Escolar Documentos
Profissional Documentos
Cultura Documentos
Keratocon
Enviado por
Ana-Maria MisiciTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Keratocon
Enviado por
Ana-Maria MisiciDireitos autorais:
Formatos disponíveis
C L I N I C A L
A N D
E X P E R I M E N T A L
OPTOMETRY
INVITED REVIEW
New perspectives on keratoconus as revealed by
corneal confocal microscopy
Clin Exp Optom 2008; 91: 1: 3455
Nathan Efron* BScOptom PhD DSc
Joanna G Hollingsworth BSc(Hons) PhD
MCOptom
*
Institute of Health and Biomedical
Innovation and School of Optometry,
Queensland University of Technology,
Brisbane, Australia
Optometry Giving Sight, Association of
Optometrists, London, United Kingdom
E-mail: n.efron@qut.edu.au
Submitted: 1 May 2007
Revised: 20 June 2007
Accepted for publication: 6 July 2007
DOI:10.1111/j.1444-0938.2007.00195.x
Confocal microscopy (CM) of keratoconus is reviewed. In the Manchester Keratoconus
Study (MKS), slit scanning CM was used to evaluate 29 keratoconic patients and light
microscopy (LM) was performed on two of the keratoconic corneas post-keratoplasty.
The findings of the MKS are compared with other CM studies. Consideration of the
differences between studies of cell counts is confounded by the use of different experimental controls. A consensus exists among studies with respect to qualitative observations. The epithelium appears more abnormal with increasing severity of keratoconus.
In severe disease, the superficial epithelial cells are elongated and spindle shaped,
epithelial wing cell nuclei are larger and more irregularly spaced and basal epithelial
cells are flattened. Bowmans layer is disrupted and split in the region of the cone
and intermixed with epithelial cells and stromal keratocytes. Stromal haze and hyperreflectivity observed with CM correspond with apical scarring seen with the slitlamp
biomicroscope (SLB). Hyper-reflective keratocyte nuclei are thought to indicate the
presence of fibroblastic cells. Increased haze detected with CM is found with LM to be
due to fibroblastic accumulation and irregular collagen fibres. Dark stromal bands
observed with CM correlate with the appearance of Vogts striae with SLB. Desemets
membrane appears normal with both CM and LM. Some evidence of endothelial cell
elongation is observed with CM. The application of CM to ophthalmic practice has
facilitated a greater understanding of medical and surgical approaches that are used to
treat keratoconus. This review offers new perspectives on keratoconus and provides a
framework, against which tissue changes in this visually debilitating condition can be
studied in a clinical context in vivo using CM.
Key words: confocal microscope, cornea, keratoconus, keratocyte
Up to the end of the 20th Century, our
clinical view of tissue compromise in living patients with corneal disease was
restricted to what could be observed
macroscopically and under magnification
of up to 40 using a slitlamp biomicroscope (SLB). In the case of
keratoconus, the SLB serves as an
invaluable tool for examining gross tissue
Clinical and Experimental Optometry 91.1 January 2008
34
changes such as apical scarring, Vogts
striae, Fleischer ring (iron deposits
around the base of the cone), corneal
thinning, protrusion and hydrops.1 Other
techniques such as retinoscopy,2 corneal
topographic analysis,3 pachometry3 and
optical coherence tomography3 can assist
in the diagnosis and characterisation of
this condition.
The relatively recent introduction of
the corneal confocal microscope (CM)
has dramatically changed the ophthalmic
clinical landscape, allowing eye-care practitioners to non-invasively view the living
human cornea at magnifications of up to
700.4 Whereas the SLB facilitates observation of the three basic corneal layers
the epithelium, stroma and endothe 2007 The Authors
Journal compilation 2007 Optometrists Association Australia
Corneal confocal microscopy of keratoconus Efron and Hollingsworth
Cornea plana
Normal cornea
Keratoconus
Keratoglobus
Figure 1. Normal and abnormal forms of the human cornea, progressing (left to right) from the flattest to the steepest corneal forms
liumthe CM allows the cornea to be
observed in vivo at a cellular level.4 Specifically, it is possible to observe individual cells and cell nuclei in the various
layers of the epithelium and endothelium,5,6 cell borders and nuclei of stromal
keratocytes, Langerhans cells,7 the fine
epithelial sub-basal nerve plexus8 and
newly-discovered features such as stromal microdots.9 Pathogens such as
acanthamoeba10 and fungi11 can also be
seen in diseased eyes. This technology is
allowing researchers and clinicians to
embark on a new journey of discovery
that is resulting in a more complete
and deeper understanding of the living
human cornea in health and disease and
may pave the way towards the development of new medical and surgical
approaches to the treatment of corneal
disease.
The human cornea can manifest in a
variety of abnormal shapes (Figure 1).
This review will focus on research that has
employed CM to characterise the clinical
histopathology of the keratoconic cornea.
Keratoconus is classically considered
as an asymmetrical, progressive, noninflammatory disorder causing an axial
corneal ectasia. It is characterised by
stromal thinning and corneal steepening,
leading to irregular astigmatism and myopia, which cause a marked distortion in
vision.1,12 Ultrastructural studies1316 have
demonstrated tissue pathology at all levels
of the keratoconic cornea.
This paper will review recent studies
that have used CM to examine patients
suffering from keratoconus, to construct a
comprehensive model of the clinical histopathology of the living keratoconic cornea. Consideration will also be given to
the use of CM to develop a greater understanding of the keratoconic cornea with
concurrent disease and medical and surgical interventions for keratoconus.
THE MANCHESTER KERATOCONUS
STUDY
The Manchester Keratoconus Study
(MKS),1720 which will form the cornerstone of this review, is a recently completed examination of 29 keratoconic
patients (mean age 31 10 years; range 16
to 49 years), who presented consecutively
to the outpatient clinic of the Royal Eye
Hospital in Manchester, UK. Some patients were new to the clinic (referred for
a definitive diagnosis) and some were
existing patients. Both eyes of all patients
were examined, however, due to three
patients having unilateral disease and a
further four patients having previously undergone penetrating keratoplasty, data
were obtained from 51 eyes.
The mean age at diagnosis, as reported
by the patients, was 21 8 years (range 4
2007 The Authors
Journal compilation 2007 Optometrists Association Australia
to 42 years). Male patients made up 76 per
cent of the study group. A family history
of keratoconus was present in 17 per cent
of patients. The majority of patients (62
per cent) were Caucasian, 24 per cent were
of Asian descent and 14 per cent were AfroCaribbean. Ninety per cent of patients
had bilateral keratoconus and 52 per cent
reported that they suffered from some
form of atopy, such as asthma, eczema,
hay fever, general allergies or a combination of these. One patient also suffered
from retinitis pigmentosa. There were no
other associated systemic conditions. A
large number of patients reported a history of eye rubbing (66 per cent).
Fifty per cent of eyes were currently fitted with rigid contact lenses, the majority
of which showed some level of apical
touch (64 per cent). Thirty-three per cent
of eyes were corrected with spectacles.
One patient was fitted bilaterally with
scleral contact lenses. Three patients were
awaiting surgery and were no longer using
any form of visual correction.
Clinical investigative techniques
SLITLAMP BIOMICROSCOPY
All eyes were examined with a SLB and 27
per cent of eyes displayed corneal staining, 37 per cent of eyes demonstrated corneal scarring and 37 per cent of eyes had
Vogts striae.
Clinical and Experimental Optometry 91.1 January 2008
35
Corneal confocal microscopy of keratoconus Efron and Hollingsworth
CORNEAL TOPOGRAPHY
Corneal topography was attempted on
all 51 eyes using the EyeSys 2000 Corneal Analysis System (EyeSys Technologies, Houston, Texas, USA). This
enabled disease severity to be classified
by corneal curvature, using the same system as used in the Collaborative Longitudinal Evaluation of Keratoconus
(CLEK) study.21 According to this system,
disease severity is classified with respect
to the curvature of the steepest corneal
meridian as follows: mild, less than 45 D;
moderate, 45 to 52 D; and severe, more
than 52 D.
Corneal topographical maps were produced from 46 eyes. In the remaining
five eyes, the cornea was too distorted or
scarred to obtain a reading of corneal curvature; these were classified as severe keratoconus. The average steep keratometric
reading was 52.1 7.9 D (range 42.5 to
81.0 D). The majority of patients had
either moderate or severe keratoconus;
specifically, 12 per cent of eyes exhibited
mild keratoconus, 39 per cent of eyes had
moderate keratoconus and 49 per cent
of eyes were classified as having severe
keratoconus.
CONFOCAL MICROSCOPY
All keratoconic patients and control subjects were examined using an in vivo slit
scanning real time CM (Tomey Confoscan
P4, Erlangen, Germany) fitted with an
Achroplan
40X/0.75NA
immersion
objective. One drop of local anaesthetic
(Benoxinate Hydrochloride 0.4%, Chauvin Pharmaceuticals, Romford, UK) was
instilled into the lower fornix of the
eye.22 A drop of polymer gel (Viscotears,
CIBA Vision, Duluth, Georgia, USA) was
applied to the microscope probe prior to
the examination to optically couple the
microscope objective lens to the cornea.
CM was performed on the central cornea
of all eyes.
Images obtained of the corneal layers of
the 51 keratoconic eyes during CM examinations were stored on S-VHS videotape.
Each examination was evaluated frame
by frame by a single examiner. Images
were saved of the epithelium, Bowmans
layer, the anterior and posterior stroma,
Clinical and Experimental Optometry 91.1 January 2008
36
Desemets membrane (where visible)
and the endothelium. In the course of
scanning through the cornea along the
central anterior-posterior axis, image
frames of the anterior stroma were taken
to be those immediately posterior to
Bowmans layer and image frames of the
posterior stroma were taken to be those
immediately anterior to the endothelium.
In addition, images showing any abnormality were saved regardless of their position within the cornea.
For quantitative analysis, only the right
eye of each study participant was examined; however, in cases where it was not
possible to use the right eye (such as in
unilateral keratoconus or if the right eye
had previously undergone penetrating
keratoplasty), the left eye was used. Thus,
quantitative data were obtained from 29
eyes. Quantitative analysis was conducted
using dedicated software that came with
the CM (Confocommander 2.7.1, Tomey,
Erlangen, Germany). At least three frames
were analysed for each corneal layer and
an average was taken. When examining
images of the endothelium a minimum of
50 cells was evaluated.
During the course of the study, it became apparent that the images obtained
of the keratoconic stroma were degraded
to varying degrees. Many images were hazy
and often had a hyper-reflective appearance. Keratocyte nuclei were poorly differentiated in hazy images, rendering
analysis difficult. To quantify the levels of
haze and hyper-reflectivity, a grading scale
of this phenomenon was constructed from
representative images (Figure 2). The
meaning of each level of grading is explained in Table 1. The level of haze in
each stromal image analysed in this work
was graded using this tool.
HISTOLOGICAL STUDIES
Two of the patients examined in this study
(referred to as Patient A and Patient B)
went on to have penetrating keratoplasty
and the excised corneal buttons were subsequently available for examination using
light microscopy (LM). Following surgical
removal, the corneal buttons were placed
in 10 per cent neutral buffered formalin
(pH 7.6). The buttons were cut into two
sections along the vertical meridian, dehydrated through graded alcohols (70, 90
and 100 per cent), de-lipidised in xylene
and impregnated with paraffin wax at
56C.
Patient A had unilateral keratoconus.
Limited cross-sections of the central cornea of this patient were available and were
stained with haemotoxylin and eosin.
Serial step sections were prepared from
the excised cornea of Patient B and were
stained in an alternating manner with haemotoxylin and eosin, Periodic acid-Schiff
and Massons trichrome.
The histological appearance of the corneas of these two patients is considered
below in the relevant sections relating to
each corneal substructure.
THE CORNEA IN KERATOCONUS
Superficial epithelial cells
CM images of the superficial epithelial
cell layer were obtained in 20 per cent of
eyes in the MKS.1720 A normal appearance5,6 was noted in eight per cent of
eyes, all of which were classified as having
moderate keratoconus. Irregular superficial cells with an elongated or spindle-like
shape were found in 12 per cent of eyes.
These patients were classified as having
severe keratoconus (Figure 3).
The CM appearance of elongated epithelial cells has been observed by others.
Somodi and colleagues23 reported seeing
obviously elongated superficial epithelial
cells arranged in a whorl-like fashion.
Wygledowska-Promienska and associates24
noted that desquamating epithelial cells
were elongated and arranged around
the apex of the cornea. Uakhan and
colleagues25 observed the epithelial cells
to be elongated in 18 per cent of keratoconic eyes (all with severe keratoconus).
Desquamating, elongated superficial epithelial cells were observed in one patient.
Weed and associates26 noted that desquamating superficial epithelial cells with
bright cell boundaries were easily visible
in keratoconic eyes.
Uakhan and colleagues25 found that
the density of superficial epithelial cells in
keratoconic eyes (942 137 cells/mm2)
2007 The Authors
Journal compilation 2007 Optometrists Association Australia
Corneal confocal microscopy of keratoconus Efron and Hollingsworth
Grade 0
Grade 1
Grade 2
Grade 3
Grade 4
Figure 2. Grading scale for quantifying the level of haze and hyper-reflectivity in CM images of the corneal stroma. The various grades
are defined in Table 1.
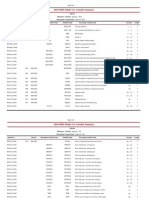
Grade
Severity
Description
Normal
Keratocyte nuclei clearly defined.
Accurate analysis possible in all cases.
Trace
Keratocyte nuclei visible; some background haze.
Accurate analysis possible in most cases.
Mild
Some keratocyte nuclei visible;
many keratocytes partially obscured by haze.
Accurate analysis possible in some cases.
Moderate
Keratocytes almost completely obscured by haze.
Accurate analysis possible in few cases.
Severe
Keratocytes completely obscured by haze;
extreme levels of hyper-reflectivity.
Accurate analysis not possible.
Table 1. Explanation of grades of level of haze and hyper-reflectivity in the corneal
stroma depicted in Figure 2
was not significantly different from that of
age and gender-matched controls (1,087
971 cells/mm2). This contrasts with the
specular microscopy results of Tsubota
and associates,27 who found the mean size
of superficial epithelial cells to be increased in keratoconus.
Mocan and Irkec28 proposed that the
instillation of fluorescein prior to CM
can enhance the imaging characteristics
of this technique. They observed increased intracytoplasmic and nuclear
staining of the superficial epithelium
that was more readily visible after instillation of fluorescein. They suggested that
this increased intracytoplasmic and nuclear staining in the superficial corneal
epithelium of patients with keratoconus
might be indicative of increased epithelial turnover.
Wing cells
The wing cell layer of the epithelium
appeared normal5,6 in only eight per cent
of eyes, all of which had moderate keratoconus. In patients with severe keratoconus, the wing cell layer displayed large,
irregularly spaced nuclei (16 eyes of 12
patients) (Figure 4). No images of the
wing cell layer were obtained from the
remaining patients.
The mean diameter of the wing cell
nuclei in the keratoconic patients (9.2
1.0 m) was significantly greater (p <
0.0001) than that of the normal population (6.4 0.8 m).
Basal epithelial cells
CM images of the epithelial basal cell layer
revealed considerable inter- and intra-
2007 The Authors
Journal compilation 2007 Optometrists Association Australia
patient variability. A normal appearance
of visible cell borders with a regular
arrangement of cells5,6 was found in eight
per cent of eyes, all of which were classified as having either mild or moderate
keratoconus. The most common finding
was a hazy appearance (22 eyes of 16
patients). In 12 per cent of eyes, the basal
cell layer had an irregular appearance,
with large cells and faint cell borders
(Figure 5). These images showed some
similarities to the images obtained of the
wing cell layer but were differentiated
from wing cell images by virtue of their
location adjacent to Bowmans layer. Most
of these eyes were classified as having
severe keratoconus.
The average basal epithelial cell diameter in keratoconic patients (11.4 1.2 m)
was significantly greater (p < 0.05) than
that in control subjects (10.4 0.9 m).
This is consistent with the finding of Weed
and associates,26 who found that that basal
cell density in moderate keratoconus
(4,592 414 cells/mm2) and severe
keratoconus (4,530 596 cells/mm2) was
lower than that of age- and sex-matched
controls (4,912 434 cells/mm2). The
opposite was found by Uakhan and colleagues,25 who reported that basal cell
density in keratoconic eyes (11,273
5,009 cells/mm2) was greater than that of
age- and sex-matched controls (5,941
1,853 cells/mm2). Consistent with this,
Uakhan and colleagues25 reported basal
cell area to be lower (p < 0.05) in keratoconic eyes (115 49 m2) compared with
non-keratoconic controls (179 97 m2).
The epithelial basal cell densities
reported by Uakhan and colleagues25
Clinical and Experimental Optometry 91.1 January 2008
37
Corneal confocal microscopy of keratoconus Efron and Hollingsworth
were significantly higher than those
reported by Weed and associates26 in both
keratoconic patients (unpaired t-test:
moderate keratoconus t = 3.5, p < 0.001,
severe keratoconus t = 4.5, p < 0.0001)
and non-keratoconic control subjects (t =
2.1, p = 0.038). The reason for this is unclear but may be related to the type of
morphometric analysis used. Perhaps also
the authors used different criteria for
locating and imaging the basal cell layer;
for example, imaging at a slightly more
anterior plane in the basal epithelium will
result in a slightly lower cell density
because cells begin to spread laterally
when they progress anteriorly, as part of
the normal growth patterns of the epithelium. Notwithstanding these differences,
both studies appear to be internally consistent, with keratoconus and control eyes
imaged and measured using the same
techniques. Thus, the differences between
keratoconus and control data within each
study must be considered to be valid
findings.
Brightly reflective deposits were observed by Uakhan and colleagues25 within
the basal epithelial cells of 44 per cent
of keratoconic eyes. This material was
thought to represent haemosiderin accumulation corresponding to the Fleischer
ring in those eyes. Rokita-Wala and associates29 observed similar changes using
CM and suggested that the brightly reflective material represents clusters of iron deposits, based on similar appearances in
patients with corneal scars and those who
have been subjected to radial keratotomy
and photorefractive keratectomy.
In the MKS,1720 LM of the corneas of
Patients A and B revealed apparent variations in epithelial thickness across the
cornea in keratoconus. The epithelium
appeared to be thinner in the central
region and thicker towards the inferior
cornea (Figure 6). Similar pan-corneal
variations in epithelial thickness in
keratoconus have been observed using in
vitro techniques of light microscopy30 and
transmission31 and scanning32 electron
microscopy.
Chi, Katzin and Teng33 suggested that
the primary lesion in the keratoconic eye
is located in the basal epithelial cells. They
Clinical and Experimental Optometry 91.1 January 2008
38
Spindle-like epithelial cells
Normal epithelial cells
Irregular & bright epithelial cells
Figure 3. Top row: CM images of the superficial corneal epithelium
A. Elongated spindle-like superficial epithelial cells of Patient B
B. Normal superficial epithelium
C. Irregular elongated superficial cells (left field) and apparently normal superficial
epithelial cells (right field) of Patient B
D. Light microscopic image of the apex of the cone of Patient B, showing regions of
elongated and irregular epithelial cells that correspond to the CM images (40 objective)
Keratoconus
Normal cornea
Figure 4
A. CM image of large, irregularly spaced nuclei in the wing cell layer of the epithelium
in keratoconus
B. CM image of normal wing cell layer
observed degenerative changes early in
the disease. In the later stages of keratoconus, they noted that basal cells disappear
and the epithelium is represented by one
or two layers of flattened superficial cells
lying on an abnormal basement membrane, Bowmans layer or directly on the
anterior stroma.33 The LM and CM obser 2007 The Authors
Journal compilation 2007 Optometrists Association Australia
Corneal confocal microscopy of keratoconus Efron and Hollingsworth
vations in the MKS1720 confirm these histological observations.
Tsubota and associates27 were the first to
report the appearance of elongated superficial cells in vivo using the specular microscope. They found elongated superficial
epithelial cells, which became sharp and
spindle-like in severe cases of keratoconus.
Spindle-shaped cells are characteristic of
the wound-healing response and its associated cellular migration34 and the presence of such cells has also been noted in
patients who have undergone penetrating
keratoplasty or epikeratophakia.35 All of
the corneas displaying elongated superficial cells in the MKS1720 were classified as
severe keratoconus.
Keratoconus
Normal cornea
Figure 5
A. CM image of large cells with faint borders and general haze, in the basal cell layer
of the epithelium in keratoconus
B. CM image of normal basal cell layer
Sub-basal nerve plexus
Patel and McGhee36 used laser scanning
CM to produce two-dimensional reconstructions of the corneal sub-basal nerve
plexus in four eyes of four patients with
keratoconus. This was achieved by having
patients fixate on targets arranged in a
grid to enable imaging of the cornea in
a wide range of positions. A mean of
402 57 images was obtained for each
cornea, to create confluent montages
(Figure 7). The mean dimensions of the
corneal areas mapped were 6.6 0.7 mm
horizontally and 5.9 0.7 mm vertically.
Thus, these authors were essentially able
to elucidate the overall distribution of subbasal nerves in the living central to midperipheral human cornea in keratoconus.
All corneas exhibited abnormal subbasal nerve architecture compared with
patterns previously observed in normal
corneas.8 At the apex of the cone, there
was a tortuous network of nerve fibre bundles, many of which formed closed loops.
At the topographic base of the cone, nerve
fibre bundles appeared to follow the contour of the base, with many of the bundles
running concentrically in this region
(Figure 8). Central sub-basal nerve density was significantly lower (p < 0.01) in
keratoconic corneas (10,478 2,188 m/
mm2) compared with normal corneas
(21,668 1,411 m/mm2).
Uakhan and colleagues25 reported that
nerve fibres in the sub-basal layer had a
thickened, prominent appearance in 14
Inferior cornea
Cone apex (scarred)
Thickened epithelium
(10 layers)
Superior cornea
Thinned epithelium
(3 layers)
Normal epithelium
(5-6 layers)
Figure 6. Whole mount LM section of the cornea of Patient B (top), showing regional
variations in epithelial thickness (bottom)
keratoconic eyes (29 per cent of their sample). Nine of these eyes had severe keratoconus, four had moderate keratoconus
and one had mild keratoconus. The mean
sub-basal nerve fibre thickness was
4.1 0.7 m (range 3.1 to 5.3 m) in keratoconic eyes and 3.7 0.5 m (range 3.1
to 4.6 m) in control eyes. In 31 per cent
2007 The Authors
Journal compilation 2007 Optometrists Association Australia
of keratoconic eyes, sub-basal nerve fibres
showed structural changes, such as excessive branching and curling.
Bowmans layer
Bowmans layer appeared normal5,6 in 22
per cent of eyes when viewed with CM,
that is, as an amorphous, acellular layer.
Clinical and Experimental Optometry 91.1 January 2008
39
Corneal confocal microscopy of keratoconus Efron and Hollingsworth
400 m
Figure 7
A. Schematic showing the architecture of the normal human sub-basal nerve plexus.
B. Wide-field CM montage consisting of 428 images, depicting the architecture of the
sub-basal nerve plexus in a patient with moderate keratoconus. Reproduced with permission from Patel and McGhee.36
60.00
57.00
54.00
51.00
48.00
45.00
42.00
39.00
36.00
33.00
30.00
Anterior tangential
power (D)
2 cm
Figure 8. Electronic tracings of nerve fibre bundles provide schematics devoid of background data in four keratoconic patients, labelled A, B, C and D. These tracings are
superimposed, to scale, onto the corresponding anterior tangential corneal topographical maps of these patients. Reproduced with permission from Patel and McGhee.36
Clinical and Experimental Optometry 91.1 January 2008
40
None of the keratoconic corneas in this
group with a normal appearance of Bowmans layer displayed corneal scarring. All
eyes were classified as having moderate or
severe disease.
Bowmans layer had an abnormal
appearance in the remaining 57 per cent
of eyes. The type of abnormality varied
between patients. In many cases, both epithelial nuclei and keratocyte nuclei from
the anterior stroma appeared to be in the
same plane as Bowmans layer. In some
images of Bowmans layer, nerve fibres
appeared to run in and out of the plane
of the field of view. An increased level of
haze was apparent in many images, which
corresponded to increased haze in the
anterior stroma. The images of Bowmans
layer from three patients (three eyes) contained hyper-reflective patches. Some
images also displayed what appeared to
be hyper-reflective nuclei of the keratocytes (seven eyes). These hyper-reflective
changes were seen only in patients with
apical scarring.
In agreement with the findings of the
MKS,1720 Somodi and colleagues23 and
Wygledowska-Promienska and associates24
noted highly reflective changes near Bowmans layer. Somodi and colleagues23 also
observed fold-like structures. These may
have been artefacts induced by pressure of
the cone tip of the CM against the corneal
surface. Such artefacts have been reported
to occur with the use of CMs that require
corneal contact3739 and the instrument
used by Somodi and colleagues23 required
corneal contact. Another explanation for
the appearance of fold-like structures is
that these may have been so-called Kstructures, which are features that have
been reported to appear in the region of
Bowmans layer in the normal cornea.40
Contrary to the above observations, Uakhan and colleagues25 and Weed and
associates26 were unable to detect any
abnormalities in Bowmans layer in their
keratoconic patients.
In the MKS,1720 histological examination of the cornea of Patient B revealed
Bowmans layer to progress from a normal
single layer to an abnormal bilayer, as it
approached the apical region and to
become split and fragmented in the
2007 The Authors
Journal compilation 2007 Optometrists Association Australia
Corneal confocal microscopy of keratoconus Efron and Hollingsworth
immediate proximity of the apical scar
(Figure 9A). The bilayer appearance is evident in the corresponding CM image
(Figure 9B), in which keratocyte nuclei
can be observed to the right of the field
and a generally amorphous field is
observed on the left, with the odd faint
keratocyte nucleus and a single nerve
fibre traversing the frame. The normal
CM appearance of Bowmans layer is
shown in Figure 9C. With the CM, Bowmans layer appeared as a hyper-reflective
field (Figure 9D) in the heavily scarred
region of the cone.
Many research groups13,14,16,33,41 have
reported the presence of breaks and discontinuities in Bowmans layer in keratoconus using LM and both transmission
and scanning electron microscopy. Sawaguchi and colleagues16 used scanning
electron microscopy to examine the keratoconic cornea and found breaks in Bowmans layer and irregular thinning. These
findings are consistent with the appearance of this layer with the CM in the
majority of the keratoconic eyes in the
MKS.1720 LM of the cornea of Patient B
confirmed that the irregular appearance
of Bowmans layer using CM was consistent with fragmentation and breaks in
Bowmans layer.
The ruptured areas of Bowmans layer
have been reported to be filled with either
epithelium or proliferated collagenous tissue that is derived from the anterior
stroma.13,14,16,33,41 Chi, Katzin and Teng33
documented keratoblasts and newly
formed connective tissue in areas where
Bowmans layer had been destroyed. In
the MKS,1720 LM examination of the cornea confirmed that hyper-reflective nuclei
seen with the CM corresponded to fibroblastic cells. Histological examination of
the cornea of Patient B demonstrated considerable disruption to Bowmans layer in
the region of the apical scar, which consisted of abnormal collagenous material
and fibroblasts. These findings are in
agreement with the observations of Chi,
Katzin and Teng.33 These authors described the presence of keratoblasts, however, at the time that their study was
conducted, it was not known that keratocytes were able to be activated into a fibro-
Scar tissue
Split field
Normal
Hyper-reflectivity
Figure 9. LM image of the apical region of the cornea of Patient B (10 objective). The
dotted circle indicates the scarred region of the cone. The arrows indicate the path of
Bowmans layer, which appears as a single layer at the extreme right of the field and then
splits into a bilayer. The bilayer separates and then rejoins towards the left of the field
to form a bilayer again. The CM images (bottom row) indicate various appearances of
Bowmans layer:
B. Split field in Patient B
C. Normal appearance in a control subject
D. Hyper-reflectivity
blastic status. This was demonstrated many
years later.42
Stroma
Stromal images of the central cornea
obtained by CM showed varying amounts
of haze and hyper-reflectivity. Extreme
levels of haze were present in 44 per
cent of eyes. When visible in these
corneas, the keratocyte nuclei often
displayed an irregular, hyper-reflective
appearance. Severe haze was found to
correspond with apical scarring on SLB
evaluation in 35 per cent of eyes. The
four eyes in which apical scarring was
not apparent when viewed with the SLB
displayed less severe levels of haze on
CM. The remaining eyes showed only
mild degrees of haze. In these patients,
keratocyte nuclei were easily distinguished and had an appearance similar
to that seen in the normal eye.5,6
2007 The Authors
Journal compilation 2007 Optometrists Association Australia
The level of haze was quantified using
the grading scale (Figure 2). The presence of scarring on SLB examination was
significantly related to the level of haze
seen on CM. This was true for both the
anterior (F = 7.6, p < 0.05) and posterior
stroma (F = 5.193, p < 0.05). In some
cases, the location of scarring observed
with the SLB corresponded to the region
of apical touch of the rigid contact lens
that the patient was wearing. Figure 10
illustrates the co-location of contact lens
apical touch and apical scarring in a keratoconic patient (not from the MKS).
Regression analysis was employed to
investigate the effects of haze on the
apparent keratocyte density (KD). Increasing levels of haze were associated with
a reduction in the apparent KD. This
relationship was of a much higher significance for the anterior (r2 = 0.52, F = 24.9,
p < 0.0001) than the posterior stroma
Clinical and Experimental Optometry 91.1 January 2008
41
Corneal confocal microscopy of keratoconus Efron and Hollingsworth
(r2 = 0.16, F = 4.6, p = 0.04). These findings support the validity of the keratoconic haze grading scale. Surprisingly, the
degree of stromal haze was not shown to
bear any relationship to disease severity as
classified by corneal curvature.
Haze in the corneal stroma of keratoconic eyes, especially the anterior stroma,
has also been noted by others, in agreement with the MKS.1720 Uakhan and
colleagues25 reported increased background illumination and reflectivity, and
irregular arrangement of stromal keratocyte nuclei in the anterior stroma of 29
per cent of eyes. They suggested that this
appearance was consistent with varying
degrees of haze and stromal scarring
observed using SLB.
Wygledowska-Promienska and associates24 noted an apparent disarrangement
of collagen fibres reflected by bright
background illumination in the anterior
region of the stroma beneath Bowmans
layer. Somodi and colleagues23 also
observed increased reflectivity in the anterior stroma. In the posterior stroma, keratocytes had extremely long almost parallel
processes, however, in scarred stroma, the
keratocytes were spindle-shaped and
arranged irregularly.
Keratocyte density
An assessment of stromal KD in keratoconus is confounded by two key factors. First,
patients with keratoconus are typically fitted with rigid contact lenses to neutralise
corneal distortion and afford satisfactory
vision. The more severe the condition, the
more likely it is that rigid lenses are being
worn. With the exception of one research
group,43 the general consensus in the literature is that, in normal subjects, contact
lens wear causes an apparent reduction in
KD.4448 This is thought to occur as a result
of the physical impact of lenses on the
corneal epithelium, which releases inflammatory mediators that cause keratocyte
apoptosis.49 Thus, there is a need to determine whether the reduction in KD associated with keratoconus is due to the effects
of lens wear or the direct pathological
effects of keratoconus or possibly both.
Second, as discussed above, the corneal
stroma in keratoconus is often hazy and it
Clinical and Experimental Optometry 91.1 January 2008
42
Figure 10
A. Central bearing of a rigid lens fitted to a patient with keratoconus, revealed with the
aid of fluorescein
B. Same eye as shown in (A) with lens removed. The apical scarring visible within the
pupil corresponds to the region of contact lens bearing. This patient is not from the
MKS. (Photographs courtesy Ruth Cornish)
is difficult to see keratocytes in the presence of significant haze, leading to a
potential under-estimation of KD in such
cases.
The four studies19,25,26,44 that have
addressed the question of KD in keratoconus adopted different approaches in
attempting to account for these confounding influences. Table 2 provides a
summary of estimates of KD published in
these works.19,25,26,44 In reviewing the data
in this table, it should be noted that the
absolute cell densities reported by Erie
and associates44 can not be directly compared with the other data displayed in
the table because Erie and associates44
expressed cell density as a volumetric
measure (cells/mm3), whereas all other
data are expressed as a function of cell
area (cells/mm2). It is not possible to convert between the two units because the
depth of the CM sections used to calculate
field volume was not stated by Erie and
associates.44
Most of the keratoconic patients in the
MKS1720 were wearing rigid contact lenses,
so a control experiment50 was conducted
to determine the effects of rigid lens wear
on KD in non-keratoconic subjects. Slit
scanning CM (Tomey Confoscan P4) was
used to evaluate KD in 22 subjects who
had been wearing rigid lenses on a longterm, daily wear basis. These data were
compared to those of 22 non-lens-wearing
control subjects. Subjects with a previous history of polymethyl methacrylate
(PMMA) lens wear showed a reduction
(p < 0.0001) in anterior keratocyte density
(AKD) and an increased level of haze in
the anterior stroma. When the data of all
22 subjects were combined, AKD and posterior keratocyte density (PKD) appeared
unaffected by rigid lens wear (p = 0.10
and 0.34, respectively). Therefore, nonlens-wearing non-keratoconic subjects
were used as experimental controls in
the MKS. In view of the subsequent study
by Kallinikos and Efron,49 which demonstrated a reduction in KD at all corneal
depths in patients wearing rigid contact
lenses (with no prior PMMA lens wear),
the control used in the MKS may have
been inappropriate.
To remove the confounding effects of
haze-induced image degradation on KD
in the MKS,1720 any images classified as
having haze of grade 2 or above were
removed from the analysis. The mean
anterior and posterior keratocyte densities
were found to be significantly lower in the
keratoconic than control eyes, specifically,
the AKD and PKD were 19 and 10 per cent
lower than in controls, respectively.
Overall, atopy, a history of eye rubbing
and the presence of corneal staining
were related to AKD (r2 = 0.78, F = 9.4,
2007 The Authors
Journal compilation 2007 Optometrists Association Australia
Corneal confocal microscopy of keratoconus Efron and Hollingsworth
Author
Year
Anterior stroma
Control
Keratoconus
Erie and colleagues
44
Hollingsworth, Efron and Tullo19
Uakhan and colleagues25
Weed and associates26
2002
2005
2006
2007
24,564 8,750
32,724 7,105c
909 91d
879 371c
883 111b,e
952 122b,f
883 111b,e
952 122b,f
Posterior stroma
Keratoconus
Control
p-value
35,630 3,858
31,168 6,818c
1,119 80c
1,082 195c
609 66b
609 66b
761 118c
761 118c
p < 0.001
NSg
p < 0.001
p < 0.05
p < 0.001
p < 0.001
p < 0.001
p < 0.001
11,118 3,454
15,219 5,572c
528 50d
547 95c
550 54b,e
599 97b,f
550 54b,e
599 97b,f
p-value
18,704 4,313
18,129 3,515c
584 77c
703 109c
470 63b
470 63b
504 80c
504 80c
p < 0.001
NSg
p < 0.004
p < 0.05
p < 0.001
p < 0.001
NSg
p < 0.001
Units of density are cells/mm3 for Erie and colleagues44 and cells/mm2 for all other authors
Only lens wearers
c
Only non-lens wearers
d
Mixture of lens wearers and non-lens wearers
e
Moderate keratoconus
f
Advanced keratoconus
g
Not significant (p > 0.05)
b
Table 2. Keratocyte densitiesa in patients with keratoconus reported by various authors
P = 0.005) but not PKD. Post hoc analysis
revealed that atopy (p = 0.009), a history
of eye rubbing (p = 0.006) and corneal
staining (p = 0.035) were each significantly associated with AKD. Contact lens
wear, race and the presence of a scar were
unrelated to AKD or PKD.
Erie and associates44 measured KD in
four groups: lens-wearing and nonlens-wearing keratoconic patients and
lens-wearing and non-lens-wearing nonkeratoconic control subjects. Among
those who did not wear contact lenses, no
difference in AKD and PKD was found
between keratoconic patients and nonkeratoconic control subjects. Among contact lens wearers, AKD and PKD were
found 31 and 41 per cent lower in keratoconic patients compared with nonkeratoconic control subjects, respectively.
These authors concluded that KD is normal in keratoconic patients but keratocyte
loss is somehow exacerbated by lens wear.
As Erie and associates44 excluded patients
with severe keratoconus from their study,
interpretation of their results must be
confined to changes that occur in mild to
moderate keratoconus.
In the study of Uakhan and colleagues,25 only non-lens wearing keratoconic and control subjects were
examined. These authors found AKD and
PKD to be 19 and 22 per cent lower than
in controls, respectively. Although this
finding contradicts that of Erie and associates,38 who found no difference in AKD
or PKD between non-lens-wearing keratoconic and control subjects, it should be
noted that the keratoconic patients in the
experiment of Uakhan and colleagues25
were not confined to those with mild to
moderate disease. In fact, 54 per cent of
their experimental group were classified
as having severe keratoconus. Uakhan
and colleagues25 did not explain how
their patients with severe keratoconus
managed to see, given that they apparently were not corrected with rigid contact lenses or any other form of contact
lenses. Considered together, the findings
of Erie and associates38 and Uakhan and
colleagues25 suggest that keratocyte loss in
keratoconus may be related to disease
severity.
Weed and associates26 assessed patients
with moderate and advanced keratoconus
who wore contact lenses and found significantly higher KD compared with nonlens-wearing control subjects. Specifically,
AKD was 14 per cent higher in patients
displaying moderate keratoconus, and
AKD and PKD were 20 and 16 per cent
2007 The Authors
Journal compilation 2007 Optometrists Association Australia
higher in patients with advanced keratoconus. Compared with lens-wearing control
subjects, AKD and PKD were 31 and 15
per cent higher in patients displaying
moderate keratoconus, and 36 and 22 per
cent higher in patients with advanced
keratoconus. The findings of Weed and
associates26 of higher KD in keratoconic
patients directly contradict those of the
MKS1720 of a lower KD in keratoconic
patients.
In view of the different approaches outlined above in determining KD in keratoconic patients, it is difficult to reconcile
the results of these works. Three of the
four papers that addressed this issue19,25,44
indicate a lower KD in keratoconus but
the extent to which these changes reflect
the effects of lens wear versus the underlying pathological changes in keratoconus
remains unclear. One possibility, suggested by Kallinikos and Efron49 is that
changes in KD may be a function of lateral
cell migration and redistribution as well
as, or instead of, cellular apoptosis. A
combination of these phenomena could
explain both increases and decreases in
KD.
The original ideaconceived half a
century ago by Chi, Katzin and Teng13,33
that the earliest ultrastructural changes in
Clinical and Experimental Optometry 91.1 January 2008
43
Corneal confocal microscopy of keratoconus Efron and Hollingsworth
Epithelium
Stroma
Receptor for
Interleukin-1
Keratocyte
Endothelium
Epithelial trauma
Interleukin-1 B
Normal cornea
Keratoconus
Figure 11. Theory of keratocyte apoptosis in keratoconus. Left: The normal cornea. Keratocytes have receptors for Interleukin-1.
Right: The keratoconic cornea.
A. Keratocytes have four times as many receptors for Interleukin-1 as a normal cornea
B. Epithelial trauma causes a release of Interleukin-1, which floods the cornea
C. Most of the Interleukin-1 has left the cornea, but some remains bound to receptors
D. Interleukin-1 bound to the receptors induces keratocyte dysgenesis and apoptosis
keratoconus occur at the epithelial basement membrane, has been extended
recently by Wilson and colleagues,45 who
suggest that epithelial damage causes a
reduction in AKD through apoptosis. This
is thought to be triggered by cytokines
(including interleukin 1 and Fas-ligand)
released from the damaged epithelial
cells.51 An increased number of anterior
keratocytes exhibit signs of apoptosis in
the keratoconic cornea when compared to
normal corneas and corneas suffering
from other diseases.52 It has also been
shown that the keratocytes within the keratoconic cornea have four times as many
receptors for interleukin 1, potentially
sensitising them to this cytokine.53 CM
reports of reduced AKD in keratoconus19,25,44 and the LM observations
from the MKS1720 are consistent with the
notion that keratocyte apoptosis induced
by epithelial damage is one of the mechanisms responsible for the reduction in
AKD in keratoconus (Figure 11). The clinical evidence of this is the presence of significant corneal fluorescein staining in
keratoconic patients as observed in the
MKS.1720
Clinical and Experimental Optometry 91.1 January 2008
44
Confocal versus light microscopy
1720
In the MKS,
hyper-reflective keratocyte
nuclei and stromal haze were apparent
when examining CM images of the cornea
of Patient B (Figure 12). Evaluation of the
serial step sections prepared for LM
revealed the presence of disorganised tissue, confirming the SLB appearance of
apical scarring in this patient. The scarred
region measured approximately 220 m at
its widest point. Accurate measurement of
hyper-reflective regions in CM images was
not possible as there was no defined border, however, the size of the regions of
hyper-reflectivity observed with the CM
was roughly consistent with measurements
of the scar taken from the histological
samples.
Examination of tissue sections from the
cornea of Patient B at higher magnification revealed a dense accumulation of
fibroblasts in the region of the scar. Nuclei
were rounded and more irregular in
shape compared to the elongated, flattened appearance of normal keratocyte
nuclei.5,6 The extra-cellular matrix was
highly irregular compared to the nonscarred peripheral area of the same cor-
nea. Some of the images obtained from
CM of Patient B contained a mixture of
hyper-reflectivity and evidence of epithelial nuclei and are thought to represent
images taken from near the apex of the
scar.
Previous ultrastructural studies have
shown the keratoconic stroma to be distorted in regions where there are breaks
in Bowmans layer.16,35,54 Fibrillar degeneration and fibroblastic accumulation have
been demonstrated in the stroma beneath
these breaks.33 Keratocyte morphology has
also been shown to be abnormal in the
keratoconic eye.13 These observations are
consistent with CM observations in the
MKS1720 of significant abnormalities of
keratocyte nuclei, stromal haze and
hyper-reflectivity. Hyper-reflective keratocyte nuclei probably represent fibroblasts
as observed with the LM.
Research into the wound-healing
response of the stroma has revealed the
presence of hyper-reflective keratocyte
nuclei. These have been referred to as
activated keratocytes, that is, keratocytes
activated to a repair phenotype (or fibroblasts). Using rabbit corneas, Mller 2007 The Authors
Journal compilation 2007 Optometrists Association Australia
Corneal confocal microscopy of keratoconus Efron and Hollingsworth
Keratoconus
A
partly responsible for the transparency of
the cornea.59 Mller-Pedersen and colleagues55 suggested that the deposition of a
new extra-cellular matrix may also contribute to corneal haze following photorefractive keratectomy.
Stromal nerves
Normal cornea
Normal keratocyte nuclei
Figure 12
A. CM image of hyper-reflective and distorted keratocyte nuclei in Patient B, possibly
representing activated fibroblasts.
B. CM image of keratocyte nuclei in a normal control subject
C. LM of anterior stroma of Patient B. The box indicates a region of distorted keratocyte
nuclei. Normal keratocytes are present below this region (40 objective).
Pedersen and co-workers55 showed that the
haze apparent on CM following photorefractive keratectomy was due to the
increased reflectivity of migrating and activated keratocytes. Similar findings have
been documented in humans. In the early
stages of keratocyte activation, the nuclei
become more apparent. A more extreme
wound-healing response results in the cell
bodies becoming visible.56 Transmission
electron microscopy has shown that these
hyper-reflective cells represent keratocytes
activated to a repair phenotype.57 The
MKS1720 demonstrated what appears to be
activation of keratocytes in association
with apical scarring in the keratoconic eye.
The apparent association between stromal
haze and the appearance of activated keratocytes suggests that keratocyte hyperreflectivity may serve as a useful marker of
disease progression in longitudinal studies
of keratoconus, which could be monitored
in vivo using CM.
The extreme levels of stromal haze
observed with the CM cannot be attributed solely to an accumulation of fibroblasts. Keratocytes are known to be
responsible for the production of the
extracellular matrix and in turn, this
affects the arrangement of collagen within
the corneal stroma. LM of the cornea of
Patient B revealed the presence of abnormal collagenous tissue surrounding fibroblasts. Studies using X-ray diffraction have
shown that the normal arrangement of
collagen fibres is severely disrupted in
scarred regions of the keratoconic eye.58
This is clearly demonstrated by the histological investigations performed in the
MKS.1720 The irregular arrangement of
this tissue will contribute significantly to
the resulting stromal haze observed using
CM as the normal lattice arrangement of
the collagen fibres is disrupted. Regular
arrangement of the collagen fibres
within the corneal stroma is known to be
2007 The Authors
Journal compilation 2007 Optometrists Association Australia
Simo Mannion, Tromans and ODonnell60
investigated stromal nerve morphology
and corneal sensitivity in 13 patients with
keratoconus and 13 age-matched control
subjects, using in vivo CM and noncontact (air puff) corneal aesthesiometry. Stromal nerve fibre density was found
to be significantly lower in keratoconic
patients (1,018 490 m) versus control
subjects (1,821 790 m) (p = 0.006). The
mean diameter of stromal nerve fibres
was found to be greater in patients with
keratoconus (10.2 4.6 m) compared to
control subjects (5.5 1.9 m) (p = 0.007).
The orientation of stromal nerve fibres in
the patients with keratoconus appeared
to be altered from the predominantly
vertical orientation seen in control
subjects.
Corneal touch threshold was similar in
the two groups, although corneal sensitivity in patients with keratoconus using contact lens corrections (1.18 0.19 g/mm2)
was reduced (that is, the air puff pressure needed to be higher to elicit a
sensation) compared to the contact lenswearing control subjects (0.98 0.05 g/
mm2) (p = 0.03). Simmo Mannion and
colleagues60 concluded that there is a
significant reduction in stromal nerve
density in the keratoconic cornea, the
reduced stromal nerve density is a cause
of the reduced corneal sensitivity in keratoconic contact lens wearers and the thickened stromal nerve fibres observed in
keratoconic corneas may explain why
prominent stromal nerves are often seen
using SLB in such patients.61
Corneal nerves may play an active role
in the degenerative changes that occur in
keratoconus, by facilitating keratocyteepithelial interactions. Brookes and
associates62 observed nuclei of aberrant
anterior keratocytes wrapping around
nerves as they passed through the otherwise acellular Bowmans layer from the
Clinical and Experimental Optometry 91.1 January 2008
45
Corneal confocal microscopy of keratoconus Efron and Hollingsworth
stroma to the epithelium. As the keratoconus progressed and Bowmans layer
degraded, these keratocytes were seen to
express higher levels of the lysosomal
enzymes cathepsin B and G and to
become displaced anteriorly into the epithelium. Localised nerve thickening also
developed within the epithelium in association with cathepsin B and G expression
and appeared to be destructive to the cornea. Specifically, the authors noted that
enzyme activity by keratocytes seemed to
be causing localised structural degradation of the anterior stroma, leading to
near-complete destruction of both Bowmans layer and the stroma. Observations
of apparent intermixing of epithelial cells,
keratocytes from the anterior stroma and
nerve fibres within split sections of Bowmans layer made in the MKS1720 using
CM and LM, support the keratocyteepithelial interaction theory of Brookes
and associates.62
Striae
Alternating dark and light bands were
observed with CM in the stromal images
of 45 per cent of keratoconic eyes examined in the MKS.1720 The bands corresponded with the appearance of Vogts
striae on SLB examination. Figure 13A
shows a SLB image of striae visible
in a keratoconic patient. When magnified, the image of the striae taken with
the SLB (Figure 13B) is strikingly similar
to the CM image of bands in the posterior stroma of a keratoconic patient
(Figure 13C).
Bands observed with the CM were most
commonly in the posterior stroma. Posterior bands varied in width, ran mainly in
a near vertical direction and appeared to
run a straight course through individual
image frames. Keratocyte nuclei were
located in between the bands but their
distribution appeared unaffected by the
presence of bands. Nerve fibres appeared
to run a straight course through the
bands. When present, bands in the anterior stroma showed greater variability in
width and direction within a single
frame. Bands were present only in the
anterior stroma in more severe levels of
keratoconus. No obvious correlate of
Clinical and Experimental Optometry 91.1 January 2008
46
Figure 13
A. SLB image of a keratoconic cornea, with striae visible in the optic section
B. Magnified image of the striae shown in (A)
C. CM image of bands in the posterior stroma of a patient with keratoconus
banding could be observed with the LM
(Figure 14).
Uakhan and colleagues25 observed
folds, which they referred to as Vogts
striae, in 50 per cent of the keratoconic
eyes they examined. Folds were seen in the
anterior stroma in 21 eyes (44 per cent),
in the mid-stroma in 21 eyes (44 per cent)
and in the posterior stroma in 24 eyes (50
per cent). Interestingly, their description
of stromal folds as representing crests and
troughs suggests that they believe folds to
have a three-dimensional construct. For
example, Uakhan and colleagues25 stated
that keratocyte nuclei were visible only
over the light bands, which they called
crests, and were not seen on longitudinal
dark bands, which they believed corresponded to troughs. Posterior stromal
folds were observed in 14 eyes with severe
keratoconus, eight eyes with moderate
keratoconus and two eyes with mild keratoconus. In the earlier studies of Wygledowska-Promienska and associates24 and
Somodi and colleagues,23 folds were
observed only in the posterior stroma.
The images obtained in the MKS1720
suggest that the stromal bands seen
with the CM represent collagen lamellae
under stress rather than folds. Komai
and Ushiki63 demonstrated a differential
arrangement of collagen lamellae in the
anterior and posterior corneal stroma.
Anterior lamellae are 0.5 to 30 m wide,
they have a flat tape-like shape, run in
random directions and are often intertwined. The lamellae of the posterior
stroma are wider (100 to 200 m) and
have the appearance of broad sheets.63
The CM images obtained of bands in
the anterior and posterior stroma show
a similar pattern to those described
by Komai and Ushiki.63 Anterior stromal
bands are narrower and irregularly spaced.
A tape-like shape was observed in some
patients. The pattern of banding varied in
sequential frames. Bands in the posterior
stroma were wider, regularly spaced and
often consistent in direction in several
sequential frames. If clinically observed
Vogts striae represented folds (rather
than lines of stress), then their appearance
2007 The Authors
Journal compilation 2007 Optometrists Association Australia
Corneal confocal microscopy of keratoconus Efron and Hollingsworth
Anterior stroma
Mid stroma
Posterior stroma
Figure 14. Bands observed with CM in keratoconus
A. Bands of varying width in the anterior stroma, running orthogonally at approximately
90 degrees and 180 degrees
B. Fine vertical bands in the anterior stroma. A bifurcating nerve fibre and keratocytes
are visible.
C. Vertically oriented bands in the mid-stroma
D. Vertically oriented bands in the mid-stroma with faint horizontal banding
E. Bands in the posterior stroma, with a nerve fibre crossing horizontally. Keratocytes
are visible only between the dark bands.
F. Widely-spaced dark bands in the posterior stroma
on CM would not be expected to be
related to the pattern of collagen lamellae.
The transparency of the corneal stroma
in the normal eye is, in part, due to the
regular and precise arrangement of the
collagen fibrils. Maurice59 demonstrated
that for the corneal stroma to be transparent, it is necessary that fibrils are parallel,
equal in diameter and have their axes disposed in a regular lattice formation. This
regular arrangement results in mutual
interference of the light rays leading to
minimal light scattering.59 This effect is
likely to be greatest at the posterior
stroma, as a result of the more regular
fibril arrangement found posteriorly.64
The banded appearance of the stroma
observed on CM in keratoconic patients
may represent a widespread, irregular
separation of individual collagen fibrils
within the lamellae. Indeed, a number
of authors6567 has demonstrated marked
abnormalities in the organisation of the
anterior corneal collagen lamellae of
keratoconic corneas.
Disruption to the arrangement of collagen lamellae at any level of the stroma
will cause light to be refracted differently,
thereby having an effect on the mutual
interference of light rays passing through
the corneal stroma. The CM images containing stromal bands demonstrate variations in contrast, presumably due to the
disrupted arrangement and irregular separation of the collagen fibrils. CM images
of stromal bands in keratoconus do not
have the uniformity of images obtained of
collagen fibrils in the normal cornea.58,65
Both of these findings indicate significant
alterations of the collagen fibre arrangement in the keratoconic eye. This may be
partly responsible for the reduced vision
in keratoconic patients.
Tripathi and Bron68 described the
appearance of a secondary mosaic in the
cornea, the structural basis of which lies in
the particular arrangement of many prominent collagen lamellae of the anterior
stroma that take an oblique course to gain
insertion into Bowmans layer. This can
2007 The Authors
Journal compilation 2007 Optometrists Association Australia
not be seen in the normal eye because
Bowmans layer is under tension due to
intraocular pressure. However, Dangel
and Kracher69 observed the mosaic pattern in 75 per cent of eyes of keratoconic
patients wearing rigid lenses versus five
per cent of non-keratoconic rigid lens
wearers. These observations introduce the
possibility that the disarrangement of the
collagen network in the keratoconic eye
somehow facilitates the appearance of a
mosaic pattern when the cornea is stressed
by the pressure of a rigid lens. Thus, the
appearance of dark bands in keratoconic
patients in the MKS (50 per cent of whom
were wearing rigid lenses) may be, at least
in part, a manifestation of this mosaic
formation.
The direction of the bands in the posterior stroma was found to correlate well
with the steepest Sim-K axis of the cornea
as determined by corneal topography.18
Therefore, it seems probable that the orientation of the bands is due to a pattern
of stress in the collagen lamellae emerging
from the apex of the cone. By way of example, consider Figure 15A, which is a schematic representation of a presumed stress
pattern, templated on top of a topographical map of a keratoconic cornea, which
may emanate from the apex of an inferonasally located cone.
If the objective lens of the CM were to
be positioned for examination of the central cornea, an area superior and slightly
temporal to the cone apex would be examined (Figure 15A, red box). Stress lines
would run through the field of view at
about 80 degrees (using conventional
ophthalmic lens axis notation). This
would result in dark banding as shown in
Figure 15B. If the objective lens of the CM
were to be positioned for examination of
the apex of the cone (Figure 15A, blue
box), stress lines might be seen running
through the field of view at a variety of
angles. This would result in dark banding
as shown in Figure 15C.
The orientation of banding in the stromal images of keratoconic patients observed in CM images captured from the
central cornea are consistent with this
schematic model. In many patients, the
cones were located inferiorly to the cenClinical and Experimental Optometry 91.1 January 2008
47
Corneal confocal microscopy of keratoconus Efron and Hollingsworth
Nasal
Temporal
Figure 15. Model to illustrate the stress pattern theory of stromal banding observed in
keratoconus
A. Topographic map of a keratoconic cornea, with stress lines emanating from the apex
of the cone. The red box indicates the region of central cornea and the blue box the
region of the cone, imaged with the CM.
B. Expected CM image of the central cornea, with predominantly vertically oriented
bands corresponding to stress lines running in that direction
C. Expected CM image of the cone, with bands running in all directions
tre of the cornea and the banding was
near-vertical. The findings for the patient with a centrally located cone are also
consistent with this theory. This patient
displayed highly irregular posterior banding, namely, faint bands were apparent
horizontally in addition to more prominent vertically orientated bands. This
mixed banding pattern indicates that the
stress in the cornea corresponds to the
apex of the centrally located cone. Further research would need to be undertaken, by way of imaging banding
patterns at various locations on keratoconic corneas, to test the hypothesis that
banding represents stress lines emanating
from the cone apex.
X-ray scattering has unambiguously
demonstrated that the majority of collagen fibrils in the central cornea adopt a
preferred orientation in the inferiorsuperior and nasal-temporal directions.70
If observations of banding (with the CM)
and striae (with the SLB) in the central
Clinical and Experimental Optometry 91.1 January 2008
48
cornea are related to the orientation of
collagen fibrils, then these formations
would be expected to be found horizontally as well as vertically. On examination
with CM in the MKS,1720 horizontal and
vertical bands were observed in the anterior stroma and predominantly vertical
striae were observed in the posterior
stroma. Vogts striae in the same patients
seemed to be predominantly oriented
vertically when viewed with the SLB.
Although the early literature71 suggests
that Vogts striae are primarily vertically
oriented when observed with the SLB,
more recent anecdotal SLB observations
of striae in keratoconus patients (Gavin
OCallaghan, personal communication)
indicate that striae can occur at any orientation (Figure 16). In addition, based on
their observations of photographic images
of striae captured from over 1,500 keratoconic patients, senior authors of the CLEK
study21 are of the opinion that striae in
keratoconus can occur at any angle (Karla
Zadnik, Joe Barr and Timothy Edrington,
personal communication).
Smolek and McCarey72,73 studied the
cohesive strength of corneal lamellae
across the cornea. Investigations of the
lamellae in the vertical meridian have
shown that the inferior cornea has the
least cohesive strength.73 Varying patterns
of cohesive strength were seen between
individuals but paired corneas often display the same strength profiles. Smolek73
reported a circumstantial correlation
between cohesive strength and the patterns seen in the different forms of corneal ectasia.
In keratoconus, the cone is most often
located inferiorly or centrally,74 corresponding to the areas of reduced strength
found by Smolek.73 The appearance of
stromal banding in the MKS1720 may represent a stress-related change in corneal
lamellae, corresponding to areas of
reduced strength in the cornea and the
formation of an ectatic cone-like protrusion in that area. Examination of other
ectatic degenerations such as keratoglobus and pellucid marginal degeneration
may shed further light on this hypothesis
by revealing different patterns of banding
corresponding to regions of reduced
cohesive strength of stromal lamellae and
clinical evidence of ectasia.
Desemets membrane
No abnormalities were detected with the
CM at the level of Desemets membrane
in the MKS;1720 however, WygledowskaPromienska and associates24 observed central detachment of the Desemets membrane and the endothelium from the
stroma in advanced keratoconus. Uakhan and colleagues25 observed folds at
the level of Desemets membrane in eight
per cent of keratoconic eyes.
Using LM, Chi, Katzin and Teng33
observed folds and buckling at the level of
Desemets membrane in the later stages
of keratoconus and ruptures were observed in Desemets membrane in 12
per cent of corneas. These defects were
filled first with endothelial cells and later
with a newly formed membrane. Ruptures
in Desemets membrane are thought to
be associated with previous cases of cor 2007 The Authors
Journal compilation 2007 Optometrists Association Australia
Corneal confocal microscopy of keratoconus Efron and Hollingsworth
Figure 16. SLB photographs from patients with keratoconus
A. Oblique or Y-shaped striae (arrow)
B. Horizontal striae (arrows) (Photograph courtesy Gavin OCallaghan)
Keratoconus
Normal cornea
Figure 17
A. Elongated endothelial cells in the inferior right field of a CM image of a patient with
keratoconus
B. CM image of normal endothelium in a control subject
neal hydrops. That Desemets membrane was normal in the MKS1720 is not
surprising in view of the absence of a previous history of hydrops in any of the
patients.
Endothelium
The endothelial images obtained from
one patient in the MKS1720 displayed evidence of elongated cells (Figure 17). This
appearance was verified by a masked inde-
pendent observer who was experienced in
evaluating CM images. The region of the
stroma anterior to these elongated cells
and the remainder of the field of the
endothelium adjacent to the elongated
cells appeared normal. There was no evidence of elongated endothelial cells in
any other patient examined with the CM.
The mean endothelial cell density
(ECD) in keratoconus was six per cent
greater than that of normal controls.
2007 The Authors
Journal compilation 2007 Optometrists Association Australia
Many of the endothelial images seemed to
display a large number of smaller cells
with only scattered large cells, however,
there was no difference in endothelial
polymegethism between keratoconic patients (0.35 0.05) and control subjects
(0.38 0.07) (paired t-test: t = 1.8, p =
0.08).
Pleomorphism and enlarged endothelial cells were seen in 13 per cent of eyes
with severe keratoconus by Uakhan and
colleagues.25 In one (two per cent) eye
with severe keratoconus with no identifiable history of acute hydrops, folds in
Desemets membrane and endothelial
guttata were observed. These authors
found no difference in mean ECD or
mean endothelial cell area between keratoconic patients and controls. In eyes
with severe keratoconus, the mean ECD
was lower than in eyes with moderate
(p < 0.05) or mild (p < 0.05) keratoconus
and the mean endothelial cell area was
higher than in eyes with mild keratoconus
(p < 0.05). The mean endothelial cell hexagonality was lower in keratoconic eyes
(p < 0.05). Weed and associates26 found
no difference in ECD between keratoconic patients and control subjects.
With three different studies indicating
either increased,19 decreased25 or normal26
ECD and either decreased or normal polymegethism in keratoconus, our understanding of the true state of the corneal
endothelium in keratoconus remains
uncertain. A summary of ECD in keratoconic patients as measured by various
authors is presented in Table 3.
Early studies with specular microscopy
showed that there is a significant increase
in the amount of pleomorphism and polymegethism in the keratoconic eye75,76
however, these studies did not disclose
whether the patients examined wore contact lenses. Halibis77 has shown that the
level of polymegethism and pleomorphism in keratoconic patients is similar to
that of lens-wearing controls. This finding
is consistent with those of the MKS.1720
Hoffer and Kraff78 investigated the
endothelium in a large series of normal
eyes using specular microscopy and found
that ECD was significantly higher in eyes
with a longer axial length. Using the same
Clinical and Experimental Optometry 91.1 January 2008
49
Corneal confocal microscopy of keratoconus Efron and Hollingsworth
technique, Esgin and Erda79 demonstrated an increase in central ECD following wear of high oxygen transmissible
rigid lenses. In the majority of cases, myopia and rigid lens-wear are features of
keratoconus. This may account for the
increased ECD found in the MKS.1720
In the MKS,1720 the endothelial cells of
the cornea of Patient B appeared normal
when viewed with LM (Figure 18). It was
not possible to correlate these findings
against those from CM as the endothelium
of Patient B was obscured by high levels of
haze in the anterior cornea.
In the early stages of keratoconus, the
endothelium has a normal appearance
when viewed with the LM.33 In more
advanced cases, it shows flattening and
the nuclei are further apart.33 Specular
microscopy has revealed an increase in
pleomorphism and also a high proportion
of small endothelial cells in keratoconus.75
Large elongated cells were also apparent
adjacent to the cone, with the long axis of
these cells oriented towards the cone
apex.75 Such observations are consistent
with the notion that corneal tissue is being
stretched as a result of ectasia. In the
MKS,1720 evidence of endothelial cell
elongation was observed in only one
patient. The lack of cellular elongation in
the majority of the study group may be
attributed to the fact that the central cornea (thus typically not the centre of the
cone) was imaged in all patients.
LM of the endothelium of Patients A
and B showed the cells of this layer to be
normal in appearance. Endothelial cell
degeneration has been reported in corneas with more severe levels of keratoconus, with the damage being more prevalent at the base of the cone rather than at
the apex.15 These changes were not
observed with the CM in the MKS,1720
probably due to the fact that only the central cornea was investigated and the endothelium beneath the cone was often obscured by haze and scarring.
KERATOCONUS AND CONCURRENT
CORNEAL DISEASE
The CM has been used to examine cases
of disease that have occurred in the corClinical and Experimental Optometry 91.1 January 2008
50
Author
Year
Keratoconus
Control
p-value
Hollingsworth, Efron and Tullo19
Uakhan and colleagues25
Weed and associates26
2005
2006
2007
3,250 352b
2,754 312c
2,888 380d,e
2,941 464d,f
3,056 365c
2,900 354c
3,043 264c
3,043 264c
p < 0.05
NSg
NSg
NSg
Units of density are cells/mm2
Mixture of lens wearers and non-lens wearers
c
Only non-lens wearers
d
Only lens wearers
e
Moderate keratoconus
f
Advanced keratoconus
g
Not significant (p > 0.05)
Table 3. Endothelial cell densitiesa in patients with keratoconus reported by various
authors
Endothelial cell nuclei
Figure 18
A. LM section of the cornea of Patient B (10 objective)
B. Enlarged LM image of the endothelium of Patient B (20 objective). Arrows indicate
nuclei of endothelial cells.
nea of keratoconic patients. Such studies are important because they can
provide unique insights into the keratoconic cornea by revealing how this tissue
responds to the stress of additional
pathology.
Acute hydrops
Grupcheva and associates80 reported the
case of a Caucasian man with a history of
keratoconus since teenage years. He presented with unusual bilateral keratoconus
with acute hydrops that had developed
2007 The Authors
Journal compilation 2007 Optometrists Association Australia
Corneal confocal microscopy of keratoconus Efron and Hollingsworth
over a three- to four-month period. The
patient had no previous history of contact
lens wear.
At the time of examination, the patient
presented with spectacle visual acuity of
6/60 in both eyes. Typical conical deformation of each cornea was evident with
the SLB, with well-circumscribed oedema
at the apex of the cone, which was slightly
more prominent in the cornea of the right
eye. No other pathology was highlighted
on clinical examination. Orbscan topography could not be performed as a result of
decreased corneal transparency. Accurate
intraocular pressure measurement was not
possible.
Anterior stromal oedema was observed,
with marked subepithelial bullae and folds
in Desemets membrane. Corneal scarring was present only anteriorly at the
level of Bowmans layer. These in vivo CM
findings confirmed the diagnosis of keratoconus with a less common bilateral presentation of acute hydrops.
Epidemic keratoconjunctivitis
Alsuhaibani, Sutphin and Wagoner81
reported the case of a 14-year-old Saudi
girl with keratoconus who developed
sub-epithelial infiltrates after the onset
of bilateral epidemic keratoconjunctivitis.
CM of the left cornea, conducted eight
weeks after the onset of the infection,
showed many highly reflective dendritic
cells at the level of the basal epithelium
and anterior stroma. Many highly reflective fusiform and round cells were
observed within the anterior stroma, with
decreasing density in progressively deeper
layers of the stroma. These findings were
not present on CM that had been performed two weeks before the onset of
epidemic keratoconjunctivitis. In this case,
CM examination provided clear evidence
of an inflammatory response localised to
the basal epithelium and anterior stroma
of the central cornea.
MEDICAL AND SURGICAL
INTERVENTIONS IN KERATOCONUS
A number of medical and surgical approaches can be applied to the treatment of keratoconus. The CM facilitates
investigation of the efficacy of these treatments in uncomplicated cases and allows
adverse reactions to be studied at a cellular level.
Riboflavin-UVA-induced collagen
cross-linking
Wollensak, Spoerl and Seiler82 have
described the technique of riboflavin/
ultraviolet A (UVA)-induced collagen
cross-linking, which is designed to bring
the progression of keratoconus to a
halt. The underlying theory is that
there will be an increase in corneal biomechanical stiffness due to enhanced
collagen crosslinking as a result of the
treatment.
Mazzotta and colleagues83 assessed corneal tissue modifications using this treatment in a group of 10 patients with
progressive keratoconus, as well as regeneration of the epithelium and subepithelial nerve plexus, using the HRT II CM.
Treatment included instillation of a 0.1%
riboflavin/20% dextran solution five minutes before UVA irradiation and every five
minutes for a total of 30 minutes thereafter. A dual UVA (370 nm) light-emitting
diode was used to generate radiant energy
of 5.4 Joule/cm2. The protocol included
the operation followed by antibiotic medication and eye dressing with a soft therapeutic contact lens.
After five days of soft contact lens wear,
the corneal epithelium displayed a regular morphology and density with CM. Disappearance of subepithelial stromal
nerve fibres was observed in the central
irradiated area where initial reinnervation was observed microscopically one
month after the operation. No changes in
nerve fibres were observed in the peripheral untreated cornea, with a clear lateral
transition between the two areas. Six
months after the operation, the anterior
subepithelial stroma was recolonised by
nerve fibres with restoration of corneal
sensitivity.83
A similar pattern of disappearance and
regeneration of keratocytes was observed
using CM.84 A reduction in KD in the anterior and intermediate stroma and stromal
oedema, was observed immediately after
treatment. Keratocytes were observed to
2007 The Authors
Journal compilation 2007 Optometrists Association Australia
repopulate the central cornea three
months after the operation and the
oedema had disappeared. At six months
post-operatively, keratocyte repopulation
was complete. No endothelial damage was
observed at any time.
Intrastromal corneal ring implants
Intrastromal corneal ring implants are
corneal inlays made of plastic, with an arc
length of 150 degrees, which are used for
the correction of low to moderate myopia.
The outward radial tension of these rings
leads to a reduction in curvature of the
cornea and a normalisation of corneal
topography, resulting in reduced myopia,
less optical aberration and improved
vision. More recent developments of this
technique include short arc length segments (130 degrees) for the correction of
myopia concurrent with astigmatism and
radially-placed corneal inlays for the correction of hyperopia.
Ruckhofer and colleagues85 used CM
to examine the corneas of a series of
keratoconic patients who had implants
inserted at a single surgical centre.
Weeks and months after implantation,
lamellar channel deposits regularly
appeared around the segments. This
material was thought to consist of intracellular lipids.
Kymionis and associates86 examined 17
eyes of 15 patients with keratoconus aged
24 to 52 years (mean: 34 11 years), who
had completed five years after insertion of
two intrastromal segments of 0.45 mm
thickness in the cornea of each eye. When
examined using CM, most patients exhibited normal central corneal morphology
in all layers, with normal epithelial cells,
subepithelial nerve plexus, keratocyte distribution and endothelial morphology.
Needle-shaped keratocytes and tortuous
sub-basal nerves were observed within the
stroma in one patient. Microdeposits,
stretched keratocytes and mild fibrosis
were observed at or close to the anterior
channel of all patients. At the plane of
the implant, oval-shaped deposits were
observed along the channel. One patient
exhibited increased fibrosis or collagen
disruption a few microns away from the
ring segment.
Clinical and Experimental Optometry 91.1 January 2008
51
Corneal confocal microscopy of keratoconus Efron and Hollingsworth
Epikeratophakia
87
Shi and colleagues used CM to study
24 cases of keratoconus from three days
to five years after epikeratophakia. The
tissue lens was observed to be covered
by apparently flattened superficial corneal epithelial cells three to four days
post-operatively. Epithelial wing and
basal cells were also observed but the
morphology and arrangement of these
cells were irregular with low cell density.
The superficial flat epithelial cells appeared normal at one month and the
morphology and density of the basal epithelial cells tended to be normal at six
months post-operatively. The subepithelial nerve plexus appeared irregular at
18 months but appeared normal two
years post-surgery.
In the stroma of the tissue lens, keratocytes appeared circular, dot-shaped, rodshaped or reticular. A few normal keratocytes were observed at the periphery of the
tissue lens two years post-operatively. At
five years, KD in the periphery remained
lower than that in the centre of the tissue
lens. Stromal nerves appeared in the tissue
lens six months after surgery and the quantity of nerves had increased after two years
but was still less than normal after five
years. There was no change in the stroma
and endothelium of the recipient cornea.
Penetrating keratoplasty
A longitudinal evaluation of four patients
who had undergone penetrating keratoplasty was undertaken by Hollingsworth,
Efron and Tullo20 for 12 months after
surgery, using slit scanning CM. The procedure was preformed because of keratoconus (two patients), Fuchs dystrophy
and lattice dystrophy.
Patients were examined on four occasions over a 12-month period after surgery. The epithelium varied in appearance
between patients and took at least 12
months to appear normal. Bowmans layer
was viewed as an acellular layer immediately after surgery with no evidence of
nerve fibres, although some nerve components were apparent 12 months after
surgery. Stromal nerves were not visible
immediately after surgery. One year following penetrating keratoplasty, there was
Clinical and Experimental Optometry 91.1 January 2008
52
evidence of thin nerves running a straight
course through the central stroma. AKD
and PKD were lower in the transplanted
cornea and appeared to remain constant
over a period of 12 months.
Activated keratocytes were seen in the
anterior stroma of all patients. They
appeared to be responsible for significant levels of corneal haze. The time
within which this keratocyte activation occurred varied between individuals. ECD
decreased at an accelerated rate over the
12-month period.
Imre, Resch and Nagymihaly88 examined seven eyes with clear grafts at 15 and
66 months after penetrating keratoplasty.
The preoperative diagnoses were keratoconus (two), granular corneal dystrophy
(two), pseudophakic bullous keratopathy
(two) and corneal ulcer (one). Mean density of basal epithelial cells was 3,928 378
cells/mm2 at 15 months and 3,284 565
cells/mm2 at 66 months post-operatively.
At 15 months, AKD and PKD were 750
113 and 601 98 cells/mm2, respectively, and at 66 months these measures
were 383 53 and 411 98 cells/mm2,
respectively. ECD decreased from 1719
576 cells/mm2 at 15 months to 965 272
cells/mm2 at 66 months. The results of
this study are consistent with the findings
of the MKS.1720 Both were longitudinal
evaluations and suggest that there is an
ongoing decline in the cellular integrity of
corneal grafts up to six years following
penetrating keratoplasty.
Niederer and colleagues89 conducted a
cross-sectional CM study comparing corneas from 42 patients after penetrating
keratoplasty with those of 30 controls.
Patients were assessed by ophthalmic
history, clinical examination and computerised corneal topography. Time after surgery ranged from one month to 40 years
(mean: 85 105 months). Significant
reductions in epithelial CD (p < 0.001),
KD (p < 0.001) and endothelial CD (p <
0.001) were noted in comparison with
control corneas. Significant reductions in
sub-basal nerve fibre density (p < 0.001)
and nerve branching (p < 0.001) were also
noted. ECD decreased (r = -0.472; p =
0.003) and nerve fibre density increased
(r = 0.328; p = 0.034) with time after
surgery. As an indication for transplantation, keratoconus was associated with
higher sub-basal nerve fibre densities (p =
0.003) than other indications for corneal
transplantation. Neither nerve fibre nor
cell density was correlated with visual acuity. The authors concluded that profound
reductions in cell density at every level of
the transplanted cornea and alterations to
the sub-basal plexus are apparent up to 40
years after penetrating keratoplasty.
Forseto Ados and associates90 reported
the case of a 36-year-old female patient
with keratoconus who suffered epithelial
in-growth after penetrating keratoplasty.
This patient had developed a welldelimited posterior hazy membrane covering the inferior two thirds of the cornea
three months after an uneventful penetrating keratoplasty. A posterior corneal
line was present resembling an endothelial graft rejection line but with no keratic
precipitates or corneal oedema. Ocular
hypertension was not observed. CM
showed the epithelium and stroma to be
normal. Two distinct cell types were presented at the endothelium layer. Enlarged
endothelial cells were observed in the
superior part of the cornea up to the leading edge of the hazy membrane. In the
middle and inferior part of the graft, the
cells were larger with polygonal shape and
easily recognisable hyper-reflective nuclei,
suggestive of epithelial cells. The patient
promptly received another penetrating
graft and histologic analysis confirmed the
diagnosis of epithelial in-growth.
CONCLUSIONS
This review has illustrated how the CM can
be used to identify and evaluate morphological alterations to the corneal epithelium, sub-basal nerve plexus, Bowmans
layer, stroma, Desemets membrane and
endothelium in keratoconus. The results
of morphometric analyses by various
authors are equivocal, so further studies
will be required to accurately determine
quantitative cellular characteristics of the
keratoconic cornea.
Pathological changes observed using
CM in the corneas of patients with keratoconus could serve as a basis for clinical
2007 The Authors
Journal compilation 2007 Optometrists Association Australia
Not reported.
Collagen fibres misaligned and irregularly thinned.
Fragmentation and breaks.
Breaks filled with epithelium, proliferated
collagenous tissue, keratoblasts, connective tissue.
Fibrillar degeneration and fibroblast accumulation
beneath breaks in Bowmans layer.
Abnormal morphology and activation of keratocytes.
Ruptures fill with endothelial cells and newly-formed
membrane.
Not reported.
Bilayer formation near scar.a
Fragmentation in region of scar.a
Irregular keratocyte nuclei within
bilayer space.a
Disorganised tissue.a
Dense accumulation of fibroblasts.a
Keratocyte nuclei more rounded
and irregular in shape.a
Folds, buckling and ruptures.a
Cell flattening and nuclei further
apart.a
Nerve fibre bundles follow the contour of the base
of the cone.
Bundles run concentrically.
Nerve fibres have a thickened, prominent appearance.
Epithelial cells and/or keratocytes sometimes visible.
Nerve fibres run in and out the field of view.
Increased level of haze.
Hyper-reflective patches.
Haze and hyper-reflectivity.
Keratocyte nuclei irregular shape and hyper-reflective.
Alternating light and dark bands.
Normal.
Limited evidence of elongated endothelial cells.
Hydrops in the
proximity of
Desemets
membrane.
Normal.
Desemets
membrane
Endothelium
Table 4. Appearance of corneal layers in keratoconus using various observational techniques
Vogts striae.
Scarring and haze.
Oedema.
Stroma
Journal compilation 2007 Optometrists Association Australia
Severe keratoconus.
Superficial scarring
and haze.
Bowmans
layer
2007 The Authors
Cannot be seen.
Sub-basal
nerve plexus
Endothelial cell degeneration.
Basal cells degenerate and disappear.
Epithelium becomes one or two layers of superficial
cells.
Abnormal basement membrane.
Overall thinning.a
Individual cells appear flattened.a
Columnar appearance of basal cells
is not apparent.a
Superficial cells: elongated or spindle-shaped. a
Wing cells: large, irregularly-spaced nuclei. a
Basal cells: hazy; irregular with visible nuclei. a
Fleischer ring.
Haze.
Epithelium
Corneal
Layer
Slitlamp
biomicroscopy
(in vitro)
Confocal microscopy
(in vitro)
Light microscopy
(in vitro)
Electron microscopy
(in vitro)
Corneal confocal microscopy of keratoconus Efron and Hollingsworth
decision-making. For example, it might be
possible to detect changes in epithelial
cell size or dark lines (striae) in the
stroma, very early in the disease process,
providing early detection for keratoconus.
The grading scale for stromal haze could
be adopted as a basis for classifying or
categorising the severity of keratoconus.
Evidence of splitting or substantial disruption to Bowmans layer could serve as a
criterion for undertaking penetrating
keratoplasty.
The appearance of the corneal layers in
keratoconus with the CM, compared with
that observed with the SLB, LM and electron microscopy, is summarised in Table 4.
CM images of keratoconic corneas in vivo
have also been correlated with images
obtained from in vitro samples of keratoconic corneas using the more established
technique of LM. This work provides a
framework against which cellular changes
in keratoconus can be studied using CM
in a clinical context.
CM has facilitated a greater understanding of medical and surgical approaches
that can be applied to the treatment of
keratoconus. The extent of tissue compromise can be assessed at a cellular level to
aid diagnosis and can be used to evaluate
the recovery process and the efficacy of
different treatment interventions.
REFERENCES
1. Rabinowitz YS. Keratoconus. Surv Ophthalmol 1998; 42: 297319.
2. Chopra I, Jain AK. Between eye asymmetry
in keratoconus in an Indian population.
Clin Exp Optom 2005; 88: 146152.
3. Haque S, Simpson T, Jones L. Corneal and
epithelial thickness in keratoconus: a comparison of ultrasonic pachymetry, Orbscan
II and optical coherence tomography. J
Refract Surg 2006; 22: 486493.
4. Patel DV, McGhee CN. Contemporary in
vivo confocal microscopy of the living
human cornea using white light and laser
scanning techniques: a major review. Clin
Exp Ophthalmol 2007; 35: 7188.
5. Efron N, Perez-Gomez I, Mutalib HA, Hollingsworth J. Confocal microscopy of the
normal human cornea. Contact Lens Ant Eye
2001; 24: 1624.
6. Hollingsworth J, Perez-Gomez I, Mutalib
HA, Efron N. A population study of the
normal cornea using an in vivo, slitscanning confocal microscope. Optom Vis
Sci 2001; 78: 706711.
Clinical and Experimental Optometry 91.1 January 2008
53
Corneal confocal microscopy of keratoconus Efron and Hollingsworth
7. Zhivov A, Stave J, Vollmar B, Guthoff R. In
vivo confocal microscopic evaluation of
Langerhans cell density and distribution in
the corneal epithelium of healthy volunteers and contact lens wearers. Cornea 2007;
26: 4754.
8. Patel DV, McGhee CN. Mapping of the normal human corneal sub-basal nerve plexus
by in vivo laser scanning confocal microscopy. Invest Ophthalmol Vis Sci 2005; 46:
44854488.
9. Bhnke M, Masters BR. Long-term contact
lens wear induces a corneal degeneration
with microdot deposits in the corneal
stroma. Ophthalmology 1997; 104: 1887
1896.
10. Parmar DN, Awwad ST, Petroll WM, Bowman RW, McCulley JP, Cavanagh HD. Tandem scanning confocal corneal microscopy
in the diagnosis of suspected acanthamoeba
keratitis. Ophthalmology 2006; 113: 538547.
11. Brasnu E, Bourcier T, Dupas B, Degorge S,
Rodallec T, Laroche L, Borderie V, Baudouin C. In vivo confocal microscopy in
fungal keratitis. Br J Ophthalmol 2006; 91:
588591.
12. Krachmer JH, Feder RS, Belin MW. Keratoconus and related noninflammatory corneal thinning disorders. Surv Ophthalmol
1984; 28: 293322.
13. Teng CC. Electron microscope study of the
pathology of keratoconus: I. Am J Ophthalmol 1963; 55: 1847.
14. Scroggs MW, Proia AD. Histopathological
variation in keratoconus. Cornea 1992; 11:
553559.
15. Sturbaum CW, Peiffer RL Jr. Pathology of
corneal endothelium in keratoconus. Ophthalmologica 1993; 206: 192208.
16. Sawaguchi S, Fukuchi T, Abe H, Kaiya T,
Sugar J, Yue BY. Three-dimensional scanning electron microscopic study of keratoconus corneas. Arch Ophthalmol 1998; 116:
6268.
17. Hollingsworth JG, Bonshek RE, Efron N.
Correlation of the appearance of the keratoconic cornea in vivo by confocal microscopy and in vitro by light microscopy. Cornea
2005; 24: 397405.
18. Hollingsworth JG, Efron N. Observations of
banding patterns (Vogt striae) in keratoconus: a confocal microscopy study. Cornea
2005; 24: 162166.
19. Hollingsworth JG, Efron N, Tullo AB. In
vivo corneal confocal microscopy in keratoconus. Ophthalmic Physiol Opt 2005; 25: 254
260.
20. Hollingsworth JG, Efron N, Tullo AB. A longitudinal case series investigating cellular
changes to the transplanted cornea using
confocal microscopy. Contact Lens Ant Eye
2006; 29: 135141.
21. Zadnik K, Barr JT, Gordon MO, Edrington
TB. Biomicroscopic signs and disease severity in keratoconus. Collaborative LongitudiClinical and Experimental Optometry 91.1 January 2008
54
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
nal Evaluation of Keratoconus (CLEK)
Study Group. Cornea 1996; 15: 139146.
Perez-Gomez I, Hollingsworth J, Efron N.
Effects of benoxinate hydrochloride 0.4%
on the morphological appearance of the
cornea using confocal microscopy. Contact
Lens Ant Eye 2004; 27: 4548.
Somodi S, Hahnel C, Slowik C, Richter A,
Weiss DG, Guthoff R. Confocal in vivo
microscopy and confocal laser-scanning fluorescence microscopy in keratoconus. Ger J
Ophthalmol 1996; 5: 518525.
Wygledowska-Promienska D, Rokita-Wala I,
Gierek-Ciaciura S, Piatek-Koronowska G.
The alterations in corneal structure at III/
IV stage of keratoconus by means of confocal microscopy and ultrasound biomicroscopy before penetrating keratoplasty. Klin
Oczna 1999; 101: 427432.
Uakhan OO, Kanpolat A, Ylmaz N, zkan
M. In vivo confocal microscopy findings in
keratoconus. Eye Contact Lens 2006; 32: 183
191.
Weed KH, Macewen CJ, Cox A, McGhee
CN. Quantitative analysis of corneal microstructure in keratoconus utilising in vivo
confocal microscopy. Eye 2007; 21: 614623.
Tsubota K, Mashima Y, Murata H, Sato N,
Ogata T. Corneal epithelium in keratoconus. Cornea 1995; 14: 7783.
Mocan MC, Irkec M. Fluorescein enhanced
confocal microscopy in vivo for the evaluation of corneal epithelium. Clin Experiment
Ophthalmol 2007; 35: 3843.
Rokita-Wala I, Gierek-Ciaciura S, Majlinger
R, Wygledowska-Promienska D. Iron deposits in cornea in confocal microscope. Klin
Oczna 2001; 103: 111115.
Scroggs MW, Proia AD. Histopathological
variation in keratoconus. Cornea 1992; 11:
553539.
Aktekin M, Sargon MF, Cakar P, Celik HH,
Firat E. Ultrastructure of the cornea epithelium in keratoconus. Okajimas Folia Anat Jpn
1998; 75: 4553.
Jongebloed WL, Worst JF. The keratoconus
epithelium studied by SEM. Doc Ophthalmol
1987; 67: 171181.
Chi HH, Katzin HM, Teng CC. Histopathology of keratoconus. Am J Ophthalmol 1956;
42: 847860.
Tsubota K. In vivo observation of the corneal epithelium. Scanning 1994; 16: 295
299.
Tsubota K, Yamada M, Naoi S. Specular
microscopic observation of human corneal
epithelial abnormalities. Ophthalmology
1991; 98: 184191.
Patel DV, McGhee CN. Mapping the corneal sub-basal nerve plexus in keratoconus
by in vivo laser scanning confocal microscopy. Invest Ophthalmol Vis Sci 2006; 47:
13481351.
Patel DV, McGhee CN. Contemporary in
vivo confocal microscopy of the living
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
51.
52.
human cornea using white light and laser
scanning techniques: a major review. Clin
Experiment Ophthalmol 2007; 35: 7188.
Szaflik JP. Comparison of in vivo confocal
microscopy of human cornea by white light
scanning slit and laser scanning systems.
Cornea 2007; 26: 438445.
Auran JD, Koester CJ, Rapaport R, Florakis
GJ. Wide field scanning slit in vivo confocal
microscopy of flattening-induced corneal
bands and ridges. Scanning 1994; 16: 182
186.
Kobayashi A, Yokogawa H, Sugiyama K. In
vivo laser confocal microscopy of Bowmans
layer of the cornea. Ophthalmology 2006;
113: 22032208.
Kaas-Hansen M. The histopathological
changes of keratoconus. Acta Ophthalmol
Scand 1993; 71: 411414.
Fini ME. Keratocyte and fibroblast phenotypes in the repairing cornea. Prog Retin Eye
Res 1999; 18: 529551.
Patel SV, McLaren JW, Hodge DO,
Bourne WM. Confocal microscopy in vivo
in corneas of long-term contact lens wearers. Invest Ophthalmol Vis Sci 2002; 43: 995
1003.
Erie JC, Patel SV, McLaren JW, Nau CB,
Hodge DO, Bourne WM. Keratocyte density in keratoconus. A confocal microscopy
study. Am J Ophthalmol 2002; 134: 689695.
Jalbert I, Stapleton F. Effect of lens wear on
corneal stroma: preliminary findings. Aust
NZ J Ophthalmol 1999; 27: 211213.
Efron N, Mutalib HA, Perez-Gomez I, Koh
HH. Confocal microscopic observations of
the human cornea following overnight contact lens wear. Clin Exp Optom 2002; 85: 149
155.
Efron N, Perez-Gomez I, Morgan PB. Confocal microscopic observations of stromal
keratocytes during extended contact lens
wear. Clin Exp Optom 2002; 85: 156160.
Kallinikos P, Morgan P, Efron N. Assessment of stromal keratocytes and tear film
inflammatory mediators during extended
wear of contact lenses. Cornea 2006; 25: 1
10.
Kallinikos P, Efron N. On the etiology of
keratocyte loss during contact lens wear.
Invest Ophthalmol Vis Sci 2004; 45: 30113020.
Hollingsworth JG, Efron N. Confocal
microscopy of the corneas of long-term
rigid contact lens wearers. Contact Lens Ant
Eye 2004; 27: 5764.
Wilson SE, He YG, Weng J, Li Q, McDowall
AW, Vital M, Chwang EL. Epithelial injury
induces keratocyte apoptosis: hypothesized
role for the interleukin-1 system in the
modulation of corneal tissue organization
and wound healing. Exp Eye Res 1996; 62:
325327.
Kim WJ, Rabinowitz YS, Meisler DM, Wilson
SE. Keratocyte apoptosis associated with
keratoconus. Exp Eye Res 1999; 69: 475481.
2007 The Authors
Journal compilation 2007 Optometrists Association Australia
Corneal confocal microscopy of keratoconus Efron and Hollingsworth
53. Fabre EJ, Bureau J, Pouliquen Y, Lorans G.
Binding sites for human interleukin 1
alpha, gamma interferon and tumor necrosis factor on cultured fibroblasts of normal
cornea and keratoconus. Curr Eye Res 1991;
10: 585592.
54. Tuori AJ, Virtanen I, Aine E, Kalluri R,
Miner JH, Uusitalo HM. The immunohistochemical composition of corneal basement membrane in keratoconus. Curr Eye
Res 1997; 16: 792801.
55. Mller-Pedersen T, Li HF, Petroll WM,
Cavanagh HD, Jester JV. Confocal microscopic characterization of wound repair
after photorefractive keratectomy. Invest
Ophthalmol Vis Sci 1998; 39: 487501.
56. Mller-Pedersen T, Cavanagh HD, Petroll
WM, Jester JV. Stromal wound healing
explains refractive instability and haze
development after photorefractive keratectomy: a 1-year confocal microscopic study.
Ophthalmology 2000; 107: 12351245.
57. Ohno K, Mitooka K, Nelson LR, Hodge
DO, Bourne WM. Keratocyte activation and
apoptosis in transplanted human corneas
in a xenograft model. Invest Ophthalmol Vis
Sci 2002; 43: 10251031.
58. Daxer A, Fratzl P. Collagen fibril orientation in the human corneal stroma and its
implication in keratoconus. Invest Ophthalmol Vis Sci 1997; 38: 121129.
59. Maurice DM. The structure and transparency of the cornea. J Physiol 1957; 136: 263
286.
60. Simo Mannion L, Tromans C, ODonnell
C. An evaluation of corneal nerve morphology and function in moderate keratoconus. Contact Lens Ant Eye 2005; 28: 185
192.
61. Simo Mannion L, Tromans C, ODonnell
C. Corneal nerve structure and function in
keratoconus: A case report. Eye Contact Lens
2007; 33: 106108.
62. Brookes NH, Loh IP, Clover GM, Poole CA,
Sherwin T. Involvement of corneal nerves
in the progression of keratoconus. Exp Eye
Res 2003; 77: 515524.
63. Komai Y, Ushiki T. The three-dimensional
organization of collagen fibrils in the
human cornea and sclera. Invest Ophthalmol
Vis Sci 1991; 32: 22442258.
64. Freund DE, McCally RL, Farrell RA, Cristol
SM, LHernault NL, Edelhauser HF. Ultrastructure in anterior and posterior stroma
of perfused human and rabbit corneas.
Relation to transparency. Invest Ophthalmol
Vis Sci 1995; 36: 15081523.
65. Morishige N, Wahlert AJ, Kenney MC,
Brown DJ, Kawamoto K, Chikama T,
Nishida T, Jester JV. Second-harmonic
imaging microscopy of normal human and
keratoconus cornea. Invest Ophthalmol Vis
Sci 2007; 48: 10871094.
66. Stachs O, Bochert A, Gerber T, Koczan D,
Thiessen HJ, Guthoff RF. The extracellular
67.
68.
69.
70.
71.
72.
73.
74.
75.
76.
77.
78.
79.
80.
81.
2007 The Authors
Journal compilation 2007 Optometrists Association Australia
matrix structure in keratoconus. Ophthalmologe 2004; 101: 384389.
Hayes S, Boote C, Tuft SJ, Quantock AJ,
Meek KM. A study of corneal thickness,
shape and collagen organisation in keratoconus using videokeratography and X-ray
scattering techniques. Exp Eye Res 2007; 84:
423434.
Tripathi RC, Bron AJ. Secondary anterior
crocodile shagreen of Vogt. Br J Ophthalmol
1975; 59: 5963.
Dangel ME, Kracher GP, Stark WJ. Anterior
corneal mosaic in eyes with keratoconus
wearing hard contact lenses. Arch Ophthalmol 1984; 102: 888890.
Meek KM, Blamires T, Elliott GF, Gyi TJ,
Nave C. The organisation of collagen fibrils
in the human corneal stroma: a synchrotron X-ray diffraction study. Curr Eye Res
1987; 6: 841846.
Katz HH. A hypothesis for the formation of
vertical corneal striae as observed in the
wearing of softlens contact lenses and in
keratoconus. Am J Optom Physiol Opt 1976;
53: 420421.
Smolek MK, McCarey BE. Interlamellar
adhesive strength in human eyebank corneas. Invest Ophthalmol Vis Sci 1990; 31:
10871095.
Smolek MK. Interlamellar cohesive
strength in the vertical meridian of human
eye bank corneas. Invest Ophthalmol Vis Sci
1993; 34: 29622969.
McMahon TT, Robin JB, Scarpulla KM,
Putz JL. The spectrum of topography
found in keratoconus. CLAO J 1991; 17:
198204.
Laing RA, Sandstrom MM, Berrospi AR,
Leibowitz HM. The human corneal endothelium in keratoconus: A specular microscopic study. Arch Ophthalmol 1979; 97:
18671869.
Matsuda M, Suda T, Manabe R. Quantitative analysis of endothelial mosaic pattern
changes in anterior keratoconus. Am J Ophthalmol 1984; 98: 4349.
Halabis JA. Analysis of the corneal endothelium in keratoconus. Am J Optom Physiol
Opt 1987; 64: 5153.
Hoffer KJ, Kraff MC. Normal endothelial
cell count range. Ophthalmology 1980; 87:
861866.
Esgin H, Erda N. Endothelial cell density
of the cornea during rigid gas permeable
contact lens wear. CLAO J 2000; 26: 146
150.
Grupcheva CN, Craig JP, Sherwin T,
McGhee CN. Differential diagnosis of corneal oedema assisted by in vivo confocal
microscopy. Clin Experiment Ophthalmol
2001; 29: 133137.
Alsuhaibani AH, Sutphin JE, Wagoner MD.
Confocal microscopy of subepithelial infiltrates occurring after epidemic keratoconjunctivitis. Cornea 2006; 25: 778780.
82. Wollensak G, Spoerl E, Seiler T. Riboflavin/
ultraviolet-a-induced collagen crosslinking
for the treatment of keratoconus. Am J Ophthalmol 2003; 135: 620627.
83. Mazzotta C, Traversi C, Baiocchi S, Sergio
P, Caporossi T, Caporossi A. Conservative
treatment of keratoconus by riboflavinUVA-induced cross-linking of corneal
collagen: qualitative investigation. Eur J
Ophthalmol 2006; 16: 530535.
84. Mazzotta C, Balestrazzi A, Traversi C, Baiocchi S, Caporossi T, Tommasi C, Caporossi
A. Treatment of progressive keratoconus by
riboflavin-UVA-induced cross-linking of
corneal collagen: Ultrastructural analysis by
Heidelberg Retinal Tomograph II in vivo
confocal microscopy in humans. Cornea
2007; 26: 390397.
85. Ruckhofer J. Clinical and histological studies on the intrastromal corneal ring segments (ICRS(R), Intacs(R)). Klin Monatsbl
Augenheilkd 2002; 219: 557574.
86. Kymionis GD, Siganos CS, Tsiklis NS, Anastasakis A, Yoo SH, Pallikaris AI, Astyrakakis
N, Pallikaris IG. Long-term follow-up of
Intacs in keratoconus. Am J Ophthalmol
2007; 143: 236244.
87. Shi W, Xie L, Li S, Yuan F, Liu H. Observation on healing process of corneal lens
after epikeratophakia with confocal
microscopy. Zhonghua Yan Ke Za Zhi 2002;
38: 295297.
88. Imre L, Resch M, Nagymihaly A. In vivo
confocal corneal microscopy after keratoplasty. Ophthalmologe 2005; 102: 140146.
89. Niederer RL, Perumal D, Sherwin T,
McGhee CN. Corneal innervation and cellular changes after corneal transplantation: an in vivo confocal microscopy
study. Invest Ophthalmol Vis Sci 2007; 48:
621626.
90. Forseto Ados S, Dos Santos MS, Sampaio A,
Mascaro V, Nos W. Diagnosis of epithelial
ingrowth after penetrating keratoplasty
with confocal microscopy. Cornea 2006; 25:
11241127.
Corresponding author:
Professor Nathan Efron
School of Optometry and
Institute of Health and Biomedical
Innovation
Queensland University of Technology
Kelvin Grove QLD 4059
AUSTRALIA
E-mail: n.efron@qut.edu.au
Clinical and Experimental Optometry 91.1 January 2008
55
Você também pode gostar
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Globus Electrostimulation User Guide PDFDocumento88 páginasGlobus Electrostimulation User Guide PDFFranciscoAinda não há avaliações
- Goljan Step 1 QuestionsDocumento3 páginasGoljan Step 1 QuestionsMary0% (1)
- IAP Guideline For Vitamin D Supplementation PDFDocumento7 páginasIAP Guideline For Vitamin D Supplementation PDFBandya SahooAinda não há avaliações
- NIH Public Access: The Pathogenesis of Systemic Lupus Erythematosus - An UpdateDocumento12 páginasNIH Public Access: The Pathogenesis of Systemic Lupus Erythematosus - An UpdateYessicaMariñosKirosAinda não há avaliações
- Physical ExaminationDocumento7 páginasPhysical ExaminationCha CulveraAinda não há avaliações
- List of Equipment and Supplies For Pediatric Units.Documento11 páginasList of Equipment and Supplies For Pediatric Units.vruttika parmar0% (1)
- Peds GIDocumento41 páginasPeds GIGladys SudiyantoAinda não há avaliações
- Faktor Risiko Kejadian Arthritis Gout Pada Pasien Rawat Jalan Di Rumah Sakit Dr. Wahidin Sudirohusodo, MakassarDocumento8 páginasFaktor Risiko Kejadian Arthritis Gout Pada Pasien Rawat Jalan Di Rumah Sakit Dr. Wahidin Sudirohusodo, MakassarEster DewAinda não há avaliações
- Report On DR.B.R.K.R Govt - Ayurvedic College & Hospital, Erragadda, HyderabadDocumento22 páginasReport On DR.B.R.K.R Govt - Ayurvedic College & Hospital, Erragadda, HyderabadRavindra Singh PalAinda não há avaliações
- Patient Rights & Responsibilities 03 Aug 2011Documento1 páginaPatient Rights & Responsibilities 03 Aug 2011Jv SinghAinda não há avaliações
- BrainwashingDocumento2 páginasBrainwashingSahnoune MohamedAinda não há avaliações
- Rhinitis Vasomotor Dek AmiDocumento15 páginasRhinitis Vasomotor Dek AmineviAinda não há avaliações
- Morphology of AcetabulumDocumento14 páginasMorphology of AcetabulumChee Wai HongAinda não há avaliações
- IIMC PPT June 16 June FinalDocumento28 páginasIIMC PPT June 16 June FinalSumeet GoelAinda não há avaliações
- Temephos 50 e C PDFDocumento2 páginasTemephos 50 e C PDFHARISH BARMAMAinda não há avaliações
- Oral Physiology ReviewerDocumento20 páginasOral Physiology ReviewerCamille Baybay100% (1)
- Prevalence of Water Borne Diseases Within Households in The Bamendankwemunicipalitynorth West Cameroon 2332 0893 1000122Documento7 páginasPrevalence of Water Borne Diseases Within Households in The Bamendankwemunicipalitynorth West Cameroon 2332 0893 1000122Welly SuryaAinda não há avaliações
- Health ICT Master PlanDocumento6 páginasHealth ICT Master Planaboix253Ainda não há avaliações
- Homeo MedicinesDocumento31 páginasHomeo MedicinesSaleem RazaAinda não há avaliações
- NHIS Variable SummaryDocumento4 páginasNHIS Variable SummaryJin SiclonAinda não há avaliações
- Distinguishing Between The Validity and Utility of Psychiatric DiagnosesDocumento9 páginasDistinguishing Between The Validity and Utility of Psychiatric DiagnosesMónica GarzaAinda não há avaliações
- Fatal Respiratory Failure During A "Technical" Rebreather Dive at Extreme PressureDocumento6 páginasFatal Respiratory Failure During A "Technical" Rebreather Dive at Extreme Pressuretonylee24Ainda não há avaliações
- Listeners' Attitudes Toward Children With Voice ProblemsDocumento8 páginasListeners' Attitudes Toward Children With Voice ProblemsparismonamourAinda não há avaliações
- AMOpportunities Certificate of ImmunizationDocumento1 páginaAMOpportunities Certificate of Immunizationashish guptaAinda não há avaliações
- Elements of MorphologyDocumento16 páginasElements of MorphologySyrk12Ainda não há avaliações
- Agenda: Scientific Program 6 Saudi Hematology Research DayDocumento7 páginasAgenda: Scientific Program 6 Saudi Hematology Research Daynemoo80 nemoo90Ainda não há avaliações
- Manual de Fixação Interna Rigida Craniofacial PDFDocumento14 páginasManual de Fixação Interna Rigida Craniofacial PDFFernandaJolyMacedoAinda não há avaliações
- ABASII Sample Report F Hr2Documento60 páginasABASII Sample Report F Hr2kalla55100% (1)
- HypochondriasisDocumento2 páginasHypochondriasisThe LullabyAinda não há avaliações