Escolar Documentos
Profissional Documentos
Cultura Documentos
Ectopic Pregnancy: Clinical Manifestations and Diagnosis
Enviado por
Edna LópezDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Ectopic Pregnancy: Clinical Manifestations and Diagnosis
Enviado por
Edna LópezDireitos autorais:
Formatos disponíveis
1/17/2016
Ectopicpregnancy:Clinicalmanifestationsanddiagnosis
OfficialreprintfromUpToDate
www.uptodate.com2016UpToDate
Ectopicpregnancy:Clinicalmanifestationsanddiagnosis
Author
TogasTulandi,MD,MHCM
SectionEditor
RobertLBarbieri,MD
DeputyEditor
SandyJFalk,MD,FACOG
Alltopicsareupdatedasnewevidencebecomesavailableandourpeerreviewprocessiscomplete.
Literaturereviewcurrentthrough:Dec2015.|Thistopiclastupdated:Sep02,2015.
INTRODUCTIONAnectopicpregnancyisanextrauterinepregnancy.Almostallectopicpregnanciesoccurin
thefallopiantube(98percent)[1],butotherpossiblesitesinclude:cervical,interstitial(alsoreferredtoascornual
apregnancylocatedintheproximalsegmentofthefallopiantubethatisembeddedwithinthemuscularwallofthe
uterus),hysterotomyscar,intramural,ovarian,orabdominal.Inaddition,inrarecases,amultiplegestationmaybe
heterotopic(includebothauterineandextrauterinepregnancy).
Thediagnosisofectopicpregnancyisbaseduponacombinationofmeasurementoftheserumquantitativehuman
chorionicgonadotropin(hCG)andfindingsontransvaginalultrasonography(TVUS).
Theclinicalmanifestationsanddiagnosisofectopicpregnancywillbereviewedhere.Thistopicwillfocusmainly
onthediagnosisoftubalpregnancy.Thesurgicaltreatmentofectopicpregnancyisreviewedelsewhere.Related
topicsregardingectopicpregnancyarediscussedindetailseparately,including:
Epidemiology,riskfactors,andpathology(see"Ectopicpregnancy:Incidence,riskfactors,andpathology")
Managementwithmethotrexate(see"Ectopicpregnancy:Choosingatreatmentandmethotrexatetherapy")
Surgicaltreatment(see"Ectopicpregnancy:Surgicaltreatment")
Expectantmanagement(see"Ectopicpregnancy:Expectantmanagement")
Diagnosisandmanagementofuncommonsites(see"Abdominalpregnancy,cesareanscarpregnancy,and
heterotopicpregnancy")
CLINICALPRESENTATIONThemostcommonclinicalpresentationofectopicpregnancyisfirsttrimester
vaginalbleedingand/orabdominalpain[2].Ectopicpregnancymayalsobeasymptomatic.
Normalpregnancydiscomforts(eg,breasttenderness,frequenturination,nausea)aresometimespresentin
additiontothesymptomsspecificallyassociatedwithectopicpregnancy.Theremaybealowerlikelihoodofearly
pregnancysymptoms,becauseprogesterone,estradiol,andhumanchorionicgonadotropin(hCG)maybelowerin
ectopicpregnancythaninnormalpregnancy[35].
Inaretrospectivestudyof2026pregnantwomenwhopresentedtotheemergencydepartmentwithfirsttrimester
vaginalbleedingandabdominalpain,376(18percent)werediagnosedwithectopicpregnancy.Ofthese376
women,76percenthadvaginalbleedingand66percenthadabdominalpain[6].Inapopulationbasedregistryof
ectopicpregnancyfromFrance,theincidenceofrupturewas18percent[7].
Clinicalmanifestationsofectopicpregnancytypicallyappearsixtoeightweeksafterthelastnormalmenstrual
period,butcanoccurlater,especiallyifthepregnancyisinanextrauterinesiteotherthanthefallopiantube.
Anectopicpregnancymaybeunrupturedorrupturedatthetimeofpresentationtomedicalcare.Tubalrupture(or
ruptureofotherstructuresinwhichanectopicpregnancyisimplanted)canresultinlifethreateninghemorrhage.
Anysymptomssuggestiveofruptureshouldbenoted.Theseincludesevereorpersistentabdominalpainor
symptomssuggestiveofongoingbloodloss(eg,feelingfaintorlossofconsciousness).
Basedupontheconcernabouttheriskofruptureatthetimeorafterpresentation,cliniciansshouldconsider
ectopicpregnancyasadiagnosisinanywomanofreproductiveagewithvaginalbleedingand/orabdominalpain
http://www.uptodate.com/contents/ectopicpregnancyclinicalmanifestationsanddiagnosis?topicKey=OBGYN%2F5487&elapsedTimeMs=4&source=search
1/19
1/17/2016
Ectopicpregnancy:Clinicalmanifestationsanddiagnosis
whohasthefollowingcharacteristics:(1)pregnant,butdoesnothaveaconfirmedintrauterinepregnancy(IUP)(2)
pregnancystatusuncertain,particularlyifamenorrheaof>4weeksprecededthecurrentvaginalbleeding(3)in
rarecases,awomanwhopresentswithhemodynamicinstabilityandanacuteabdomenthatisnotexplainedby
anotherdiagnosis.
VaginalbleedingTheamountandtimingofvaginalbleedingvaryandthereisnobleedingpatternthatis
pathognomonicforectopicpregnancy.Bleedingmayrangefromscantbrownstainingtohemorrhage.Bleedingis
typicallyintermittent,butmayoccurasasingleepisodeorcontinuously.
Thevaginalbleedingassociatedwithectopicpregnancyistypicallyprecededbyamenorrhea.However,some
womenmaymisinterpretbleedingasnormalmenses,andmaynotrealizetheyarepregnantpriortodeveloping
symptomsassociatedwithectopicpregnancy.Thisisparticularlytrueinwomenwhohaveirregularmensesor
whodonotkeeptrackofmenstrualcycles.
Bleedingoccursinmanyotherconditionsinearlypregnancy.(See'Differentialdiagnosis'below.)
AbdominalpainThepainassociatedwithectopicpregnancyisusuallylocatedinthepelvicarea.Itmaybe
diffuseorlocalizedtooneside.Incasesinwhichthereisintraperitonealbloodthatreachestheupperabdomenor
inrarecasesofabdominalpregnancy,thepainmaybeinthemiddleorupperabdomen.Ifthereissufficient
intraabdominalbleedingtoreachthediaphragm,theremaybereferredpainthatisfeltintheshoulder.Blood
poolingintheposteriorculdesac(pouchofDouglas)maycauseanurgetodefecate.
Thetiming,character,andseverityofabdominalpainvary,andthereisnopainpatternthatispathognomonicfor
ectopicpregnancy.Theonsetofthepainmaybeabruptorslow,andthepainmaybecontinuousorintermittent.
Thepainmaybedullorsharpitisgenerallynotcrampy.Thepainmaybemildorsevere.Tubalrupturemaybe
associatedwithanabruptonsetofseverepain,butrupturemayalsopresentwithmildorintermittentpain.
DIAGNOSTICEVALUATION
OverviewThemaingoalsandstepsoftheevaluationofawomanwithasuspectedectopicpregnancyare:
Confirmthatthepatientispregnant(see'Humanchorionicgonadotropin'below).
Determinewhetherthepregnancyisintrauterineorectopic(inrarecases,thepregnancyisheterotopic).
Determinethesiteoftheectopicpregnancy.
Determinewhetherthestructureinwhichthepregnancyisimplanted(mostcommonly,thefallopiantube)
hasrupturedandwhetherthepatientishemodynamicallystable.Failuretodiagnoseectopicpregnancy
beforetubalrupturelimitsthetreatmentoptionsandincreasesmaternalmorbidityandmortality.
Performadditionaltestingtoguidefurthermanagement(eg,bloodtypeandantibodyscreen,pretreatment
testingformethotrexatetherapy).
HistoryAmenstrualhistoryshouldbetakenandtheestimatedgestationalageshouldbecalculated.(See
"Prenatalassessmentofgestationalageandestimateddateofdelivery".)
Thehistoryshouldfocusonthepresenceandcharacteristicsofvaginalbleedingandabdominalpain.(See
'Clinicalpresentation'above.)
Riskfactorsforectopicpregnancyshouldbeelicited,includingpriorectopicpregnancy,currentuseofan
intrauterinedevice,priortuballigation,andinvitrofertilization(IVF)(table1).However,over50percentofwomen
areasymptomaticbeforetubalruptureanddonothaveanidentifiableriskfactorforectopicpregnancy[8].A
populationbasedFrenchstudyidentifiedfourfactorsthatincreasedtheriskofrupturewhenanectopicpregnancy
wassuspected:(1)neverhavingusedcontraception,(2)historyoftubaldamageandinfertility,(3)inductionof
ovulation,and(4)highlevelofhumanchorionicgonadotropin(hCG,atleast10,000IU/L)[7].Theoverallrateof
tubalruptureinthisserieswas18percent.(See"Ectopicpregnancy:Incidence,riskfactors,andpathology",
sectionon'Riskfactors'.)
http://www.uptodate.com/contents/ectopicpregnancyclinicalmanifestationsanddiagnosis?topicKey=OBGYN%2F5487&elapsedTimeMs=4&source=search
2/19
1/17/2016
Ectopicpregnancy:Clinicalmanifestationsanddiagnosis
Themedicalandsurgicalhistoryshouldbereviewed,sincethismayimpacttreatment.Thefocusshouldbeon
obstetrichistoryandpelvicorabdominalsurgicalhistoryandmedicalcomorbiditiesthatarepotential
contraindicationsforsurgeryormethotrexatetherapy(eg,renalorhepaticdisease).(See"Ectopicpregnancy:
Choosingatreatmentandmethotrexatetherapy",sectionon'Contraindications'.)
PhysicalexaminationVitalsignsshouldbemeasuredandhemodynamicstabilityassessed.Inyoung,healthy
patientswithbloodloss,assessingthevitalsignsshouldincludeanevaluationforposturalchange.However,vital
signs,includingposturalchanges,maybenormalearlyinthecourseofsignificantbleedingduetocompensatory
mechanisms[9].Womenwithhemodynamicinstabilityandsuspectedectopicpregnancyrequireemergency
surgery.(See"Initialmanagementoftraumainadults",sectionon'Circulation'.)
Theabdominalexaminationisoftenunremarkableormayreveallowerabdominaltenderness.Ifrupturewith
significantbleedinghasoccurred,theabdomenmaybedistendedanddiffuseorlocalizedtendernesstopalpation
and/orreboundtendernessmaybefoundonexamination.
Acompletepelvicexaminationshouldbeperformed.Thespeculumexaminationisusedtoconfirmthattheuterus
isthesourceofbleeding(ratherthanacervicalorvaginallesion)andtoassessthevolumeofbleedingbynoting
thequantityofbloodinthevaginaandpresenceorabsenceofactivebleedingfromthecervix.
Abimanualpelvicexaminationisperformedtheexaminationisoftenunremarkableinawomanwithasmall,
unrupturedectopicpregnancy.Palpationoftheadnexashouldbeperformedwithonlyasmalldegreeofpressure,
sinceexcessivepressuremayruptureanectopicpregnancy.Findingsonexaminationmayincludecervical
motion,adnexal,and/orabdominaltenderness.Anadnexalmassisnotedinsomewomen.
Theuterusmaybesomewhatenlarged,butwilllikelybesmallerthanappropriateforgestationalage.Uterine
enlargementinwomenwithectopicpregnancymaybeduetoendocrinechangesofpregnancy,rarecasesof
heterotopicpregnancy,orincidentaluterinepathology(mostcommonly,uterinefibroids).
DiagnostictestingThetestsusedtodiagnoseanectopicpregnancyareacombinationofserumquantitative
hCGlevelandtransvaginalultrasound(TVUS)(algorithm1andtable2).
TransvaginalultrasoundTVUSisthemostusefulimagingtestfordeterminingthelocationofapregnancy.
TVUSshouldbeperformedaspartoftheinitialevaluationandmayneedtoberepeated,dependinguponthehCG
levelorasuspicionofrupture.Theultrasoundshouldbeperformedbyaclinicianwithexpertiseingynecologic
ultrasoundandwiththeevaluationofectopicpregnancy,wheneverpossible.
TVUSalone(withoutmeasurementofhCG)canexcludeordiagnoseanectopicpregnancyonlyifoneofthe
followingfindingsispresent:
Findingsdiagnosticofanintrauterinepregnancy(IUP,gestationalsacwithayolksacorembryo).
Findingsdiagnosticofapregnancyatanectopicsite(gestationalsacwithayolksacorembryo).
Ineithercase,agestationalsacaloneisnotsufficientfordiagnosis.Insomeectopicgestations,apseudosacis
formedthatmayappeartobeagestationalsac(see"Ultrasonographyofpregnancyofunknownlocation",section
on'Pseudosac').Cardiacactivitymayormaynotbepresent.
Inthegreatmajorityofcases,eithertwofindingsaboveexcludesordiagnosesanectopicgestation.Therare
exceptionsareheterotopicpregnanciesandmisdiagnosesofanIUP(ie,interstitialpregnancyorrudimentaryhorn
pregnancy).Inareviewof568casesofrudimentaryuterinehornpregnanciesfrom1900to1999,arupturerateof
50percentwasfoundwith80percentoccurringbeforethethirdtrimester[10].(See'Heterotopicpregnancy'below
and'Interstitialpregnancy'below.)
TVUScanalsodetectfindingsthataresuggestive,butnotdiagnostic,ofectopicpregnancy.Anadnexalmassis
themostcommonultrasoundfindinginectopicpregnancyandispresentin89percentormoreofcases[1113].
IfTVUSisnondiagnostic,itmaybebecausethegestationistooearlytobevisualizedonultrasound.Ifso,serial
http://www.uptodate.com/contents/ectopicpregnancyclinicalmanifestationsanddiagnosis?topicKey=OBGYN%2F5487&elapsedTimeMs=4&source=search
3/19
1/17/2016
Ectopicpregnancy:Clinicalmanifestationsanddiagnosis
measurementsoftheserumhCGconcentrationshouldbetakenuntilthehCGdiscriminatoryzoneisreached[14].
(See'Clinicalprotocol'below.)
Theultrasoundexaminationisalsousedtoevaluatewhetherruptureofthetubeorotherstructurehasoccurred.A
findingofechogenicfluid(consistentwithblood)inthepelvicculdesacand/orabdomenisconsistentwith
rupture.However,asmallamountoffluidispresentinmanywomenandasmallamountofbloodmaybepresent
inotherconditions(eg,spontaneousabortion).Arupturedovariancystisanotherconditionthatiscommonin
pregnantwomenandmayresultinasmallorlargeamountofblood.Ruptureisindicatedbyultrasoundfindingsof
freefluid(blood)intheabdominalcavity.
UltrasoundevaluationforectopicpregnancyversusIUPisdiscussedindetailseparately.(See"Ultrasonography
ofpregnancyofunknownlocation".)
Eitherultrasoundorotherabdominalimagingmodalitiesareusedforevaluationintherarecasesofabdominal
pregnancy.(See"Abdominalpregnancy,cesareanscarpregnancy,andheterotopicpregnancy",sectionon
'Diagnosticevaluation'.)
HumanchorionicgonadotropinMeasurementofhCGisperformedinitiallytodiagnosepregnancyand
thenfollowedtoassessforectopicpregnancy.Forfollowup,hCGismeasuredserially(every48to72hours)to
determinewhethertheincreaseisconsistentwithanabnormalpregnancy.AsinglehCGmeasurementalone
cannotconfirmthediagnosisofectopicornormalpregnancy.
TheinitialtesttodiagnosepregnancymaybeeitheraurineorserumhCG.Onceapregnancyisconfirmed,if
ectopicpregnancyissuspected,theserumhCGisthenrepeatedserially(typicallyeverytwodays)toassess
whethertheincreaseinconcentrationisconsistentwithanabnormalpregnancy.Insomecases,thediagnosisof
ectopicpregnancycanbemadeafterasinglemeasurementofhCGincombinationwithtransvaginalultrasound,if
thehCGisabovethediscriminatoryzoneandtransvaginalultrasoundshowsnoevidenceofanintrauterine
pregnancyandthepresenceoffindingsthatsuggestanectopicpregnancy.(See'Transvaginalultrasound'above.)
Inpregnantwomen,hCGcanbedetectedinserumandurineasearlyaseightdaysaftertheluteinizinghormone
surge(approximately21to22daysafterthefirstdayofthelastmenstrualperiodinwomenwith28daycycles).
ThehCGconcentrationinanormalIUPrisesinacurvilinearfashionuntilabout41daysofgestation,afterwhichit
risesmoreslowlyuntilapproximately10weeks,andthendeclinesuntilreachingaplateauinthesecondandthird
trimesters[15].ItisnotpossibletodeterminewhetherapregnancyisnormalfromasinglehCGlevelbecause
thereisawiderangeofnormallevelsateachweekofpregnancy[16].(See"Clinicalmanifestationsanddiagnosis
ofearlypregnancy",sectionon'Serumpregnancytest'and"Humanchorionicgonadotropin:Testinginpregnancy
andgestationaltrophoblasticdiseaseandcausesoflowpersistentlevels",sectionon'Pregnancy'.)
StudiesinviableIUPshavereportedthefollowingchangesinserumhCG[17,18]:
Themeandoublingtimeforthehormonerangesfrom1.4to2.1daysinearlypregnancy.
In85percentofviableIUPs,thehCGconcentrationrisesbyatleast66percentevery48hoursduringthe
first40daysofpregnancyonly15percentofviablepregnancieshavearateofriselessthanthisthreshold.
Theslowestrecordedriseover48hoursassociatedwithaviableIUPwas53percent.
AserumhCGthatdoesnotriseappropriatelyisconsistentwithanabnormalpregnancy.ThehCGconcentration
risesatamuchslowerrateinmost,butnotall,ectopicandnonviableIUPs[18,19].Inoneseries,asanexample,
only21percentofectopicpregnancieswereassociatedwithhCGlevelsthatfollowedtheminimumdoublingtime
ofaviableIUP(definedinthisseriesas53percentincreaseovertwodays)[18].
AdecreasinghCGconcentrationismostconsistentwithafailedpregnancy(eg,arrestedpregnancy,anembryonic
pregnancy,tubalabortion,spontaneouslyresolvingectopicpregnancy,completeorincompleteabortion).
ThehCGresultvariesacrossdifferentassaysandlaboratories.Theintraassayandinterassayvariabilitiesdepend
http://www.uptodate.com/contents/ectopicpregnancyclinicalmanifestationsanddiagnosis?topicKey=OBGYN%2F5487&elapsedTimeMs=4&source=search
4/19
1/17/2016
Ectopicpregnancy:Clinicalmanifestationsanddiagnosis
onthetypeofassay.Inonestudy,theintraassayandinterassaycoefficientofvariationwere4.87and
6.25percent,respectively[20].Thus,interpretationofserialhCGconcentrationsismorereliablewhentheassays
areperformedinthesamelaboratory.Inaddition,thepossibilityoffalselypositiveornegativehCGtestresults
shouldbeconsidered[21,22].(See"Humanchorionicgonadotropin:Testinginpregnancyandgestational
trophoblasticdiseaseandcausesoflowpersistentlevels",sectionon'Falsenegativetest(hookeffect)'and
"Humanchorionicgonadotropin:Testinginpregnancyandgestationaltrophoblasticdiseaseandcausesoflow
persistentlevels",sectionon'Falsepositivetestor"phantomhCG"'.)
DiscriminatoryzoneThediscriminatoryzoneistheserumhCGlevelabovewhichagestationalsac
shouldbevisualizedbyTVUSifanIUPispresent.
Inmostinstitutions,thediscriminatoryzoneisaserumhCGlevelof1500or2000IU/LwithTVUS.Thereported
sensitivityandspecificityofhCGof>1500IU/Lare15.2and93.4percent,andforanhCGlevelof>2000IU/L,
theyare10.9and95.2percent,respectively[23].Thelevelishigherfortransabdominalultrasound(approximately
6500IU/L),butTVUSisthestandardmodalityusedtoevaluateectopicpregnancy.
Settingthediscriminatoryzoneat2000IU/Linsteadof1500IU/Lminimizestheriskofinterferingwithaviable
IUP,ifpresent,butincreasestheriskofdelayingdiagnosisofanectopicpregnancy.
However,thecorrectleveltouseforthediscriminatoryzoneiscontroversial.Theuseof1500or2000IU/Lasthe
discriminatoryzoneisbaseduponobservationsthatanintrauterinegestationalsaccouldbedetectedbyTVUSin
patientswithserumhCGconcentrationsaslowas800IU/Landwasusuallyidentifiedbyexpert
ultrasonographersatconcentrationsabove1500to2000IU/L[24].Inonerepresentativestudy,185of188(98
percent)IUPsinwomenwithhCGabove1500IU/Lwerevisualized[25].Itisimportanttonotethatthereisa
variationinthelevelofhCGacrosspregnanciesforeachgestationalageandthediscriminatorylevelsarenot
alwaysreliable.Accordingly,beforedecidingonmethotrexatetreatment,onehastobesurethatthereisno
possibilityofaviableintrauterinepregnancy.
Anothercauseforvariationofthediscriminatoryzoneisthatitisdependentupontheskilloftheultrasonographer,
thequalityoftheultrasoundequipment,thepresenceofphysicalfactors(eg,fibroids,multiplegestation),andthe
laboratorycharacteristicsofthehCGassayused.
ClinicalprotocolTheclinicalprotocolfortheevaluationforanectopicpregnancyincludesassessment
withserumhCGandTVUS:
HCGbelowthediscriminatoryzoneAserumhCGconcentration<1500or2000IU/L(oranothervalue,
thediscriminatoryzonefortheinstitutionshouldbeused)shouldbefollowedbyrepeatedmeasurementof
quantitativehCGtofollowtherateofrise.Asnotedabove,foraviableIUP,themeanhCGdoublingtimeis
1.4to2.1daysandslowestrecordedriseover48hoursassociatedwithaviableIUPwas53percent.Also,
thesamelaboratoryshouldbeusedforserialmeasurements.(See'Humanchorionicgonadotropin'above.)
ThemostcommonprotocolistomeasurethehCGeverytwodays.Inourpractice,wefindthat
measurementevery72hoursismorepracticalthanevery48hours,andallowing72hoursfordoublinghelps
toavoidmisclassifyingthoseviablepregnancieswithslowerthanaveragedoublingtimes.Thus,theprotocol
isasfollows:
hCGisrisingnormally(increasingbyatleast53percentin48hoursORdoublingin72hours)The
patientshouldbeevaluatedwithTVUSwhenthehCGreachesthediscriminatoryzone.Atthattime,an
IUPorectopicpregnancycanbediagnosedbyTVUS.
hCGisrising,butNOTnormallyThelackofanormalriseinhCGacrossthreemeasurements(the
initialserumquantitativehCGandtwoadditionalserialmeasurements)isconsistentwithanabnormal
pregnancy(anectopicgestationorIUPthatwillultimatelyabort).ThehCGlevelmayberisingslowly
ormayplateauatorveryclosetothepreviouslevel.Thecliniciancanbereasonablycertainthata
normalIUPisnotpresent.Thenumberofserialmeasurementstousetomakethediagnosishasnot
http://www.uptodate.com/contents/ectopicpregnancyclinicalmanifestationsanddiagnosis?topicKey=OBGYN%2F5487&elapsedTimeMs=4&source=search
5/19
1/17/2016
Ectopicpregnancy:Clinicalmanifestationsanddiagnosis
beenwellstudied.Somedatasuggestthatuseofthreeserialmeasurementsismoreeffectivethantwo
measurements[26].
InpatientswithanabnormalriseinhCG,theTVUSshouldberepeated.Iftherearefindingsthat
confirmanIUP,anectopicpregnancyisexcludedandthepatientshouldbemanagedasafailed
pregnancy.Ifanadnexalmassconsistentwithanectopicpregnancyisvisualized,thenmedicalor
surgicaltreatmentisadministeredforapresumedectopicpregnancy.Ifanadnexalmassisnot
visualized,somecliniciansadministermethotrexateandothersperformcurettagetoexcludeanIUP
andtherebyavoidmedicaltherapyofnonviableIUP[27].(See'Curettage'below.)
hCGisdecreasingAdecreasinghCGismostconsistentwithafailedpregnancy(eg,spontaneous
abortion,tubalabortion,spontaneouslyresolvingectopicpregnancy).Tofollowupwiththesepatients,
weeklyhCGconcentrationsshouldbemeasureduntiltheresultisundetectable.
Patientswhoarebeingfollowedforsuspectedectopicpregnancyshouldbecounseledabouttheriskofrupture
andshouldbeadvisedtocallifsymptomsassociatedwithruptureoccur.Theseincludethenewonsetofora
significantworseningofabdominalpain,vaginalhemorrhage,orfeelingfaint.Inaddition,womenwithasuspected
ectopicpregnancyshouldbecounseledaboutpossibleoutcomesoftheevaluation,includingviableIUPortheend
ofapregnancywithtreatmentforectopicpregnancy.
hCGabovethediscriminatoryzoneForwomenwithaquantitativeserumhCGabovethediscriminatory
zone,theresultsofTVUSguidemanagement.IfTVUSdoesnotrevealanIUPandshowsacomplex
adnexalmass,anextrauterinepregnancyisalmostcertain.Treatmentofectopicpregnancyshouldbe
instituted.
Thediagnosisofectopicpregnancyislesscertainifnocomplexadnexalmasscanbevisualized,since
thereisvariabilityinthelevelofexpertiseamongultrasonographers.Furthermore,aserumhCG>1500IU/L
withoutvisualizationofintrauterineorextrauterinepathologymayrepresentamultiplegestation,sincethere
isnoprovendiscriminatorylevelformultiplegestations.Forthesereasons,ournextstepinthisclinical
scenarioistorepeattheTVUSexaminationandhCGconcentrationtwodayslater.IfanIUPisstillnot
observedonTVUS,thenthepregnancyisabnormal.
AncillarydiagnostictestsAdditionaldiagnostictestshavebeenusedinwomenwithsuspectedectopic
pregnancy.Exceptinselectedcases,suchtestsdonotprovideadditionalclinicallyusefulinformation.
ProgesteroneSerumprogesteroneconcentrationsarehigherinviableIUPsthaninectopicpregnancies
andIUPsthataredestinedtoabort[28].Ametaanalysisof26cohortstudiesincluding9436womeninthefirst
trimesterofpregnancyevaluateduseofasinglemeasurementofserumprogesteroneforthediagnosisofa
nonviablepregnancy[29].Forwomenwithbleedingorpainandaninconclusivepelvicultrasound,aprogesterone
<3.2to6ng/mL(10.2to19.1nmol/L)hadasensitivityof75percentandaspecificityof98percent.Forwomen
withbleedingorpainalone,aprogesterone<10ng/mL(31.8nmol/L)hadasensitivityof67percentanda
specificityof96percent.
Thepredictivevalueofalowserumprogesteroneforidentifyingnonviablepregnanciesvarieswiththepatient
population.Thesensitivityandspecificityofalowserumprogesteroneconcentrationforpredictinganonviable
pregnancyinspontaneouslypregnantpatientsaredifferentfromthoseininfertilepatientswhohaveundergone
controlledovarianhyperstimulationforIVForintrauterineinsemination[30].
Inourexperience,progesteronemeasurementsmerelyconfirmdiagnosticimpressionsalreadyobtainedbyhCG
measurementsandtransvaginalsonography.Wedonotroutinelymeasureserumprogesterone.However,
measurementofserumprogesteronemaybeusefulinapatientwithabdominalpainandbleedingandwhohasa
serumhCGlevelbelowthatexpectedforhergestationalage.Itshouldbenoted,however,thatthedefinitionofa
lowprogesteroneisunclear.
CurettageTheintrauterinelocationofapregnancyisdiagnosedwithcertaintyiftrophoblastictissueis
http://www.uptodate.com/contents/ectopicpregnancyclinicalmanifestationsanddiagnosis?topicKey=OBGYN%2F5487&elapsedTimeMs=4&source=search
6/19
1/17/2016
Ectopicpregnancy:Clinicalmanifestationsanddiagnosis
obtainedbyuterinecurettage.Obviously,theuseofcurettageasadiagnostictoolislimitedbythepotentialfor
disruptionofaviablepregnancy.Moreover,falsenegativescanoccur:chorionicvilliarenotdetectedby
histopathologyin20percentofcurettagespecimensfromelectiveterminationofpregnancy[31].Pipelle
endometrialbiopsyisevenlesssensitivethancurettagefordetectionofvillisensitivitiesreportedintwosmall
serieswere30and60percent[32,33].Ifcurettageisperformed,serumhCGlevelscanbefollowedpostcurettage
ifhistopathologydoesnotconfirmtheclinicalimpression.WhenanIUPhasbeenevacuated,hCGlevelsshould
dropbyatleast15percentthedayafterevacuation[27].
SomeexpertshaverecommendedperformingcurettageonlyonwomenwithbothahCGconcentrationbelowthe
discriminatoryzoneandalowdoublingrate[34,35].Approximately30percentofthesepatientshaveanonviable
intrauterinegestationandtheremainderhaveanectopicpregnancy[35,36].Knowingtheresultsofcurettage
avoidsunnecessarymethotrexatetreatmentofthe30percentofpatientswithoutectopicpregnancy.
Adecisionanalysiscomparingthecost/complicationratesinpatientswhoundergodiagnosticcurettagebefore
administrationofmethotrexatewiththosewhodonothaveacurettageconcludedtherewasnosignificantbenefit
ofoneapproachovertheother[36].However,theauthors'preferencewastoperformcurettageinthesepatients
tobemorecertainofthediagnosis,andfeltthisinformationwasusefulprognostically(eg,riskofrecurrence)and
forfuturedecisionmaking.Incontrast,weandothersbelieveitismorepracticalandlessinvasivetocontinue
observationoradministeronedoseofmethotrexatethantoperformcurettage[37,38].Thesideeffectsofonedose
ofmethotrexatearenegligible.Inaddition,curettagecarriesariskofintrauterineadhesionformation.(See"Ectopic
pregnancy:Choosingatreatmentandmethotrexatetherapy"and"Intrauterineadhesions".)
OthertestsRarely,laparoscopyisusedtoconfirmthediagnosisifhCGandultrasoundresultsare
ambiguous.Anectopicpregnancydetectedatlaparoscopyshouldbetreatedimmediatelybysurgery.Inthis
situation,amedicalapproachconfersadditionalriskandhasnoprovenbenefit.
Historically,culdocentesiswasusedtodetectbloodintheposteriorculdesachowever,thisfindingcanbeeasily
demonstratedwithtransvaginalultrasound.Bloodintheposteriorculdesacmaybefrombleedingfroman
unrupturedorrupturedtubalpregnancy,butitmayalsobetheresultofarupturedovariancyst.Therefore,a
culdocentesispositiveforbloodisnondiagnostic.(See"Culdocentesis".)
AdditionaltestingAdditionaltestingisperformedtoevaluatethepatientshemodynamicstatus,Rh(D)type.If
methotrexatetreatmentisapossibility,pretreatmentlaboratorytestsshouldbedrawn.
CompletebloodcountWomenwithsuspectedectopicpregnancyshouldbeevaluatedforanemiawitha
hemoglobinand/orhematocrit.
Inseverecases,ifheavybleedingissuspected,measurementofplateletsorcoagulationtestsmayalsobe
indicated.(See"Massivebloodtransfusion",sectionon'Alterationsinhemostasis'.)
Ifectopicpregnancyisdiagnosedandtreatmentwithmethotrexateisconsidered,acompletebloodcountispartof
thepretreatmentlaboratoryevaluation.
BloodtypeandscreenARh(D)typingandantibodyscreenshouldbedrawnifnotpreviouslyperformed
duringthecurrentpregnancy.WomenwithbleedinginpregnancywhoareRh(D)negativeshouldbegivenantiD
immuneglobulin.(See"PreventionofRh(D)alloimmunization".)
Ifsignificantbleedingissuspected,asampleshouldbesenttothebloodbankforcrossmatchingforpotential
transfusion.
PretreatmentlaboratorytestsForwomentreatedwithmethotrexate,pretreatmenttestingtypicallyincludes
acompletebloodcountandrenalandliverfunctiontests.(See"Ectopicpregnancy:Choosingatreatmentand
methotrexatetherapy",sectionon'Pretreatmenttesting'.)
DIAGNOSISThediagnosisofectopicpregnancyisaclinicaldiagnosismadebaseduponserialserumhuman
chorionicgonadotropin(hCG)testingandtransvaginalultrasound(TVUS).(See'Transvaginalultrasound'above
http://www.uptodate.com/contents/ectopicpregnancyclinicalmanifestationsanddiagnosis?topicKey=OBGYN%2F5487&elapsedTimeMs=4&source=search
7/19
1/17/2016
Ectopicpregnancy:Clinicalmanifestationsanddiagnosis
and'Humanchorionicgonadotropin'above.)
Histologicconfirmationofthediagnosisisnottypicallyrequired.Inselectedcases,uterinecurettageisperformed
toconfirmtheabsenceofanintrauterinepregnancy(IUP)priortomethotrexatetherapy.Ifanectopicpregnancyis
treatedsurgically,histologicconfirmationisobtainedfollowingtreatment.
DiagnosticcriteriaThediagnosticcriteriadependupontherelationshiptothehCGdiscriminatoryzone(serum
hCGlevelabovewhichagestationalsacshouldbevisualizedbyTVUSifanIUPispresent).ThehCGlevelof
thediscriminatoryzonevaries,butinmostinstitutionsitis1500to2000IU/L(see'Discriminatoryzone'aboveand
'Clinicalprotocol'above):
Belowthediscriminatoryzone
IftheserialhCGleveldoesnotriseappropriatelyacrossatleastthreemeasurements48to72hours
apartandthereisnoevidenceonTVUSthatconfirmsanIUP,thepregnancyisconsideredabnormal.
Apresumptivediagnosisofectopicpregnancycanbemadeandthepatientmaybetreated.Inselected
cases,uterinecurettageisperformedtoconfirmtheabsenceofanIUP(see'Curettage'above).
IftheserialserumhCGlevelisrisingappropriately,thepatientisfolloweduntilthehCGisabovethe
discriminatoryzone.
AbovethediscriminatoryzoneThediagnosisismadebasedupontheabsenceofTVUSfindingsthat
diagnoseanIUPORfindingsatanextrauterinesitethatconfirmanectopicpregnancy.Thepresenceofa
gestationalsacwithayolksacorembryoisdiagnosticofapregnancy.Thegestationalsacisanearly
findingandissuggestiveof,butdoesnotfullyconfirm,anIUP(see'Transvaginalultrasound'above).
Ultrasoundfindingssuggestiveofanectopicpregnancyinthefallopiantube,ovary,orothersitesfurthersupport
thediagnosis,butarenotdiagnosticontheirown(see'Transvaginalultrasound'above).
IntheabsenceofadefinitivesonogramconfirminganIUPorhistopathologicfindings,itissometimesimpossible
todifferentiatebetweenanectopicpregnancyandanearlyfailedintrauterinegestation.Thisisreferredtoasa
pregnancyofunknownlocationand8to40percentareultimatelydiagnosedasectopicpregnancies[23].
RupturedversusnonrupturedectopicpregnancyDiagnosisofruptureofthestructurewithinwhichthe
ectopicgestationisimplanted(usuallythefallopiantube)isaclinicaldiagnosis.Thetypicalfindingsofruptureare
abdominalpain,shoulderpainduetodiaphragmaticirritationbybloodintheperitonealcavity,andeventually,
hypotensionandshock.Abdominalexaminationfindingsincludetendernessandpossibleperitonealsigns.The
typicalfindingonTVUSisfreebloodintheperitonealcavity.However,thepresenceorabsenceofperitonealfree
fluidisnotareliableindicatorofwhetheranectopicpregnancyhasruptured.(See"Ultrasonographyofpregnancy
ofunknownlocation",sectionon'Peritonealfreefluid'.)
Forwomenwhoundergosurgery,thediagnosisofrupturecanbemadebydirectvisualization.
DIFFERENTIALDIAGNOSISTheclassicsymptomsofectopicpregnancyarevaginalbleedingandabdominal
pain.
Thedifferentialdiagnosisofbleedingorpainearlyinpregnancyalsoincludes[39]:
Physiologic(ie,believedtoberelatedtoimplantation)
Spontaneousabortion
Gestationaltrophoblasticdisease
Cervical,vaginal,oruterinepathology
Subchorionichematoma
Nonuterinesourcesofbleedingcanbeidentifiedbyphysicalexamination.Screeningforcervicalcancershould
alsobeperformed,asappropriate(table3).(See"Differentialdiagnosisofgenitaltractbleedinginwomen"and
http://www.uptodate.com/contents/ectopicpregnancyclinicalmanifestationsanddiagnosis?topicKey=OBGYN%2F5487&elapsedTimeMs=4&source=search
8/19
1/17/2016
Ectopicpregnancy:Clinicalmanifestationsanddiagnosis
"Screeningforcervicalcancer".)
Evenifanothersourceofbleedingisidentified,allwomenwithfirsttrimesterbleedingshouldbeevaluatedby
transvaginalultrasonography.Whenthehumanchorionicgonadotropin(hCG)concentrationisunusuallyhighfor
thegestationalage,gestationaltrophoblasticdiseaseshouldbesuspected.Theevaluationoffirsttrimestervaginal
bleedingisoutlinedinthealgorithm(algorithm2)andisdiscussedseparately.(See"Overviewoftheetiologyand
evaluationofvaginalbleedinginpregnantwomen"and"Spontaneousabortion:Riskfactors,etiology,clinical
manifestations,anddiagnosticevaluation"and"Hydatidiformmole:Epidemiology,clinicalfeatures,and
diagnosis".)
Thedifferentialdiagnosisoflowerabdominalpaininwomenincludesurinarytractinfection,kidneystones,
diverticulitis,appendicitis,ovarianneoplasms,ovariancystrupture,ovariantorsion,endometriosis,endometritis,
leiomyomas,pelvicinflammatorydisease,andpregnancyrelatedconditions.(See"Diagnosticapproachto
abdominalpaininadults".)
SPECIALISSUES
MultiplegestationInwomenwithanintrauterinemultiplepregnancy,theserumhumanchorionicgonadotropin
(hCG)levelcouldbehigherthan1500mIU/mLandyetultrasoundexaminationwillnotrevealanintrauterine
pregnancy(IUP)[14].Levelsofover9000IU/Lhavebeendescribedforintrauterinetripletpregnanciesunobserved
bytransvaginalultrasound(TVUS)[40].
HeterotopicpregnancyTheinvestigationforectopicpregnancycanbeterminated,undermostcircumstances,
ifatransvaginalsonogramrevealsanIUP.Heterotopicpregnancy(combinedintrauterineandextrauterine
pregnancy)israre,exceptamongwomenconceivingthroughinvitrofertilization(IVF).Theextrauterinepregnancy
isusuallyinthefallopiantube,butcanbeatanotherlocation,suchasthecervix.(See"Abdominalpregnancy,
cesareanscarpregnancy,andheterotopicpregnancy".)
Earlydiagnosisofheterotopicpregnancyisdifficultbecauseoflackofsymptoms.Thus,ahighindexofsuspicion
forthisdiagnosisisimportant,especiallyinpatientswhohaveundergoneIVFandwhoexperienceabdominalpain
orvaginalbleeding.
SerialhCGconcentrationsarenotinterpretableinthepresenceofbothaviableintrauterineandectopicpregnancy.
Onultrasoundexamination,thediagnosisissuggestedbyvisualizationofbothanectopicpregnancyandIUPor
thepresenceofechogenicfluidintheposteriorculdesacinthepresenceofanIUP.Heterotopictubal
pregnancieshavebeenreportedaslateas16weeksofgestation,whileabdominalorrudimentaryhorn
pregnanciescancontinuetodeveloplateingestation[41,42].
Theultrasonographershouldcarefullyexaminenotonlytheuterus,butalsotheadnexaofwomenwhoconceive
followingIVF.WesuggestthatwomenwithaconfirmedIUPwhoareexperiencingabdominalpainorvaginal
bleedingundergoserialTVUSexaminationseveryweekuntilthepossibilityofaconcomitanttubalectopic
pregnancycanbeeliminated.
Thediagnosisandmanagementofheterotopicpregnancyarediscussedseparately.(See"Abdominalpregnancy,
cesareanscarpregnancy,andheterotopicpregnancy",sectionon'Heterotopicpregnancy'.)
UncommonsitesofectopicpregnancyThepossibilitythatanectopicpregnancymayoccurinanontubal
location,orevenbilaterally[43],shouldbeconsidered.Theseectopicpregnancysitesareuncommon,andinclude
cervical,hysterotomyscar,rudimentaryuterinehorn,interstitial,ovarian,andabdominalpregnancy.Regardlessof
thelocation,theendometriumoftenrespondstoovarianandplacentalproductionofpregnancyrelatedhormones,
sovaginalbleedingisacommonsymptom.
Cervicalpregnancyisestimatedtooccurin1/2500to1/18,000pregnanciesandaccountsfor1percentof
ectopicpregnancies[44].
Interstitialpregnancyaccountsforupto1to3percentofectopicpregnancies[45,46].
http://www.uptodate.com/contents/ectopicpregnancyclinicalmanifestationsanddiagnosis?topicKey=OBGYN%2F5487&elapsedTimeMs=4&source=search
9/19
1/17/2016
Ectopicpregnancy:Clinicalmanifestationsanddiagnosis
Ovarianpregnancyoccursin1/2100to1/60,000pregnanciesandaccountsfor1to3percentofectopic
pregnancies[47].
Abdominalpregnancyaccountsforupto1.4percentofectopicpregnancies[48].Thesepregnanciescango
undetecteduntilanadvancedageandoftenresultinseverehemorrhage[49].Ratesofmaternalmortality
havebeenreportedashighas20percent[41,50].
Intramuralpregnancyreferstopregnancyimplantedwithinthemyometriumoftheuterus.Thistypeof
pregnancyisextremelyrarewithlessthan50reportedcasesintheliterature[51].
OvarianpregnancySonographicdiagnosisofanovarianpregnancyisdifficult.Ultrasoundevaluationfor
ovarianpregnancyisdiscussedindetailseparately.(See"Ultrasonographyofpregnancyofunknownlocation".)
Thediagnosisofovarianpregnancyistypicallymadeatthetimeofsurgery,butdifferentiationfromahemorrhagic
ovariancystorpregnancyinthedistalfallopiantubecanbedifficult.Ultrasoundmaysuggestthediagnosis
preoperatively[47].Stricthistopathologicalcriteriaareusedtodistinguishovarianpregnanciesfromthose
originatinginthefallopiantube.Theexactdiagnosisisnotclinicallyimportant,asthesepregnanciesareusually
treatedbysurgicalexcisionoftheinvolvedorgans.Methotrexatetreatmenthasbeensuccessfulincasereports
[52].(See"Ectopicpregnancy:Incidence,riskfactors,andpathology",sectionon'Ovarianpregnancy'.)
InterstitialpregnancyTheinterstitialportionofthefallopiantubeistheproximalsegmentthatisembedded
withinthemuscularwalloftheuterus.Apregnancyimplantedatthissiteiscalledaninterstitialpregnancy(figure
1)thetermcornualpregnancyisalsowidelyusedtodescribeapregnancyatthislocation.Originally,theterm
cornualpregnancyreferredonlytopregnanciesimplantedineitherthehornofabicornuateuterus,arudimentary
hornofaunicornuateuterus,orinonesideofaseptatedorpartiallyseptateduterus[46].
AninterstitialpregnancycanbedifficulttodistinguishonultrasoundfromanIUPthatiseccentricallypositioned.
Ultrasoundevaluationforinterstitialpregnancyisdiscussedindetailseparately.(See"Ultrasonographyof
pregnancyofunknownlocation".)
Grossly,aninterstitialpregnancyappearsasagestationalswellinglateraltotheinsertionoftheroundligament
(figure1)[46].Theuniqueanatomiclocationofaninterstitialpregnancyoftenleadstoadelayindiagnosis,
althoughanaveragedelayofonlyfourdaysincomparisonwithtubalpregnancieswasreportedinalargeseries
[53].
Interstitialpregnancypresentswithruptureinapproximately20to50percentofcases[5456].Aseriesofcases
ofinterstitialpregnancyreportedtoasurgicalregistryincluded14patientswithtubalrupture,allofwhichwere
before12weeks[54].Thisisincontrasttopreviousreportsthatruptureofinterstitialpregnancyoccurredlatein
pregnancy.Otherclinicalmanifestationsarethesameasforallectopicgestations(pelvicorabdominalpain,
vaginalbleeding)[53].
Althoughthematernalmortalityrateassociatedwithtubalpregnancyisdecreasing,therateforinterstitial
pregnanciesremainsat2to2.5percentbecauseofmisdiagnosisofthesegestationsasIUPs.
OthersitesDiagnosisandmanagementofcesareanscarandabdominalpregnancyarediscussedindetail
separately.(See"Abdominalpregnancy,cesareanscarpregnancy,andheterotopicpregnancy".)
ScreeningasymptomaticwomenRoutineprenatalcaredoesnotincludeserialmeasurementofserumhCG.
Theexceptionstothisarewomenathighriskofanectopicpregnancy,includingthosewithanIVFpregnancy,
pregnancyafterreconstructivesurgeryofthefallopiantube,orpriorhistoryofectopicpregnancy.Forwomenwho
aremonitoredinthisway,anectopicpregnancymaypresentwithanabnormalriseinhCG.Thenormalpatternof
theriseinserumhCGinearlypregnancyisdiscussedbelow.(See'Humanchorionicgonadotropin'above.)
Inourpractice,wemonitorwomenathighriskofectopicpregnancy(table1)withlaboratoryandimagingstudies.
Weusethesameprotocolasforthediagnosisofectopicpregnancy,andstartwiththefirstmissedmensesor
afterembryotransferforIVF.Thegoalistoestablishthediagnosisearlytoavoidrupture.(See"Ectopic
http://www.uptodate.com/contents/ectopicpregnancyclinicalmanifestationsanddiagnosis?topicKey=OBGYN%2F5487&elapsedTimeMs=4&source=searc
10/19
1/17/2016
Ectopicpregnancy:Clinicalmanifestationsanddiagnosis
pregnancy:Incidence,riskfactors,andpathology",sectionon'Riskfactors'and"Invitrofertilization",sectionon
'Monitoringforpregnancy'.)
NATURALHISTORYIfleftuntreated,anectopicpregnancyinthefallopiantubecanprogresstoatubal
abortionortubalrupture,oritmayregressspontaneously.
RuptureTubalruptureisusuallyassociatedwithprofoundhemorrhage,whichcanbefatalifsurgeryisnot
performedexpeditiouslytoremovetheectopicgestation.Salpingectomyisthemostcommonsurgical
approachwhenthetubehasruptured.Rupturedectopicpregnancyisthemajorcauseofpregnancyrelated
maternalmortalityinthefirsttrimester[57].Mostofthesedeathsoccurpriortohospitalizationorproximate
tothewoman'sarrivalintheemergencydepartment.
AbortionTubalabortionreferstoexpulsionoftheproductsofconceptionthroughthefimbria.Thiscanbe
followedbyresorptionofthetissueorbyreimplantationofthetrophoblastsintheabdominalcavity(ie,
abdominalpregnancy)orontheovary(ie,ovarianpregnancy).Tubalabortionmaybeaccompaniedbysevere
intraabdominalbleeding,necessitatingsurgicalintervention,orbyminimalbleeding,notrequiringfurther
treatment.
SpontaneousresolutionTheincidenceofspontaneousresolutionofanectopicpregnancyisunknown.In
oneolder(1955)seriesof119hospitalizedpatientswithtypicalectopicpregnancysymptoms,57weresafely
managedexpectantly,withoutsurgicalormedicalintervention(exceptopiates)[58].Itisdifficulttopredict
whichpatientswillexperienceuncomplicatedspontaneousresolution.Potentialcandidatesare
hemodynamicallystablewomenwithaninitialhCGconcentrationlessthan2000IU/Lthatisdeclining[59].
Gestationalproductsleftinthefallopiantubemayresorbcompletelyor,lesscommonly,maycausetubal
obstruction[60].Alternatively,atubalabortionmayoccur.
INFORMATIONFORPATIENTSUpToDateofferstwotypesofpatienteducationmaterials,"TheBasics"and
"BeyondtheBasics."TheBasicspatienteducationpiecesarewritteninplainlanguage,atthe5thto6thgrade
readinglevel,andtheyanswerthefourorfivekeyquestionsapatientmighthaveaboutagivencondition.These
articlesarebestforpatientswhowantageneraloverviewandwhoprefershort,easytoreadmaterials.Beyond
theBasicspatienteducationpiecesarelonger,moresophisticated,andmoredetailed.Thesearticlesarewritten
atthe10thto12thgradereadinglevelandarebestforpatientswhowantindepthinformationandarecomfortable
withsomemedicaljargon.
Herearethepatienteducationarticlesthatarerelevanttothistopic.Weencourageyoutoprintoremailthese
topicstoyourpatients.(Youcanalsolocatepatienteducationarticlesonavarietyofsubjectsbysearchingon
"patientinfo"andthekeyword(s)ofinterest.)
Basicstopics(see"Patientinformation:Ectopicpregnancy(TheBasics)")
BeyondtheBasicstopics(see"Patientinformation:Ectopic(tubal)pregnancy(BeyondtheBasics)")
SUMMARYANDRECOMMENDATIONS
Anectopicpregnancyisanextrauterinepregnancy.Almostallectopicpregnanciesoccurinthefallopiantube
(98percent),butotherpossiblesitesinclude:cervical,interstitial,hysterotomyscar,ovarian,orabdominal.In
rarecases,amultiplegestationmaybeheterotopic(includebothauterineandextrauterinepregnancy).(See
'Introduction'aboveand'Uncommonsitesofectopicpregnancy'above.)
Abdominalpainandvaginalbleedingarethemostcommonsymptomsofectopicpregnancy.Ectopic
pregnancyshouldbesuspectedinanywomenofreproductiveagewiththesesymptoms,especiallythose
whohaveriskfactors(table1).However,over50percentofwomenareasymptomaticbeforetubalrupture
anddonothaveanidentifiableriskfactorforectopicpregnancy.(See'Clinicalpresentation'above.)
Thekeycomponentsoftheevaluationofawomanwithsuspectedectopicgestationareatransvaginal
http://www.uptodate.com/contents/ectopicpregnancyclinicalmanifestationsanddiagnosis?topicKey=OBGYN%2F5487&elapsedTimeMs=4&source=searc
11/19
1/17/2016
Ectopicpregnancy:Clinicalmanifestationsanddiagnosis
ultrasound(TVUS)examinationandquantitativehumanchorionicgonadotropin(hCG)level.ThehCGis
measuredseriallyevery48to72hours.(See'Clinicalprotocol'above.)
Additionaltestingisperformedtoevaluateforanemia,forRh(D)bloodtyping,andforpretreatmentevaluation
forpotentialmethotrexatetherapy.(See'Additionaltesting'above.)
ThediagnosisofectopicpregnancyisaclinicaldiagnosismadebaseduponserialhCGtestingandTVUS.A
diagnosisofectopicpregnancycannotbemadebaseduponasinglehCGresult.Histologicconfirmationof
thediagnosisisnottypicallyrequired.(See'Transvaginalultrasound'aboveand'Humanchorionic
gonadotropin'aboveand'Diagnosis'above.)
ThediagnosticcriteriadependupontherelationshiptothehCGdiscriminatoryzone(serumhCGlevelabove
whichagestationalsacshouldbevisualizedbyTVUSifanintrauterinepregnancy[IUP]ispresent).The
hCGlevelofthediscriminatoryzonevaries,butinmostinstitutionsitis1500to2000IU/L.(See
'Discriminatoryzone'aboveand'Diagnosticcriteria'above.)
IftheserialhCGisrisingabnormally(doesnotincreasebyatleast53percentin48hoursORdoubling
in72hours)andisbelowthediscriminatoryzone,thediagnosisismadebaseduponthehCGpattern.
IfthehCGisabovethediscriminatoryzone,thediagnosisismadebaseduponultrasoundfindingsthat
confirmeitheranintrauterineorextrauterinepregnancy(gestationalsacwithayolksacorembryo).
Diagnosisofruptureofthestructurewithinwhichtheectopicgestationisimplanted(usuallythefallopian
tube)isaclinicaldiagnosismadeprimarilybaseduponafindingofechogenicfluid(consistentwithblood)in
thepelvicculdesacand/orabdomencombinedwiththepresenceofabdominalpainand/ortenderness.(See
'Rupturedversusnonrupturedectopicpregnancy'above.)
UseofUpToDateissubjecttotheSubscriptionandLicenseAgreement.
Topic5487Version25.0
http://www.uptodate.com/contents/ectopicpregnancyclinicalmanifestationsanddiagnosis?topicKey=OBGYN%2F5487&elapsedTimeMs=4&source=searc
12/19
1/17/2016
Ectopicpregnancy:Clinicalmanifestationsanddiagnosis
GRAPHICS
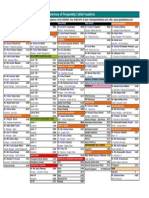
Riskfactorsforectopicpregnancy
Degreeofrisk
High
Moderate
Low
Riskfactors
Oddsratio
Previousectopicpregnancy
9.347
Previoustubalsurgery
6.011.5
Tuballigation
3.0139
Tubalpathology
3.525
InuteroDESexposure
2.413
CurrentIUDuse
1.145
Infertility
1.128
Previouscervicitis(gonorrhea,
chlamydia)
2.83.7
Historyofpelvicinflammatory
disease
2.13.0
Multiplesexualpartners
1.44.8
Smoking
2.33.9
Previouspelvic/abdominal
surgery
0.933.8
Vaginaldouching
1.13.1
Earlyageofintercourse(<18
years)
1.12.5
Forwomenundergoingassistedreproductivetechnology(ART)procedures,theriskofectopic
pregnancyvariesaccordingtothetypeofARTprocedure,thewoman'sreproductivehealth
characteristics,andestimatedembryoimplantationpotential. 1
WomenwhoundergoARTareatmuchhigherriskofheterotopicpregnancythanwomenwho
conceivenaturally(152/100,000versus3.3to6.4/100,000). 2
References:
1. ClaytonHB,SchieveLA,PetersonHB,etal.Ectopicpregnancyriskwithassistedreproductive
technologyprocedures.ObstetGynecol2006107:595.
2. ClaytonHB,SchieveLA,PetersonHB,etal.Acomparisonofheterotopicandintrauterineonly
pregnancyoutcomesafterassistedreproductivetechnologiesintheUnitedStatesfrom1999to
2002.FertilSteril200787:303.
Adaptedfrom:
1. AnkumWM,MolBWJ,VanDerVeenF,BossuytPMM.Riskfactorsforectopicpregnancy:ameta
analysis.FertilSteril199665:1093.
2. MurrayH,BaakdahH,BardellT,TulandiT.Diagnosisandtreatmentofectopicpregnancy.CMAJ
2005173:905.
3. BouyerJ,CosteJ,ShojaeiT,etal.Riskfactorsforectopicpregnancy:acomprehensiveanalysis
basedonalargecasecontrol,populationbasedstudyinFrance.AmJEpidemiol2003157:185.
Graphic82282Version5.0
http://www.uptodate.com/contents/ectopicpregnancyclinicalmanifestationsanddiagnosis?topicKey=OBGYN%2F5487&elapsedTimeMs=4&source=searc
13/19
1/17/2016
Ectopicpregnancy:Clinicalmanifestationsanddiagnosis
Testsforsuspectedectopicpregnancy
EP:ectopicpregnancyIUP:intrauterinepregnancyTVS:transvaginalultrasoundhCG:human
chorionicgonadotropin.
Graphic80606Version2.0
http://www.uptodate.com/contents/ectopicpregnancyclinicalmanifestationsanddiagnosis?topicKey=OBGYN%2F5487&elapsedTimeMs=4&source=searc
14/19
1/17/2016
Ectopicpregnancy:Clinicalmanifestationsanddiagnosis
Significanceoffeaturesassociatedwithectopicpregnancy
Features
SN(percent)
SP(percent)
Clinicalfeatures
Estimatedgestationalage<70days
95
27
Vaginalbleeding
69
26
Abdominalpain
97
15
Abdominaltenderness
85
50
Peritonealsigns
23
95
Cervicalmotiontenderness
33
91
Adnexaltenderness
69
62
Adnexalmass
96
100
89
Separatefromovary
93
99
Cardiacactivity
20
100
Yolksacorembryo
37
100
Tubalring/yolksacorembryo
65
99
Any
63
69
Echogenic
56
96
95
98
Transvaginalultrasound
Nointrauterinegestationalsac
Adnexalmass
FluidinpouchofDouglas
ColorflowDoppler
hCGcombinedwithtransvaginalultrasound
Emptyuterus
1000mIU/mL
4396
86100
1500mIU/mL
4099
8496
2000mIU/mL
3848
8098
1000mIU/mL
73
85
1500mIU/mL
4664
9296
2000mIU/mL
55
96
Adnexalmass*
Sn:sensitivitySp:specificityhCG:betahumanchorionicgonadotropin.
*MassorfluidinculdesacforhCG1500mIU/mLand2000mIU/mL.
Datafrom:Ramakrishnan,K,Scheid,DC.Ectopicpregnancy:Forgetthe"classicpresentation"ifyou
wanttocatchitsooner:Anewalgorithmtoimprovedetection.JournalofFamilyPractice200655:388.
Graphic80277Version3.0
http://www.uptodate.com/contents/ectopicpregnancyclinicalmanifestationsanddiagnosis?topicKey=OBGYN%2F5487&elapsedTimeMs=4&source=searc
15/19
1/17/2016
Ectopicpregnancy:Clinicalmanifestationsanddiagnosis
Causesofabnormalgenitaltractbleedinginwomen
Genitaltractdisorders
Uterus
Benigngrowths:
Trauma
Sexualintercourse
Sexualabuse
Endometrialhyperplasia
Foreignbodies(includingintrauterine
device)
Adenomyosis
Pelvictrauma(eg,motorvehicleaccident)
Leiomyomas(fibroids)
Straddleinjuries
Endometrialpolyps
Cancer:
Endometrialadenocarcinoma
Sarcoma
Infection:
Pelvicinflammatorydisease
Endometritis
Ovulatorydysfunction
Cervix
Benigngrowths:
Cervicalpolyps
Ectropion
Endometriosis
Cancer:
Invasivecarcinoma
Metastatic(uterus,choriocarcinoma)
Infection:
Cervicitis
Vulva
Benigngrowths:
Skintags
Sebaceouscysts
Condylomata
Angiokerataoma
Cancer
Vagina
Benigngrowths:
Gartnerductcysts
Polyps
Drugs
Contraception:
Hormonalcontraceptives
Intrauterinedevices
Postmenopausalhormonetherapy
Anticoagulants
Tamoxifen
Corticosteroids
Chemotherapy
Phenytoin
Antipsychoticdrugs
Antibiotics(eg,duetotoxicepidermal
necrolysisorStevensJohnsonsyndrome)
Systemicdisease
Diseasesinvolvingthevulva:
Crohn'sdisease
Behcet'ssyndrome
Pemphigoid
Pemphigus
Erosivelichenplanus
Lymphoma
Bleedingdisorders:
vonWillebranddisease
Thrombocytopeniaorplateletdysfunction
Acuteleukemia
Somecoagulationfactordeficiencies
Advancedliverdisease
Thyroiddisease
Adenosis(aberrantglandulartissue)
http://www.uptodate.com/contents/ectopicpregnancyclinicalmanifestationsanddiagnosis?topicKey=OBGYN%2F5487&elapsedTimeMs=4&source=searc
16/19
1/17/2016
Ectopicpregnancy:Clinicalmanifestationsanddiagnosis
Cancer
Polycysticovarysyndrome
Vaginitis/infection:
Chronicliverdisease
Bacterialvaginosis
Cushing'ssyndrome
Sexuallytransmitteddiseases
Hormonesecretingadrenalandovarian
tumors
Atrophicvaginitis
Uppergenitaltractdisease
Renaldisease
Fallopiantubecancer
Emotionalorphysicalstress
Ovariancancer
Smoking
Pelvicinflammatorydisease
Excessiveexercise
Pregnancycomplications
Diseasesnotaffectingthegenital
tract
Urethritis
Bladdercancer
Urinarytractinfection
Inflammatoryboweldisease
Hemorrhoids
Other
Endometriosis
Vasculartumorsandanomaliesinthe
genitaltract
Graphic74527Version8.0
http://www.uptodate.com/contents/ectopicpregnancyclinicalmanifestationsanddiagnosis?topicKey=OBGYN%2F5487&elapsedTimeMs=4&source=searc
17/19
1/17/2016
Ectopicpregnancy:Clinicalmanifestationsanddiagnosis
Algorithmvaginalbleeding
*Thisstepmaybeomittedinwomenwhoareknowntohaveanintrauterinepregnancy.
Proceeddirectlytoultrasoundexamination.
Graphic68130Version2.0
http://www.uptodate.com/contents/ectopicpregnancyclinicalmanifestationsanddiagnosis?topicKey=OBGYN%2F5487&elapsedTimeMs=4&source=searc
18/19
1/17/2016
Ectopicpregnancy:Clinicalmanifestationsanddiagnosis
Normalfemalereproductiveanatomy
Graphic55921Version2.0
http://www.uptodate.com/contents/ectopicpregnancyclinicalmanifestationsanddiagnosis?topicKey=OBGYN%2F5487&elapsedTimeMs=4&source=searc
19/19
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- 9 To 5 Props PresetsDocumento4 páginas9 To 5 Props Presetsapi-300450266100% (1)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Vturn-NP16 NP20Documento12 páginasVturn-NP16 NP20José Adalberto Caraballo Lorenzo0% (1)
- Use Acupressure to Conceive FasterDocumento15 páginasUse Acupressure to Conceive Fastersale18100% (1)
- UMR Introduction 2023Documento110 páginasUMR Introduction 2023tu reves mon filsAinda não há avaliações
- Roadblocks Overcome Cruise PurchaseTITLE Top 15 Cruise Hesitations Answered TITLE How to Convince People Cruises Worth CostDocumento4 páginasRoadblocks Overcome Cruise PurchaseTITLE Top 15 Cruise Hesitations Answered TITLE How to Convince People Cruises Worth CostJanel Castillo Balbiran33% (3)
- PHAR342 Answer Key 5Documento4 páginasPHAR342 Answer Key 5hanif pangestuAinda não há avaliações
- Ucg200 12Documento3 páginasUcg200 12ArielAinda não há avaliações
- Diagnostic and Statistical Manual of Mental Disorders: Distinction From ICD Pre-DSM-1 (1840-1949)Documento25 páginasDiagnostic and Statistical Manual of Mental Disorders: Distinction From ICD Pre-DSM-1 (1840-1949)Unggul YudhaAinda não há avaliações
- Guide Propedevt Stomat 2c EngDocumento256 páginasGuide Propedevt Stomat 2c EngJhoel Jhonatan Torres MuñozAinda não há avaliações
- HVDC BasicDocumento36 páginasHVDC BasicAshok KumarAinda não há avaliações
- Ic Audio Mantao TEA2261Documento34 páginasIc Audio Mantao TEA2261EarnestAinda não há avaliações
- Slaked Lime MSDS Safety SummaryDocumento7 páginasSlaked Lime MSDS Safety SummaryFurqan SiddiquiAinda não há avaliações
- Impact of Covid-19 On Audit Quality: Presented byDocumento13 páginasImpact of Covid-19 On Audit Quality: Presented byMST. SADIYA SULTANAAinda não há avaliações
- Grab Go Porter S 5 ForcesDocumento2 páginasGrab Go Porter S 5 ForcesUtkarsh SharmaAinda não há avaliações
- Schneider Electric PowerPact H-, J-, and L-Frame Circuit Breakers PDFDocumento3 páginasSchneider Electric PowerPact H-, J-, and L-Frame Circuit Breakers PDFAnonymous dH3DIEtzAinda não há avaliações
- Directory of Frequently Called Numbers: Maj. Sheikh RahmanDocumento1 páginaDirectory of Frequently Called Numbers: Maj. Sheikh RahmanEdward Ebb BonnoAinda não há avaliações
- Chapter 21Documento39 páginasChapter 21Hamza ElmoubarikAinda não há avaliações
- Full SyllabusDocumento409 páginasFull SyllabusSanthana BharathiAinda não há avaliações
- 2.1. Pharmacological Therapeutics. 2.2. Basic Cardiac Life Support (BCLS) and Advanced Cardiac Life Support (ACLS) in Neonates and ChildDocumento3 páginas2.1. Pharmacological Therapeutics. 2.2. Basic Cardiac Life Support (BCLS) and Advanced Cardiac Life Support (ACLS) in Neonates and Childclint xavier odangoAinda não há avaliações
- Nursing Plan of Care Concept Map - Immobility - Hip FractureDocumento2 páginasNursing Plan of Care Concept Map - Immobility - Hip Fracturedarhuynh67% (6)
- Auramo Oy spare parts listsDocumento12 páginasAuramo Oy spare parts listsYavuz ErcanliAinda não há avaliações
- Book 1Documento94 páginasBook 1JOHNAinda não há avaliações
- Maximizing Oredrive Development at Khoemacau MineDocumento54 páginasMaximizing Oredrive Development at Khoemacau MineModisa SibungaAinda não há avaliações
- BS 5911-120Documento33 páginasBS 5911-120Niranjan GargAinda não há avaliações
- Elem. Reading PracticeDocumento10 páginasElem. Reading PracticeElissa Janquil RussellAinda não há avaliações
- Female Reproductive System Histology IDocumento5 páginasFemale Reproductive System Histology ISolomon Seth SallforsAinda não há avaliações
- Consumer Behaviour: Group ProjectDocumento5 páginasConsumer Behaviour: Group ProjectAanchal MahajanAinda não há avaliações
- Pack Alimentacion Clin in Perin 14Documento194 páginasPack Alimentacion Clin in Perin 14Paz BustosAinda não há avaliações
- Pulsar2 User Manual - ENDocumento83 páginasPulsar2 User Manual - ENJanette SouzaAinda não há avaliações
- Hotel Housekeeping EQUIPMENTDocumento3 páginasHotel Housekeeping EQUIPMENTsamahjaafAinda não há avaliações