Escolar Documentos
Profissional Documentos
Cultura Documentos
Obgyn PDF
Enviado por
Sandhya Putri ArisantiDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Obgyn PDF
Enviado por
Sandhya Putri ArisantiDireitos autorais:
Formatos disponíveis
L**e_SS,h#.0t-osgZ.xX:F?'b4!I{rio+>wh1tE|;_;PfeP<.
s0,'-
<m:e.0'rX,AwS+"-JG4t-rsit,{;3Ss*eb==S.>jEEM3.t_sw*<_i-;';ris:w,S.Z1
_@.:w,"o$*-C.AN};
gi,.:rkE70rtsf.!,-'S^ c.',
..
+ l:
Tract Infection during
Pregnancy: Its Association with
Maternal Morbidity and Perinatal
Outcome
Urinary
t^7S-e; "
it
:.
.t.:
s:
.S ;f,
2{
-;
'S M is ,- p
.i.-l . s
,:#
.^^,
;,t';.
;4t,Qj.
..............
..
',}
4, X
B t>R.iF'-+.'S
bR" ..
';
....
> -; +.
<- -! >-- et s
fU;
.;
;j_t4b
e;3tg'
!.!6
*ilgg-'4
'>;ffiffi
i2x?;Q
*.,
-sz,.g
...
* { X tS
s z__d.s .
*; :,; 4=s..i e*. .:.
v
2' ;'Sx {s v*'s i
*;
--
..
,w, ?..
.$*
':
-. .> -
t S;, s 8
.4 s e-
..
...
t ,,';
-sS
:.
;'
S\^,7el;
;'
"
^ "
''
.t
..
Introduction
Despite a plethora of research since
Kass first noted an association between
untreated urinary tract infection and
perinatal mortality in 1962,1 the extent
to which antepartum urinary tract infection affects maternal and perinatal health
remains ambiguous. At present, the only
certain conclusion is that the risk of
progression to pyelonephritis greatly
increases during pregnancy, with rates as
high as 30% reported among untreated
women.1-7
*ito
fi;hD .\-
t.
->'.
.24
*E
*|
Laura A. Schieve, MS, Arden Handler, DrPH, Ronald Hershow, MD,
Victoria Persky, MD, and Faith Davis, PhD
::
Antepartum urinary tract infection
has also been implicated as a risk factor
for adverse perinatal outcomes-premature birth and/or low birthweightl,3-5'7-14
and perinatal deathl"4'9-in numerous
observational studies. However, an equal
number of negative findings have been
reported.2'6"15-28 Results of clinical trials
examining the effect of antibiotic treatment on reducing the risk of low
birthweight have been inconsistent as
well.1'3'4'7'9'10 In addition, associations
have been documented between antepartum urinary tract infection and a variety
of maternal complications of pregnancy,
including hypertension/preeclampsia,4'5,7,8"17
anemia,8'9"15'22 amnionitis,21 and endometritis.29 The causal nature of these
associations is questionable, because it is
not always clear whether an episode of
urinary tract infection preceded the
particular outcome of interest, especially
in regard to maternal hypertension and
anemia. Although the definitions of
these outcomes in many studies render it
difficult to determine the proper sequence of events, a temporal relationship between urinary tract infection and
hypertension was clearly established by
Stuart et al.,5 and a temporal relationship between urinary tract infection and
anemia was established by Brumfitt.9
These results support possible causal
relationships. As with the perinatal
outcomes, many investigators have also
failed to demonstrate any effect with
urinary tract infection and maternal
outcomes.2'6'11'16'20,2427 Limited sample
sizes and inadequate control of confounders may partially explain the discrepancy in findings to date.
This study used registry data to
examine associations between antepartum urinary tract infection and adverse
maternal and perinatal outcomes independent of other possible risk factors.
The large sample size afforded by the
registry also provided an opportunity to
evaluate possible mechanisms through
which urinary tract infection might exert
an effect on pregnancy outcome.
Methods
We performed a retrospective cohort analysis with data from the University of Illinois Perinatal Network database, a registry of more than 150 000
obstetric events occurring from 1983
through 1989 in 14 hospitals in the
Chicago area. Trained personnel abstracted more than 450 maternal, fetal,
and neonatal variables from patients'
medical records upon completion of
pregnancy. We limited our analysis to
1988 and 1989 because of changes in
abstracting format. We also limited the
analysis to the four hospitals with the
The authors are with the School of Public
Health, University of Illinois at Chicago.
Requests for reprints should be sent to
Laura A. Schieve, MS, Program in Epidemiology and Biostatistics, School of Public Health,
University of Illinois at Chicago, PO Box
6998, Chicago, IL 60680.
This paper was accepted June 2, 1993.
ft
Ji i*4'8d'Sj Nb sr
b s
American Journal of Public Health 405
Schieve et al.
largest obstetric populations to allow a
feasible reabstraction of a subset of
records, in order to assess the exposure
classification more thoroughly. All singleton live births and fetal deaths were
included, with the exception of 115
subjects for whom information on urinary tract infection was not recorded
(0.4% of the sample). In all, 25 746
women were included in this analysis;
1988 (7.7%) were considered positive for
antepartum urinary tract infection and
constituted the exposure group. The
remainder constituted the nonexposed
group.
Classification of urinary tract infection was based on (1) a positive urine
culture during the antepartum period, as
noted by a health care provider and
recorded in the medical record, or (2) a
diagnosis of urinary tract infection and/or
pyelonephritis during the antepartum
period recorded in the medical record.
This allowed inclusion of cases of urinary tract infection diagnosed by a
variety of methods, including culture,
rapid-screening techniques, and clinical
presentation. In most cases, it was not
possible to discern the way in which a
diagnosis was made from the information provided in the record. Our definition of urinary tract infection encompassed both asymptomatic and
symptomatic infections because it included those individuals for whom a
positive culture was recorded without a
stated diagnosis of urinary tract infection. However, we were unable to determine the proportion of our exposed
group that was symptomatic from the
information provided.
The perinatal outcomes examined
in this study include perinatal death
(fetal death or neonatal death within the
first 28 days of life, providing that the
infant had not been discharged from the
hospital), low birthweight (2500 g or
lower) prematurity (less than 37 weeks
gestation), preterm low birthweight (2500
g or lower and less than 37 weeks
gestation), and small for gestational age
(birthweight less than the 10th percentile of the birthweight distribution of the
singleton deliveries in the database at
each gestational age and infant sex).
Maternal outcomes evaluated include premature labor (onset of labor
prior to 37 weeks of gestation, even if the
episode was resolved and the pregnancy
went to term), hypertension/preeclampsia (diagnosis of pregnancy-induced hypertension or preeclampsia specified by
a health care provider), anemia (hemato406 American Journal of Public Health
crit less than 30%), amnionitis (diagnosis of amnionitis, chorioamnionitis, membranitis, or placentitis), and endometritis
(diagnosis of endometritis or endomyometritis). Because the exact timing of
maternal complications was not recorded for this data set, it is unknown
whether an episode of urinary tract
infection actually preceded each of these
outcomes. Therefore, this study is actually cross-sectional with respect to the
maternal outcomes.
Because sexual intercourse is a risk
factor for both urinary tract and genital
tract infections and since genital tract
infections may also be associated with
adverse reproductive outcome, the detection of one or more genital tract pathogens during the antepartum period
(syphilis, gonorrhea, genital herpes, condyloma, chlamydia, Beta Streptococcus
vaginal infection, Candida albicans,
Trichomonas vaginalis, Gardnerella vaginalis, unspecified vaginitis or cervicitis)
was treated as a potential confounder in
this analysis. Since ascertainment of
antepartum urinary tract infection may
have varied by hospital, odds ratios were
also adjusted for hospital of delivery.
Other variables evaluated as potential
confounders include age ( < 20, 20
through 29, 2 30 years), race/ethnicity
(White/Asian/other, Black, Hispanic),
and prior pregnancy history. Pregnancy
history was classified as follows: (1)
primigravida, (2) at least one pregnancy
ending in adverse outcome (congenital
anomaly; fetal, neonatal, or postneonatal death; ectopic pregnancy or hydatid
mole; spontaneous abortion; premature
birth; or term birth with intrauterine
growth retardation), (3) at least one
pregnancy ending in induced abortion
and no others ending in adverse outcomes or (4) all pregnancies ending in
healthy outcomes (term births with no
congenital anomalies or growth retardation).
Odds ratios (ORs) and 95% testbased confidence intervals (CIs) were
computed for exposure to antepartum
urinary tract infection and all perinatal
and maternal outcomes. Mantel-Haenszel adjusted odds ratios were estimated
from stratified analyses of all associations controlling for each of the potential confounders individually.30 These
summary estimates were evaluated with
Breslow-Day tests of homogeneity.
Unconditional logistic regression
was used to simultaneously adjust for
age, race, prior pregnancy history, hospital of delivery (A, B, C, or D), and
antepartum genital tract infection for
each outcome. In addition, because
univariate analysis revealed that the risk
estimate for urinary tract infection and
perinatal death was not homogeneous
with respect to age, urinary tract infection and age interaction terms were
entered into the model with perinatal
death. Odds ratios were calculated from
beta coefficients, and 95% confidence
intervals were calculated from the respective standard errors.31
Because any association between
urinary tract infection and adverse reproductive outcome may vary by the severity
of infection, we repeated our analysis
after subdividing the exposure group by
progression to pyelonephritis. This analysis is presented only for the perinatal
outcomes, however, since the number of
subjects with both pyelonephritis and
one of the maternal outcomes under
study was very small and odds ratios
were difficult to interpret. The relationship between the timing of infection and
each outcome variable would also be of
interest. Unfortunately, the data to
address this issue were not available.
We also explored possible mechanisms by which urinary tract infection
might affect perinatal outcome. Hypertension, anemia, and amnionitis were
evaluated as possible intermediaries in
the association between urinary tract
infection and adverse perinatal outcome, because each of these conditions
has been previously implicated as a
consequence of antepartum urinary tract
infection4,5'7-9'15'17'21'= and a risk factor
for adverse perinatal outcome.32-35 These
analyses were limited to preterm low
birthweight, the outcome with which
urinary tract infection appeared most
strongly associated, because any effect
would be most likely with this association. We repeated both crude and
multivariable analyses, excluding subjects with each of the postulated intermediary variables to assess whether the
associations persisted in their absence.
Finally, in an effort to discern
whether urinary tract infection per se is
a risk factor for preterm low birthweight
or whether the infectious process in
general creates risk, the effect of urinary
tract infection was compared with other
infections commonly acquired by women
of childbearing age, specifically genital
and upper respiratory tract infections.
The study population was divided into
five mutually exclusive exposure groups:
urinary tract infection only, genital tract
infection only, upper respiratory tract
March 1994, Vol. 84, No. 3
Urinary Tract Infections
infection only, multiple infections (more
than one of these three infections), and
none of these infections. Odds ratios
were calculated for each exposure group
and preterm low birthweight, with the no
infection group as the reference category.
Results
As shown in Table 1, the exposure
groups were not homogeneous with
respect to the potential confounding
variables under study. Subjects classified
in the urinary tract infection category
were more likely than those in the
nonexposed group to be non-White, to
be younger, to have delivered at hospital
D, and to have had an antepartum
genital tract infection. They were less
likely to have had a prior pregnancy that
ended in a healthy outcome.
Women exposed to antepartum urinary tract infection were found to be at
greater risk (unadjusted) of delivering
infants with low birthweights, premature
infants, preterm infants with low birthweights, and infants small for gestational
age than those who were not exposed
(Table 2). They were also more likely to
experience premature labor, hypertension/preeclampsia, anemia, and amnionitis during pregnancy. Although the
perinatal mortality and endometritis
rates were higher among the exposure
group, these differences did not reach
statistical significance.
The risk of urinary tract infection
on adverse perinatal outcomes was greatest among those with the most severe
infection, pyelonephritis (Table 3). However, because only a small percentage of
subjects (8.1%) progressed to pyelonephritis, the odds ratios after excluding
these subjects from the exposure group
were virtually the same as when exposure was defined as both pyelonephritis
and nonpyelonephritis cases of urinary
tract infection combined.
After single-factor adjustment for
age, race, hospital of delivery, prior
pregnancy history, and genital tract
infections, all statistically significant associations in the crude analysis, with the
exception of the urinary tract infectionsmall for gestational age association,
remained elevated (data not shown). A
significant association was also found
between urinary tract infection and
perinatal death when maternal age was
between 20 and 29 years.
Multivariable adjustment reduced
the risk estimates, but the associations
March 1994, Vol. 84, No. 3
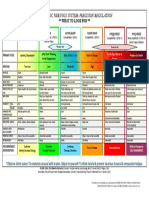
TABLE 1 Selected Characteristics of Study Subjects, by Exposure to
Antepartum Urinary Tract Infection
Characteristic
Race*
White/Asian/other
Black
Hispanic
Age*
<20
20-29
30+
Hospital of delivery*
A
B
C
D
Prior pregnancy history*
Primigravida
Previous adverse outcome
Induced abortion (no adverse outcome)
All healthy outcomes
Genital tract infection*
Exposed
(n = 1988), %
Nonexposed
(n = 23 758), %
28.7
30.1
41.1
47.0
17.8
35.3
22.6
57.5
19.9
13.9
54.5
31.6
17.5
28.9
15.3
38.3
36.6
25.5
15.9
22.1
30.7
27.4
11.9
30.0
21.2
29.4
24.0
10.0
36.7
11.3
*P < .001 by chi-square test for proportional differences for comparison between exposure groups.
between antepartum urinary tract infection and low birthweight, prematurity,
preterm low birthweight, premature labor, hypertension, anemia, and amnionitis remained statistically significant
(Table 4). As in the univariate analysis,
the small for gestational age adjusted
odds ratio was not significant, and the
adjusted odds ratio for perinatal death
was significant only for those 20 to 29
years old.
Neither the crude nor the adjusted
odds ratio was modified when hypertension, anemia, or amnionitis cases were
deleted from the urinary tract infectionpreterm low birthweight analyses (adjusted OR excluding hypertension = 1.4,
95% CI = 1.2, 1.7; adjusted OR excluding anemia = 1.5, 95% CI = 1.2, 1.8;
adjusted OR excluding amnionitis = 1.4,
95% CI = 1.1, 1.7). The risk of preterm
low birthweight was virtually the same
for women with an antepartum urinary
tract infection only, an antepartum genital tract infection only, or both types of
infection (Table 5). (Because of the
unstable estimates from the multivariable analyses, only the unadjusted estimates are presented.) Women exposed
to upper respiratory tract infection only
were at no greater risk of delivering
preterm low-birthweight infants than
were those in the "infection-free" group.
Discussion
We found that women who acquire
urinary tract infections during pregnancy are at increased risk of delivering
low-birthweight, premature, and preterm low-birthweight infants. Our odds
ratios of 1.4 for low birthweight, 1.3 for
prematurity, and 1.5 for preterm low
birthweight compare well with a recent
meta-analysis of exposure to antepartum
urinary tract infection that reported
typical relative risks of 1.5 and 2.0 for
associations with low birthweight and
prematurity, respectively.36 Antepartum
urinary tract infection was not associated with delivering infants small for
gestational age after multivariable adjustment for potential confounding variables, suggesting that urinary tract infection affects low birthweight through
premature delivery rather than growth
retardation. This is further illustrated by
the relatively strong association between
urinary tract infection and premature
labor. Antepartum urinary tract infection was also found to be associated with
increased maternal morbidity (hypertension, anemia, and amnionitis).
An association between urinary tract
infection and perinatal death was found
only among the 20- to 29-year-olds. One
plausible explanation is that younger
American Journal of Public Health 407
Schieve et al.
TABLE 2-Unadjusted Odds Ratios for Exposure to Antepartum Urinary Tract
Infection and Selected Perinatal and Maternal Outcomes
Odds
Outcome
Nonexposed
Exposed
Ratio
95% Confidence
Interval
Perinatal
Perinatal death
Yes
No
Birthweight, g
<2500
>2500
Gestational age, wk
<37
.37
Preterm low birthweight
Yes
No
Small for gestational age
Yes
No
32
1 956
291
23467
13
1.3
09,9
225
1 759
1 779
21 942
16
1.4,1.8
293
1 687
2 546
21 137
1.4
1.3,1.6
155
1 821
1 144
22 505
1.7
1.4, 2.0
258
1 717
2 529
21 108
13
1
1.1
1,.1.4
0.9,1.9
Maternal
Premature labor
Yes
No
Hypertension
Yes
No
Anemia
Yes
No
Amnionitis
Yes
No
Endometritis
Yes
No
2211
21 547
1.8
1.6, 2.0
1 679
122
973
22 785
1.5
1.3,1.9
1 862
123
716
23 042
2.1
1.8, 2.6
1 861
54
1 929
413
234311
1612
306
25
203
1 957
23 525
1.6
1.2,2.1
1.5
1.0, 2.2
Note. Subjects missing information on an outcome variable are not included in that analysis. The
maximum number missing is 134 (small for gestational age).
TABLE 3-Association between Antepartum Urinary Tract Infection and Selected
Perinatal Outcomes, by Progression to Pyelonephritis
Pyelonephritis
Nonpyelonephritis
Odds
Ratio
95% Confidence
Interval
Odds
Radio
95% Confidence
Outcome
Perinatal death
Low birthweight
Prematurity
Preterm low birthweight
Small for gestational age
2.6
1.9
1.9
2.5
1.5
1.1, 6.2
1.2, 2.9
1.3, 2.9
1.6, 4.0
1.0,2.3
1.2
1.5
1.4
1.6
1.2
0.8,1.8
1.3,1.8
1.2,1.6
1.3,1.9
1.1,1.4
and older women are exposed to mul-
tiple competing risks for adverse outcomes-low socioeconomic status and
related factors among the younger age
group and biological factors among the
408 American Journal of Public Health
Interval
older age group-which masks the impact of urinary tract infection.37
While several previous investigations have found comparable results,
they have suffered from small sample
sizes and were not adequately able to
control for confounding. Of particular
interest is whether the effects of urinary
tract infection are independent of other
infections with similar risk factors for
acquisition, such as sexually transmitted
diseases. We were able to adjust for
antepartum sexually transmitted diseases and other genital tract pathogens
in our analysis and did not find any
change in the odds ratios. In addition,
urinary tract infection and genital tract
infection appear to have had similar
effects on preterm low birthweight, as
evidenced by the comparable odds ratios, when each type of infection was
evaluated individually. However, we did
not distinguish the genital infection
category by specific pathogens. Our
analysis also shows that the associations
observed between urinary tract infection
and both adverse perinatal outcome and
maternal morbidity were not due to
confounding by age, race, prior pregnancy history, or hospital of delivery.
A major weakness of this study is
the method of exposure ascertainment.
While most prior investigations have
been conducted prospectively, with urine
cultures on all women under investigation available to classify urinary tract
infection, this study relied on a positive
culture result or physician diagnosis of
urinary tract infection and/or pyelonephritis in the medical record. This
retrospective classification of urinary
tract infection raised a number of concerns about the validity and reliability of
this variable. Although it was impossible
for us to assess validity directly, we
reabstracted a random sample of charts
from our study population to evaluate
the reliability of the original abstraction
process and to provide some sense of
potential limitations of the urinary tract
infection variable beyond abstraction
error. In all, 217 charts were reabstracted, 112 from the exposed group
(5%) and 105 from the nonexposed
group (0.4%).
Agreement between this second
abstraction and the original classification of urinary tract infection in the
database was 96.2% for the nonexposed
group but only 69.6% for the exposure
group. (That is, 30.4% of our exposure
group was not reclassified as having a
urinary tract infection, during the second abstraction.) Further evaluation of
these apparently misclassified subjects
revealed that the incidence of adverse
outcomes was lower in this group than
for those classified correctly as having a
March 1994, Vol. 84, No. 3
Urinary Tract Infections
TABLE 4-Adjusted Odds Ratios
for Exposure to Antepartum Urinary Tract
Infection and Selected
Perinatal and Maternal
Outcomes
Outcome
Odds
Ratio
Perinatal
Perinatal death
0.3
Age<20d
1.8
Age2G-29d
1.1
Age30+d
1.4
Low birthweight
1.3
Prematurity
Pretermlowbirth- 1.5
weight
1.1
Small for gestational age
Maternal
Premature labor 1.6
1.4
Hypertension
1.6
Anemia
1.4
Amnionitis
1.0
Endometritis
95% Confidence
Interval
0.1,1.3
1.1,2.8
0.5,2.3
1.2,1.6
1.1,1.4
1.2,11.7
0.9,1.3
1.4,1.8
1.2,1.7
1.3, 2.0
1.1, 1.9
0.6,1.5
Note. Estimates were adjusted for race,
age, prior pregnancy history, hospital of
delivery, and genital tract pathogens by
means of unconditional logistic regression. Subjects missing information on
outcome or confounding variables are
not included in that analysis. The maximum number missing is 357 (small for
gestational age). Stratum-specffic estimates were adjusted for race, prior
pregnancy history, hospital of delivery,
and genital tract pathogens.
urinary tract infection. Therefore, including these subjects in the exposure group
biased our results toward the null hypothesis, and the true associations are likely
to be stronger than our estimates indicate.
In addition to abstraction quality,
the classification of urinary tract infection used in this study is subject to a
number of other potential shortcomings.
First, if a woman did not receive
prenatal care, an episode of urinary tract
infection may have occurred during
pregnancy that went unrecorded. In
addition, even if a woman did receive
prenatal care, her prenatal care record
may not have been incorporated into her
hospital of delivery medical record,
potentially resulting in a missed case of
urinary tract infection. Our reabstraction revealed that 13.4% of our study
population did not receive prenatal care
and that the prenatal care record was
unavailable for an additional 4.8%.
March 1994, Vol. 84, No. 3
TABLE 5-Unadjusted Odds Ratios for Exposure to Antepartum Urinary Tract
Infection (UTI), Genital Tract Infection, Upper Respiratory Tract
Infection (URI), and Combinations of These Infections for
Preterm Low Birthweight
Exposure
Odds Ratio
95% Confidence Interval
Negative for all 3 infections
UTI only
Genital infection only
URI only
Multiple infections
UTI and URI
UTI and genital infection
URI and genital infection
All 3 infections
19 927
1 464
2 475
1 053
706
94
394
194
24
1.0
1.8
1.5
0.8
1.6
1.4
1.9
1.2
0.9
1.4, 2.1
1.3,1.8
0.6,1.2
1.2, 2.2
0.6, 3.3
1.3, 2.7
0.6, 2.3
0.1, 6.1
In addition to receipt of prenatal
care, we were also concerned about the
prevalence of laboratory screening for
urinary tract infection. Although most
prenatal care regimes include an antepartum urinalysis, not all routinely incorporate urine cultures. We found that
antepartum urine cultures were recorded for only 33.2% of our reabstracted sample. This is most likely an
underestimate, because it is feasible that
urine cultures performed during the
antepartum period were not always
recorded in the medical record. However, it is still cause for concern, since
urinary tract infection may be asymptomatic and urinalysis alone may be insensitive. Although these data suggest that
cases of asymptomatic urinary tract
infection may have gone undetected in
this population, any consequent bias
would again be toward the null hypothesis because comparison groups would
be more homogeneous on exposure.
Given the potential errors in classification, it is encouraging to note that the
prevalence of urinary tract infection at
each hospital under study fell within the
2% to 10% range seen in other investigations.1,3,5,6,12,15,26 This rate was actually
exceeded at one hospital that serves a
large number of indigent women, an
observation also consistent with current
literature.
Although the registry does not
contain information on antibiotic treatment for urinary tract infection, we
found, during our reabstraction, that
antibiotics were prescribed for 84.6% of
those correctly classified as having such
an infection, indicating that the exposure group involves mainly treated cases.
Assuming that the association between urinary tract infection and prematurity is real, the mechanism by which
the former might exert such an effect is
not well established. Several investigators have demonstrated a high incidence
(up to 50%) of pyelographic abnormalities, indicative of chronic pyelonephritis,
in bacteriuric women.4'38 It is plausible,
then, that the effect of urinary tract
infection on premature birth could be
indirectly mediated by occult renal abnormalities that result in antepartum maternal complications such as hypertension/
preeclampsia or anemia. Our data do
not support this hypothesis, because no
change in the odds ratio was observed
for the association between urinary tract
infection and preterm low birthweight
when women with either hypertension or
anemia were excluded from analysis. We
cannot eliminate other possible effects
of renal abnormalities, however.
It is also conceivable that urinary
tract infection affects premature labor
directly, through the development of
amnionitis. It has been previously suggested that bacterial infection of the
amniotic fluid is a risk factor for premature delivery.3435 One hypothesis contends that bacterial enzymes such as
collagenase may weaken the fetal membranes and predispose them to rupture,
which subsequently triggers the onset of
labor.39 It has also been postulated that
bacterial products such as phospholipase
A and C or endotoxins may stimulate
prostaglandin biosynthesis by the fetal
membranes, which then initiates labor.40
Alternatively, these bacterial products
might stimulate the patient's immune
system, causing the release of monokines
(particularly Platelet Activating Factor,
Interleukin-1, and Tumor Necrosis Factor) that then trigger prostaglandin
production.40 It has also been demonstrated that bacteriuric women may
subsequently develop an amniotic fluid
American Journal of Public Health 409
Schieve et al.
infection with the same organisms commonly isolated from urine specimens,
namely coliform bacteria such as Escherichia coli. 21 We found no change in the
odds ratio after deleting cases of amnionitis, although subclinical amniotic infection has been repeatedly documented4143
and may have been a latent causative
factor in this population.
Future studies are needed to address the interrelationship between urinary tract infection, amnionitis, and
premature labor. Ideally, these associations should be explored in a prospective
study with well-defined criteria for both
exposure and outcome variables.
Although the mechanism remains
unclear, these data, along with prior
investigations, indicate that antepartum
urinary tract infection indeed affects
both maternal and perinatal health, even
when treated. Early prenatal screening
of women for urinary tract infection and
treatment of women found to be bacteriuric are already indicated to prevent
progression to pyelonephritis. The associations documented here provide further compelling support for screening to
identify patients at risk for adverse
pregnancy outcomes. [
Acknowledgments
We are grateful to the University of Illinois
Perinatal Management Group for allowing us
access to the database. In addition, we would
like to thank Deborah Rosenberg and Cynthia Ferre for their assistance with computer
programming and Susan Ataman, Susan
Johnson, and Edna Brooks for their help with
data collection.
References
1. Kass EH. Pyelonephritis and bacteriuria:
a major problem in preventive medicine.
Ann Intem Med. 1962;56:46-53.
2. Bryant RE, Windom RE, Vineyard JP,
Sanford JP. Asymptomatic bacteriuria in
pregnancy and its association with prematurity. JLab Clin Med. 1964;63:224-231.
3. LeBlanc AL, McGanity WJ. The impact
of bacteriuria in pregnancy-a survey of
1300 pregnant patients. Biol Med. 1964;22:
336-347.
4. Kincaid-Smith P, Bullen M. Bacteriuria
in pregnancy. Lancet. 1965;1:395-399.
5. Stuart KL, Cummins GTM, Chin WA.
Bacteriuria, prematurity, and the hypertensive disorders of pregnancy. Br Med J.
1965;1:554-556.
6. Little PJ. The incidence of urinary infection in 5000 pregnant women. Lancet.
1966;4:925-928.
410 American Journal of Public Health
7. Wren BG. Subclinical urinary infection in
pregnancy. Med JAust. 1969;1:1220-1226.
8. Naeye RL. Urinary tract infections and
the outcome of pregnancy. Adv Nephrol.
1986;15:95-102.
9. Brumfitt W. The effects of bacteriuria in
pregnancy on maternal and fetal health.
KidneyInt. 1975;8:S113-S119.
10. Savage WE, Haj SN, Kass EH. Demographic and prognostic characteristics of
bacteriuria in pregnancy. Medicine. 1967;
46:385-407.
11. Condie AP, Williams JD, Reeves DS,
Brumfitt W. Complications of bacteriuria
in pregnancy. In: O'Grady F, Brumfitt W,
eds. Urinary Tract Infection. London,
England: Oxford University Press; 1968:
148-159.
12. Gruneberg RN, Leigh DA, Brumfitt W.
Relationship of bacteriuria in pregnancy
to acute pyelonephritis, prematurity, and
fetal mortality. Lancet. 1969;2:1-3.
13. McGrady GA, Daling JR, Peterson DR.
Maternal urinary tract infection and
adverse fetal outcomes. Am J Epidemiol.
1985;121:377-381.
14. Henderson M, Reinke WA. The relationship between bacteriuria and prematurity. In: Kass EH, ed. Progress in Pyelonephritis. Philadelphia, Pa: FA Davis; 1965:
27-32.
15. Layton R. Infection of the urinary tract in
pregnancy: an investigation of a new
routine in antenatal care. J Obstet Gynaecol Br Commonwealth. 1964;71:927-933.
16. Sleigh JD, Robertson JG, Isdale MH.
Asymptomatic bacteriuria in pregnancy. J
Obstet Gynaecol Br Commonwealth. 1964;
71:74-81.
17. Norden CW, Kilpatrick WH. Bacteriuria
of pregnancy. In: Kass EH, ed. Progress in
Pyelonephritis. Philadelphia, Pa: FA Davis;
1965:64-72.
18. Whalley PJ. Bacteriuria in pregnancy. In:
Kass EH, ed. Progress in Pyelonephritis.
Philadelphia, Pa: FA Davis; 1965:50-57.
19. Wilson MG, Hewitt WL, Monzon OT.
Effect of bacteriuria on the fetus. NEnglJ
Med. 1966;274:1115-1118.
20. Dixon HG, Brant HA. The significance of
bacteriuria in pregnancy. Lancet. 1967;1:
19-20.
21. Patrick MJ. Influence of maternal renal
infection on the foetus and infant. Arch
Dis Child. 1967;42:208-213.
22. Robertson JG, Livingstone JRB, Isdale
MH. The management and complications
of asymptomatic bacteriuria in pregnancy. J Obstet Gynaecol Br Commonwealth. 1968;75:59-65.
23. Elder HA, Santamarina BAG, Smith S,
Kass EH. The natural history of asymptomatic bacteriuria during pregnancy: the
effect of tetracycline on the clinical
course and the outcome of pregnancy.
Am J Obstet Gynecol 1971;111:441-462.
24. Schamadan WE. Bacteriuria during pregnancy. Am J Obstet GynecoL 1964;89:1015.
25. Carroll R, MacDonald D, Stanley JC.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
Bacteriuria in pregnancy. Obstet Gynecol.
1968;32:525-527.
Bobeck S, Schersten B. Detection and
diagnosis of bacteriuria in pregnancy.
Practitioner. 1974;212:257-262.
Gilstrap LC, Leveno KJ, Cunningham
FG, Whalley PJ, Roark ML. Renal
infection and pregnancy outcome. Am J
Obstet Gynecol. 1981;141:709-716.
Reddy J, Cambell A. Bacteriuria in
pregnancy. Aust NZ J Obstet Gynaecol.
1985;25:176-178.
Monif GRG. Intrapartum bacteriuria and
postpartum endometritis. Obstet Gynecol.
1991;78:245-248.
Rothman KJ. Modem Epidemiology. Boston, Mass: Little, Brown; 1986:177-236.
Hosmer DW, Lemeshow S. Applied Logistic Regression. New York, NY: Wiley;
1989:38-81.
Kramer MS, McLean FH, Eason EL,
Usher RH. Maternal nutrition and spontaneous preterm birth. Am J Epidemiol.
1992;136:574-583.
Lieberman E, Ryan KJ, Monson RR,
Schoenbaum SC. Association of maternal
hematocrit with premature labor. Am J
Obstet Gynecol. 1988;159:107-114.
Chellam VG, Rushton DI. Chorioamnionitis and funiculitis in the placentas of 200
births weighing less than 2.5 kg. Br J
Obstet Gynaecol. 1985;92:808-814.
Guzick DS, Winn K. The association of
chorioamnionitis with preterm delivery.
Obstet Gynecol. 1985;65:11-16.
Romero R, Oyarzun E, Mazor M, Sirtori
M, Hobbins JC, Bracken M. Metaanalysis of the relationship between
asymptomatic bacteriuria and preterm
delivery/low birth weight. Obstet Gynecol.
1989;73:576-582.
37. Institute of Medicine. Preventing Low
Birthweight. Washington, DC: National
Academy Press; 1985:46-93.
38. Diokno AC, Compton A, Seski J, Vinson
R. Urologic evaluation of urinary tract
infection in pregnancy. J Reprod Med.
1986;31:23-26.
39. Cox SM. Infection-induced preterm labor. In: Gilstrap LC, Faro S, eds. Infections in Pregnancy. New York, NY: Alan
R Liss Inc; 1990:247-253.
40. Romero R, Mazor M. Infection and
preterm labor. Clin Obstet Gynecol. 1988;
31:553-584.
41. Miller JM, Hill GB, Welt SI, Pupkin MJ.
Bacterial colonization of amniotic fluid in
the presence of ruptured membranes.
Obstet Gynecol. 1980;137:451-458.
42. Bobitt JR, Hayslip CC, Damato JD.
Amniotic fluid infection as determined by
transabdominal amniocentesis in patients
with intact membranes in premature
labor.AmJObstet Gynecol. 1981;140:947952.
43. Leigh J, Garite TJ. Amniocentesis and
the management of premature labor.
Obstet Gynecol. 1986;67:500-506.
March 1994, Vol. 84, No. 3
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Sandhya 1Documento8 páginasSandhya 1Sandhya Putri ArisantiAinda não há avaliações
- Acs - Sept.12Documento72 páginasAcs - Sept.12Sandhya Putri ArisantiAinda não há avaliações
- Sandhya 4Documento7 páginasSandhya 4Sandhya Putri ArisantiAinda não há avaliações
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- AnkleDocumento9 páginasAnkleSwan YeongAinda não há avaliações
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Sandhya 4Documento7 páginasSandhya 4Sandhya Putri ArisantiAinda não há avaliações
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Sandhya 5Documento4 páginasSandhya 5Sandhya Putri ArisantiAinda não há avaliações
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- Jurnal Vertigo Sandhya PDFDocumento8 páginasJurnal Vertigo Sandhya PDFSandhya Putri ArisantiAinda não há avaliações
- Respiratory Distress SyndromeDocumento16 páginasRespiratory Distress SyndromeSandhya Putri ArisantiAinda não há avaliações
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Sandhya 1Documento8 páginasSandhya 1Sandhya Putri ArisantiAinda não há avaliações
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- Respiratory Distress SyndromeDocumento16 páginasRespiratory Distress SyndromeSandhya Putri ArisantiAinda não há avaliações
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Acs - Sept.12Documento72 páginasAcs - Sept.12Sandhya Putri ArisantiAinda não há avaliações
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Jurnal Mata Sandhya PDFDocumento8 páginasJurnal Mata Sandhya PDFSandhya Putri ArisantiAinda não há avaliações
- BPT - Free MedicalDocumento8 páginasBPT - Free MedicalSandhya Putri ArisantiAinda não há avaliações
- ObatantihipertensiDocumento15 páginasObatantihipertensiSandhya Putri ArisantiAinda não há avaliações
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Jurnal Vertigo PDFDocumento5 páginasJurnal Vertigo PDFSandhya Putri ArisantiAinda não há avaliações
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Jurnal Mata Sandhya PDFDocumento8 páginasJurnal Mata Sandhya PDFSandhya Putri ArisantiAinda não há avaliações
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Respiratory Distress SyndromeDocumento16 páginasRespiratory Distress SyndromeSandhya Putri ArisantiAinda não há avaliações
- 1471 2415 14 151 PDFDocumento7 páginas1471 2415 14 151 PDFSandhya Putri ArisantiAinda não há avaliações
- UltraCal XS PDFDocumento2 páginasUltraCal XS PDFKarina OjedaAinda não há avaliações
- Sistema NervosoDocumento1 páginaSistema NervosoPerisson Dantas100% (2)
- Kera Ritual Menu - With DensifiqueDocumento8 páginasKera Ritual Menu - With Densifiquee.K.e.kAinda não há avaliações
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Peplu Theory ApplicationDocumento7 páginasPeplu Theory ApplicationVarsha Gurung100% (1)
- REACH - Substances of Very High ConcernDocumento3 páginasREACH - Substances of Very High Concerna userAinda não há avaliações
- Maria MontessoriDocumento2 páginasMaria MontessoriGiulia SpadariAinda não há avaliações
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Purpose 1Documento4 páginasPurpose 1Rizzah MagnoAinda não há avaliações
- Tiger Paint Remover SDSDocumento10 páginasTiger Paint Remover SDSBernard YongAinda não há avaliações
- Report Decentralised Planning Kerala 2009 OommenDocumento296 páginasReport Decentralised Planning Kerala 2009 OommenVaishnavi JayakumarAinda não há avaliações
- Lab Exercise 11 Urine Specimen CollectionDocumento7 páginasLab Exercise 11 Urine Specimen CollectionArianne Jans MunarAinda não há avaliações
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (120)
- Transformer Oil BSI: Safety Data SheetDocumento7 páginasTransformer Oil BSI: Safety Data Sheetgeoff collinsAinda não há avaliações
- AnumwraDocumento30 páginasAnumwratejasAinda não há avaliações
- L 65 - Prevention of Fire and Explosion, and Emergency Response On Offshore Installations - Approved Code of Practice and Guidance - HSE - 2010Documento56 páginasL 65 - Prevention of Fire and Explosion, and Emergency Response On Offshore Installations - Approved Code of Practice and Guidance - HSE - 2010Barkat UllahAinda não há avaliações
- 11 - Chapter 3Documento52 páginas11 - Chapter 3joshniAinda não há avaliações
- CelecoxibDocumento2 páginasCelecoxibXtinegoAinda não há avaliações
- Case Presentation 1Documento18 páginasCase Presentation 1api-390677852Ainda não há avaliações
- Forging An International MentorshipDocumento3 páginasForging An International MentorshipAbu SumayyahAinda não há avaliações
- MIP17 - HSE - PP - 001 Environment Management Plan (EMP) 2021 REV 3Documento40 páginasMIP17 - HSE - PP - 001 Environment Management Plan (EMP) 2021 REV 3AmeerHamzaWarraichAinda não há avaliações
- CCAC MSW City Action Plan Cebu City, PhilippinesDocumento6 páginasCCAC MSW City Action Plan Cebu City, Philippinesca1Ainda não há avaliações
- Economics Assignment (AP)Documento20 páginasEconomics Assignment (AP)Hemanth YenniAinda não há avaliações
- NitrotolueneDocumento3 páginasNitrotolueneeriveraruizAinda não há avaliações
- A Seminar Report On Pharmacy ServicesDocumento20 páginasA Seminar Report On Pharmacy Servicesrimjhim chauhanAinda não há avaliações
- Dr. Mohamed Ali Hamedh - DKA - 2023Documento25 páginasDr. Mohamed Ali Hamedh - DKA - 2023ÁýáFáŕőúgAinda não há avaliações
- Transport OshDocumento260 páginasTransport OshAnlugosiAinda não há avaliações
- Alpha-2 Adrenergic Agonists (Dexmedetomidine) Pekka Talke MD UCSF Faculty Development Lecture Jan 2004Documento53 páginasAlpha-2 Adrenergic Agonists (Dexmedetomidine) Pekka Talke MD UCSF Faculty Development Lecture Jan 2004Nur NabilahAinda não há avaliações
- 863-5-Hylomar - Univ - MSDS CT1014,3Documento3 páginas863-5-Hylomar - Univ - MSDS CT1014,3SB Corina100% (1)
- ED Produk KF - KF (Nama Apotek)Documento19 páginasED Produk KF - KF (Nama Apotek)Eko FebryandiAinda não há avaliações
- Biological Spill Clean UpDocumento5 páginasBiological Spill Clean UpNAMPEWO ELIZABETHAinda não há avaliações
- An Introduction To PrescribingDocumento12 páginasAn Introduction To PrescribingNelly AlvaradoAinda não há avaliações
- Rizal's Visit To The United States (1888Documento23 páginasRizal's Visit To The United States (1888Dandy Lastimosa Velasquez57% (7)
- The Obesity Code: Unlocking the Secrets of Weight LossNo EverandThe Obesity Code: Unlocking the Secrets of Weight LossNota: 4 de 5 estrelas4/5 (6)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsAinda não há avaliações