-Human Factors and Ergonomics in Manufacturing & Service Industries PDFDocumento16 páginasHung Et Al-2009-Human Factors and Ergonomics in Manufacturing & Service Industries PDFDiego A Echavarría AAinda não há avaliações
- Dynamic Imaging of The Fetal Heart Using Metric Optimized GatingDocumento19 páginasDynamic Imaging of The Fetal Heart Using Metric Optimized GatingdpnairAinda não há avaliações
- Deep Neural Network Based Classification of Cardiotocograms Outperformed Conventional AlgorithmsDocumento9 páginasDeep Neural Network Based Classification of Cardiotocograms Outperformed Conventional AlgorithmsPANKAJ JADHAVAinda não há avaliações
- Siira Et Al-2005-BJOG An International Journal of Obstetrics & GynaecologyDocumento6 páginasSiira Et Al-2005-BJOG An International Journal of Obstetrics & GynaecologyvenkayammaAinda não há avaliações
- Home Sleep Tests For Obstructive Sleep Apnea (OSA) : Mukesh Kapoor, MD, and Glen Greenough, MDDocumento6 páginasHome Sleep Tests For Obstructive Sleep Apnea (OSA) : Mukesh Kapoor, MD, and Glen Greenough, MDPhạm Văn HiệpAinda não há avaliações
- Applied Sciences: Respiration Monitoring For Premature Neonates in NicuDocumento11 páginasApplied Sciences: Respiration Monitoring For Premature Neonates in NicuNicole LantinAinda não há avaliações
- Focal and Non-focal Epilepsy Localization_ a ReviewDocumento19 páginasFocal and Non-focal Epilepsy Localization_ a ReviewHadj Abdelkader BENGHENIAAinda não há avaliações
- New Seep Apnea AIDocumento15 páginasNew Seep Apnea AIgauravchauAinda não há avaliações
- Outcomes of Neonates With Perinatal Asphyxia at A Tertiary Academic Hospital in Johannesburg, South AfricaDocumento6 páginasOutcomes of Neonates With Perinatal Asphyxia at A Tertiary Academic Hospital in Johannesburg, South Africaeen265Ainda não há avaliações
- Aina - Tugas Final Test Berpikir KritisDocumento20 páginasAina - Tugas Final Test Berpikir KritisSylviviani ZelviaAinda não há avaliações
- Animals: Contactless Video-Based Heart Rate Monitoring of A Resting and An Anesthetized PigDocumento14 páginasAnimals: Contactless Video-Based Heart Rate Monitoring of A Resting and An Anesthetized PigKoekoeh SantosoAinda não há avaliações
- European J of Heart Fail - 2009 - Mortara - Home Telemonitoring in Heart Failure Patients The HHH Study Home or HospitalDocumento7 páginasEuropean J of Heart Fail - 2009 - Mortara - Home Telemonitoring in Heart Failure Patients The HHH Study Home or HospitalnjdshdshuAinda não há avaliações
- Intracranial Hemorrhage in Full-Term Newborns: A Hospital-Based Cohort StudyDocumento10 páginasIntracranial Hemorrhage in Full-Term Newborns: A Hospital-Based Cohort StudyTriponiaAinda não há avaliações
- 2001.00155Documento35 páginas2001.00155silvalimaaf94Ainda não há avaliações
- Remote and Longterm Selfmonitoring of Electroencephalographic and Noninvasive Measurable Variables at Home in Patients With Epilepsy EEGHOME Protocol For An Observational studyJMIR Research ProtocolsDocumento12 páginasRemote and Longterm Selfmonitoring of Electroencephalographic and Noninvasive Measurable Variables at Home in Patients With Epilepsy EEGHOME Protocol For An Observational studyJMIR Research ProtocolsMiguel PalacioAinda não há avaliações
- Clinical NeurophysiologyDocumento32 páginasClinical NeurophysiologyPIERRELEEAinda não há avaliações
- Analysis Software CTG RecordingsDocumento2 páginasAnalysis Software CTG RecordingsaoecmAinda não há avaliações
- Echography and Doppler of the BrainNo EverandEchography and Doppler of the BrainChiara RobbaAinda não há avaliações
- Ceu Guidance Young People 2010Documento35 páginasCeu Guidance Young People 2010Tareq SawanAinda não há avaliações
- Platelet MicroparticleDocumento9 páginasPlatelet MicroparticlevenkayammaAinda não há avaliações
- Preeclampsia Nice Guide UkDocumento295 páginasPreeclampsia Nice Guide UkDavid Zuluaga LemaAinda não há avaliações
- Power Point of PosterDocumento28 páginasPower Point of PostervenkayammaAinda não há avaliações
- Venous Thromboembolism (VTE) and Hormonal Contraception 014 PDFDocumento16 páginasVenous Thromboembolism (VTE) and Hormonal Contraception 014 PDFTaraAinda não há avaliações
- ACOG Issues Less Restrictive Guidelines For Vaginal Birth After Cesarean DeliveryDocumento6 páginasACOG Issues Less Restrictive Guidelines For Vaginal Birth After Cesarean DeliveryvenkayammaAinda não há avaliações
- Venous Thromboembolism (VTE) and Hormonal Contraception 014 PDFDocumento16 páginasVenous Thromboembolism (VTE) and Hormonal Contraception 014 PDFTaraAinda não há avaliações
- Ymj 55 367Documento7 páginasYmj 55 367venkayammaAinda não há avaliações
- Guidelines For The Management of Occupational Exposures To HBV, HCV, and HIV and Recommendations For Postexposure ProphylaxisDocumento58 páginasGuidelines For The Management of Occupational Exposures To HBV, HCV, and HIV and Recommendations For Postexposure ProphylaxisvenkayammaAinda não há avaliações
- Preeclampsia Nice Guide UkDocumento295 páginasPreeclampsia Nice Guide UkDavid Zuluaga LemaAinda não há avaliações
- Hum. Reprod.-2005-Farquharson-3008-11Documento4 páginasHum. Reprod.-2005-Farquharson-3008-11venkayammaAinda não há avaliações
- Name Rinku Agarwal Ward Obg Iii DOA 30/9/15 Ip - No 1192431 AGE 24 Yrs DOD 3/10/15 Op No. 3407817 SEX FDocumento2 páginasName Rinku Agarwal Ward Obg Iii DOA 30/9/15 Ip - No 1192431 AGE 24 Yrs DOD 3/10/15 Op No. 3407817 SEX FvenkayammaAinda não há avaliações
- Covering LetterDocumento1 páginaCovering LettervenkayammaAinda não há avaliações
- Twin Pregnancy With A Complete Hydatidiform Mole and Coexisting FoetusDocumento3 páginasTwin Pregnancy With A Complete Hydatidiform Mole and Coexisting FoetusvenkayammaAinda não há avaliações
- Twin Pregnancy With A Complete Hydatidiform Mole and Coexisting FoetusDocumento7 páginasTwin Pregnancy With A Complete Hydatidiform Mole and Coexisting FoetusvenkayammaAinda não há avaliações
- Successful Pregnancy Outcome With Massive Bilateral Angiomyolipoma - A Case ReportDocumento5 páginasSuccessful Pregnancy Outcome With Massive Bilateral Angiomyolipoma - A Case ReportvenkayammaAinda não há avaliações
- Shubhangi Mande, Sangeeta Chippa, Dipti Vaidya & Swati ShiradkarDocumento3 páginasShubhangi Mande, Sangeeta Chippa, Dipti Vaidya & Swati ShiradkarvenkayammaAinda não há avaliações
- Siira Et Al-2005-BJOG An International Journal of Obstetrics & GynaecologyDocumento6 páginasSiira Et Al-2005-BJOG An International Journal of Obstetrics & GynaecologyvenkayammaAinda não há avaliações
- Comparing TVS and Hysteroscopy for AUB DiagnosisDocumento11 páginasComparing TVS and Hysteroscopy for AUB DiagnosisvenkayammaAinda não há avaliações
- Name Rinku Agarwal Ward Obg Iii DOA 30/9/15 Ip - No 1192431 AGE 24 Yrs DOD 3/10/15 Op No. 3407817 SEX FDocumento2 páginasName Rinku Agarwal Ward Obg Iii DOA 30/9/15 Ip - No 1192431 AGE 24 Yrs DOD 3/10/15 Op No. 3407817 SEX FvenkayammaAinda não há avaliações
- Pi Is 0002937808008806Documento7 páginasPi Is 0002937808008806venkayammaAinda não há avaliações
- Name Rinku Agarwal Ward Obg Iii DOA 30/9/15 Ip - No 1192431 AGE 24 Yrs DOD 3/10/15 Op No. 3407817 SEX FDocumento2 páginasName Rinku Agarwal Ward Obg Iii DOA 30/9/15 Ip - No 1192431 AGE 24 Yrs DOD 3/10/15 Op No. 3407817 SEX FvenkayammaAinda não há avaliações
- Thrombophilia and Unexplained Pregnancy Loss in Indian PatientsDocumento5 páginasThrombophilia and Unexplained Pregnancy Loss in Indian PatientsvenkayammaAinda não há avaliações
- Rajiv Gandhi University of Health Sciences - Karnataka Bangalore Annexure II: Proforma For Registration of Subject For DissertationDocumento14 páginasRajiv Gandhi University of Health Sciences - Karnataka Bangalore Annexure II: Proforma For Registration of Subject For DissertationvenkayammaAinda não há avaliações
- Effective Postoperative Pain Management StrategiesDocumento10 páginasEffective Postoperative Pain Management StrategiesvenkayammaAinda não há avaliações
- Hum. Reprod.-2004-Carp-191-5Documento5 páginasHum. Reprod.-2004-Carp-191-5venkayammaAinda não há avaliações
- LH 11 180 190 220 230 270 280 390 400 Breaker Safety & Operating InstructionsDocumento304 páginasLH 11 180 190 220 230 270 280 390 400 Breaker Safety & Operating InstructionshadensandorAinda não há avaliações
- WSO 2022 IB Working Conditions SurveyDocumento42 páginasWSO 2022 IB Working Conditions SurveyPhạm Hồng HuếAinda não há avaliações
- Design and Built-A4Documento2 páginasDesign and Built-A4farahazuraAinda não há avaliações
- Aço X6NiCrTiMoVB25!15!2 - 1.4980 Austenitic SteelDocumento2 páginasAço X6NiCrTiMoVB25!15!2 - 1.4980 Austenitic SteelMoacir MachadoAinda não há avaliações
- Indonesia Organic Farming 2011 - IndonesiaDOCDocumento18 páginasIndonesia Organic Farming 2011 - IndonesiaDOCJamal BakarAinda não há avaliações
- General Specifications: Detail ADocumento1 páginaGeneral Specifications: Detail AJeniel PascualAinda não há avaliações
- Q1 Tle 4 (Ict)Documento34 páginasQ1 Tle 4 (Ict)Jake Role GusiAinda não há avaliações
- Reading and Listening 2Documento4 páginasReading and Listening 2Hải Anh TạAinda não há avaliações
- B.Sc. (AGRICULTURE) HORTICULTURE SYLLABUSDocumento31 páginasB.Sc. (AGRICULTURE) HORTICULTURE SYLLABUSgur jazzAinda não há avaliações
- SVIMS-No Que-2Documento1 páginaSVIMS-No Que-2LikhithaReddy100% (1)
- Jairo Garzon 1016001932 G900003 1580 Task4Documento12 páginasJairo Garzon 1016001932 G900003 1580 Task4Jairo Garzon santanaAinda não há avaliações
- Forest Fire Detection and Guiding Animals To A Safe Area by Using Sensor Networks and SoundDocumento4 páginasForest Fire Detection and Guiding Animals To A Safe Area by Using Sensor Networks and SoundAnonymous 6iFFjEpzYjAinda não há avaliações
- Vaginal Examinations in Labour GuidelineDocumento2 páginasVaginal Examinations in Labour GuidelinePooneethawathi Santran100% (1)
- Tutorial 7: Electromagnetic Induction MARCH 2015: Phy 150 (Electricity and Magnetism)Documento3 páginasTutorial 7: Electromagnetic Induction MARCH 2015: Phy 150 (Electricity and Magnetism)NOR SYAZLIANA ROS AZAHARAinda não há avaliações
- Akshaya Trust NgoDocumento24 páginasAkshaya Trust NgodushyantAinda não há avaliações
- Dr. Namrata Misra Head of Bioinnovations at KIIT UniversityDocumento1 páginaDr. Namrata Misra Head of Bioinnovations at KIIT Universitymanisha maniAinda não há avaliações
- Reach Out and Read Georgia Selected For AJC Peachtree Road Race Charity Partner ProgramDocumento2 páginasReach Out and Read Georgia Selected For AJC Peachtree Road Race Charity Partner ProgramPR.comAinda não há avaliações
- Alok ResumeDocumento3 páginasAlok Resumealok choudharyAinda não há avaliações
- Li Ching Wing V Xuan Yi Xiong (2004) 1 HKC 353Documento11 páginasLi Ching Wing V Xuan Yi Xiong (2004) 1 HKC 353hAinda não há avaliações
- 2024 - Chung 2024 Flexible Working and Gender Equality R2 CleanDocumento123 páginas2024 - Chung 2024 Flexible Working and Gender Equality R2 CleanmariaAinda não há avaliações
- Directory of Frequently Called Numbers: Maj. Sheikh RahmanDocumento1 páginaDirectory of Frequently Called Numbers: Maj. Sheikh RahmanEdward Ebb BonnoAinda não há avaliações