Escolar Documentos
Profissional Documentos
Cultura Documentos
Sanp 00174
Enviado por
rafikaTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Sanp 00174
Enviado por
rafikaDireitos autorais:
Formatos disponíveis
Review article
Dravet syndrome: an update
Vanessa S. van Dam, Christian M. Korff
Neuropdiatrie, Hpital des Enfants, Genve, Switzerland
Funding / potential competing interests: Christian Korff was supported by SNF (SPUM) n140332. No potential conflict of interest relevant to this article
was reported.
Summary
Dravet syndrome is a severe epilepsy syndrome of infancy characterised by
seizures of multiple types, often prolonged and particularly fever-sensitive,
with onset in the first year of life, and subsequent developmental delay. This
article aims to present updated data on this syndrome, for which complete
and extensive clinical descriptions led to the discovery of a link with a major
gene, SCN1A, on which abnormalities are found in at least 70% of the patients tested. Our review article follows and summarises the data published
in a 2011 supplement issue of Epilepsia, entitled Severe Myoclonic Epilepsy
Dravet Syndrome: Thirty years Later.
Key words: Dravet syndrome
Introduction
Dravet syndrome is a severe epilepsy syndrome of infancy
characterised by seizures of multiple types, often prolonged
and particularly fever-sensitive, with onset in the first year
of life, and subsequent developmental delay. This article
aims to present updated data on this syndrome, for which
complete and extensive clinical descriptions led to the discovery of a link with a major gene, SCN1A, on which
abnormalities are found in at least 70% of the patients tested
[14]. Our review article follows and summarises the data
published in a 2011 supplement issue of Epilepsia, entitled
Severe Myoclonic E
pilepsy Dravet Syndrome: Thirty years Later
[5].
Historical considerations
Dravet syndrome was identified by Dr Charlotte Dravet in
1978 as severe myoclonic epilepsy in infancy (SMEI) [6].
Two forms were described later, according to predominant
clinical features: typical SMEI and atypical or borderline
SMEI (SMEB), in which myoclonic seizures are lacking
and developmental delay may be milder [710]. Because of
this clinical heterogeneity, the eponym Dravet syndrome
Correspondence:
Christian M. Korff, MD
Neuropdiatrie, Hpital des Enfants
Hpitaux Universitaires de Genve HUG
6, rue Willy Donz
CH-1211 Genve 14
Switzerland
christian.korff[at]hcuge.ch
has been preferred to SMEI (Engel, 2001). Dravet syndrome
fulfils the criteria of an epileptic encephalopathy as defined
by the International League Against Epilepsy (ILAE) in
2010: an electroclinical syndrome associated with a high
probability of encephalopathic features that present or
worsen after the onset of epilepsy tending to be pharmacoresistant [11, 12].
The frequency of Dravet syndrome is estimated at
around 1/20000 to 1/30000 births [10]. In epileptic children
aged less than 15 years, the rate of Dravet syndrome is 1.4%
[13].
Vaccinations (especially for pertussis) have been falsely
implicated as a causal factor in children with a so-called
vaccine encephalopathy. Most of these children in fact had
a de novo mutation on SCN1A [14] in a context of Dravet
syndrome. Although vaccinations, through the febrile reaction they induce, may facilitate earlier onset of Dravet syndrome in patients with SCN1A mutations, these should not
be withheld because they do not affect the outcome of the
disease, and their benefits clearly outweigh the risks [15].
Clinical presentation
Seizures start during the first year of life in otherwise normal
infants. The initial event is often a prolonged, apparently
generalised or unilateral clonic seizure. It f requently appears
in the context of a febrile disease, which may make it
difficult to differentiate Dravet syndrome from a simple
febrile seizure, initially. Additional nonfebrile seizure types
rapidly appear, though, and repeated status epilepticus
episodes, pharmacoresistance and developmental delay are
the rule.
Seizure types
The various seizure types that may be observed in Dravet
syndrome include:
Convulsive seizures, such as apparently generalised
clonic seizures or tonic-clonic seizures, and alternating
unilateral clonic seizures: most of these are, in fact,
secondarily generalised events, or so-called unstable
seizures, shifting from one hemisphere to the other.
They tend to persist throughout the patient history.
Myoclonic seizures: these can be massive, involving
all muscles and sometimes leading to a fall, or milder,
involving only the axial muscles and described as head
nods. They usually occur several times a day, either
S W I S S A R C H I V E S O F N E U R O L O G Y A N D P S Y C H I A T R Y 2013;164(5):1537 www.sanp.ch | www.asnp.ch
153
Review article
isolated or in short bursts, without clear impairment of
consciousness. Dravet syndrome has to be differentiated
from myoclonic epilepsy in infancy (MEI), a rare epileptic syndrome occurring in the first two years of life in
normal children, characterised by brief generalised myoclonic seizures with a good response to valproic acid, and
a favourable long-term prognosis [16, 17].
Atypical absence seizures: these are characterised by a
sudden impairment of consciousness of variable intensity, and may be combined with a myoclonic component. They may be difficult to differentiate from pure
myoclonic seizures. They occur in 40% to 93% of the
cases [18].
Focal seizures: these are focal motor seizures of a limb
and/or a hemiface, with or without loss of consciousness
and autonomic symptoms, which can secondarily generalise. These seizures occur in 43% to 78.6% of patients
[1921].
Tonic seizuresare exceptional in Dravet syndrome.
The occurrence rate for each seizure type is not known with
precision.
All seizures are sensitive to elevated body temperature
(fever, hot water immersion, intense physical exercise), and
photosensitivity (noted in 40% of the patients, often during
the first year of life) or pattern sensitivity are frequent [19].
Development and behaviour
The developmental phenotype spectrum is wide. In most
patients, developmental delay occurs after the second year
of life. Mental retardation (mostly moderate to severe)
occurs in all children, and their language progresses very
slowly. On the motor side, typical children start walking and
talking at a normal age, but their gait remains unsteady.
Neurological deterioration (motor disorders, including
pyramidal or extrapyramidal signs, coordination difficulties,
balance and fine motor disabilities) is often observed on
follow-up.
The development is often reported as stagnating
during the next years of life. Early prolonged seizures have
not been associated with a worse developmental outcome,
but the lack of early absences and myoclonic seizures seem
to be associated with a better outcome. The presence or
absence of SCN1A mutations has not yet been clearly
correlated with a specific developmental phenotype [20].
Behavioural disorders include autistic traits, hyper
activity, and attention deficit, opposition and sleep disorders,
and are often concurrent with the cognitive decline.
Cass-Perrot et al. [21] evaluated the neuropsychological
features of 20 patients over 3 years. All children with
Dravet syndrome had cognitive and behavioural problems.
Neuropsychological skills were all deficient, in motor, linguistic and visual aspects. Every patient had poor motor
function with limited coordination skills; language expression and comprehension was problematic, with dysarthria
and no fluency; all had v
isual-constructive and visual-spatial
deficits.
EEG findings
As with seizures, a great variability exists in electro
encephalographic (EEG) features. Although some seizure
types may be more specific for Dravet syndrome, such as the
aforementioned falsely generalised and unstable seizures, no
interictal or ictal electroencephalography findings are
pathognomonic. Rather, it is their progressive modification
(as described below) that may suggest the diagnosis [19].
Interictal EEG
The background activity is often normal until the end of the
first year of life. Theta activity, as well as brief discharges of
spike waves, may appear early in the course of the disease.
A steady state is often noted between two to five years, with
increasing paroxysmal discharges of generalised spike waves
and fast polyspike waves, and slowing of the background.
Sleep recordings usually show physiological features. The
background activity may remain normal in up to 40% of
patients with Dravet syndrome [22].
Ictal EEG
Falsely generalised seizures may be associated with either a
focal onset, bilateral asymmetric abnormalities from the
onset till the offset, or bilateral discharges (such as a slow
spike or a spike wave) from the onset, but becoming asymmetric later on.
Unstable seizures are characterised by alternating
discharges emerging from different parts of the brain. The
location of the EEG discharges may change during the same
event, and the pathways of propagation are variable from
one seizure to another.
Myoclonic seizures show generalised or multiple spike
waves at 3 or more Hz with two or three brief bursts of
extensor postural changes.
Atypical absences are associated with generalised irregular spike waves at 23.5 Hz.
Focal seizures usually correlate with a rhythmic
sequence of fast polyspike intermixed with theta activity
arising from the unilateral temporo-parieto-occipital region.
Obtundation status usually correlates with diffuse dysrhythmia of slow waves with focal and diffuse spikes [19].
Genetics
Overall, 70% to 80% of Dravet syndrome patients carry a
mutation on the gene that encodes the alpha 1 subunit of
the sodium channel (SCN1A) [23]. Harkin et al. showed that
patients with c lassic Dravet syndrome more frequently carry
SCN1A mutations than patients with the borderline form
[24].
SCN1A is one of the most relevant epilepsy genes, and
has been involved in a constantly growing number of
epilepsies, in addition to Dravet syndrome, such as GEFS+,
atypical Panayiotopoulos syndrome, and various types of
epileptic encephalopathies, among others.
S W I S S A R C H I V E S O F N E U R O L O G Y A N D P S Y C H I A T R Y 2013;164(5):1537 www.sanp.ch | www.asnp.ch
154
Review article
The alpha 1 subunit is involved in the activation of
ABAergic interneurons in the neocortex and the hippo
G
campus. The major mechanism of SCN1A-related epilepsies
is likely to be a loss of function of these inhibitory inter
neurones [25, 26].
More than 500 mutations along the gene have been
described in patients with Dravet syndrome [2729].
Seventy percent are sequence mutations (40% of which are
truncating, 40% missense and 20% splice-site). Most of
these are de novo, and 5% to 10% are familial [14]. Somatic
or germline mosaicism has been reported in some patients
and may explain the existence of a healthy transmitting
parent, which has been recently reported [29]. Exon deletions or chromosomal r earrangements of SCN1A account for
around 3%. Truncating mutations are linked with an earlier
age of onset of seizures [28]. No correlation between the
presence of a specific mutation and seizure type has been
found.
Mutations of protocadherin 19 (PCDH19) have been
found in SCN1A-negative female patients with a Dravet syndrome-like phenotype, also known as epilepsy limited to
females with mental retardation [30, 31]. One Dravet syndrome patient has been r eported to carry a mutation in the
gamma 2 subunit gene of the GABA-A receptor (GABRG2)
[32] and another one on SCN1B [33]. One Dravet syndrome
patient has been reported as harbouring mutations in both
SCN1A and SCN9A, suggesting that SCN9A variant can be a
modifier-gene for Dravet syndrome [34].
In 20% to 30% of patients, the underlying genetic
defect remains unknown. Other genes are likely to be
discovered in a near future with the increasing availability of
continuously improving genetic techniques.
Neuroimaging
Most Dravet syndrome patients have a normal brain magnetic resonance imaging (MRI). Nonspecific structural
abnormalities may be observed in some children. These include diffuse cerebral or cerebellar atrophy, increased white
matter signal, ventricular abnormalities, cortical dysplasia or
arachnoid cysts [5]. In a few patients, cortical-subcortical
atrophy developed over the years [35]. Two systematic
retrospective studies have investigated MRI findings in
Dravet syndrome patients [36, 37]. Siegler et al. [36] found
hippocampal sclerosis in 10 of 14 children with Dravet syndrome (nine unilateral, one bilateral) after eight years of
follow-up: six of these ten had an initial normal MRI, and
none of them had mesial temporal lobe epilepsy. The
authors concluded that prolonged febrile convulsions may
be responsible for hippocampal sclerosis, but that additional
factors (genetic, developmental and individual sensitivity)
are also likely to play a role in the process. Striano et al. [37]
analysed 58 Dravet syndrome patients and found that 13 patients (22.4%) had MRI anomalies: eight had cortical brain
atrophy (ventricular abnormalities in three, cerebellar
atrophy in one and hyperintense white matter signal in
one), three showed ventricular enlargement only, one had
unilateral hippocampal sclerosis, and one had focal cortical
dysplasia. Only one patient had hippocampal sclerosis,
which led the
authors to conclude that an association
etween prolonged febrile seizures and hippocampal sclerob
sis is unlikely in Dravet syndrome. The origin of these structural focal abnormalities remains uncertain. No correlation
has been found between MRI a bnormalities and epilepsy
severity. Single-photon emission computed tomography
(SPECT) or positron emission tomography (PET) studies
showed unilateral or bilateral hypoperfusion or hypometa
bolism, but without strict correlation with EEG findings.
Pharmacological treatment
Seizures in Dravet syndrome are invariably difficult to control. The combination of stiripentol, valproate and clobazam
was demonstrated to be particularly effective in two randomised controlled trials [38]. Compared with placebo, a
70% reduction in seizure frequency was reported [38]. This
combination also seems to reduce the duration of seizures.
It is currently recommended to start stiripentol as soon
as the diagnosis of Dravet syndrome is secure. Stiripentol is
a GABAergic agent that acts as a modulator of the GABA-A
receptor via its alpha 3 subunit [39]. Stiripentol is also an
inhibitor of cytochrome P450 with potential increase in
plasma concentration of other antiepileptic drugs, whose
dosage should be reduced accordingly. Side effects include
drowsiness, slowing of mental function, ataxia, diplopia, loss
of appetite, weight loss, abdominal pain and neutropenia,
but overall, stiripentol has a good long-term safety profile.
Topiramate, levetiracetam and bromide may be efficient as
adjunctive therapies. A favourable effect of add-on fenfluramine has also been recently suggested (ICNA congress,
Brisbane, 2012).
Lamotrigine, carbamazepine, vigabatrin and pheno
barbital may worsen seizures and should be avoided in
Dravet syndrome patients.
Nonpharmacological treatments
The ketogenic diet
The ketogenic diet (KD) is a valuable addition or alternative
to medication in Dravet syndrome. In a recent study [40] of
16 patients with Dravet syndrome, two were seizure-free,
ten had a 75% to 99% decrease and four a 50% to 74% decrease in seizures, after a minimum two years of follow-up.
Caraballo et al. [41] showed that most of their Dravet syndrome patients treated with a KD for at least one year had a
decrease of more than 75% in their seizures, that all had a
better quality of life and that all had a reduction in the number of antiepileptic drugs required. The reported favourable
effects on seizure control and on EEG features seem to be
long-lasting, even after the diet has been discontinued. The
classical diet is based on a 4:1 ratio of fat to carbohydrates
and protein (90% of the energy comes from fat and 10%
from carbohydrates and protein). It mimics the biochemical
response to starvation and ketone bodies b
ecome the main
source of energy for the brain. A
lternative diets, such as the
Atkins diet and the low-glycaemic index diet seem to be as
S W I S S A R C H I V E S O F N E U R O L O G Y A N D P S Y C H I A T R Y 2013;164(5):1537 www.sanp.ch | www.asnp.ch
155
Review article
efficient as the classic KD [42]. Expert recommendations on
the use of the KD have been published [43]. Because several
inborn errors of metabolism are absolute contraindications
for the KD, these should be ruled out before starting the
diet. Patients on a KD should be supplemented with sugarfree multivitamin products. Counselling and frequent follow-up visits with paediatric neurologists and nutritionists,
as well as biological parameter monitoring are needed. Its
long-term safety profile is favourable. In a recent study
which analysed the effects of the KD after more than six
years of follow-up [44], rare complications, such as kidney
stones, decreased growth and bone fractures, were reported,
but lipid profiles were not significantly affected.
Vagus nerve stimulation
Vagus nerve stimulation (VNS) may be an alternative treatment, but further studies in Dravet syndrome are needed as
only rare patients have benefitted from this approach. Three
Dravet syndrome p
atients were reported by Cersosimo et al.
[45]: two of them had a 50% to 74% decrease in seizure
frequency, one remained unchanged. The efficacy pro
gressively improved with treatment durations of up to 36
months. No significant c omplications were reported, except
transient local pain and voice hoarseness.
Outcome in adulthood and mortality
A few patients were followed up until adulthood [22].
Moderate to severe mental retardation and impairment of
communication skills were observed in all of them. Motor
abnormalities often include cerebellar features affecting
gross and fine movements. Owing to orthopaedic problems,
such as kyphoscoliosis, flat or claw feet, walking is often
difficult. In some patients, a major personality disorder, with
autistic or psychotic features, has been observed. Patients
who live independently are the exception. The social outcome is poor, as well. Epileptic seizures become less frequent
and nocturnal generalised tonic-clonic seizures with a focal
onset are the most frequently observed. Fever, photo- and
pattern sensitivity decreases with age [46].
A high risk of mortality exists in Dravet syndrome, particularly during childhood. Major causes of death include
complications of status epilepticus in younger children, and
sudden unexpected death in epilepsy (SUDEP) in older ones.
The minimum SUDEP rate is estimated at 15.4% [22, 35].
Future perspectives
Dravet syndrome should be suspected in any healthy child
with prolonged and recurrent convulsions triggered by fever
or hyperthermia in the first year of life, particularly if the
evolution shows a polymorphic pharmacoresistant epilepsy
with psychomotor delay. The presence of SCN1A abnormalities is an additional diagnostic argument, and genetic analyses should be rapidly performed in order to optimise management and treatment approaches. The role of additional
genes such as SCN9A modifying SCN1A requires more
studies, and a precise phenotype-genotype correlation
r emains to be established. Most cerebral MRI of Dravet syndrome patients are normal, but some develop atrophy or
hippocampal sclerosis on follow-up. The origin of these
structural abnormalities remains unclear. No correlation
seems to exist between the presence of MRI abnormalities
and the duration or severity of epilepsy. Structural changes
may themselves become a substrate for the development of
encephalopathic features. Recently developed imaging tools
such as simultaneous recording of electroencephalography
and functional magnetic resonance (EEG-fMRI), spectro
scopy or diffusion tensor imaging (DTI), may help charac
terise this syndrome. In a recent study, Moehring et al. tried
to identify a specific epileptic network in ten patients
with SCN1A-positive Dravet syndrome using EEG-fMRI; no
common a ctivation pattern was observed in the nine children in whom blood oxygen dependent level signal changes
were identified [47].
The reasons for cognitive decline is not yet elucidated,
either. The question whether Dravet syndrome is a true
epileptic encephalopathy or not remains open. Inherent to
the concept of epileptic encephalopathy is the notion that
suppression of epileptic seizures may improve development.
Recent observations show that less severe cognitive and
behavioural disorders may occur if the diagnosis is made
early in the course of the condition and if adequate drug
therapy is used [48].
In conclusion, long-term prospective studies are needed
to establish whether earlier diagnosis, adequate treatment
and better seizure control may influence the progress of the
clinical deterioration observed in this severe condition.
References
1 Nabbout R, Gennaro E, Dalla Bernardina B, Dulac O, Madia F, Bertini E, et al.
Spectrum of SCN1A mutations in severe myoclonic epilepsy of infancy.
Neurology. 2003;60:196167.
2 Wallace RH, Hodgson BL, Grinton BE, Gardiner RM, Robinson R,
Rodriguez-Casero V, et al. Sodium channel alpha1-subunit mutations
in severe myoclonic epilepsy of infancy and infantile spasms. Neurology.
2003;61:7659.
3 Fujiwara T, Sugawara T, Mazaki-Miyazaki E, Takahashi Y, Fukushima K,
Watanabe M, et al. Mutations of sodium channel alpha subunit type 1
(SCN1A) in intractable childhood epilepsies with frequent generalized
tonic-clonic seizures. Brain. 2003;126:53146.
4 Claes L, Del-Favero J, Ceulemans B, Lagae L, Van Broeckhoven C,
De Jonghe P. De novo mutations in the sodium-channel gene SCN1A cause
severe myoclonic epilepsy of infancy. Am J Hum Genet. 2001;68:132732.
5 Dravet C, Bureau M, Dalla Bernardina B, Guerrini R. Severe myoclonic
epilepsy in infancy (Dravet syndrome) 30 years later. Epilepsia. 2011;52
(Suppl 2):12.
6 Dravet C. Les pilepsies graves de lenfant. La Vie Mdicale. 1978;8:5438.
7 Ogino T, Ohtsuka Y, Yamatogi Y, Oka E, Ohtahara S. The epileptic syndrome
sharing common characteristics during early childhood with severe myoclonic
epilepsy in infancy. Jpn J Psychiatry Neurol. 1989;43:47981.
8 Dravet C BM, Guerrini R, Giraud N, Roger J. Severe myoclonic epilepsy
in infancy. In: Roger J, Bureau M, Dravet C, Dreifuss FE, Perret A, Wolf P,
editors. Epileptic syndromes in infancy, childhood and adolescence.
2nd ed. London: John Libbey & Company Ltd; 1992. p. 7588.
9 Kanazawa. Medically intractable generalized tonic-clonic or clonic seizures
in infancy. J Epil. 1992;5:1438.
10 Yakoub M, Dulac O, Jambaque I, Chiron C, Plouin P. Early diagnosis of severe
myoclonic epilepsy in infancy. Brain Dev. 1992;14:299303.
11 Berg AT, Berkovic SF, Brodie MJ, Buchhalter J, Cross JH, van Emde Boas W,
et al. Revised terminology and concepts for organization of seizures and
epilepsies: report of the ILAE Commission on Classification and Terminology,
2005-2009. Epilepsia. 2010;51:67685.
12 Catarino CB, Liu JY, Liagkouras I, Gibbons VS, Labrum RW, Ellis R, et al.
Dravet syndrome as epileptic encephalopathy: evidence from long-term
course and neuropathology. Brain. 2011;134:2982-3010.
S W I S S A R C H I V E S O F N E U R O L O G Y A N D P S Y C H I A T R Y 2013;164(5):1537 www.sanp.ch | www.asnp.ch
156
Review article
13 Dura-Trave T, Yoldi-Petri ME, Gallinas-Victoriano F. Epilepsy in children
in Navarre, Spain: epileptic seizure types and epileptic syndromes.
J Child Neurol. 2007;22:8238.
14 Berkovic SF, Harkin L, McMahon JM, Pelekanos JT, Zuberi SM, Wirrell EC,
et al. De-novo mutations of the sodium channel gene SCN1A in alleged
vaccine encephalopathy: a retrospective study. Lancet Neurol. 2006;5:
48892.
15 McIntosh AM, McMahon J, Dibbens LM, Iona X, Mulley JC, Scheffer IE, et al.
Effects of vaccination on onset and outcome of Dravet syndrome:
a retrospective study. Lancet Neurol. 2010;9:5928.
16 Auvin S, Pandit F, De Bellecize J, Badinand N, Isnard H, Motte J, et al. Benign
myoclonic epilepsy in infants: electroclinical features and long-term follow-up
of 34 patients. Epilepsia. 2006;47:38793.
17 Darra F, Fiorini E, Zoccante L, Mastella L, Torniero C, Cortese S, et al.
Benign myoclonic epilepsy in infancy (BMEI): a longitudinal electroclinical
study of 22 cases. Epilepsia. 2006;47 (Suppl 5):315.
18 Dravet C GR. Dravet syndrome. Topics in Epilepsy, John Libbey Eurotext.
2011;3:22.
19 Bureau M, Dalla Bernardina B. Electroencephalographic characteristics
of Dravet syndrome. Epilepsia. 2011;52 (Suppl 2):133.
20 Ragona F, Granata T, Dalla Bernardina B, Offredi F, Darra F, Battaglia D, et al.
Cognitive development in Dravet syndrome: a retrospective, multicenter
study of 26 patients. Epilepsia. 2011;52:38692.
21 Cass-Perrot C WM, Dravet C. Neuropsychological aspects of severe
myoclonic epilepsy in infancy. Neuropsychology of Childhood Epilepsy, edited
by Jambaqu et al. 2001.
22 Dravet C DG, Battaglia D Severe myoclonic epilepsy of infancy (Dravet
syndrome). In: Nikaronova M, Genton P, Sabers A, editors. Topics in epilepsy.
Long term evolution of epileptic encephalopathies. Montrouge: John Libbey
Eurotext; 2009. p. 2938.
23 Marini C, Scheffer IE, Nabbout R, Suls A, De Jonghe P, Zara F, et al.
The genetics of Dravet syndrome. Epilepsia. 2011;52 (Suppl 2):249.
24 Harkin LA, McMahon JM, Iona X, Dibbens L, Pelekanos JT, Zuberi SM, et al.
The spectrum of SCN1A-related infantile epileptic encephalopathies.
Brain. 2007;130:84352.
25 Yu FH, Mantegazza M, Westenbroek RE, Robbins CA, Kalume F, Burton KA,
et al. Reduced sodium current in GABAergic interneurons in a mouse model
of severe myoclonic epilepsy in infancy. Nat Neurosci. 2006;9:11429.
26 Ogiwara I, Miyamoto H, Morita N, Atapour N, Mazaki E, Inoue I, et al. Nav1.1
localizes to axons of parvalbumin-positive inhibitory interneurons: a circuit
basis for epileptic seizures in mice carrying an Scn1a gene mutation.
J Neurosci. 2007;27:59035914.
27 Mulley JC, Nelson P, Guerrero S, Dibbens L, Iona X, McMahon JM, et al.
A new molecular mechanism for severe myoclonic epilepsy of infancy: exonic
deletions in SCN1A. Neurology. 2006;67:10945.
28 Marini C, Mei D, Temudo T, Ferrari AR, Buti D, Dravet C, et al. Idiopathic
epilepsies with seizures precipitated by fever and SCN1A abnormalities.
Epilepsia. 2007;48:167885.
29 Depienne C, Trouillard O, Saint-Martin C, Gourfinkel-An I, Bouteiller D,
Carpentier W, et al. Spectrum of SCN1A gene mutations associated with
Dravet syndrome: analysis of 333 patients. J Med Genet. 2009;46:18391.
30 Depienne C, Bouteiller D, Keren B, Cheuret E, Poirier K, Trouillard O, et al.
Sporadic infantile epileptic encephalopathy caused by mutations in PCDH19
resembles Dravet syndrome but mainly affects females. PLoS Genet.
2009:5:e1000381.
31 Scheffer IE, Turner SJ, Dibbens LM, Bayly MA, Friend K, Hodgson B, et al.
Epilepsy and mental retardation limited to females: an under-recognized
disorder. Brain. 2008;131:91827.
32 Harkin LA, Bowser DN, Dibbens LM, Singh R, Phillips F, Wallace RH, et al.
Truncation of the GABA(A)-receptor gamma2 subunit in a family with
generalized epilepsy with febrile seizures plus. Am J Hum Genet. 2002;70:
5306.
33 Patino GA, Claes LR, Lopez-Santiago LF, Slat EA, Dondeti RS, Chen C, et al.
A functional null mutation of SCN1B in a patient with Dravet syndrome.
J Neurosci. 2009;29:1076478.
34 Singh NA, Pappas C, Dahle EJ, Claes LR, Pruess TH, De Jonghe P, et al.
A role of SCN9A in human epilepsies, as a cause of febrile seizures and as
a potential modifier of Dravet syndrome. PLoS Genet. 2009;5:e1000649.
35 Dravet C BM, Oguni H, Fukuyama Y, Dokar O. Severe myoclonic epilepsy
in infancy (Dravet Syndrome). In: Roger J, Bureau M, Dravet C, Genton P,
Tassinari CA, Wolf P, editors. Epileptic syndromes in infancy, childhood and
adolescence. 4th ed. London: John Libbey Eurotext Ltd; 2005. p. 89113.
36 Siegler Z, Barsi P, Neuwirth M, Jerney J, Kassay M, Janszky J, et al.
Hippocampal sclerosis in severe myoclonic epilepsy in infancy: a retro
spective MRI study. Epilepsia. 2005;46:7048.
37 Striano P, Mancardi MM, Biancheri R, Madia F, Gennaro E, Paravidino R,
et al. Brain MRI findings in severe myoclonic epilepsy in infancy and
genotype-phenotype correlations. Epilepsia. 2007;48:10926.
38 Chiron C, Marchand MC, Tran A, Rey E, dAthis P, Vincent J, et al. Stiripentol
in severe myoclonic epilepsy in infancy: a randomised placebo-controlled
syndrome-dedicated trial. STICLO study group. Lancet. 2000;356:163842.
39 Fisher JL. The effects of stiripentol on GABA(A) receptors. Epilepsia. 2011;52
(Suppl 2):768.
40 Caraballo RH. Nonpharmacologic treatments of Dravet syndrome: focus on
the ketogenic diet. Epilepsia. 2011;52 (Suppl 2):7982.
41 Caraballo RH, Cersosimo RO, Sakr D, Cresta A, Escobal N, Fejerman N.
Ketogenic diet in patients with Dravet syndrome. Epilepsia. 2005;46:
53944.
42 Kossoff EH, Zupec-Kania BA, Amark PE, Ballaban-Gil KR, Christina Bergqvist
AG, Blackford R, et al. Optimal clinical management of children receiving the
ketogenic diet: recommendations of the International Ketogenic Diet Study
Group. Epilepsia. 2009;50:30417.
43 Stafstrom CE, Zupec-Kania B, Rho JM. Epilepsia. Ketogenic diet and
treatments. Introduction/perspectives. Epilepsia. 2008;49 (Suppl 8):12.
44 Groesbeck DK BR, Kossoff EH. Long-term use of the ketogenic diet in the
treatment of epilepsy. Dev Med Child Neurol. 2006;48:97881.
45 Cersosimo RO, Bartuluchi M, De Los Santos C, Bonvehi I, Pomata H,
Caraballo RH. Vagus nerve stimulation: effectiveness and tolerability in
patients with epileptic encephalopathies. Childs Nerv Syst. 2011;27:78792.
46 Akiyama M, Kobayashi K, Yoshinaga H, Ohtsuka Y. A long-term follow-up
study of Dravet syndrome up to adulthood. Epilepsia. 2010;51:104352.
47 Moehring J, von Spiczak S, Moeller F, Helbig I, Wolff S, Jansen O, et al.
Variability of EEG-fMRI findings in patients with SCN1A-positive Dravet
syndrome. Epilepsia. 2013;54:91826.
48 Buoni S, Orrico A, Galli L, Zannolli R, Burroni L, Hayek J, et al. SCN1A
(2528delG) novel truncating mutation with benign outcome of severe
myoclonic epilepsy of infancy. Neurology. 2006;66:6067.
S W I S S A R C H I V E S O F N E U R O L O G Y A N D P S Y C H I A T R Y 2013;164(5):1537 www.sanp.ch | www.asnp.ch
157
Você também pode gostar
- Bahasa Inggris: Kumpulan N Al Latihan Njian Renerimaan Eal N Regawai Negeri NipilDocumento6 páginasBahasa Inggris: Kumpulan N Al Latihan Njian Renerimaan Eal N Regawai Negeri NipilrafikaAinda não há avaliações
- Iaet 11 I 4 P 229Documento4 páginasIaet 11 I 4 P 229rafikaAinda não há avaliações
- Jurnal Glaukoma PrintDocumento15 páginasJurnal Glaukoma PrintrafikaAinda não há avaliações
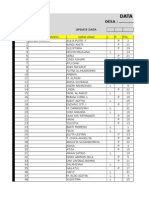
- Data Base Kia Muara BulianDocumento1.263 páginasData Base Kia Muara BulianrafikaAinda não há avaliações
- Data Base Kia Muara BulianDocumento1.269 páginasData Base Kia Muara BulianrafikaAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5795)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1091)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Phenytoin PAR 45Documento65 páginasPhenytoin PAR 45Lourdes VictoriaAinda não há avaliações
- Presentasi Jurnal Kejang DemamDocumento21 páginasPresentasi Jurnal Kejang DemamSeptiana WahyuAinda não há avaliações
- Seizure Acute ManagementDocumento29 páginasSeizure Acute ManagementFridayana SekaiAinda não há avaliações
- Brain Tumours and Driving - A Guide For Clinicians Cancer Institute NSWDocumento2 páginasBrain Tumours and Driving - A Guide For Clinicians Cancer Institute NSWmyscribe0% (1)
- Need For Speed Porsche Unleashed - Manual - Win - EN PDFDocumento32 páginasNeed For Speed Porsche Unleashed - Manual - Win - EN PDFdAinda não há avaliações
- Epilepsy SeizuresDocumento1 páginaEpilepsy Seizuresapi-518183280Ainda não há avaliações
- 3rd International Congress On Neurology and Epidemiology: AbstractsDocumento94 páginas3rd International Congress On Neurology and Epidemiology: AbstractsKanchanaKesavanAinda não há avaliações
- Epilepsy and Literary Creativeness. DostoevskyDocumento17 páginasEpilepsy and Literary Creativeness. DostoevskyAlejandro BejaranoAinda não há avaliações
- AKP Paper 2 PDFDocumento54 páginasAKP Paper 2 PDFMostafa Mahmoud Elsebey100% (2)
- CNS Path Pharm KelnerDocumento9 páginasCNS Path Pharm Kelnerjazzdoc007Ainda não há avaliações
- CDC MMR, MMR+V, MMRV Seizure RatesDocumento4 páginasCDC MMR, MMR+V, MMRV Seizure RatesVaccineInformation83% (6)
- Acupunture For Small Animal Neurologic DisordersDocumento19 páginasAcupunture For Small Animal Neurologic DisordersJorge VergaraAinda não há avaliações
- Neonatal SeizuresDocumento25 páginasNeonatal SeizuresJUAN CAMILO LANDAZURIAinda não há avaliações
- Assessment of Non-Epileptic Seizures - Link PDFDocumento6 páginasAssessment of Non-Epileptic Seizures - Link PDFKaram Ali ShahAinda não há avaliações
- MCQ Neuro SampleDocumento12 páginasMCQ Neuro SampleMutiara AdystiAinda não há avaliações
- Comparison of BenzodiazepinesDocumento8 páginasComparison of BenzodiazepinesDarryl BettsAinda não há avaliações
- 4 Oet Reading Summary 2.0Documento19 páginas4 Oet Reading Summary 2.0Vijayalakshmi Narayanaswami0% (3)
- Febrile Convulsion & EpilepsyDocumento17 páginasFebrile Convulsion & EpilepsyprajwalAinda não há avaliações
- Manual PDFDocumento17 páginasManual PDFcendol dawetAinda não há avaliações
- Management of Medically Compromised Orthodontic PatientsDocumento64 páginasManagement of Medically Compromised Orthodontic Patientsakshi1947Ainda não há avaliações
- Newborn EmergenciesDocumento83 páginasNewborn EmergencieshwelpAinda não há avaliações
- CNS History TakingDocumento4 páginasCNS History TakingDuha B. Salim100% (1)
- Medical and Surgical Emergencies Karen BallDocumento62 páginasMedical and Surgical Emergencies Karen Ballapi-195799092Ainda não há avaliações
- Verbena OfficinalisDocumento4 páginasVerbena OfficinalisRama Ammar FaresAinda não há avaliações
- Key FactsDocumento3 páginasKey FactsionutmateAinda não há avaliações
- Vol 7 No. 3Documento99 páginasVol 7 No. 3G VenkateshAinda não há avaliações
- Warning: Read Before Playing: Minimum System RequirementsDocumento11 páginasWarning: Read Before Playing: Minimum System Requirementsaulia aqobyAinda não há avaliações
- Brunner Normal Intracranial Pressure 10-20 MMHGDocumento16 páginasBrunner Normal Intracranial Pressure 10-20 MMHGlovely99_dyahAinda não há avaliações
- Case Report Kejang NeonatusDocumento12 páginasCase Report Kejang NeonatusSonya HyekyoAinda não há avaliações
- EpilepsyDocumento36 páginasEpilepsypodki gurungAinda não há avaliações