Escolar Documentos
Profissional Documentos
Cultura Documentos
Perspective of Synaptic Protection After Post-Infarction Treatment With Statins
Enviado por
DrGasnasTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Perspective of Synaptic Protection After Post-Infarction Treatment With Statins
Enviado por
DrGasnasDireitos autorais:
Formatos disponíveis
Gutirrez-Vargas et al.
Journal of Translational Medicine (2015) 13:118
DOI 10.1186/s12967-015-0472-6
REVIEW
Open Access
Perspective of synaptic protection after
post-infarction treatment with statins
Johanna Andrea Gutirrez-Vargas1, Angel Cespedes-Rubio1,2 and Gloria Patricia Cardona-Gmez1*
Abstract
Stroke is the second most common cause of death in people over 45 years of age in Colombia and is the leading
cause of permanent disability worldwide. Cerebral ischemia is a stroke characterized by decreased blood flow due
to the occlusion of one or more cerebral arteries, which can cause memory problems and hemiplegia or paralysis,
among other impairments. The literature contains hundreds of therapies (invasive and noninvasive) that exhibit a
neuroprotective effect when evaluated in animal models. However, in clinical trials, most of these drugs do not
reproduce the previously demonstrated neuroprotective property, and some even have adverse effects that had
not previously been detected in animal experimentation.
Statins are drugs that inhibit 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase, the rate-limiting
enzyme in cholesterol synthesis. Several studies have shown that statin therapy in an animal model of focal cerebral
ischemia reduces infarct volume, as well as markers of neurodegeneration, activates neuronal survival pathways,
and improves performance on learning and memory tests. Given the implied therapeutic benefit and the limited
understanding of the mechanism of action of statins in brain repair, it is necessary to address the biochemical
and tissue effects of these drugs on synaptic proteins, such as NMDA receptors, synaptic adhesion proteins, and
cytoskeletal proteins; these proteins are highly relevant therapeutic targets, which, in addition to giving a structural
account of synaptic connectivity and function, are also indicators of cellular communication and the integrity of the
bloodbrain barrier, which are widely affected in the long term post-cerebral infarct but, interestingly, are protected
by statins when administered during the acute phase.
Keywords: Cerebral ischemia, Statins, Synaptic proteins, Synaptic plasticity, Post-infarct protection
Introduction
Stroke is the third leading cause of death in industrialized
countries [1] and the most common cause of disability in
adults worldwide [2]. In Latin America, the main causes of
the risk of death are cardiovascular accidents and stroke
due to a sedentary lifestyle, diabetes, atherosclerosis,
smoking, and hypertension. These diseases also increase
the risk of developing neurodegenerative diseases, such
as Alzheimer and vascular dementia [3].
Industrialized countries have turned their interest to the
aforementioned health issues as increasing life expectancy
has made them more prevalent in most of the world, becoming the silent epidemic of the current millennium. Developing countries are also increasing their life expectancy,
* Correspondence: patricia.cardonag@udea.edu.co
1
Cellular and Molecular Neurobiology Area, Group of Neuroscience of
Antioquia, School of Medicine, SIU, University of Antioquia UdeA, Calle 70
No. 52-21, Medelln, Colombia
Full list of author information is available at the end of the article
and this disorder is beginning to become a public health
problem with few current alternatives for healing.
Cerebral ischemia
Cerebral ischemia is a type of stroke characterized by a
transient or permanent reduction in blood flow due to
embolic or thrombotic occlusion of one or more cerebral
arteries [4,5]. Depending on the duration of the reduced
blood flow and infarct location, cerebral ischemia can
cause various clinical manifestations, including paralysis
or hemiplegia, aphasia, and deficits in learning and memory processes, among other clinical manifestations [6].
If blood vessels that supply blood to all or most of the
brain become clogged, the injury is called global ischemia,
which usually happens during a heart attack or severe systemic hypotension [7]. However, if only the occlusion of
vessels supplying blood to a certain area of the brain occurs, a focal ischemia is generated [8]. Approximately 80%
2015 Gutirrez-Vargas et al.; licensee BioMed Central. This is an Open Access article distributed under the terms of the
Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use,
distribution, and reproduction in any medium, provided the original work is properly credited. The Creative Commons Public
Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this
article, unless otherwise stated.
Gutirrez-Vargas et al. Journal of Translational Medicine (2015) 13:118
Page 2 of 9
of cases of focal ischemia result from occlusion of the
middle cerebral artery (MCA) [9].
In focal ischemia, the region that suffers the most severe degree of hypoperfusion progresses rapidly towards
irreversible damage due to a necrotic death, which represents the ischemic core. This area exhibits low cerebral
blood flow (<10% of the baseline value) and the irreversible failure of energy metabolism [10]. The remaining
hypoperfused tissue surrounding the ischemic core has
an imbalance in the mechanisms of the autoregulation
of blood flow and is known as the penumbra zone [11,12].
In this region, neurons show alterations in functionality,
although they retain a minimum metabolic activity that
preserves structural integrity for a longer period of time,
following a pattern of apoptotic death (Figure 1A) [13,14].
The penumbra is potentially recoverable and, as such, represents a key target for therapeutic intervention in cerebral ischemia [15]; however, unless perfusion is improved
or the cells become relatively resistant to the injury, the
cells of the penumbra zone are at risk of dying within a
few hours by necrosis [10,16].
response to the released neurotransmitter, which allows
the transmission of information (Figures 1B, 2A) [19,20].
Among neurotransmitter receptors, NMDA receptors
have been extensively studied because they represent the
largest subclass of glutamate receptors in mammalian
excitatory synapses. They consist of four subunits, two
of which are NR1 combined with NR2 (NR2A-D) or NR3
(NR3A-B) subunits [21]. These receptors play a central
role in synaptic transmission, neuronal plasticity, regulation of neuronal development, and connectivity, as well as
in memory and learning processes, primarily due to their
permeability to Ca2+ [22-24].
Located at the synapses, the NMDA receptors are not
static proteins; in fact, the number and composition of
NMDA receptors can be modified, which provides a dynamic mechanism for the regulation of synaptic efficacy
and remodeling [25]. Different regions of the receptor,
as well as scaffold proteins, such as PSD-95, and other
proteins of the postsynaptic density, all participate in the
mechanisms of internalization of NMDA. NMDA receptors that bind to PSD-95 are stable in the membrane and
are less likely to be internalized (Figures 1B, 2A), while receptors that are not bound to proteins of the postsynaptic
density can be readily internalized. This mechanism can
remove from the membrane surface NMDA receptors
that are not permanent at the synapse [26].
The overactivation of NMDA receptors in cerebral ischemia induces excitotoxic cell death. Excessive activation
of NMDA induces a rapid and specific transcriptional inhibition of the NR1 subunit promoter in a process that is
strictly dependent on Ca2+ influx through the receptor.
NR1 transcriptional inhibition results in a progressive
reduction of its mRNA, which leads to a progressive reduction of the protein [27]. Overstimulation of NMDA
receptors can lead to a progressive decline in receptor
activity because its functionality depends strictly on the
expression of hetero-oligomers NR1/NR2 on the cell
surface [28].
Studies have shown that NR2A and NR2B subunits play
different roles in excitotoxic cell death [29]. While inhibition of NR2B induces cell death and prevents motor and
cognitive recovery [30], inhibition of the NR2A subunit
leads to cell survival in a model of cerebral ischemia [29].
In models of excitotoxicity, it has been seen that excessive
activation of the NMDA receptors leads to increased intracellular calcium, which results in the activation of calpain,
a protease that mediates cellular toxicity [31,32]. This protease efficiently cuts the C-terminal region of the NR2A
and NR2B subunit, producing truncated subunits that lack
certain sequences near serine-1303, which are critical to
the formation of signaling complexes in the postsynaptic
membrane [33]. The end result is the uncoupling of
NMDA receptors from scaffolding proteins, such as PSD95 (Figures 1C, 2B), affecting synaptic function [32].
Excitotoxicity in cerebral ischemia
The interruption of blood flow into the brain due to ischemia results in the deprivation of oxygen and glucose, reducing the energy available for the operation of brain cells
[8]. Neurons in particular become unable to maintain the
ion gradients needed for cell function and homeostasis
[17], which results in excessive neuronal depolarization,
increased release of excitatory neurotransmitters, and reduced capacity of the reuptake of these neurotransmitters
by astrocytes. The overloading of glutamate, the main
excitatory neurotransmitter in the central nervous system (CNS) of mammals, leads to prolonged stimulation
of AMPA ionotropic glutamate receptors (-amino-3hydroxy-5-methyl-4-isoxazolepropionic acid) and NMDA
receptors (N-methyl-D-aspartic acid), dramatically increasing the influx of calcium (Ca2+), sodium (Na+), potassium (K+), and water into the neurons [18]. Excessive
accumulation of ions and the simultaneous dysregulation
of various signaling pathways activate catabolic processes
mediated by proteases, lipases, and nucleases, which disrupt neuronal function and lead to cell death [8,17].
Cerebral ischemia and alteration of synaptic
proteins
Ionotropic Receptors
After the establishment of neuronal connections during
development, the synapse remains highly dynamic and
undergoes changes in morphology and efficiency, which
are dependent on activity. The presynaptic terminal includes the machinery for neurotransmitter release, while
post-synaptic sites include proteins such as neurotransmitter receptors and signaling proteins that promote the
Gutirrez-Vargas et al. Journal of Translational Medicine (2015) 13:118
Figure 1 (See legend on next page.)
Page 3 of 9
Gutirrez-Vargas et al. Journal of Translational Medicine (2015) 13:118
Page 4 of 9
(See figure on previous page.)
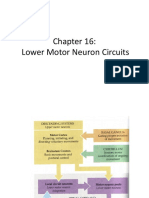
Figure 1 Neurodegeneration and protection in a focal cerebral ischemia model in rats. A) Histopathology of focal cerebral ischemia (tMCAO)
model in rats. a) Panoramic representative image of a whole rat brain with tMCAO injury. b) Contralateral and ipsilateral images from cerebral
ischemic rat tissue with Hematoxilin-eosin staining at the 3,80 mm bregma. LH = left hemisphere, RH = Right hemisphere, square = Selected area
from CA1 area. Scale bar = 1,7 mm. c), d), e) Left side representative images from Sham rats and Right side representative images from ischemic
rats. c) Hematoxilin-eosin staining 100x from CA1 square in b). Scale bar = 50 m. d) Hyperphosphorylated tau immunoreactivity (AT-8) staining
40X in CA1 area. Scale bar = 70 m. e) Fluorojade staining 10x. Scale bar = 100 m. B), C) and D) Comparative hypothetical model of synaptic
proteins alteration following cerebral ischemia and Atorvastatin treatment. B) Sham, C) Ischemia and D) ATV-treated ischemia. B) Synaptic
complexes formed by proteins of synaptic adhesion (cadherins and catenins), glutamate receptors, and scaffold proteins, such as PSD-95 are
associated in a normal condition (Sh = Sham). C) Glutamate receptors are uncoupled from PSD-95 and are accumulated in the cytoplasm due to
retention of subunits in the endoplasmic reticulum (ER) because of the loss of transport toward synapses due to the alteration of microtubules
and the cytoskeleton. Proteins that regulate the cytoskeleton, such as RhoA increased and synaptic complexes formed by the complex cadherins/
catenins, glutamate receptors, and post-synaptic proteins, such as PSD-95 are lost. D) Model of protection by statins after cerebral ischemia.
Synaptic complexes formed by proteins of synaptic adhesion (cadherins and catenins), glutamate receptors, and scaffold proteins, such as PSD-95
are restored in synapse, inducing neuronal connectivity. ISCH= Ischemia, ATV = Atorvastatin.
The results obtained in our research group show that
subunits of NMDA receptors are expressed in the cytoplasm following ischemia [30], which may be related to a
deficiency in the assembly of the different subunits making up the receiver and/or problems in the transport
from the receptor to the synapses (Figure 1C). In the
knockout mouse for NR1, both reduction in the dendritic
distribution and accumulation in the cytoplasm of the
NR2B subunit [34] are observed, perhaps because of the
loss of the assembly of functional NMDA receptors to
the synaptic membrane or because NMDA receptors with
NR2B subunits located in the synaptic density are internalized by endocytosis to perform autoregulation and
avoid the continuous influx of calcium. It is known that
clathrin-mediated endocytosis is a mechanism that regulates the synaptic expression of NMDA receptors containing NR2B during synaptic maturation in processes
such as long-term potentiation (LTP) or long-term depression (LTD) as well as in response to a ligand [35].
Cytoskeletal proteins and cell adhesion
Transport from the receptor to and from synaptic sites
may be lost due to alteration of the microtubules and
damage to the actin cytoskeleton [36] (Figure 1C),
microtubule-associated proteins (MAP2) involved in the
regulation of vesicle transport during development or
regeneration of neuronal processes [37]. Our work and
other previous studies have found that these proteins
are redistributed in the soma after the acute post-ischemia
period [38,39], which is considered an indicator of excitotoxic damage and loss of microtubule stability [38,39]
(Figure 1C). The actin cytoskeleton is primarily mediated
by the Rho GTPases, proteins that regulate its maintenance, remodeling, and stability [40]. The RhoA and Rac1
proteins are among the most studied of the Rho GTPases.
In general terms, RhoA regulates actin assembly associated with processes of cellular shrinkage due to stress
[41,42], while Rac regulates actin polymerization, which is
related to axonal growth and stability and the increase of
dendritic processes [41,43]. Our research shows that RhoA
activity is increased in excitotoxic death processes [44]
(Figures 1C, 2B), and inhibiting this activity reduces
markers of neurodegeneration as well as improves
learning and memory processes in cerebral ischemia
[45]. Complementarily, in the acute post-ischemia period
(24 hours), Rac1 activity decreases and this protein is
redistributed in the soma and in aberrant neuronal processes, which forms part of the process of chronic neurodegeneration [38].
Disassembly of the cytoskeleton in cerebral ischemia
mediated by RhoA activation and inactivation of Rac is
associated with the disruption of synaptic adhesion mediated by the complex of cadherin/catenins and [40],
proteins that are present in both presynaptic and postsynaptic sites. Cadherins promote cell adhesion, and their
association with catenins allows the control of different
intracellular signaling pathways [19,46,47]. Structurally,
cadherins have an extracellular domain comprising most
of the polypeptide chain, generally composed of five repetitions, four of which are capable of binding extracellular
calcium. This extracellular domain mediates calciumdependent homophilic interactions with cadherins of
adjacent neurons. The cytoplasmic region includes the
binding sites to a variety of proteins, including catenins
[48]. Catenins are cytosolic proteins that are basically
subdivided into three groups: -catenin, N-catenin,
and p120 catenin (p120 ctn). The distal region of the
cadherins cytoplasmic domain includes the binding site
for -catenin, while the nearest region to the membrane
contains the binding site for family members of p120
ctn. The protein N-catenin binds to the complex by
binding with -catenin [19].
In our recent studies using a model of focal ischemia in
rats, the levels of N-cadherin, p120 catenin, and N catenin in the cerebral cortex and hippocampus were significantly reduced, as was their association with PSD-95 and
glutamate receptors (NMDA and AMPA) (Figures 1C,
2B), which represents the loss of synaptic adhesion and of
Gutirrez-Vargas et al. Journal of Translational Medicine (2015) 13:118
Page 5 of 9
Figure 2 Schematic representations of cell signalling alteration following cerebral ischemia and Atorvastatin treatment. A) Sham, B) Ischemia and C) ATVtreated ischemia. A) NMDA receptors, synaptic adhesion proteins and PSD-95 are associated in the synapse. The stability of the actin cytoskeleton is
regulated by the RhoGTPasas (Rac, RhoA) balance and microtubules by protein such as MAP2. B) After cerebral ischemia cell adhesion is lost by alteration
in the cadherin-catenin complex; NMDA receptors and PSD-95 protein are distributed to the cytoplasm. The increased activity of RhoA, destabilizes actin
cytoskeleton and GSK3b activation leads to tau hyperphosphorylation disassembling microtubules. C) Treatment with atorvastatin recovers the adhesion
protein complex as well as the location NMDA receptor synapses associated to PSD-95. Additionally atorvastatin leads to AKT activation promoting cell
survival. Recovery of the actin cytoskeleton is mediated by the increased activity of Rac and RhoA reduction, and finally atorvastatin stabilize microtubules.
Gutirrez-Vargas et al. Journal of Translational Medicine (2015) 13:118
Page 6 of 9
complexes associated with synaptic plasticity [44]. Additionally, there was an interdependence between Rac activity and the N catenin distribution in dendrites, which
was lost in the event of glutamate excitotoxicity in primary
neuronal cultures [49].
Glycogen synthase kinase-3 (GSK-3) is an essential
protein downstream of Akt that is involved in the pathological process of brain damage. The PI3K/Akt signal
transduction pathway may affect the activity of GSK-3.
Active Akt inhibits GSK-3 activity via phosphorylation
[50]. Sustained activation of GSK-3 is pro-apoptotic in
cerebral ischemia, because this leads to hyperphosphorylation of tau, microtubule destabilization (Figure 2B) and
cognitive impairment.
The foregoing are some of the cellular and biochemical events underlying the impairment and neuronal
death after cerebral ischemia; however, it is important to
understand the precise mechanisms of the proteins
involved in the synapse, and their implication in morphological and functional recovery. Such knowledge is
invaluable in the development of effective neuroprotective strategies to achieve an improved clinical outcome,
which results not only in survival but also in a higher
quality of life for patients who suffer acute cerebrovascular events, and to reduce or prevent long-term physical
and mental consequences.
III, used Rosuvastatin on early window for preventing
recurrence of ischemic stroke.
However, in addition to their effect on the lipid
profile, statins are also credited with effects that are independent of the reduction of cholesterol synthesis,
called pleiotropic effects. By inhibiting the conversion of
hydroxy-methylglutaryl Coenzyme A (HMG-CoA) to Lmevalonate, statins block the synthesis of important
isoprenoids, such as farnesyl pyrophosphate (FPP) and
geranylgeranyl pyrophosphate (GGPP), which are important intermediates for the post-translational modification
of Rho GTPases (RhoA, Rac, and Cdc42) [53]. Among the
pleiotropic effects reported in cerebral ischemia are the improvement of endothelial function, the stability of the atherosclerotic plaque, the attenuation of oxidative stress and
inflammation, and the inhibition of the thrombogenic response [53]. Previous studies conducted on cerebral ischemia showed that statins improve neurological function
and increase cerebral blood flow [55-57], mitigating the
effects of inflammation and post-traumatic hypoperfusion
[53], in addition to protecting blood vessels and promoting the processes of angiogenesis, neurogenesis, and synaptogenesis after cerebral ischemia [58].
Using an embolic model, simvastatin-treated rats showed
a significant infarct volume reduction and neurological improvement compared to vehicle-treated group. Analyzing
their homogenated brains by two-dimensional fluorescence
Difference in Gel Electrophoresis (DIGE) technology, observed that the protective effect of simvastatin can be
attributable to oxidative stress response attenuation and
bloodbrain barrier protection after cerebral ischemia [59].
There are some additional evidences in humans, where the
treatment with statins is not only associated to a reduced
incidence of stroke but with reduced stroke severity, as
well [60]. In a small pilot trial with simvastatin in acute ischemic stroke (AIS), Montaner et al. showed more cases of
complete functional recovery after 3 months of treatment
with simvastatin (40 mg/day) in comparison with the nontreated group (p < 0.05). The significant improvement was
observed on the third day of treatment [61].
A study by Kawashima et al. showed that cerivastatin
reduce the stroke-associated infiltration of inflammatory
cells, superoxide production in the cerebral parenchyma,
and cerebral damage caused by stroke, as well as delay
the appearance of stroke-associated symptoms and death
in stroke-prone, spontaneously hypertensive rats [62]. Recently, we found that atorvastatin treatment increases the
expression of brain-derived neurotrophic factor (BDNF)
in an NR2B-dependent manner [30]; this trophic factor is
involved in survival [63] and is correlated with motor recovery and with spatial learning and memory (29). We
also confirmed that statins activate the PI3K/Akt pathway
(Figure 2C) and Ras/Erk, which transduce survival signals
and in turn promote synaptic plasticity [44].
Statins as treatment after a cerebral ischemia
The pharmacological approach for inducing neuroprotection after an injury due to cerebral ischemia aims at
blocking signaling pathways that trigger cell death, to induce synaptic connectivity, and functional recovery. The
main goal is to limit the devastating consequences of reduced blood flow in the penumbra zone induced by reperfusion [14,51].
Statins are the drugs of choice for the treatment of
hypercholesterolemia that lower low density lipoproteins
(LDL) and triglycerides [52]. The mechanism of action
of these drugs is via competitive and selective inhibition
of 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA)
reductase, the rate-limiting enzyme in cholesterol synthesis because it is responsible for the conversion of 3hydroxy-3-methylglutaryl CoA to mevalonate, which is
a precursor of cholesterol [52,53]. Studies such as the
Heart Protection Study, in which statin therapy significantly reduces the coronary mortality rate and incidence of stroke, confirm the need for strict control of
the lipid profile to reduce the overall risk and the
mortality rate caused by cardiovascular diseases and
stroke [54]. Also, a recently completed clinical trial,
NCT02225834 in phase IV, used Atorvastatin as acute
stroke treatment to evaluate separate effects on immunoinflamatory markers and atherothorombosis; or a recently terminated clinical trial, NCT01364220 in phase
Gutirrez-Vargas et al. Journal of Translational Medicine (2015) 13:118
Effect of statins on synaptic proteins
In an experimental model of focal cerebral ischemia, we
describe that in addition to neurological recovery and
the reduction of infarct volume and of neurodegeneration
markers, statin therapy during the acute post-ischemia
phase achieves the restoration of proteins involved in neuronal connectivity, such as NMDA receptors [30], synaptic
adhesion proteins (cadherins and catenins) and cytoskeletal
proteins (RhoA and Rac) [44]. Atorvastatin restores the
levels of N-cadherin, p120 catenin and N catenin protein
in the cerebral cortex and in the hippocampus along with
the association of this complex of cadherins/catenins with
the PSD-95 protein (Figure 1D) [44]. These findings
support the restoration of synaptic complexes in cerebral
ischemia following statin therapy. Additionally, we have
found that atorvastatin treatment prevents the cytoplasmic distribution of subunits of glutamate receptors (NR1,
NR2B NMDA) and recovers their association with PSD95 and with proteins of synaptic adhesion (Figure 1D)
[30]. The latter is related to the recovery of microtubule
stability due to statin therapy, as MAP2 immunoreactivity
is restored both in the somatosensory cortex and in the
hippocampus [30,44], enabling the transport of the receptors and their stability at the synapses (Figure 1 D). The
recovery of synaptic molecular complexes that involve
NMDA receptors and synaptic adhesion proteins is correlated with a recovery of the motor and spatial learning
and memory deficits caused by ischemia [30].
Complementarily, we describe that atorvastatin postischemia treatment tended to reduce RhoA activity which
leads to recovery the actin cytoskeleton (Figure 2C) [44].
By down-regulating Rho/Rho kinase signaling pathways,
statins increase the stability of eNOS mRNA and induce
activation of eNOS through phosphatidylinositol 3-kinase/
Akt/eNOS pathway restoring endothelial function [64].
The beneficial effects of Akt activation are not limited to
eNOS phoshorylation but extend to the promotion of survival neuronal (Figure 2C).
Perspective
It is becoming necessary to advance both theoretically
and experimentally in the study of the factors involved
in cerebral ischemia and in the rigorous evaluation of
the drugs to be used and, with these results, to be able
to impact more precisely a population at increased risk
of suffering stroke. The purpose is to prevent, block, or
meet the needs of the affected community not only in
the short-term but also in the medium- and long-term
post-cerebral infarct period. This development must be
accompanied by training and improving the expertise
necessary for diagnosis and for making decisions in clinical treatment inside and outside the therapeutic window
as well as by prevention programs designed to reduce
Page 7 of 9
neurodegenerative disorders in general and to improve
quality of life and access to health services.
According to the above, our work has specifically contributed to elucidating the mechanisms of pathogenesis
and therapy in cerebral ischemia as well as to the understanding of the mechanisms and the cellular and molecular
targets of protection by statins. Our previous results and
the issues raised in this review allow us to recommend
from preclinical study in rats that atorvastatin, a drug
already on the market for human consumption as a
treatment for hypercholesterolemia, could be used as a
protective treatment during the first 6 hours postischemic infarct. Its administration for at least three
days and ideally longer, with attention to the patients
adherence to the drug and its quality, could potentially
reduce or prevent the medium- and long-term severity
of neurologic dysfunction and of emotional and cognitive compromise in patients.
Conclusion
In summary, statin therapy after a cerebral infarct blocks
the spread of damage and helps to restore brain morphology and functionality, at least based on the induction
of trophic factors such as BDNF and of cell adhesion
proteins that generate a platform for synaptic proteins,
such as PSD-95, and NMDA receptors to settle and generate synaptic connectivity, neurotransmission, and cognitive and motor function recovery.
Competing interests
The authors declare that they have no competing interests.
Authors contributions
All authors reviewed, edited and approved the final manuscript.
Acknowledgments
We would like to thank AJE for editing the manuscript and Tania Marquez
for assistance in maintaining the rat colonies in the SPF vivarium of the
University of Antioquia. This research was supported by Colciencias (project
# 111545921467); CODI, University of Antioquia, Colombia.
Author details
1
Cellular and Molecular Neurobiology Area, Group of Neuroscience of
Antioquia, School of Medicine, SIU, University of Antioquia UdeA, Calle 70
No. 52-21, Medelln, Colombia. 2Neurodegenerative Diseases Research Group,
Department of Animal Health - Faculty of Veterinary Medicine - University of
Tolima, Ibague, Colombia.
Received: 28 October 2014 Accepted: 23 March 2015
References
1. Lo EH, Dalkara T, Moskowitz MA. Mechanisms, challenges and opportunities
in stroke. Nat Rev Neurosci. 2003;4:399415.
2. Donnan GA. International Journal of Stroke. Editorial. Int J Stroke. 2008;3:157.
3. Imfeld P, Bodmer M, Schuerch M, Jick SS, Meier CR. Risk of incident stroke in
patients with Alzheimer disease or vascular dementia. Neurology.
2013;81:9109.
4. Briones TL, Suh E, Jozsa L, Woods J. Behaviorally induced synaptogenesis
and dendritic growth in the hippocampal region following transient global
cerebral ischemia are accompanied by improvement in spatial learning.
Exp Neurol. 2006;198:5308.
Gutirrez-Vargas et al. Journal of Translational Medicine (2015) 13:118
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
Gao J, Duan B, Wang DG, Deng XH, Zhang GY, Xu L, et al. Coupling
between NMDA receptor and acid-sensing ion channel contributes to
ischemic neuronal death. Neuron. 2005;48:63546.
Kemp JA, McKernan RM. NMDA receptor pathways as drug targets. Nat
Neurosci. 2002;5(Suppl):103942.
Traystman RJ. Animal models of focal and global cerebral ischemia. ILAR J.
2003;44:8595.
Dirnagl U, Iadecola C, Moskowitz MA. Pathobiology of ischaemic stroke: an
integrated view. Trends Neurosci. 1999;22:3917.
Durukan A, Tatlisumak T. Acute ischemic stroke: overview of major
experimental rodent models, pathophysiology, and therapy of focal cerebral
ischemia. Pharmacol Biochem Behav. 2007;87:17997.
Lo EH. A new penumbra: transitioning from injury into repair after stroke.
Nat Med. 2008;14:497500.
Baron JC. Perfusion thresholds in human cerebral ischemia: historical
perspective and therapeutic implications. Cerebrovasc Dis.
2001;11 Suppl 1:28.
Moustafa RR, Baron JC. Pathophysiology of ischaemic stroke: insights from
imaging, and implications for therapy and drug discovery. Br J Pharmacol.
2008;153 Suppl 1:S4454.
Mies G, Iijima T, Hossmann KA. Correlation between peri-infarct DC shifts
and ischaemic neuronal damage in rat. Neuroreport. 1993;4:70911.
Moskowitz MA, Lo EH, Iadecola C. The science of stroke: mechanisms in
search of treatments. Neuron. 2010;67:18198.
Baron JC, von Kummer R, del Zoppo GJ. Treatment of acute ischemic stroke.
Challenging the concept of a rigid and universal time window. Stroke.
1995;26:221921.
Lo EH. Experimental models, neurovascular mechanisms and translational
issues in stroke research. Br J Pharmacol. 2008;153 Suppl 1:S396405.
Szydlowska K, Tymianski M. Calcium, ischemia and excitotoxicity. Cell
Calcium. 2010;47:1229.
Won SJ, Kim DY, Gwag BJ. Cellular and molecular pathways of ischemic
neuronal death. J Biochem Mol Biol. 2002;35:6786.
Arikkath J. Regulation of dendrite and spine morphogenesis and plasticity
by catenins. Mol Neurobiol. 2009;40:4654.
Allyson J, Dontigny E, Auberson Y, Cyr M, Massicotte G. Blockade of
NR2A-containing NMDA receptors induces Tau phosphorylation in rat
hippocampal slices. Neural Plast. 2010;2010:340168.
Dingledine R, Borges K, Bowie D, Traynelis SF. The glutamate receptor ion
channels. Pharmacol Rev. 1999;51:761.
Constantine-Paton M, Cline HT, Debski E. Patterned activity, synaptic
convergence, and the NMDA receptor in developing visual pathways. Annu
Rev Neurosci. 1990;13:12954.
Choi DW. Calcium: still center-stage in hypoxic-ischemic neuronal death.
Trends Neurosci. 1995;18:5860.
Groc L, Bard L, Choquet D. Surface trafficking of N-methyl-D-aspartate
receptors: physiological and pathological perspectives. Neuroscience.
2009;158:418.
Lau CG, Zukin RS. NMDA receptor trafficking in synaptic plasticity and
neuropsychiatric disorders. Nat Rev Neurosci. 2007;8:41326.
Wenthold RJ, Prybylowski K, Standley S, Sans N, Petralia RS. Trafficking of
NMDA receptors. Annu Rev Pharmacol Toxicol. 2003;43:33558.
Gascon S, Deogracias R, Sobrado M, Roda JM, Renart J, Rodriguez-Pena A,
et al. Transcription of the NR1 subunit of the N-methyl-D-aspartate receptor
is down-regulated by excitotoxic stimulation and cerebral ischemia. J Biol
Chem. 2005;280:3501827.
Monyer H, Sprengel R, Schoepfer R, Herb A, Higuchi M, Lomeli H, et al.
Heteromeric NMDA receptors: molecular and functional distinction of
subtypes. Science. 1992;256:121721.
Liu Y, Wong TP, Aarts M, Rooyakkers A, Liu L, Lai TW, et al. NMDA receptor
subunits have differential roles in mediating excitotoxic neuronal death
both in vitro and in vivo. J Neurosci. 2007;27:284657.
Gutierrez-Vargas JA, Munoz-Manco JI, Garcia-Segura LM, Cardona-Gomez
GP. GluN2B N-methyl-D-aspartic acid receptor subunit mediates
atorvastatin-Induced neuroprotection after focal cerebral ischemia.
J Neurosci Res. 2014;92:152948.
Simpkins KL, Guttmann RP, Dong Y, Chen Z, Sokol S, Neumar RW, et al.
Selective activation induced cleavage of the NR2B subunit by calpain.
J Neurosci. 2003;23:1132231.
Gascon S, Sobrado M, Roda JM, Rodriguez-Pena A, Diaz-Guerra M.
Excitotoxicity and focal cerebral ischemia induce truncation of the NR2A
Page 8 of 9
33.
34.
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
51.
52.
53.
54.
55.
56.
and NR2B subunits of the NMDA receptor and cleavage of the scaffolding
protein PSD-95. Mol Psychiatry. 2008;13:99114.
Guttmann RP, Baker DL, Seifert KM, Cohen AS, Coulter DA, Lynch DR.
Specific proteolysis of the NR2 subunit at multiple sites by calpain.
J Neurochem. 2001;78:108393.
Fukaya M, Kato A, Lovett C, Tonegawa S, Watanabe M. Retention of NMDA
receptor NR2 subunits in the lumen of endoplasmic reticulum in targeted
NR1 knockout mice. Proc Natl Acad Sci U S A. 2003;100:485560.
Zhang S, Edelmann L, Liu J, Crandall JE, Morabito MA. Cdk5 regulates the
phosphorylation of tyrosine 1472 NR2B and the surface expression of
NMDA receptors. J Neurosci. 2008;28:41524.
Dehmelt L, Halpain S. The MAP2/Tau family of microtubule-associated
proteins. Genome Biol. 2005;6:204.
Sheetz MP, Pfister KK, Bulinski JC, Cotman CW. Mechanisms of trafficking in
axons and dendrites: implications for development and neurodegeneration.
Prog Neurobiol. 1998;55:57794.
Johanna GV, Fredy CA, David VC, Natalia MV, Angel CR, Patricia CG. Rac1
activity changes are associated with neuronal pathology and spatial
memory long-term recovery after global cerebral ischemia. Neurochem Int.
2010;57:76273.
Hoskison MM, Yanagawa Y, Obata K, Shuttleworth CW. Calcium-dependent
NMDA-induced dendritic injury and MAP2 loss in acute hippocampal slices.
Neuroscience. 2007;145:6679.
Covington MD, Burghardt RC, Parrish AR. Ischemia-induced cleavage of
cadherins in NRK cells requires MT1-MMP (MMP-14). Am J Physiol Renal
Physiol. 2006;290:F4351.
Ridley AJ, Hall A. Distinct patterns of actin organization regulated by the
small GTP-binding proteins Rac and Rho. Cold Spring Harb Symp Quant
Biol. 1992;57:66171.
Ridley AJ, Hall A. The small GTP-binding protein rho regulates the assembly
of focal adhesions and actin stress fibers in response to growth factors.
Cell. 1992;70:38999.
Santos Da Silva J, Schubert V, Dotti CG. RhoA, Rac1, and cdc42 intracellular
distribution shift during hippocampal neuron development. Mol Cell
Neurosci. 2004;27:17.
Cespedes-Rubio A, Jurado FW, Cardona-Gomez GP. p120 catenin/alphaNcatenin are molecular targets in the neuroprotection and neuronal plasticity
mediated by atorvastatin after focal cerebral ischemia. J Neurosci Res.
2010;88:362134.
Castro-Alvarez JF, Gutierrez-Vargas J, Darnaudery M, Cardona-Gomez GP.
ROCK inhibition prevents tau hyperphosphorylation and p25/CDK5 increase
after global cerebral ischemia. Behav Neurosci. 2011;125:46572.
Tai CY, Mysore SP, Chiu C, Schuman EM. Activity-regulated N-cadherin
endocytosis. Neuron. 2007;54:77185.
Arikkath J, Reichardt LF. Cadherins and catenins at synapses: roles in
synaptogenesis and synaptic plasticity. Trends Neurosci. 2008;31:48794.
Tanaka H, Shan W, Phillips GR, Arndt K, Bozdagi O, Shapiro L, et al.
Molecular modification of N-cadherin in response to synaptic activity.
Neuron. 2000;25:93107.
Posada-Duque RA, Velasquez-Carvajal D, Eckert GP, Cardona-Gomez GP.
Atorvastatin requires geranylgeranyl transferase-I and Rac1 activation to exert
neuronal protection and induce plasticity. Neurochem Int. 2013;62:43345.
Li X, Zhang J, Chai S, Wang X. Progesterone alleviates hypoxic-ischemic
brain injury via the Akt/GSK-3beta signaling pathway. Exp Ther Med.
2014;8:12416.
Mantz J, Degos V, Laigle C. Recent advances in pharmacologic
neuroprotection. Eur J Anaesthesiol. 2010;27:610.
Laws PE, Spark JI, Cowled PA, Fitridge RA. The role of statins in vascular
disease. Eur J Vasc Endovasc Surg. 2004;27:616.
Wang CY, Liu PY, Liao JK. Pleiotropic effects of statin therapy: molecular
mechanisms and clinical results. Trends Mol Med. 2008;14:3744.
Hamilton-Craig I. The Heart Protection Study: implications for clinical
practice. The benefits of statin therapy do not come without financial cost.
Med J Aust. 2002;177:4078.
Bosel J, Gandor F, Harms C, Synowitz M, Harms U, Djoufack PC, et al.
Neuroprotective effects of atorvastatin against glutamate-induced excitotoxicity
in primary cortical neurones. J Neurochem. 2005;92:138698.
Cimino M, Balduini W, Carloni S, Gelosa P, Guerrini U, Tremoli E, et al.
Neuroprotective effect of simvastatin in stroke: a comparison between adult
and neonatal rat models of cerebral ischemia. Neurotoxicology.
2005;26:92933.
Gutirrez-Vargas et al. Journal of Translational Medicine (2015) 13:118
Page 9 of 9
57. Cimino M, Gelosa P, Gianella A, Nobili E, Tremoli E, Sironi L. Statins: multiple
mechanisms of action in the ischemic brain. Neuroscientist. 2007;13:20813.
58. Zhang RL, Zhang ZG, Chopp M. Neurogenesis in the adult ischemic brain:
generation, migration, survival, and restorative therapy. Neuroscientist.
2005;11:40816.
59. Campos-Martorell M, Salvador N, Monge M, Canals F, Garcia-Bonilla L,
Hernandez-Guillamon M, et al. Brain proteomics identifies potential
simvastatin targets in acute phase of stroke in a rat embolic model.
J Neurochem. 2014;130:30112.
60. Greisenegger S, Mullner M, Tentschert S, Lang W, Lalouschek W. Effect of
pretreatment with statins on the severity of acute ischemic cerebrovascular
events. J Neurol Sci. 2004;221:510.
61. Montaner J, Chacon P, Krupinski J, Rubio F, Millan M, Molina CA, et al.
Simvastatin in the acute phase of ischemic stroke: a safety and efficacy pilot
trial. Eur J Neurol. 2008;15:8290.
62. Kawashima S, Yamashita T, Miwa Y, Ozaki M, Namiki M, Hirase T, et al. HMG-CoA
reductase inhibitor has protective effects against stroke events in stroke-prone
spontaneously hypertensive rats. Stroke. 2003;34:15763.
63. Chen J, Zhang C, Jiang H, Li Y, Zhang L, Robin A, et al. Atorvastatin
induction of VEGF and BDNF promotes brain plasticity after stroke in mice.
J Cereb Blood Flow Metab. 2005;25:28190.
64. Tousoulis D, Oikonomou E, Siasos G, Stefanadis C. Statins in heart failureWith
preserved and reduced ejection fraction. An update. Pharmacol Ther.
2014;141:7991.
Submit your next manuscript to BioMed Central
and take full advantage of:
Convenient online submission
Thorough peer review
No space constraints or color gure charges
Immediate publication on acceptance
Inclusion in PubMed, CAS, Scopus and Google Scholar
Research which is freely available for redistribution
Submit your manuscript at
www.biomedcentral.com/submit
Você também pode gostar
- Ischemic StrokeDocumento8 páginasIschemic StrokeRinavi Adrin RirinAinda não há avaliações
- Khoshnam2017 Article PathogenicMechanismsFollowingIDocumento20 páginasKhoshnam2017 Article PathogenicMechanismsFollowingILovin BiancaAinda não há avaliações
- Stroke: BackgroundDocumento10 páginasStroke: Backgroundjhay-r reyesAinda não há avaliações
- Role of CiticolineDocumento20 páginasRole of CiticolinesylviaAinda não há avaliações
- 2010 Hypoxic Ischemic Brain Injury Pathophysiology Neuropathology and Mechanisms KM Busl PDFDocumento9 páginas2010 Hypoxic Ischemic Brain Injury Pathophysiology Neuropathology and Mechanisms KM Busl PDFDaniel OUAinda não há avaliações
- Dapus 2Documento8 páginasDapus 2Beirnes Fernando Sembiring MAinda não há avaliações
- GlibenDocumento12 páginasGlibenAni AnnjumAinda não há avaliações
- Jurnal PDFDocumento9 páginasJurnal PDFFerdy Arif FadhilahAinda não há avaliações
- A StrokeDocumento6 páginasA StrokeCrizzy GuiaoAinda não há avaliações
- 10 Terapie S-NODocumento10 páginas10 Terapie S-NOdodutaAinda não há avaliações
- A Review On Cerebral Ischemic Stroke Mandeep Pundir, Manjinder Kour, Darshdeep SinghDocumento11 páginasA Review On Cerebral Ischemic Stroke Mandeep Pundir, Manjinder Kour, Darshdeep SinghParamjeet Kaur Paramedical SciencesAinda não há avaliações
- Se FisiopatoDocumento28 páginasSe Fisiopatocska398Ainda não há avaliações
- Cell Death Pathways in Ischemic Stroke and Targeted PharmacotherapyDocumento18 páginasCell Death Pathways in Ischemic Stroke and Targeted PharmacotherapyHeath HensleyAinda não há avaliações
- ZORA Rudiger 2Documento25 páginasZORA Rudiger 2Carlos TrellesAinda não há avaliações
- Microcirculation: From Bench to BedsideNo EverandMicrocirculation: From Bench to BedsideMaria DorobantuAinda não há avaliações
- Aps 201810Documento12 páginasAps 201810Pentol100% (1)
- Patofisiologi StrkeDocumento14 páginasPatofisiologi StrkeTeuku ILza Nanta SatiaAinda não há avaliações
- Geriatric PharmacologyDocumento13 páginasGeriatric PharmacologyJEFFERSON MUÑOZAinda não há avaliações
- Lau 2010Documento18 páginasLau 2010Oris WicaksonoAinda não há avaliações
- Dhami Et Al-2019-Journal of Neurochemistry PDFDocumento18 páginasDhami Et Al-2019-Journal of Neurochemistry PDFJawad A. KhanAinda não há avaliações
- 10.2478 - JCCM 2021 0029Documento3 páginas10.2478 - JCCM 2021 0029Elizabeth CastilloAinda não há avaliações
- Pathophysiology of StrokeDocumento11 páginasPathophysiology of StrokeAgronaSlaughterAinda não há avaliações
- Physiology, Neuromuscular Junction of Skeletal MuscleDocumento8 páginasPhysiology, Neuromuscular Junction of Skeletal Musclemethmal subasingheAinda não há avaliações
- Subarachnoid Hemorrhage and Cerebral Vasospasm - Literature ReviewDocumento6 páginasSubarachnoid Hemorrhage and Cerebral Vasospasm - Literature ReviewzixzaxoffAinda não há avaliações
- Molecular Pathophysiology of StrokeDocumento10 páginasMolecular Pathophysiology of StrokeKahubbi Fatimah Wa'aliyAinda não há avaliações
- 97 312 PDFDocumento5 páginas97 312 PDFdupuytrenAinda não há avaliações
- 2019 - Brain Functional Reserve in The Context of Neuroplasticity After StrokeDocumento10 páginas2019 - Brain Functional Reserve in The Context of Neuroplasticity After StrokeEl Tal RuleiroAinda não há avaliações
- Pathophysiology of Stroke 2Documento12 páginasPathophysiology of Stroke 2AgronaSlaughterAinda não há avaliações
- 04 Wang 2015Documento8 páginas04 Wang 2015Andrei BicanAinda não há avaliações
- Neuroinflammatory Mechanisms in Ischemic Stroke: Focus On Cardioembolic Stroke, Background, and Therapeutic ApproachesDocumento33 páginasNeuroinflammatory Mechanisms in Ischemic Stroke: Focus On Cardioembolic Stroke, Background, and Therapeutic ApproachesSonia P SAinda não há avaliações
- Meningitis EskemikDocumento17 páginasMeningitis Eskemikakbar011512Ainda não há avaliações
- WIKI Cardio Vascular AccidentDocumento2 páginasWIKI Cardio Vascular AccidentAldrin CerdaAinda não há avaliações
- Qin, Et Al. 2022Documento29 páginasQin, Et Al. 2022Ignacio BarbieriAinda não há avaliações
- Ijms 13 11753 PDFDocumento20 páginasIjms 13 11753 PDFVandy IkraAinda não há avaliações
- JMedLife 08 266Documento6 páginasJMedLife 08 266Gabriel GonzálezAinda não há avaliações
- 052 Westermeier Journal Neurology NeurophysiologyDocumento8 páginas052 Westermeier Journal Neurology NeurophysiologyRizka Leonita FahmyAinda não há avaliações
- CNS 8 353Documento8 páginasCNS 8 353Adinda MelaniAinda não há avaliações
- Neuroprotection-WPS OfficeDocumento4 páginasNeuroprotection-WPS OfficeabdoAinda não há avaliações
- Pathophysiology, Bioelectricidad, Review Stroke TINS99Documento7 páginasPathophysiology, Bioelectricidad, Review Stroke TINS99Carla Saramy MachillandaAinda não há avaliações
- Acute Stroke ArticleDocumento10 páginasAcute Stroke ArticlenesredeAinda não há avaliações
- Zarco Ordóñez KarlaDocumento2 páginasZarco Ordóñez KarlaKarla ZarcoAinda não há avaliações
- Pathophysiology Ischemic Stroke - VinaDocumento2 páginasPathophysiology Ischemic Stroke - VinaDevi Astri KusumawardaniAinda não há avaliações
- Secondary Brain Injury: Prevention and Intensive Care ManagementDocumento6 páginasSecondary Brain Injury: Prevention and Intensive Care ManagementFirah Triple'sAinda não há avaliações
- Dysfunctional Mitochondrial Dynamics in The Pathophysiology of Neurodegenerative DiseasesDocumento9 páginasDysfunctional Mitochondrial Dynamics in The Pathophysiology of Neurodegenerative DiseasesNuacha ZterezabiestAinda não há avaliações
- Novel Mechanisms of Action of Three Antiepileptic Drugs, Vigabatrin, Tiagabine, and TopiramateDocumento8 páginasNovel Mechanisms of Action of Three Antiepileptic Drugs, Vigabatrin, Tiagabine, and Topiramatedpf050Ainda não há avaliações
- 10 3390@ijms20102450Documento39 páginas10 3390@ijms20102450Lina DarkAinda não há avaliações
- Beta-Block The Septic Heart 2010Documento5 páginasBeta-Block The Septic Heart 2010Ivann FloresAinda não há avaliações
- Multiparametric IschemiaDocumento9 páginasMultiparametric IschemiaDemian PereiraAinda não há avaliações
- Clinic Trăilă of StemDocumento22 páginasClinic Trăilă of StemRadu AvramAinda não há avaliações
- Thrombolytic Therapy For StrokeDocumento13 páginasThrombolytic Therapy For Strokereza ahda kadirAinda não há avaliações
- Methylene Blue For Septic Shock - Pharmacotherapy 2010Documento16 páginasMethylene Blue For Septic Shock - Pharmacotherapy 2010Anonymous 4txA8N8etAinda não há avaliações
- Fisiopatología de La Isquemia Cerebral FocalDocumento10 páginasFisiopatología de La Isquemia Cerebral FocalshilacorinaAinda não há avaliações
- Sudden Death: Neurogenic Causes, Prediction and PreventionDocumento11 páginasSudden Death: Neurogenic Causes, Prediction and PreventionFaiq MurtezaAinda não há avaliações
- Brain Injury Following Cardiac Arrest: Pathophysiology For Neurocritical CareDocumento10 páginasBrain Injury Following Cardiac Arrest: Pathophysiology For Neurocritical CareDianis DiAinda não há avaliações
- Diabetes Mellitus and Bloodbrain Barrier Dysfunction An Overview 2329 6887 2 125Documento11 páginasDiabetes Mellitus and Bloodbrain Barrier Dysfunction An Overview 2329 6887 2 125Saifuddin HaswareAinda não há avaliações
- Pa Tho Physiology of Focal Cerebral Ischemia A Therapeutic PerspectiveDocumento10 páginasPa Tho Physiology of Focal Cerebral Ischemia A Therapeutic PerspectiveMalisa LukmanAinda não há avaliações
- TB4-Frag A Collection of StudiesDocumento20 páginasTB4-Frag A Collection of StudiesscribdAinda não há avaliações
- TMP FFC1Documento28 páginasTMP FFC1FrontiersAinda não há avaliações
- Antiarrhythmic DrugsNo EverandAntiarrhythmic DrugsAntoni Martínez-RubioAinda não há avaliações
- 12.4.09 Laudate Spinal LesionsDocumento31 páginas12.4.09 Laudate Spinal LesionsDrGasnasAinda não há avaliações
- Peripheral NeuropathyDocumento48 páginasPeripheral NeuropathyDrGasnasAinda não há avaliações
- ch15 APR LectureDocumento60 páginasch15 APR LectureDrGasnasAinda não há avaliações
- Lec. 2 - Autonomic Nervous SystemDocumento26 páginasLec. 2 - Autonomic Nervous SystemDrGasnasAinda não há avaliações
- 9 AnsDocumento25 páginas9 AnsDrGasnasAinda não há avaliações
- Autonomic Nervous SystemDocumento48 páginasAutonomic Nervous SystemDrGasnasAinda não há avaliações
- Differentiating Upper From Lower Motor Neuron LesionsDocumento4 páginasDifferentiating Upper From Lower Motor Neuron LesionsDrGasnasAinda não há avaliações
- NIH Public Access: Author ManuscriptDocumento18 páginasNIH Public Access: Author ManuscriptDrGasnasAinda não há avaliações
- Nervous SystemDocumento123 páginasNervous SystemDrGasnasAinda não há avaliações
- Chapter 16 LizDocumento58 páginasChapter 16 LizDrGasnasAinda não há avaliações
- What Imaging Teaches Us - КопияDocumento62 páginasWhat Imaging Teaches Us - КопияDrGasnas100% (1)
- Alpha-Lipoic Acid Treatment Is Neurorestorative and Promotes Functional Recovery After Stroke in RatsDocumento16 páginasAlpha-Lipoic Acid Treatment Is Neurorestorative and Promotes Functional Recovery After Stroke in RatsDrGasnasAinda não há avaliações
- Encephalitiscia3 151011085926 Lva1 App6892Documento43 páginasEncephalitiscia3 151011085926 Lva1 App6892DrGasnasAinda não há avaliações
- 4762376Documento54 páginas4762376DrGasnasAinda não há avaliações
- Role of GABA Plasticity in StrokeDocumento3 páginasRole of GABA Plasticity in StrokeDrGasnasAinda não há avaliações
- Music Listening Enhances Cognitive Recovery and Mood After Middle Cerebral Artery StrokeDocumento11 páginasMusic Listening Enhances Cognitive Recovery and Mood After Middle Cerebral Artery StrokeLAURIEJERIEAinda não há avaliações
- In Ammatory Mechanisms in Ischemic Stroke PDFDocumento11 páginasIn Ammatory Mechanisms in Ischemic Stroke PDFGustavo CabanasAinda não há avaliações
- Call For Papers: Maladaptive Plasticity and Neuropathic PainDocumento1 páginaCall For Papers: Maladaptive Plasticity and Neuropathic PainDrGasnasAinda não há avaliações
- Call For Papers: Plasticity of The Gabaergic System in Physiology and DiseaseDocumento1 páginaCall For Papers: Plasticity of The Gabaergic System in Physiology and DiseaseDrGasnasAinda não há avaliações
- UnconsciousnessDocumento91 páginasUnconsciousnessDrGasnasAinda não há avaliações
- WLK Chapter 006 NeurologicAssessDocumento57 páginasWLK Chapter 006 NeurologicAssessDrGasnasAinda não há avaliações
- Call For Papers: Neural Degeneration and Plasticity in Communication Disorders: Mechanism, Evaluation, and TreatmentDocumento1 páginaCall For Papers: Neural Degeneration and Plasticity in Communication Disorders: Mechanism, Evaluation, and TreatmentDrGasnasAinda não há avaliações
- Fernandez-Torre ClinNeuroph12-Nonconvulsive SE Adults Electroclin DifferencesDocumento8 páginasFernandez-Torre ClinNeuroph12-Nonconvulsive SE Adults Electroclin DifferencesDrGasnasAinda não há avaliações
- Nervous System Powerpoint2007 - 1Documento98 páginasNervous System Powerpoint2007 - 1DrGasnasAinda não há avaliações
- Nervous SystemDocumento58 páginasNervous SystemDrGasnasAinda não há avaliações
- Nervous SystemDocumento123 páginasNervous SystemDrGasnasAinda não há avaliações
- ReflexesDocumento35 páginasReflexesBaleli Zagala100% (1)
- Central Nervous SystemDocumento25 páginasCentral Nervous SystemDrGasnasAinda não há avaliações
- CNS PNSDocumento163 páginasCNS PNSDrGasnasAinda não há avaliações
- English Lesson PlanDocumento3 páginasEnglish Lesson PlanJeremias MartirezAinda não há avaliações
- Ministry of Truth Big Brother Watch 290123Documento106 páginasMinistry of Truth Big Brother Watch 290123Valentin ChirilaAinda não há avaliações
- Impact of Micro FinanceDocumento61 páginasImpact of Micro FinancePerry Arcilla SerapioAinda não há avaliações
- Unsung Ancient African Indigenous Heroines and HerosDocumento27 páginasUnsung Ancient African Indigenous Heroines and Herosmsipaa30Ainda não há avaliações
- Radiography Safety ProcedureDocumento9 páginasRadiography Safety ProcedureأحمدآلزهوAinda não há avaliações
- Debus Medical RenaissanceDocumento3 páginasDebus Medical RenaissanceMarijaAinda não há avaliações
- In Partial Fulfillment of The Requirements in Care of Older Adult (NCM 114)Documento2 páginasIn Partial Fulfillment of The Requirements in Care of Older Adult (NCM 114)Karen TangAinda não há avaliações
- PsychFirstAidSchools PDFDocumento186 páginasPsychFirstAidSchools PDFAna ChicasAinda não há avaliações
- Character Formation 1: Nationalism and PatriotismDocumento11 páginasCharacter Formation 1: Nationalism and Patriotismban diaz100% (1)
- 1sebastian Vs CalisDocumento6 páginas1sebastian Vs CalisRai-chan Junior ÜAinda não há avaliações
- The Role of Financial System in DevelopmentDocumento5 páginasThe Role of Financial System in DevelopmentCritical ThinkerAinda não há avaliações
- Measure For Measure AngeloDocumento1 páginaMeasure For Measure AngeloRoger Knight100% (1)
- J of Cosmetic Dermatology - 2019 - Zhang - A Cream of Herbal Mixture To Improve MelasmaDocumento8 páginasJ of Cosmetic Dermatology - 2019 - Zhang - A Cream of Herbal Mixture To Improve Melasmaemily emiAinda não há avaliações
- Million-Day Gregorian-Julian Calendar - NotesDocumento10 páginasMillion-Day Gregorian-Julian Calendar - Notesraywood100% (1)
- Attery: User Guide Dict Release 2020Documento47 páginasAttery: User Guide Dict Release 2020diegoAinda não há avaliações
- Paradigm Shift in Teaching: The Plight of Teachers, Coping Mechanisms and Productivity in The New Normal As Basis For Psychosocial SupportDocumento5 páginasParadigm Shift in Teaching: The Plight of Teachers, Coping Mechanisms and Productivity in The New Normal As Basis For Psychosocial SupportPsychology and Education: A Multidisciplinary JournalAinda não há avaliações
- Angel Number 1208 Meaning Increased FaithDocumento1 páginaAngel Number 1208 Meaning Increased FaithKhally KatieAinda não há avaliações
- Public Administration 2000 - CSS ForumsDocumento3 páginasPublic Administration 2000 - CSS ForumsMansoor Ali KhanAinda não há avaliações
- Eugène Burnouf: Legends of Indian Buddhism (1911)Documento136 páginasEugène Burnouf: Legends of Indian Buddhism (1911)Levente Bakos100% (1)
- 7 - LESSON PLAN CULTURAL HERITAGE AND CULTURAL DIVERSITY - Lesson PlanDocumento4 páginas7 - LESSON PLAN CULTURAL HERITAGE AND CULTURAL DIVERSITY - Lesson PlanRute SobralAinda não há avaliações
- Brochure 8 VT 8Documento24 páginasBrochure 8 VT 8David GonzalesAinda não há avaliações
- Plastique: Art and EducationDocumento7 páginasPlastique: Art and EducationJackStevensonAinda não há avaliações
- The Machine StopsDocumento14 páginasThe Machine StopsMICHAEL HARRIS USITAAinda não há avaliações
- Openfire XXMPP Server On Windows Server 2012 R2Documento9 páginasOpenfire XXMPP Server On Windows Server 2012 R2crobertoAinda não há avaliações
- Forecast Error (Control Chart)Documento2 páginasForecast Error (Control Chart)Jane OngAinda não há avaliações
- Arsu and AzizoDocumento123 páginasArsu and AzizoZebu BlackAinda não há avaliações
- Activity Chapter1 ManagementDocumento7 páginasActivity Chapter1 ManagementTricia Amigo SacareAinda não há avaliações
- Asset Integrity ManagementDocumento5 páginasAsset Integrity ManagementLuis100% (2)
- FreeMarkets: Procurement & Outsourcing StrategiesDocumento44 páginasFreeMarkets: Procurement & Outsourcing StrategiesFarhaad MohsinAinda não há avaliações
- PED100 Mod2Documento3 páginasPED100 Mod2Risa BarritaAinda não há avaliações