Escolar Documentos
Profissional Documentos
Cultura Documentos
Clinical Factors in Patients With Ischemic Versus
Enviado por
Lulu SupergirlDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Clinical Factors in Patients With Ischemic Versus
Enviado por
Lulu SupergirlDireitos autorais:
Formatos disponíveis
18 Zhang et al
World J Emerg Med, Vol 2, No 1, 2011
Original Article
Clinical factors in patients with ischemic versus
hemorrhagic stroke in East China
Jing Zhang, Yao Wang, Gan-nan Wang, Hao Sun, Tao Sun, Jian-quan Shi, Hang Xiao, Jin-song Zhang
Department of Emergency Medicine, First Affiliated Hospital, Nanjing Medical University, Nanjing 210029, China (Zhang
J, Wang Y, Wang GN, Sun H, Zhang JS); Department of Epidemiology and Biostatistics, Nanjing Medical University,
Nanjing 210029 China (Sun T); Department of Neurology, Affiliated Nanjing Brain Hospital, Nanjing Medical University,
Nanjing 210029, China (Shi JQ); Laboratory of Neurotoxicology, School of Public Health, Nanjing Medical University,
Nanjing 210029, China (Xiao H)
Corresponding Author: Jin-song Zhang, Email: zhangjso@sina.com
BACKGROUND: Stroke is one of the leading causes of mortality and morbidity of vascular
diseases, and its incidence maintains at a high level around the world. In China, stroke has been a
major public health problem. Because the pathogenesis of ischemic stroke is different from that of
hemorrhagic stroke, their clinical factors would not be the same. Therefore to investigate the different
effects of various effect factors on ischemic versus hemorrhagic stroke and then to enhance the
prevention are crucial to decrease the incidence.
METHODS: A total of 692 patients, consisting of 540 ischemic stroke patients and 152
hemorrhagic stroke patients from East China, were included in this study. The related factors of
stroke subtypes were collected and analyzed.
RESULTS: The factors significantly associated with ischemic stroke as opposed to hemorrhagic
stroke were family history of stroke, obesity, atherosclerotic plaque of the common carotid artery,
atrial fibrillation, hyperfibrinogenemia, transient ischemic attack (TIA), atherosclerotic plaque of
the internal carotid artery, coronary heart, lower high-density lipoproteins (lower HDL), increasing
age, diabetes mellitus, and gender (male) (P<0.05). Leukocytosis, hypertension and family history
of hypertension were the significant factors associated with hemorrhagic stroke versus ischemic
stroke. Smoking, drinking, kidney diseases and lower HDL-C were the significant factors contributing
to ischemic stroke in man. Obesity, family history of hypertension, family history of stroke,
hypercholesteremia and myocardial ischemia were the significant factors for females with ischemic
stroke.
CONCLUSIONS: The most prominent factors for overall stroke in East China were
hypertension, followed by higher pulse pressure and hypercholesteremia. The factors for ischemic
and hemorrhagic stroke are not the same. Different effects of risk factors on stroke are found in male
and female patients.
KEY WORDS: Ischemic stroke; Hemorrhagic stroke; Risk factors
World J Emerg Med 2011;2(1):18-23
DOI: 10.5847/wjem.j.1920-8642.2011.01.003
INTRODUCTION
Stroke is one of the leading causes of mortality and
morbidity of vascular diseases.[1] Its incidence maintains
at a high level around the world. In China the official
statistics from 31 regions showed that there were about
www.wjem.org
2011 World Journal of Emergency Medicine
1.5-2.0 million new stroke patients each year,[2] and it has
been a major public health problem in China.[3] Because
of the poor therapeutic result, the most important method
to reduce the morbidity of stroke is prophylaxis, which
depends on the realization and control of the risk factors
World J Emerg Med, Vol 2, No 1, 2011
for stroke.[4] Because the pathogenesis of ischemic stroke
is different from that of hemorrhagic stroke, their clinical
factors would not be the same. Hence both investigation
of the effects of various effect factors on ischemic versus
hemorrhagic stroke and and enhanced prevention are
crucial to decrease the incidence of stroke.
In this study we investigated the factors for ischemic
versus hemorrhagic stroke by analyzing the clinical data
of the patients so as to provide some scientific evidence
for stroke prevention in East China.
METHODS
Study design
This study was supported by grants from the Jiangsu
Provincial Natural Science Foundation. The protocol of
the study was reviewed and approved by the institutional
review board of Nanjing Medical University, Nanjing,
China. Informed consent was obtained from each patient,
who donated 5 mL of blood for routine and biochemistry
examination.
All patients were recruited between November 2008
and May 2010 at the First Affiliated Hospital of Nanjing
Medical University and Brain Hospital Affiliated to
Nanjing Medical University. A total of 692 hospitalized
patients with stroke were genetically unrelated ethnic Han
Chinese in East China. According to the International
Classification of Diseases, Tenth Revised Edition (ICD10), we recruited 540 ischemic stroke patients and 152
hemorrhagic stroke patients. Patients who had other
types of stroke (transient ischemic attack, subarachnoid
hemorrhage, and cerebrovascular malformation) and
severe systemic diseases (collagenosis, endocrine, and
metabolic disease (except for diabetes mellitus, DM),
inflammation, neoplastic) were excluded. Diagnosis of
stroke was based on the results of strict neurological
examination by CT, MRI, or both. The clinical data
of the patients were obtained through a questionnaire
depicted general state of health, life style, family history,
previous health history, results of laboratory and auxiliary
examinations.
The clinical factors to be observed in this study
included advanced age (male>55 years, female>65
years [5] ), gender (male-exposure), cigarette smoking
(average smoking1 cigarettes per day, and continued
more than one year), alcohol drinking (at least 1 time
per week, alcohol consumption50 mL and more than
3 months), obesity (body mass index (BMI)28 kg/m2);
family history of coronary artery disease (CAD), stroke,
hypertension and diabetes mellitus (DM); history of
19
hypertension (in line with the diagnostic criteria of China
Guidelines of Hypertension Updated 2005), increased
pulse pressure (>40 mmHg), atrial fibrillation (AF),
DM (in line with the diagnostic criteria of WHO1999),
valvular heart diseases, CAD, transient ischemic attack
(TIA), peripheral arterial thrombosis, peptic ulcer disease,
kidney disease; elevated systolic blood pressure (SBP140
mmHg), elevated diastolic blood pressure (DBP 90
mmHg), increased white blood cell (WBC>10.0109/L),
hypertriglyceridemia (triglyceride (TG)>1.7 mmol/L),
hypercholesterolemia (total cholesterol (TC)5.7 mmol/L),
low level of high-density lipoproteins (HDL<1.0 mmol/L),
hyperfibrinogenemia (fibrinogen (FIB)>4.0 g/L); ischemic
ECG changes, ECG arrhythmia; and the formation of
carotid atheroma, common carotid atheroma and vertebral
artery stenosis shown by carotid ultrasound.
Statistical analysis
Statistical analysis were performed by the SPSS 16.0
package. The continuous clinical variants were compared
by unpaired Student's t test. The Chi-square test was used
to evaluate differences in proportion of clinical factors
in patients between ischemic and hemorrhagic stroke.
We used logistic regression analysis to calculate odds
ratio (OR) of the incidence of ischemic stroke versus
hemorrhagic stroke and of incidence of ischemic stroke
(hemorrhagic stroke) in men versus in women and 95%
confidence interval.[5,6] A P value <0.05 (two-tailed) was
considered statistically significant.
RESULTS
Subtype
A total of 692 patients, 540 (78%) ischemic patients
and 152 (22%) hemorrhagic patients from East China,
were enrolled in this study. The incidence rate of ischemic
stroke in this area was obviously higher than that of
hemorrhagic stroke.
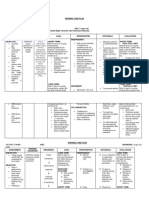
Sex and age distribution
In this series, 428 (61.85%) were male patients
and 264 (38.15%) female patients, while 59.63% of the
ischemic group and 69.74% of the hemorrhagic group
were male. Male patients account for a large propotion in
both ischemic and hemorrhagic groups. The mean age for
the ischemic group was 68.3710.59 years, which was
significantly higher than that of the hemorrhagic group
(62.1612.59 years, P<0.01). The comparison of the age
of patients with ischemic or hemorrhagic stroke was
presented in Figure 1. The proportion of 65-85 years old
www.wjem.org
20 Zhang et al
World J Emerg Med, Vol 2, No 1, 2011
patients was predominant in the ischemic group (66.48%)
and that of 55-75 years old patients in the hemorrhagic
group (53.29%). The mean age was 66.5211.25 years
for males and 67.8111.47 years for females, and there
was no significant difference.
Laboratory and auxiliary examination
The laboratory data of patients with ischemic and
hemorrhagic stroke were compared (Table 1). Briefly, mean
SBP, DBP, WBC, neutrophil ratio (NE), blood glucose
(BG), HDL, and prothrombin time (PT) were higher in the
hemorrhagic group than in the ischemic group (P<0.05).
However, BMI, TG, TC, and FIB were not statistically
significant between the two groups (P>0.05).
Clinical data
The clinical data of patients with two types of stroke
were shown in Table 2. Compared with the hemorrhagic
group, the ischemic group had a higher prevalence of
clinical factors such as advanced age, male, family history
of hypertension, hypertension, hypercholesterolemia,
obesity, family history of stroke, DM, TIA, CAD, AF,
The proportion of age
40
Ischemic stroke
35
Hemorrhagic stroke
30
25
20
15
10
5
0
<45
45-55
55-65
65-75 75-85
>85
Age (year)
Figure 1. Comparison of the age of patients with ischemic and
hemorrhagic stroke
Table 1. Comparison of clinical data of patients with ischemic and
hemorrhagic stroke
Ischemic patients
(n=540)
BMI (kg/m2)
24.05 3.17
SBP (mmHg)
142.35 22.10
DBP (mmHg)
84.59 25.24
WBC (109/L)
7.38 3.80
NE (%)
65.09 12.61
BG (mmol/L)
6.52 2.63
TG (mmol/L)
4.68 1.24
TC (mmol/L)
1.71 1.18
HDL (mmol/L)
1.15 0.33
PT (s)
12.99 2.53
FIB (g/L)
3.16 1.78
Clinical data
www.wjem.org
Hemorrhagic patients
(n=152)
23.86 2.43
154.76 28.67
91.23 18.75
9.72 4.35
74.29 12.43
7.06 2.74
4.70 1.06
1.75 1.26
1.26 0.36
13.74 2.81
2.98 0.88
P
0.488
0.000
0.003
0.000
0.000
0.028
0.841
0.724
0.001
0.002
0.223
kidney disease, hyperfibrinogenemia, low level of HDL,
the formation of carotid atheroma, the formation of
common carotid atheroma, and vertebral artery stenosis
(P<0.05). Contrarily, the hemorrhagic group might have
a higher prevalence of alcohol drinking, hypertension,
elevated SBP, elevated DBP, a family history of
hypertension, and increased WBC (P<0.05). There was
no significant difference in the distribution of cigarette
smoking, increased pulse pressure, family history of
DM, family history of CAD, valvular heart diseases,
peripheral arterial thrombosis, peptic ulcer disease,
hypertriglyceridemia, hypercholesterolemia, ischemic
ECG changes and ECG arrhythmia between the two
groups (P>0.05).
Logistic regression was used to analyze the influence
of these factors on the occurrence of different types of
stroke (gender and age-adjusted). The patients were
divided into 6 groups according to their age: <45 years,
45-55 years, 55-65 years, 65-75 years, 75-85 years, and
>85 years (Table 3).
In contrast to the hemorrhagic group, the following
factors were found to be more causatively related in
the ischemic group: family history of stroke, obesity,
common carotid atheroma, AF, hyperfibrinogenemia,
TIA, carotid atheroma, low HDL level, advanced age,
DM, male gender. Only increased WBC, hypertension
and family history of hypertension were found to be
contributive in the hemorrhagic group.
The Chi-square test was used to evaluate differences
in clinical factors for stroke in patients of both sexes.
With the increase of age, males were found to be more
susceptible to stroke. As expected, male patients had
a higher prevalence of cigarette smoking (P=0.000)
and alcohol drinking (P=0.000) while the incidence
of obesity in female patients was much higher than in
male patients. In addition, kidney disease (P=0.032)
and low HDL level (P=0.032) were common in male
patients and family history of hypertension (P=0.039),
hypertriglyceridemia (P=0.003), hypercholesterolemia
(P=0.002) and ischemic ECG changes (P=0.006) were
common in female patients.
Logistic regression was used to calculate odds ratio
of the incidence of ischemic stroke in males versus
females as well as 95% confidence interval (Table 4).
The clinical factors of stroke in males and females were
not the same. Among the factors, cigarette smoking,
alcohol drinking, kidney disease and low HDL level
were more contributive in male patients. The effects of
obesity, family history of hypertension, family history of
stroke, hypercholesterolemia and ischemic ECG changes on
World J Emerg Med, Vol 2, No 1, 2011
21
Table 2. The proportion for risk factors in patients with two types of stroke (no. %)
Risk factors
Ischemic patients (n=540)
Hemorrhagic patients (n=152)
Advanced age
420 (77.78)
96 (63.16)
Male
322 (59.63)
106 (69.74)
Cigarette smoking
126 (23.33)
41 (26.97)
Alcohol drinking
86 (15.93)
40 (26.32)
Obesity
51 (9.44)
3 (1.97)
Elevated SBP
308 (57.04)
108 (71.05)
Elevated DBP
209 (38.70)
84 (55.26)
Increased pulse pressure
505 (93.52)
144 (94.74)
Family history of hypertension
124 (22.96)
48 (31.58)
Family history of DM
40 (7.41)
12 (7.89)
Family history of stroke
53 (9.81)
5 (3.29)
Family history of CAD
33 (6.11)
5 (3.29)
Hypertension
407 (75.37)
132 (86.84)
DM
172 (31.85)
30 (19.74)
TIA
55 (10.19)
6 (3.95)
CAD
90 (16.67)
10 (6.58)
Valvular heart diseases
11 (2.04)
2 (1.32)
AF
68 (12.59)
6 (3.95)
Peripheral arterial thrombosis
10 (1.85)
0 (0)
Peptic ulcer disease
21 (3.89)
4 (2.63)
Kidney disease
26 (4.81)
1 (0.66)
Increased WBC
79 (14.63)
62 (40.79)
Hyperfibrinogenemia
87 (16.11)
11 (7.24)
Hypertriglyceridemia
97 (17.96)
30 (19.74)
Hypercholesterolemia
199 (36.85)
58 (38.16)
Low level of HDL
184 (34.07)
30 (19.74)
The formation of carotid atheroma
73 (13.52)
7 (4.61)
The formation of common carotid atheroma
101 (18.70)
8 (5.26)
Vertebral artery stenosis
29 (5.37)
1 (0.66)
Ischemic ECG changes
73 (13.52)
19 (12.50)
ECG arrhythmia
107 (19.81)
21 (13.82)
Table 3. Different influences of risk factors on the occurrence of two
types of stroke
95% CI
P
OR (versus
Risk factors
hemorrhagic patients)
Advanced age
2.122
1.335-3.374 0.002
Male
1.593
1.006-2.523 0.047
Obesity
4.863
1.313-18.005 0.018
Family history of hypertension 0.473
0.290-0.788 0.004
Family history of stroke
5.548
1.861-16.539 0.002
Hypertension
0.401
0.224-0.718 0.002
DM
1.687
1.011-2.814 0.045
AF
3.407
1.352-8.588 0.009
CAD
2.523
1.167-5.456 0.019
TIA
2.829
1.060-7.551 0.038
Low level of HDL
2. 142
1.306-3.514 0.003
Hyperfibrinogenemia
2.904
1.372-6.148 0.005
Increased WBC
0.231
0.143-0.371 0.000
The formation of carotid atheroma2.676
1.141-6.278 0.024
The formation of common
3.899
1.771-8.583 0.001
carotid atheroma
Table 4. Different influences of risk factors on the occurrence of
ischemic patients
Risk factors
OR (versus female) 95%CI
P
Advanced age
2.573
1.700-3.894 0.000
Cigarette smoking
25.646
10.271-64.027 0.000
Alcohol drinking
38.103
9.265-156.707 0.000
Obesity
0.273
0.147-0.508 0.000
Family history of hypertension 0.653
0.436-0.978 0.039
Family history of stroke
0.525
0.297-0.929 0.027
Kidney disease
2.972
1.103-8.006 0.031
Hypercholesterolemia
0.560
0.392-0.779 0.001
Low HDL level
1.535
1.060-2.223 0.023
Ischemic ECG changes
0.476
0.289-0.784 0.004
2
13.368
5.135
0.859
8.598
9.201
9.718
13.323
0.302
4.714
0.041
6.577
1.820
9.064
8.423
5.742
9.764
0.335
9.283
2.856
0.539
5.466
50.031
7.684
0.249
0.087
11.424
9.217
16.147
6.351
0.107
2.831
P
0.000
0.023
0.354
0.003
0.001
0.002
0.000
0.583
0.030
0.841
0.010
0.177
0.003
0.004
0.017
0.002
0.744
0.002
0.129
0.624
0.016
0.000
0.006
0.618
0.769
0.001
0.002
0.000
0.011
0.744
0.092
stroke were more obvious in females than in males. We
also calculated odds ratio of the incidence of hemorrhagic
stroke in men versus in women. The data showed that
male patients with cigarette smoking (OR=27.270),
alcohol drinking (OR=7.686) and female patients with
hypertriglyceridemia (OR=0.285) were more susceptible
to hemorrhagic stroke.
DISCUSSION
There are some non-modifiable risk factors of stroke,
such as age, sex, race and family history. It was reported
that the risk of stroke doubles in each successive decade
after 55 years of age.[7] The cumulative effects of aging on
the cardiovascular and cerebrovascular systems and the
progressive nature of stroke risk factors over a prolonged
period of time substantially increase the risk of stroke. In
this study we found that the incidence of ischemic stroke
in males over 55 years or in females over 65 years was
2.122 times higher than that of hemorrhagic stroke. The
result suggested that the factor of advanced age was more
important to ischemic stroke. Stroke, either ischemic or
hemorrhagic, is more prevalent in men than in women.
Lifestyle differences, such as cigarette smoking and
www.wjem.org
22 Zhang et al
alcohol drinking, may help explain this sex disparity. In
addition, there is no vascular protection of endogenous
estrogen in males and it may contribute to the risk of
stroke in men. Both paternal and maternal history of
stroke may contribute to the increasing risk of stroke. This
risk could be mediated through a variety of mechanisms.
In contrast to a recent study[8], our patients came from
East China, and of all, only family history of stroke was
the risk factor for ischemic stroke, while family history of
hypertension was the risk factor for hemorrhagic stroke.
There was no significant difference in the distribution of
family history of DM and family history of CAD between
the two types of stroke. It was suggested that differences
existed in family history among stroke patients from
different regions.
Hypertension, DM, AF, dyslipidemia and hyperfibrinogenemia, and so on are changeable risk factors for
stroke.[1,9] Reports showed that hypertension was the most
important independent risk factor for both ischemic and
hemorrhagic stroke, and that 50%-60% of patients with
stroke were triggered by hypertension, especially when
combined with increased pulse pressure.[10,11] Furthermore,
hypertension was more correlated with ischemic stroke
than hemorrhagic stroke in our study as similarly reported
elsewhere. Besides hypertension, AF was another basic
risk factor for stroke.[12] The patients with AF accounted
for 3%-5% of stroke patients per annum and there was
a nearly 6-fold increase in stroke prevalence among AF
patients.[13] We also found AF played an important role in
ischemic stroke versus hemorrhagic stroke (OR=3.407).
Cigarette smoking and alcohol drinking have long
been recognized as major risk factors for stroke. Their
pathophysiological effects are multifactorial, involving
both systemic vasculature and blood rheology. So far
it is still controversial whether the effects of cigarette
smoking and alcohol drinking on ischemic stroke are
consistent with those on hemorrhagic stroke. The data
from our study exhibited that hemorrhagic patients had
a higher prevalence of alcohol drinking than ischemic
patients, and there was a significant difference between
them. Abnormalities of serum lipids (triglycerides,
cholesterol and HDL) have traditionally been regarded
as a risk factor for coronary artery disease but not for
cerebrovascular disease. However, recent studies have
clarified the relationship between lipids and ischemic
stroke, and showed that the risk of ischemic stroke[14,15]
and the size of carotid atheroma can be reduced by
cholesterol-lowering medications.[6] Nevertheless, China
Guidelines of Hypertension Updated 2005 estimate that
hypocholesterolemia (TC<140 mg/dL) may increase the
www.wjem.org
World J Emerg Med, Vol 2, No 1, 2011
risk of hemorrhagic stroke.[16] In a large cohort of elderly
patients, [17] low triglycerides levels were associated
with an increased risk of hemorrhagic stroke. In our
study, the conclusion was discrepant. In East China,
a low level of HDL was much more closely related to
ischemic stroke risk (OR=1.535). There was no significant
difference in the prevalence of hypertriglyceridemia and
hypercholesterolemia between ischemic and hemorrhagic
patients. A larger-sample investigation is necessary to
confirm this finding. Obesity predisposes to cardiovascular
disease in general and to stroke in particular. However,
obesity prevalence increases with advancing age, and
obesity is associated with increased blood pressure, blood
sugar, and blood lipids. On the basis of these associations,
it is not surprising that obesity would be related to an
increased risk of stroke.[1] Our finding was similar to
that of other research in China.[18] In the risk factors,
the prevalence of obesity was inappreciable (9.44% in
ischemic patients and 1.97% in hemorrhagic patients) and
it was more contributive in ischemic patients.
Reports showed that carotid stenoses >50% were
detected in 7% of males and 5% of females 65 years
old in healthy people and in 45% of patients with stroke
associated with carotid stenosis of varying degree.[5,7]
We found that carotid atheroma and vertebral artery
stenosis may increase the risk of ischemic stroke.
Previously the relationship between ECG results and risk
of stroke was investigated because of non-specificity.
Because of the risk of stroke may be increased by
changing hemodynamics, we observed two types of
ECG phenomena, ischemic ECG changes and ECG
arrhythmia. Unfortunately, no positive result was found.
Atherosclerosis, the most common cause of stroke,
is believed to be a disease of chronic inflammation. A
recent study revealed that the risk of stroke recurrence
of patients with WBC>8.2109 /L in a week after stroke
was significantly higher than that of patients with
WBC<5.9109/L (OR=1.56).[19] In our study the risk factor
of increased WBC (WBC>10109/L) was associated with
hemorrhagic stroke. Its prevalence in hemorrhagic patients
was significantly higher than that in ischemic patients
(40.79% vs. 14.63%).
Helicobacter pylori (H. pylori) infection may cause
atherosclerotic stroke.[20] The mechanism has not yet been
well recognized and it is probably stroke triggered by
reducing the stability of atherosclerotic plaque through
inflammatory reaction and regulation of blood lipids.
A clinical study [21] indicated that hyperuricemia may
independently elevate the risk of ischemic stroke (hazard
ratio, 1.27 per additional 0.1 mmol/L; 95% CI, 1.18 to
World J Emerg Med, Vol 2, No 1, 2011
1.36; P<0.001). One of the limitations of this study is the
incompleteness of data due to the short study period and
its retrospective design. Some factors such as H. pylori
infection and hyperuricemia were not taken into full
consideration in the early study period.
In East China, high blood pressure is closely related
to hemorrhagic stroke. Therefore, blood pressure
control plays a vital role in prevention of the disease.
Since ischemic stroke is a kind of disease involving
multiple risk factors, it should be prevented in a
comprehensive way. In the people with a high risk of
stroke, interventions of their lifestyle and low-to-high
medication are required to ensure an economic and
efficient intervention for stroke in addition to health
education as well as enhanced control and monitoring of
the risk factors.
Although there were some defects in this study, the
regional characteristics of the results at least may be
helpful in dealing with the risk factors for stroke and its
primary prevention in East China population.
Funding: This study was supported by the Natural Science
Foundation of Jiangsu Province, China.
Ethical approval: The research protocol was reviewed and
approved by the institutional review board of Nanjing Medical
University.
Conflicts of interest: No benefits in any form have been received
or will be received from a commercial party related directly or
indirectly to the subject of this article.
Contributors: Zhang J proposed the study and wrote the paper.
All authors contributed to the design and interpretation of the study
results and to further drafts of the paper. Zhang JS is the guarantor.
REFERENCES
1 WHO. Global burden of disease 2002: deaths by age, sex and
cause for the year 2002. Geneva Switzerland: World Health
Organization, 2003.
2 Liu M, Wu B, Wang WZ, Lee LM, Zhang SH, Kong LZ. Stroke
in China: epidemiology, prevention, and management strategies.
Lancet Neurology 2007; 6: 456-464.
3 Jia Q, Liu LP, Wang YJ. Risk factors and prevention of stroke in
the Chinese population. J Stroke Cerebrovasc Dis 2010 Jul 24.
[Epub ahead of print]
4 Thomas GN, Chan P, Tomlinson B. The role of angiotensin II
type 1 receptor antagonists in elderly patients with hypertension.
Drugs Aging 2006; 23: 131-155.
5 Shi KL, Wang JJ, Li JW, Jiang LQ, Mix E, Fang F, et al. Arterial
ischemic stroke: experience in Chinese children. Pediatr Neurol
2008; 38: 186-190.
6 Liu XF ,Van Melle G, Bogousslavsky J. Analysis of risk factors
in 3901 patients with stroke. Chin Med Sci J 2005; 20: 35-39.
23
7 Goldstein LB, Adams R, Becker K, Furberg CD, Gorelick PB,
Hademenos G, et al. Primary prevention of ischemic stroke: a
statement for healthcare professionals from the Stroke Council
of the American Heart Association. Circulation 2001; 103: 163.
8 Li Z, Sun L, Zhang H, Liao Y, Wang D, Zhao B, et al. Elevated
plasma homocysteine was associated with hemorrhagic and
ischemic stroke, but methylenetetrahydrofolate reductase gene
C677T polymorphism was a risk factor for thrombotic stroke:
a Multicenter Case-Control Study in China. Stroke 2003; 34:
2085-2090. Epub 2003 Aug 7.
9 Green DM, Ropper AH, Kronmal RA, Psaty BM, Burke GL.
Cardiovascular Health Study. Serum potassium level and dietary
potassium intake as risk factors for stroke. Neurology 2002; 59:
314-320.
10 Rodgers H, Greenaway J, Davies T, Wood R, Steen N, Thomson
R. Risk factors for first-ever stroke in older people in the north
East of England: a population-based study. Stroke 2004 ; 35: 7.
11 Sara Hocker MD, Sarkis Morales-Vidal MD. Management of
arterial blood pressure in acute ischemic and hemorrhagic stroke.
Neurologic Clinics 2010; 28: 863-886
12 Kayhan C, Daffertshofer M, Mielke O, Hennerici M, Schwarz S.
Comparison between German and Turkish descent in ischemic
stroke. Risk factors, initial findings, rehabilitative therapy, and
social consequences. Nervenarzt 2007; 78:188-192.
13 Kalra L, Perez I, Melbourn A. Risk assessment and
anticoagulation for primary stroke prevention in atrial fibrillation.
Stroke 1999; 30: 1218.
14 de Craen AJ, Blauw GJ, Westendorp RG. Cholesterol and risk of
stroke: cholesterol, stroke, and age. BMJ 2006; 333: 148.
15 Smith EE, Abdullah AR, Amirfarzan H, Schwamm LH. Serum
lipid profile on admission for ischemic stroke: failure to meet
National Cholesterol Education Program Adult Treatment Panel
(NCEP2ATPIII) guidelines. Neurology 2007; 68: 660-665.
16 National Committee of the Chinese People's Political
Consultative Conference. China Guideline of Hypertension
Updated 2005. Chin J Hypertension 2005; 12: 1-53.
17 Bonaventure A, Kurth T, Pico F, Barberger-Gateau P, Ritchie K,
Stapf C, et al. Triglycerides and risk of hemorrhagic stroke vs.
ischemic vascular events: The Three-City Study. Atherosclerosis
2010; 210: 243-248. Epub 2009 Nov 10.
18 Larrue V, von Kummer R R, Mller A, Bluhmki E. Risk factors
for severe hemorrhagic transformation in ischemic stroke
patients treated with recombinant tissue plasminogen activator:
a secondary analysis of the European-Australasian Acute Stroke
Study (ECASS II). Stroke 2001; 32: 438-441.
19 Grau AJ, Boddy AW, Dukovic DA, Buggle F, Lichy C, Brandt T,
et al. Leukocyte count as an independent predictor of recurrent
ischemic events. Stroke 2004; 35: 1147-1152.
20 Majka J, Rg T, Konturek PC, Konturek SJ, Bielaski W,
Kowalsky M, et al. Influence of chronic Helicobacter pylori
infection on ischemic cerebral stroke risk factors. Med Sci Monit
2002; 8: CR675-CR684.
21 Weir CJ, Muir SW, Walters MR, Lees KR. Serum urate as an
independent predictor of poor outcome and future vascular
events after acute stroke. Stroke 2003; 34: 1951-1956.
Received June 10, 2010
Accepted after revision November 6, 2010
www.wjem.org
Você também pode gostar
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Management of DVT: Soheir Adam, MD, MSC, Frcpath Asst. Professor & Consultant Hematologist KauDocumento46 páginasManagement of DVT: Soheir Adam, MD, MSC, Frcpath Asst. Professor & Consultant Hematologist KauLulu SupergirlAinda não há avaliações
- Cardiac Case Study NDDocumento11 páginasCardiac Case Study NDapi-313165458Ainda não há avaliações
- 4 - Arterial & Venous UlcersDocumento86 páginas4 - Arterial & Venous Ulcerscharity kalinowsky100% (13)
- BMC Medical Genetics: Pathogenesis of Vestibular Schwannoma in Ring Chromosome 22Documento7 páginasBMC Medical Genetics: Pathogenesis of Vestibular Schwannoma in Ring Chromosome 22Lulu SupergirlAinda não há avaliações
- Kurth 2002Documento11 páginasKurth 2002Lulu SupergirlAinda não há avaliações
- Role of Diffusion-Weighted Imaging and Proton MR Spectroscopy in Distinguishing Between Pyogenic Brain Abscess and Necrotic Brain TumorDocumento7 páginasRole of Diffusion-Weighted Imaging and Proton MR Spectroscopy in Distinguishing Between Pyogenic Brain Abscess and Necrotic Brain TumorLulu SupergirlAinda não há avaliações
- Non-Traumatic Primary Intraventricular Hemorrhage: Sang Wook Ahn, MD・Sung-Kyun Hwang, MDDocumento6 páginasNon-Traumatic Primary Intraventricular Hemorrhage: Sang Wook Ahn, MD・Sung-Kyun Hwang, MDLulu SupergirlAinda não há avaliações
- Impact StrokeDocumento12 páginasImpact StrokeLulu SupergirlAinda não há avaliações
- Guideline 9BDocumento20 páginasGuideline 9BLulu SupergirlAinda não há avaliações
- Evoked Potentials: Principles and TechniquesDocumento5 páginasEvoked Potentials: Principles and TechniquesLulu SupergirlAinda não há avaliações
- PE Sciatica Ianeuro2Documento2 páginasPE Sciatica Ianeuro2Lulu SupergirlAinda não há avaliações
- Sciatic NerveDocumento2 páginasSciatic NerveLulu SupergirlAinda não há avaliações
- Your Guide To Succeed in Saudi LicenseDocumento2.179 páginasYour Guide To Succeed in Saudi LicenseHassan Al SinanAinda não há avaliações
- Vascular AnomaliesDocumento5 páginasVascular AnomaliesGlenda DavisAinda não há avaliações
- Heart PDFDocumento13 páginasHeart PDFPranshul KapoorAinda não há avaliações
- Handout 7 Peripheral Vascular Disorders PDFDocumento9 páginasHandout 7 Peripheral Vascular Disorders PDFGrape JuiceAinda não há avaliações
- The Endovascular Management of Ruptured Abdominal Aortic AneurysmsDocumento12 páginasThe Endovascular Management of Ruptured Abdominal Aortic AneurysmsDiilAinda não há avaliações
- Mitral Stenosis (MS) X Mitral Regurgitasi (MR)Documento25 páginasMitral Stenosis (MS) X Mitral Regurgitasi (MR)Nur Faydotus SalsabilaAinda não há avaliações
- Jurnal Internasional Pda. Kelompok 1Documento17 páginasJurnal Internasional Pda. Kelompok 1Tesalonika KarundengAinda não há avaliações
- Examination Heart Sounds and MurmursDocumento52 páginasExamination Heart Sounds and MurmursAnmol KudalAinda não há avaliações
- Cath PCI EdukasiDocumento7 páginasCath PCI EdukasiAgnesthesiaAinda não há avaliações
- Blood Supply of Bones: DR Thouseef A Majeed MS Ortho PG VMKVMCH SalemDocumento40 páginasBlood Supply of Bones: DR Thouseef A Majeed MS Ortho PG VMKVMCH SalemifrazameerAinda não há avaliações
- PY6030 Term 1Documento13 páginasPY6030 Term 1AlexaJoiceJumao-AsAinda não há avaliações
- Recent Advances in OtorhinolaryngologyDocumento22 páginasRecent Advances in OtorhinolaryngologyInderdeep Arora100% (1)
- Congenital Heart Surgery: The Appropriate Diagnosis Is Achieved byDocumento9 páginasCongenital Heart Surgery: The Appropriate Diagnosis Is Achieved byprofarmahAinda não há avaliações
- Med-Surge Study GuideDocumento39 páginasMed-Surge Study Guidefbernis1480_11022046Ainda não há avaliações
- Coronary Circulation FDocumento36 páginasCoronary Circulation FjefferyAinda não há avaliações
- Tips Vs BrtoDocumento11 páginasTips Vs BrtoCsiszár MártonAinda não há avaliações
- NCP Ineffective Tissue PerfusionDocumento4 páginasNCP Ineffective Tissue PerfusionSteffiAinda não há avaliações
- Arteritis TakayasuDocumento7 páginasArteritis TakayasuGina ButronAinda não há avaliações
- Echocardiography in Heart Failure: A Guide For General PracticeDocumento6 páginasEchocardiography in Heart Failure: A Guide For General PracticesavitageraAinda não há avaliações
- No Risk ScoreDocumento4 páginasNo Risk ScorehenrisaatjianAinda não há avaliações
- Thromboangiitis ObliteransDocumento5 páginasThromboangiitis Obliteransklinik mandiriAinda não há avaliações
- 3 Renal Vascular Disease 3Documento46 páginas3 Renal Vascular Disease 3Coy NuñezAinda não há avaliações
- AP Biology Lab Ten: Physiology of The Circulatory SystemDocumento8 páginasAP Biology Lab Ten: Physiology of The Circulatory SystemCoolAsianDude75% (4)
- Cardiac Physiology Dissertation IdeasDocumento6 páginasCardiac Physiology Dissertation IdeasBuyAPhilosophyPaperUK100% (2)
- Emergency Radiology Course - Brain, Not Bleed: 4 Review QuestionsDocumento3 páginasEmergency Radiology Course - Brain, Not Bleed: 4 Review QuestionsEmaardiantariAinda não há avaliações
- Lesson PlanDocumento4 páginasLesson PlanKirti kittuAinda não há avaliações
- A Tachycardia Using A Decrementally Conducting Concealed Accessory Pathway 2015Documento5 páginasA Tachycardia Using A Decrementally Conducting Concealed Accessory Pathway 2015Võ Từ NhấtAinda não há avaliações
- Edexcel Circulary System Past Paper Questions 1Documento10 páginasEdexcel Circulary System Past Paper Questions 1binura desilvaAinda não há avaliações