Escolar Documentos
Profissional Documentos
Cultura Documentos
1387 Comparison of Ondansetron and Combination of Ondansetron and Dexamethasone For Prevention of Postop Nausea and Vomiting in Patients Undergoing Elective Lap Chole
Enviado por
Fajar NarakusumaTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
1387 Comparison of Ondansetron and Combination of Ondansetron and Dexamethasone For Prevention of Postop Nausea and Vomiting in Patients Undergoing Elective Lap Chole
Enviado por
Fajar NarakusumaDireitos autorais:
Formatos disponíveis
ORIGINAL ARTICLE
Comparison of Ondansetron and Combination of Ondansetron
and Dexamethasone for Prevention of Post-Operative Nausea
and Vomiting in Patients Undergoing Elective Laparoscopic
Cholecystectomy
1
IRAM ALIA , MOHSIN GILLANI , ATIF HANIF , UMAR FAROOQ DAR , AMINA MIRZA
ABSTRACT
Aim: To compare the frequency of post-operative nausea and vomiting within 24 hours of operation in
patients undergoing lap. cholecystectomy administered ondansetron with and without dexamethasone.
st
th
Methods: This randomized control trial was carried out from 1 February 2015 to 30 September
2015. One hundred and sixty four patients of either sex and age ranging from 20 to 60 years
undergoing laparoscopic cholecystectomy were included. Both ASA grade I and II patients were
randomly distributed in two groups. Group A received ondansetron and dexamethasone while in group
B only ondansetron was administered I/V. Frequency of postop nausea & vomiting was compared.
Results: Twenty two patients (13.4%) were in ASA Grade I while 142 patients (86.6%) were in Grade
II. 43 patients (71.7%) were female while 17 (28.3%) were males. There were PONV 61 patients
(37.2%). Twenty eight (45.9%) patients out of eighty two from Ondansetron group and 33/82 patients
(54.1%) from Ondansetron plus dexamethasone group developed nausea or vomiting post operatively
(p value=0.41). Ondansetron & Dexamethasone group was more effective as shown by our results in
male and younger patients in terms of nausea or vomiting post operatively.
Conclusion: It is concluded that at current sample size, there is no difference in frequency of postoperative nausea and vomiting in patients undergoing laparoscopic cholecystectomy with combination
of dexamethasone and ondansetron as compared to ondansetron alone for whole cohort.
Keywords: Post-operative nausea & vomiting, Dexamethasone, Ondansetron
INTRODUCTION
Post-operative nausea and vomiting (PONV) are the
most common unpleasant experiences following
1
laparoscopic surgeries. It remains a significant
clinical issue that can detract from patients quality of
life in hospital/treatment facility, as well as in the days
2-5
immediately post-discharge.
In addition, PONV
may increase perioperative costs, increase
perioperative morbidity, increase post-anesthesia
care unit stay, prolong hospital stays, length of
stay/delay discharge, delay the time that the patient
6,7
can go back to work, and lead to readmissions.
Despite the existence of multiple tools to stratify
patients according to their risk of developing PONV
and multiple PONV treatment guidelines, clinicians
do not appear to systematically address the
treatment and/or prophylaxis of PONV in a uniform
fashion with both pharmacologic and non
----------------------------------------------------------------------
pharmacologic strategies in attempts to minimize
8-10
PONV occurrences.
Several factors have been
implicated
specifically
in
laparoscopic
cholecystectomy like carbon dioxide insufflation,
distension of the abdomen and irritation of the
11-14
diaphragm and other abdominal viscera.
Different medications have been evaluated in
PONV prophylaxis and patient satisfaction after
5
cholecystectomy .
Ondansetron,
a
5hydroxytryptamine (5-HT3) receptor antagonist, and
dexamethasone have been found to reduce PONV
significantly after laparoscopic cholecystectomy
6,14,15
compared with placebo
. A study conducted by
5
Bhattari and colleagues showed that no nausea or
emesis and no need for rescue antiemetic during first
24 h, was noted in 76% of patients who received
ondansetron alone, while similar response was seen
in 92% of patients in combination group.
Associate Professor of Anesthesiology.
Associate Professor of Surgery, Sharif Medical and Dental
College Lahore,
3
Associate Professor of Anesthesiology, Akhtar Saeed Medical &
Dental College Lahore,
4
Assistant Professor of Community Medicine, Gujranwala Medical
College, Gujranwala
Correspondence
to
Dr.
Umar
Farooq
Dar
e-mail:
umardar84@gmail.com
2
1387 P J M H S Vol. 9, NO. 4, OCT DEC 2015
SUBJECTS AND METHODS
This randomized control trial was carried out in
Departments of Anaesthesia of Akhtar Saeed
Medical & Dental College and Sharif Medical and
st
th
Dental College from 1 February 2015 to 30
September 2015. One hundred and sixty four
Iram Alia, Mohsin Gillani, Atif Hanif et al
patients of either sex and age ranging from 20 to 60
years undergoing laparoscopic cholecystectomy were
included. Using lottery method, patients were
randomized either in control or in study group.
Written informed consent was taken for participation
in the research project. The baseline characteristics
of patients were recorded on the study proforma. The
patients in group A received intravenous ondansetron
4 mg and dexamethasone 4 mg whereas Group B
patients received 4 mg of ondansetron only 30
minutes prior to the induction of anesthesia, and any
side effect during injection was recorded. The
anesthetic sequence was standardized. The patients
received a single dose of injection ceftriaxone 1gm at
the time of induction of anesthesia. All patients
received injection Diclofenac 75mg I/M thrice on the
first postoperative day and then as required. After
surgery, patients were observed for any episode of
nausea or vomiting, or whether the patient required
any anti-emetic drug in the postoperative period.
Patients were evaluated for nausea and vomiting in
the first 24 hours after intervention. The episodes of
nausea and vomiting were noted on the proforma
specifically designed for the study by the resident
surgeon.
RESULTS
There were 17 males (28.3%) and 143 female
(71.7%) patients with mean age 42.6811.56 years.
Only 22 patients (13.4%) were ASA Grade I while
rest 142 patients (86.6%) were in ASA Grade II
(Table 1). When compared the postoperative nausea
and vomiting in either group with ketamine and
ondanestron, the resultant distribution was same i.e.
non-significant (p value=0.419) (Table 2). Differences
in results were statistically not significant for
prevention of shivering (0.26) and age (0.827) with
ASA grades (Tables 3-4), To evaluate the effect of
age distribution on outcome in either group,
nausea/vomiting with groups for age showed
difference in results was statistically significant
(p=0.01) (Table 5).
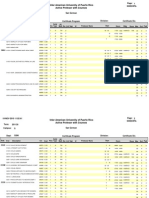
Table 1: Demographic information of the patients
Variable
No.
%
Age (years)
<40
67
40.9
>40
97
59.1
Gender
Male
17
28.3
Female
143
71.7
ASA Grade
I
22
13.4
II
142
86.6
Table 2: Comparison of efficacy (prevention of shivering) in
both groups
Prevention
Ketamine
Ondansetron
of shivering
No.
%
No.
%
Yes
6
7.3
8
9.7
No
76
92.7
74
90.3
Using Pearson Chi-Square, p value = 0.419 (Not significant)
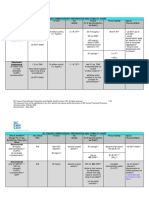
Table 3: Comparison of prevention of shivering according
ASA grades
Prevention
ASA Grade I
ASA Grade II
of shivering
No.
%
No.
%
Yes
72
87.8
73
89.0
No
10
12.2
9
11.0
Using Pearson Chi-Square, p value = 0.26 (Not significant)
Table 4: Comparison of age according to ASA grades
Age
ASA Grade I
ASA Grade II
(years)
No.
%
No.
%
<25
51
62.2
45
54.8
25 30
11
13.4
12
14.7
>30
20
24.4
25
30.5
Using Pearson Chi-Square, p value = 0.827 (Not significant)
Table 5: Comparison of age according to efficacy
Age
Prevention of shivering
(years)
Yes
No
No.
%
No.
%
<25
89
54.2
13
7.8
25 30
25
15.2
4
2.4
>30
27
16.3
10
6.1
Using Pearson Chi-Square p value= 0.01(Significant)
DISCUSSION
Post-operative nausea and vomiting is one of the
leading causes of discomfort for patients recovering
from general anesthesia. PONV can lead to
sweating, tachycardia, abdominal pain, prolonged
3
recovery duration and increased risk of aspiration. It
can be very distressing to the patient, sometimes
more than the surgery itself, and it can result in
several complications like dehydration, gastric
aspiration and wound disruption. Ondansetron, a 5hydroxytryptamine (5-HT3) receptor antagonist, and
dexamethasone have been found to reduce PONV
significantly after laparoscopic cholecystectomy
compared with placebo.
In our study, 28/82 patients (45.9%) from
Ondansetron group and 33/82 patients (54.1%) from
Ondansetron plus dexamethasone group developed
nausea or vomiting post operatively. When chi
square test was applied, difference was nonsignificant (p value= 0.419). A study conducted by
5
Bhattari and colleagues showed that no nausea or
emesis and no need for rescue antiemetic during first
24 h, was noted in 76% of patients who received
ondansetron alone, while similar response was seen
P J M H S Vol. 9, NO. 4, OCT DEC 2015 1388
Comparison of Ondansetron and Combination of Ondansetron and Dexamethasone
in 92% of patients in combination group. Our results
5
differed from Bhattari et al .
6.
CONCLUSION
It is concluded that there is no difference in frequency
of post-operative nausea and vomiting in patients
undergoing laparoscopic cholecystectomy with
combination of dexamethasone and ondansetron as
compared to ondansetron alone for whole cohort.
Ondansetron & Dexamethasone group was more
effective as shown by our results in male and
younger patients in terms of nausea or vomiting post
operatively.
7.
8.
9.
REFERENCES
1.
2.
3.
4.
5.
Eidy M, Vafaei HR, Rajabi M, Mohammadzadeh M,
Pazouki A. Effect of Ondansetron and Dexamethasone
on Post-Operative Nausea and Vomiting in Patients
Undergoing Laproscopic Cholecystectomy. J Minim
Invasive Surg Sci. 2013;2(2):138-43.
Smith HS, Smith EJ, Smith BR. Postoperative nausea
and vomiting. Ann Palliat Med.2012July;1(2):94-102.
Hessami MA,
Yari
M.
GranisetronVersus
Dexamethasone in Prophylaxis of Nausea and
Vomiting After Laparoscopic Cholecystectomy. Anesth
Pain Med.2012;2(2):81-84.
Ahmed N, Muslim M, Aurangzeb M, Zarin M.
Prevention of Postoperative Nausea and Vomiting in
Laproscopic Cholecystectomy. J.Med.Sci. January
2012; 20(1): 33-36.
Bhattarai B, Shrestha S, Singh J. Comparison of
ondansetron and combination of ondansetron and
dexamethasone as a prophylaxis for postoperative
nausea and vomiting in adults undergoing elective
laproscopic surgery.J Emerg Trauma Shock 2011;
4(2):168172.
1389 P J M H S Vol. 9, NO. 4, OCT DEC 2015
10.
11.
12.
13.
14.
15.
Alghanem SM, Massad IM, Rashed EM, Abu-Ali HM,
Daradkeh SS. Optimization of anesthesia antiemetic
measures versus combination therapy using
dexamethasone or ondansetron for the prevention of
postoperative
nausea
and
vomiting.
Surg
Endosc.2010; 24(2):353-358.
Khanna A, Sezen E, Barlow A, Rayt H, Finch JG.
Randomized clinical trial of a simple pulmonary
recruitment manoeuvre to reduce pain after
laparoscopy British J Surg 2013; 100: 1290-4.
Kyakong O, Tamdee D, Charuluxananan S.
Comparison of the effeicacy of nalbuphine, tramadol,
ondansetron and placebo in the treatment of
postanesthetic shivering after spinal anesthesia for
cesarean delivery.Asian Biomedicine.2007;2(1):189
194.
Kelsaka E, Baris S, Karakaya D, Sarihasan B.
Comparison of ondansetron and mepridine for
prevention of shivering in patients undergoing spinal
anesthesia. RegAnaesth Pain Med.2006;31(1):40 5.
Betrn AP, Merialdi M, Lauer JA. Rates of caesarean
section: analysis of global, regional and national
estimates. Paediatr Perinat Epidemiol 2007; 21:98.
Betrn AP, Gulmezoglu AM, Robson M. WHO global
survey on maternal and perinatal health in Latin
America: classifying caesarean sections. Reprod
Health 2009; 6:18-25.
Gibbons L, Belizan JM, Lauer JA. Inequities in the use
of cesarean section deliveries in the world. Am J
ObstetGynecol 2012; 206:331.e1.
Tang S, Li X, Wu Z. Rising cesarean delivery rate in
primiparous women in urban China: evidence from
three nationwide household health surveys. Am J
ObstetGynecol 2006; 195:1527-33.
Zhang J, Liu Y, Meikle S. Cesarean delivery on
maternal request in southeast China. ObstetGynecol
2008; 111:1077-83.
Penn Z, Ghaem-Maghami S. Indications for caesarean
section. Best Pract Res ClinObstetGynaecol 2001;
15:1-9.
Você também pode gostar
- Medicolegal Tips For DoctorsDocumento10 páginasMedicolegal Tips For DoctorsFajar NarakusumaAinda não há avaliações
- FrgethteheDocumento4 páginasFrgethteheFajar NarakusumaAinda não há avaliações
- Premedication With Oral Tramadol Reduces Severity of Postoperative Shivering After General AnesthesiaDocumento6 páginasPremedication With Oral Tramadol Reduces Severity of Postoperative Shivering After General AnesthesiaFajar NarakusumaAinda não há avaliações
- GGHHGVHHDocumento8 páginasGGHHGVHHFajar NarakusumaAinda não há avaliações
- Daftar Pustaka: Essential Otolaryngology Head and Neck Surgery. 8Documento3 páginasDaftar Pustaka: Essential Otolaryngology Head and Neck Surgery. 8Fajar NarakusumaAinda não há avaliações
- Typhoid FeverDocumento13 páginasTyphoid FeverFajar NarakusumaAinda não há avaliações
- 1 SD 3 18 40.91% 19 43.18% 7 15.91% 44 100.00% 4sd6 5 15.15% 18 54.55% 10 30.30% 33 100.00% 23 29.87% 37 48.05% 17 22.08% 77 100.00%Documento1 página1 SD 3 18 40.91% 19 43.18% 7 15.91% 44 100.00% 4sd6 5 15.15% 18 54.55% 10 30.30% 33 100.00% 23 29.87% 37 48.05% 17 22.08% 77 100.00%Fajar NarakusumaAinda não há avaliações
- Jam Foto Foto Foto Datang PX Les RX Diagnosis Identitas NoDocumento2 páginasJam Foto Foto Foto Datang PX Les RX Diagnosis Identitas NoFajar NarakusumaAinda não há avaliações
- Jadwal Stase RadiologiDocumento1 páginaJadwal Stase RadiologiFajar NarakusumaAinda não há avaliações
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5795)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Tubes, Lines, and Drains Basics: Harmacy Ompetency Ssessment EnterDocumento11 páginasTubes, Lines, and Drains Basics: Harmacy Ompetency Ssessment EnterJeremy HamptonAinda não há avaliações
- Fast Hugs MaidenDocumento8 páginasFast Hugs MaidenPriscila Navarro MedinaAinda não há avaliações
- Prefix, Suffix of DrugsDocumento6 páginasPrefix, Suffix of DrugsBriel Jake CabusasAinda não há avaliações
- Programa de Clases 2011-30 (10 Nov)Documento100 páginasPrograma de Clases 2011-30 (10 Nov)Juan C Belen OrtizAinda não há avaliações
- Improvement of Opioid Addiction Medication Through Extended-Release Naltrexone: A Comparative, Experimental and Laboratory ApproachDocumento3 páginasImprovement of Opioid Addiction Medication Through Extended-Release Naltrexone: A Comparative, Experimental and Laboratory ApproachMediterr J Pharm Pharm SciAinda não há avaliações
- PT - Permata Delta Agung: Halaman: (All)Documento35 páginasPT - Permata Delta Agung: Halaman: (All)abdul husainAinda não há avaliações
- May 2021 .Documento22 páginasMay 2021 .Innocent DimpleAinda não há avaliações
- Post Test - Pharma (Students Copy)Documento5 páginasPost Test - Pharma (Students Copy)irish felix100% (1)
- Pharmacokinetics Review CEE With Practice ProblemsDocumento148 páginasPharmacokinetics Review CEE With Practice ProblemsBenhur Leithold LapitanAinda não há avaliações
- Understanding The Concept of Equivalence and Non-Inferiority Trials Understanding The Concept of Equivalence and Non-Inferiority TrialsDocumento13 páginasUnderstanding The Concept of Equivalence and Non-Inferiority Trials Understanding The Concept of Equivalence and Non-Inferiority TrialsrbaezaAinda não há avaliações
- Chemo Stability Chart - AtoKDocumento59 páginasChemo Stability Chart - AtoKAfifah Nur Diana PutriAinda não há avaliações
- 11.drug StudyDocumento1 página11.drug StudyFreisanChenMandumotanAinda não há avaliações
- Tutorial 4 - Pain ManagementDocumento5 páginasTutorial 4 - Pain ManagementSAinda não há avaliações
- Sedative-Hypnotic Drugs: Michael H. Nelson, PH.D., R.PHDocumento10 páginasSedative-Hypnotic Drugs: Michael H. Nelson, PH.D., R.PHHan HopperAinda não há avaliações
- Herrero Vanrell2014Documento17 páginasHerrero Vanrell2014Fer RodriguezAinda não há avaliações
- Catalogo Petmedical Nov22Documento14 páginasCatalogo Petmedical Nov22Emile CardAinda não há avaliações
- Magstim RTMS Therapy BrochureDocumento4 páginasMagstim RTMS Therapy BrochureMuraliAinda não há avaliações
- Opioid Abusers Prefer Hydrocodone or Oxycodone For Different ReasonsDocumento1 páginaOpioid Abusers Prefer Hydrocodone or Oxycodone For Different Reasonsobx4everAinda não há avaliações
- British J Pharmacology - 2022 - White - Identifying The Core Concepts of Pharmacology Education A Global InitiativeDocumento13 páginasBritish J Pharmacology - 2022 - White - Identifying The Core Concepts of Pharmacology Education A Global InitiativeMario CorreaAinda não há avaliações
- AR 3 Airway Drug Assisted Intubation Protocol Final 2017 EditableDocumento2 páginasAR 3 Airway Drug Assisted Intubation Protocol Final 2017 EditableAlejandroCabreraBustillo100% (1)
- Intravenous TherapyDocumento3 páginasIntravenous TherapyArmandoAinda não há avaliações
- Special Articles: Awake Intubation Intubation After Induction of General AnesthesiaDocumento1 páginaSpecial Articles: Awake Intubation Intubation After Induction of General AnesthesiaOKE channelAinda não há avaliações
- 7-3-49 - Minimal Occluding Volume (MOV)Documento4 páginas7-3-49 - Minimal Occluding Volume (MOV)kitsilcAinda não há avaliações
- Acute Migraine Treatment.6Documento16 páginasAcute Migraine Treatment.6BryanAinda não há avaliações
- Halcion Triazolam Tablets, USP CIV: DescriptionDocumento14 páginasHalcion Triazolam Tablets, USP CIV: DescriptionAlberto JaramilloAinda não há avaliações
- NREMT Practice Test Bank - 4q Multiple Choice-36Documento1 páginaNREMT Practice Test Bank - 4q Multiple Choice-36Dickson Kuria MburiAinda não há avaliações
- Business Development LeadsDocumento5 páginasBusiness Development LeadsRohit GaikwadAinda não há avaliações
- Center For Drug Evaluation and Research - Afinitor-EverolomusDocumento345 páginasCenter For Drug Evaluation and Research - Afinitor-EverolomusHatem HadiaAinda não há avaliações
- General AnesthesiaDocumento6 páginasGeneral AnesthesiaTaqi MehdiAinda não há avaliações
- Dr. Sady Ribeiro and His ServicesDocumento10 páginasDr. Sady Ribeiro and His ServicesSADY RIBEIRO,M.DAinda não há avaliações