Escolar Documentos
Profissional Documentos
Cultura Documentos
Evaluacion de Screening para Disfagia en Niños
Enviado por
Sebastián Andrés ContrerasTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Evaluacion de Screening para Disfagia en Niños
Enviado por
Sebastián Andrés ContrerasDireitos autorais:
Formatos disponíveis
Brain & Development 37 (2015) 508514
www.elsevier.com/locate/braindev
Original article
Assessment of feeding and swallowing in children: Validity
and reliability of the Ability for Basic Feeding and Swallowing
Scale for Children (ABFS-C)
Anri Kamide a,, Keiji Hashimoto a, Kohei Miyamura b, Manami Honda a
a
Division of Rehabilitation Medicine and Developmental Evaluation Center, National Center for Child Health and Development, Japan
b
Tokyo Metropolitan Ohtsuka Hospital, Japan
Received 21 April 2014; received in revised form 14 August 2014; accepted 18 August 2014
Abstract
Objective: The purpose was to devise a dysphagia scale for disabled children that could be applied by various medical professionals, family members, and personnel in treatment and education institutions and facilities for disabled children and to assess the
validity and reliability of that scale, Ability for Basic Feeding and Swallowing Scale for Children (ABFS-C). Methods: Subjects
were 54 children (aged 2 months to 14 years and 7 months, median 14 months) who visited the National Center for Child Health and
Development from January 2012 to December 2013. They were examined using the Fujishimas Grade of Feeding and Swallowing
Ability (Fujishimas Grade), the Functional Independence Measure for Children (WeeFIM) and the ABFS-C composed of 5 items
(wakefulness, head control, hypersensitivity, oral motor and saliva control). Validity was evaluated according to correlations of the
ABFS-C with Fujishimas Grade or WeeFIM. To assess interrater reliability, 17 children were assessed by a doctor and occupational
therapist independently. Results: The ABFS-C scores and Fujishimas Grade were correlated using Spearman rank correlation coefcients. Fujishimas Grade was signicantly correlated with saliva control (R = 0.470) and the total ABFS-C scores (R = 0.322) but
not with wakefulness (R = 0.014), head control (R = 0.122), hypersensitivity (R = 0.009), or oral motor (R = 0.139). In addition,
the total ABFS-C scores had a signicant correlation with the total score of the WeeFIM (R = 0.562), motor WeeFIM (R = 0.451),
cognitive WeeFIM (R = 0,478), and the eating subscore of the WeeFIM (R = 0.460). Interrater reliability was demonstrated for all
items except hypersensitivity. Conclusions: There were signicant correlations between the total ABFS-C scores and Fujishimas
Grade and WeeFIM, which suggested the need for comprehensive assessments rather than assessments of individual feeding and
swallowing functions. To improve the reliability for hypersensitivity, the assessment process for hypersensitivity should be reviewed.
2014 The Japanese Society of Child Neurology. Published by Elsevier B.V. All rights reserved.
Keywords: Dysphagia; Children; ABFS-C; Clinical assessment scale
1. Introduction
Dysphagia rehabilitation in our country involves
multiple professions engaged in the treatment of primar-
ily physically disabled children with cerebral palsy or
neuromuscular disease. Recently, however, a wider
range of conditions such as developmental disorders
and tube-feeding dependency have to be addressed
Corresponding author. Address: National Center for Child Health and Development, 10-1, Okura 2-chome, Setagaya-ku, Tokyo 157-8535,
Japan. Fax: +81 (3) 3416 2222, +81 (3) 3416 0181.
E-mail address: kamide-a@ncchd.go.jp (A. Kamide).
http://dx.doi.org/10.1016/j.braindev.2014.08.005
0387-7604/ 2014 The Japanese Society of Child Neurology. Published by Elsevier B.V. All rights reserved.
A. Kamide et al. / Brain & Development 37 (2015) 508514
[1,2]. Childrens feeding and swallowing function is
developed not only through functional and morphological growth of oropharyngeal organs but also through
the development of other organs and psychophysiological functions. Consequently, children with dysphagia
can be pathogenetically classied into those aected by
retardation of functional development and those
aected by a reduction of acquired function. Features
of disability are thus so complicated that multiple assessments not only limited to the disease have to be
performed.
Neither here nor abroad, no satisfactory assessment
scale for childhood dysphagia has been established that
applies a clinical assessment based on an interview and
observation with an auxiliary diagnosis using imaging
methods [3]. Items found in textbooks for clinical assessment are wide-ranging, specialized, and timeconsuming. It is, therefore, desirable to develop an
assessment scale that would allow those with diverse
roles, varying from family members to personnel in
medical treatment institutions and welfare facilities such
as those facilities serving disabled children to arrive at a
shared understanding of dysphagia in disabled children.
We developed a feeding and swallowing function version of the Ability for Basic Movement Scale for
Children (ABMS-C) [4], which we had developed to
briey assess the ability for movement in children. In
addition, we veried the validity and reliability of the
new instrument.
2. Subjects and methods
2.1. Subjects
From January 2012 to December 2013, 54 pediatric
patients with dysphagia at the National Center for Child
Health and Development newly received rehabilitation.
There were 24 males and 30 females, and their median
age was 14 months (aged 2 months to 14 years and
7 months). They were classied according to the primary
pathogenesis as follows: organic, 17 (4, malignant disease; 3, laryngeal paralysis; 3, laryngomalacia; 2, cheilognathopalatoschisis; 2, gastroesophageal reux; 1, cleft
tongue; 1, multiple malformation; 1, esophageal atresia);
neurological, 28 (6, chromosome or genetic abnormality; 3, cerebral palsy; 3, hydrocephalus; 3, history of living donor liver transplantation; 3, extremely low birth
weight; 2, brain tumor; 2, epilepsy; 2, multiple malformation; 1, cerebrovascular disease; 1, encephalitis; 1,
hypoxic-ischemic encephalopathy; 1, history of cardiac
surgery); psychobehavioral, 5 (2, anorexia; 2, developmental disorder; 1 tube-feeding dependency after
operations); and developmental, 4 (3, tube-feeding
dependency due to inammatory bowel disease; 1,
history of cardiac surgery). They were classied
by swallowing phases as follows: postural control
509
preparation phase, 6; oral preparatory phase, 10; oral
phase, 4; pharyngeal phase, 32; and esophageal phase, 2.
This study was approved by the research ethics committee of the National Center for Child Health and
Development. Informed consent was obtained from
family members of all of the children.
2.2. Methods
2.2.1. Ability for Basic Feeding and Swallowing Scale
(ABFS-C)
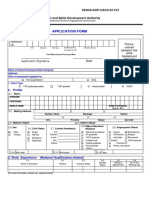
The ABFS-C is composed of 5 items pertaining to a
childs feeding and swallowing ability, i.e. wakefulness,
head control, hypersensitivity, oral motor ability, and
saliva control. Each item was rated on a 4-point scale
from 0 to 3. Fig. 1 shows assessment contents of the
ABFS-C.
Wakefulness is an index of food recognizability
reecting the patients general status prior to a feeding
and swallowing act. It is rated according to the Glasgow
Coma Scale as 0 in the case of failure to respond to pain
stimulation, as 1 if the patient is awakened by swaying
of the body, as 2 if the patient is awakened by speech,
or as 3 if the patient is awake without any stimulation.
Head control provides information on the patients
development of motor activity in the feeding posture or
the severity of neurological symptoms. As in the case of
the Ability for Basic Movement Scale for Children, [4]
head control is graded as 0 if the neck is completely
unstable, as 1 if the neck follows when both shoulders
are raised to 45 degrees, as 2 if the neck follows but stays
xed for less than 10 s when both shoulders are raised to
90 degrees, and as 3 if the neck is perfectly stable.
Hypersensitivity is a type of pediatric-specic
dysesthesia and is an index of the degree of lack of experience with feeding and swallowing. The patient is examined for such dysesthesia by slow movement of the
examiners palm while touching the patients body surface in the order of the upper and lower limbs from
the periphery to the center, the face, and around the lips
and oral cavity. Observation of changes in the patients
facial expression determines whether or not hypersensitivity is present. It is graded as 0 if hypersensitivity is
present all over the body, as 1 if it is present around
the lips, as 2 if it is present in the oral cavity, and as 3
if there is no hypersensitivity.
Oral motor ability serves as an index of the developmental degree of tongue and lip motor function and
the severity of neurological symptoms. Around the time
that a child acquires food-holding ability, he/she can
open or close the lips. Later, the child can move the tongue back and forth or up and down, and then from side
to side. Subsequently, the child becomes able to voluntarily protrude the tongue beyond the lips. Consequently, 0 represents the inability to close the lips or
move the tongue, 1 indicates lack of ability to move
510
A. Kamide et al. / Brain & Development 37 (2015) 508514
score
no response
wakefulness
to pain
no head control
head control
whole body
hypersensitivity
hypersensitive
to touch
oral motor
wakes up
when shaken
stimulus
or move tongue
can hold head up in line with can hold head up but not for
body when both
10 sec when
shoulders are
both shoulders
raised 45
are raised
degrees
90 degrees
does not like objects
does not like objects
touching lips
touching inside
or mouth area
the mouth
but cannot move
tongue
saliva control
constantly drooling
awake
when called to
can move lips
cannot close lips
wakes up
constant throat
can hold head up for
10 sec when both
shoulders are raised
90 degrees
not hypersensitive
can close lips
can close lips
and can move
and can stick
tongue inside
tongue outside
the mouth only
the mouth
throat gurgling
no throat gurgling
after stimulation
after stimulation
inside the mouth
inside the mouth
gurgling
Fig. 1. ABFS-C: Ability for Basic Feeding and Swallowing Scale for Children.
the tongue but the ability to close the lips, 2 denotes that
tongue movement is limited to the inside of the oral cavity, and 3 signies voluntary movement of the tongue
beyond the lips.
Saliva control is a risk index for aspiration that is
surmised from saliva control and the amount of food residue in the pharynx. It is graded as 0 if the child is always
unable to swallow saliva, resulting in overow of saliva
that has pooled in the oral cavity from the lips; as 1 if
pharyngeal secretions always make a gurgling sound,
as 2 if pharyngeal secretions make a gurgling sound only
after oral stimulation (stimulation is selected from gum
rubbing, gustatory stimuli, presentation of usual food,
etc. depending on the childs condition), and as 3 if there
are no gurgling sounds of pooled pharyngeal secretions
after oral stimulation.
2.2.2. Validity
To explore the validity of the ABFS-C, we assessed
the patients feeding and swallowing ability, and which
was scored according to the Fujishimas Grade of Feeding and Swallowing Ability (Fujishimas Grade) [5] and
the Food Intake LEVEL Scale (FILS) [6]. These scales
measure the severity of dysphagia by examining to what
degree patients take food orally. They are primarily
applied to adults and are used all over Japan. As these
instruments did not include factors related to childhood
growth and development, we modied them so that they
described how the child took food in a form that corresponded to that by a normally developed child of the
patients age.
Fujishimas Grade determines the severity of a swallowing disorder as necessary by using a videouoroscopic swallow study (VFSS) or a beroptic endoscopic
evaluation of swallowing (FEES). Severity is rated as
follows: Grade 1, diculty in swallowing or inability
to swallow, no indication for swallow training; Grade
2, indication only for basic swallow training; Grade 3,
aspiration occurs less often when conditions are right,
swallow training is feasible; Grade 4, feeding can be
enjoyable; Grade 5, oral intake is partially possible (1
or 2 meals); Grade 6, oral intake of 3 meals is possible
but alternative nutritional therapy is required; Grade
7, oral intake of easy-to-swallow food is possible at 3
meals; Grade 8, oral intake is possible at 3 meals unless
food is particularly hard to swallow; Grade 9, oral
intake of regular meals is possible under clinical watch
and guidance; and Grade 10, normal feeding and swallowing ability.
FILS determines the severity of dysphagia by judgment based on food forms and ratios of oral intakes
on a daily basis. Ratings are as follows: Level 1, no swallowing training is performed except for oral care; Level
2, swallowing training not using food is performed;
Level 3, swallowing training using a small quantity of
food is performed; Level 4, easy-to-swallow food less
than the quantity of a meal is ingested orally; Level 5,
easy-to-swallow food is orally ingested in one to two
meals, but alternative nutrition (non-oral nutrition such
as tube feeding and drip infusion) is also given; Level 6,
the patient is supported primarily by ingestion of easyto-swallow food in three meals, but alternative nutrition
is used as a complement; Level 7, easy-to-swallow food
is orally ingested in three meals and no alternative nutrition is given; Level 8, the patient eats three meals by
excluding food that is particularly dicult to swallow;
Level 9, there is no dietary restriction, and the patient
ingests three meals orally, but medical considerations
A. Kamide et al. / Brain & Development 37 (2015) 508514
are given; and Level 10, there is no dietary restriction,
and the patient ingests three meals orally (normal). In
the above assessment, we had the patient ingest regular
food consumed by normally developed children of the
same age (i.e. milk for a 3-mon-old baby, soft solid food
for an 8-mon-old baby).
In addition, we assessed the patients disability status
using the Functional Independence Measure for Children (WeeFIM). It is an 18-item, 7-level ordinal scale
instrument that measures a childs consistent performance of essential daily functional skills. The 18 items
are organized into 6 subscales of self-care (including eating), sphincter control, transfers, locomotion, communication, and social cognition. Total score of the motor
WeeFIM consists of scores for the subscales of self-care,
sphincter control, transfers, and locomotion. Total
scores of the cognitive WeeFIM consist of scores for
the subscales of communication and social cognition.
The Spearman rank method was employed to explore
correlations between items on the ABFS-C or total
scores of the ABFS-C and Fujishimas Grade or the
FILS in 54 pediatric patients. We similarly examined
the strength of the association between items on the
ABFS-C or total scores of the ABFS-C and the total
scores of WeeFIM, motor WeeFIM, and cognitive
WeeFIM and the eating subscore in the motor WeeFIM
in 31 children (12 boys, 19 girls; aged 2 months to
7 years and 8 months, median 11 months). Statistical
software used was SPSS Statistics 20.
2.2.3. Interrater reliability
Interrater reliability was evaluated employing examination of 17 of the above-mentioned children (8 boys, 9
girls; aged 3 months to 38 months, median 7 months).
Assessment was made separately by a doctor and an
occupational therapist using the ABFS-C at the rst
examination to seek weighted k coecients of resultant
data on individual items using the above-mentioned
software. Assessment dates diered at most by 1 week
511
between the doctor and occupational therapist involved
in the assessment. They were kept unaware of their
counterparts assessment scores during the study period.
2.2.4. Internal consistency
Internal consistency of the 5 items comprising the
ABFS-C was checked by Cronbachs coecient alpha
(Cronbachs A) in 54 pediatric patients.
3. Results
3.1. Validity
Whereas there was a signicant correlation between
Fujishimas Grade and saliva control (R = 0.470) or
the total score of the ABFS-C (R = 0.322), no obvious
correlation was found between Fujishimas Grade and
wakefulness (R = 0.014), head control (R = 0.122),
hypersensitivity
(R = 0.009)
or
oral
motor
(R = 0.134). Additionally, FILS had no signicant correlation with total scores or each item of the ABFS-C
(Table 1).
Results of the correlation coecient analysis that
compared scores of the ABFS-C and WeeFIM are
shown in Table 2. The total score of the ABFS-C
signicantly correlated with the total score of the WeeFIM (R = 0.562), motor WeeFIM (R = 0.451), cognitive WeeFIM (R = 0.478), and the eating subscore of
WeeFIM (R = 0.460). In addition, the total score of
the WeeFIM had a signicant correlation with head
control (R = 0.423) and oral motor (R = 0.440), and
the eating subscore of WeeFIM had a signicant correlation with oral motor (R = 0.373).
3.2. Interrater reliability
Scores on wakefulness and head control indicated
almost perfect interrater reliability (weighted k = 1.0,
weighted k = 0.889) while oral motor and saliva control
Table 1
Correlations of total scores of the ABFS-C with Fujishimas Grade or with FILS.
N = 54
Wakefulness
Head control
Hypersensitivity
Oral motor
Saliva control
Total score of ABFS-C
Grade
Level
Grade
Median
Range
3.00
3.00
3.00
0.00
2.00
11.00
4.00
5.00
03
03
03
03
03
015
110
110
ABFS-C: Ability for Basic Feeding and Swallowing Scale for Children.
Fujishimas Grade: Fujishimas Grade of Feeding and Swallowing Ability.
FILS: Food Intake LEVEL Scale.
*
p < 0.05.
**
p < 0.01.
Level
p
0.014
0.122
0.009
0.134
0.470**
0.322*
0.918
0.378
0.951
0.335
0.000
0.018
0.803**
0.000
p
0.225
0.001
0.086
0.043
0.331*
0.098
0.803**
0.102
0.992
0.535
0.760
0.014
0.480
0.000
512
A. Kamide et al. / Brain & Development 37 (2015) 508514
Table 2
Correlations of total scores of the ABFS-C with WeeFIM.
N = 31
Wakefulness
Head control
Hypersensitivity
Oral motor
Saliva control
Total score of
ABFS-C
Wee FIM
Total score
Motor WeeFIM
r
Median
Range
3.00
3.00
3.00
2.00
2.00
11.00
03
03
03
03
03
015
0.106
0.423*
0.071
0.440*
0.222
0.562**
0.570
0.018
0.705
0.013
0.231
0.001
0.089
0.354
0.004
0.359*
0.281
0.451*
Cognitive WeeFIM
Eating subscore of motor
WeeFIM
0.635
0.051
0.984
0.047
0.125
0.011
0.098
0.389*
0.029
0.375*
0.147
0.478**
0.601
0.031
0.878
0.038
0.429
0.007
p
0.089
0.354
0.009
0.373*
0.288
0.460**
0.634
0.051
0.964
0.039
0.116
0.009
ABFS-C: Ability for Basic Feeding and Swallowing Scale for Children.
WeeFIM: Functional Independence Measure for Children.
*
p < 0.05.
**
p < 0.01.
Table 3
Inter-rater reliability of each ABFS-C item by doctor and occupational
therapist (OT).
N = 17
Wakefulness
Head control
Hypersensitivity
Oral motor
Saliva control
*
**
Doctor
OT
Doctor
OT
Doctor
OT
Doctor
OT
Doctor
OT
Reliability
Median
Range
Weighted j
3.00
3.00
3.00
3.00
3.00
0.00
3.00
3.00
1.00
1.00
03
03
03
03
03
03
03
03
03
03
1.0*
0.000
0.889**
0.000
0.016
0.879
0.500*
0.006
0.502*
0.001
p < 0.05.
p < 0.01.
had moderate correlations (weighted k = 0.500,
weighted k = 0.502). On the other hand, hypersensitivity
showed no signicant interrater reliability (weighted
k = 0.016) (Table 3).
3.3. Internal consistency
The 5 items on the ABFS-C had appropriate internal
consistency (Cronbachs A = 0.974).
4. Discussion
The prevalence of childhood dysphagia is estimated
to fall between 25% and 45% in typically developing
children and between 33% and 80% of children with
developmental disability, [7] with an upward trend
currently in place. There are more than a few very
complicated and diversied structural, neurological
and psychobehavioral abnormalities that occur in the
process of growth and development [8]. Moreover, close
collaboration is required among disciplines to manage
disabled children since a variety of professions as well
as facilities become engaged in their management in
accordance with changes that take place from infancy/
childhood to school age/adulthood [1,2]. Consequently,
an assessment scale is desired that can easily identify the
whole picture of dysphagia in a child so that information can be shared among disciplines. At present,
however, in our country, individual facilities or communities assess dysphagia in their own distinctive ways.
Decision tables for dysphagia rehabilitation levels
and aspiration risks, which are being used in some pediatric rehabilitation centers, are the easiest to use but
they have not been satisfactorily veried for reliability
and validity [9]. An assessment approach proposed by
Murayama et al. [10] was aimed at detecting aspiration
in children with cerebral palsy and is therefore inappropriate for assessment of children with other disabilities.
A number of assessment methods for children have been
reported abroad [3,1115]. A systematic review of 27
papers published before 2012 [16] cited the Schedule
for Oral Motor Assessment (SOMA) [17] as an excellent
assessment method with regard to reliability, validity,
and clinical usefulness. This method was aimed at
assessing oral motor function and distinguishes between
normal and abnormal function by determining whether
feeding status for each of 5 food forms exceeded the
minimum level. However, it is not commonly used in
actual examinations because it is suitable only for dysphasic children with issues of the oral phase. Thus, the
reality is that there is no assessment method that is standardized for comprehensive assessment and severity
classication with substantiation of reliability and validity [11].
We therefore developed the ABFS-C to provide a
simple scale that could easily assess pediatric dysphagia
in daily life. One of the most useful points of the
A. Kamide et al. / Brain & Development 37 (2015) 508514
ABFS-C in comparison with other scales is that we can
easily record comprehensive ability regardless of dierent phases of feeding and swallowing, and then can
monitor the progress of the childs ability without a
VFSS or FEES.
Our results showed that total scores of the ABFS-C
had a signicant correlation with Fujishimas Grade,
total scores of the WeeFIM, motor WeeFIM, cognitive
WeeFIM, and the eating subscore of the WeeFIM. The
5 items on the ABFS-C had also appropriate internal
consistency. On the other hand, regarding items on the
ABFS-C, saliva control had a signicant correlation with
Fujishimas Grade but wakefulness, head control, hypersensitivity, and oral motor did not. In addition, there
were signicant correlations between total scores of the
WeeFIM and head control and oral motor. Oral motor
had the only signicant correlation with the eating subscore of the WeeFIM. Consequently, it was suggested
that severity assessment required a more comprehensive
assessment including not only individual swallowing
functions but also consciousness levels, sensation disorders and gross motor functions. FILS had no signicant
correlation with total scores of the ABFS-C or each of its
items except saliva control. This dierence from our ndings with Fujishimas Grade was because Fujishimas
Grade indicated how much the patient can do based
on a VFSS or FEES whereas FILS reected the patients
actual feeding action according to the direction by
their primary doctor [18]. Therefore, FILS was not
always determined with food forms suitable to the
patients feeding and swallowing ability probably resulting in a discrepancy between those levels and ABFS-C
scores. Moreover, since subjects diered in the causes
of dysphagia, including causative diseases and disorders
of the swallowing stages, it was suggested that the ABFSC had the potential to be used to assess disabled children
in general. Based on these results, we believe that the
ABFS-C is an eective assessment scale that reects the
severity of pediatric dysphagia.
Interrater reliability of the ABFS-C was veried in 4
items: wakefulness, head control, oral motor and saliva
control. On the other hand, such reliability was not
demonstrated in hypersensitivity, which may have been
because we do not have a good scale for evaluating
hypersensitivity in the body, lips and oral cavity. An
examiner whom the patient doesnt know has diculty
distinguishing between hypersensitivity and psychological refusal, so there might have been dierences in rating
between examiners. Since a past unpleasant experience,
a fear of strangers, or emotional insecurity due to a long
hospitalization may cause psychological refusal, it
seemed necessary to revise results of the assessment after
hearing about the patients responses when touched by a
family member. In addition, since dierent sensory stimuli other than touching with the examiners ngers,
including touching with a pacier, toothbrush or cup,
513
taste stimulus and thermal stimulus, may elicit dierent
responses, examiners might have faced diculty in decision making. We thought that there was yet room for
improvement in the assessment procedure, including
unication of kinds of sensory stimuli.
Finally, several limitations of this study should be
mentioned. First, it remains necessary to explore the
clinical utility of each item of the ABFS-C. We would
like to use the SOMA for validation in pediatric patients
with oral phase problems, and explore whether or not
scores are properly allocated to each item and whether
or not developing processes are reected in each age category using other international development evaluation
scales such as the Ages & Stages Questionnaires (ASQ)
or the Kinder Infant Development Scale (KIDs).
Second, we have to revise the assessment procedure
for hypersensitivity and its wording. Finally, it is necessary to evaluate interrater reliability between professionals and non-professionals. Then, we plan to accumulate
further cases and further revise this assessment tool.
References
[1] Mukai Y. History of developmental studies on eating function [in
Japanese]. Dental Med Res 2013;33:2334.
[2] Nagai S, Koike J. Rehabilitation for pediatric dysphagia. Sogo
Rehabil 2011;39:2317 [in Japanese].
[3] Arvedson JC, Brodsky L. Pediatric swallowing and feeding:
assessment and management. 2nd ed. New York: Singular Pub
Group Press; 2002.
[4] Miyamura K, Hashimoto K, Honda M. Validity and reliability
of Ability for Basic Movement Scale for Children (ABMS-C)
in disabled pediatric patients. Brain Dev 2011;33:
50811.
[5] Fujishima I. Rehabilitation for swallowing disorders associated
with stroke [in Japanese]. 2nd ed. Tokyo: Ishiyaku Publishers
Inc.; 1998.
[6] Kunieda K, Ohno T, Fujishima I, Hojo K, Morita T. Reliability
and validity of a tool to measure the severity of dysphagia: the
Food Intake LEVEL Scale. J Pain Symptom Manage
2013;46:2016.
[7] Lefton-Greif MA. Pediatric Dysphagia. Phys Med Rehabil Clin N
Am 2008;19:83751.
[8] Groher ME, Crary MA. Dysphagia: clinical management in
adults and children. 1st ed. St. Louis: Mosby Inc; 2009.
[9] Yokoyama M. Risk of rehabilitation in patients with profound
intellectual and multiple disease. Sogo Rehabil 2012;40:13742 [in
Japanese].
[10] Murayama K, Kanda T, Kondo I, Kitazumi E, Kodama K.
Assessment of dysphagia in the patient with cerebral palsy a
chart to estimate the possibility of aspiration in patients with
severe motor and intellectual disabilities. Jpn J Dysphagia
Rehabil 2004;8:14355 [in Japanese].
[11] Nishio M. Recent international trends in rehabilitation of
pediatric dysphagia. Jpn J Dysphagia Rehabil 2008;12:119 [in
Japanese].
[12] Stratton M. Behavioral assessment scale of oral functions in
feeding. Am J Occup Ther 1981;35:71921.
[13] Ottenbacher K, Dauck BS, Gevelinger M, Grahn V, Hassett C.
Reliability of the behavioral assessment scale of oral functions in
feeding. Am J Occup Ther 1985;39:43640.
[14] Cintas HL, Parks R, Don S, Gerber L. Brief assessment of
motor function: content validity and reliability of the upper
514
A. Kamide et al. / Brain & Development 37 (2015) 508514
extremity gross motor scale. Phys Occup Ther Pediatr
2011;31:44050.
[15] Sheppard JJ. Using motor learning approaches for treating
swallowing and feeding disorders: a review. Lang Speech Hear
Serv Sch 2008;39:22736.
[16] Benfer KA, Weir KA, Boyd RN. Clinimetrics of measures of
oropharyngeal dysphagia for preschool children with cerebral
palsy and neurodevelopmental disabilities: a systematic review.
Dev MedChild Neurol 2012;54:78495.
[17] Ko MJ, Kang MJ, Ko KJ, Ki YO, Chang HJ, Kwon JY. Clinical
usefullness of schedule for oral-motor assessment (SOMA) in
children with dysphagia. Ann Rehabil Med 2011;35:47784.
[18] Fujishima I, Oono T, Takahashi H, Katagiri H, Kuroda Y,
Ishibashi A, et al. Development of the scale of feeding and
swallowing: the Food Intake Level Scale. Jpn J Rehabil Med
2006;43:S249 [in Japanese].
Você também pode gostar
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5795)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Cdev 2 Child and Adolescent Development 2Nd Edition Spencer A Rathus Full ChapterDocumento51 páginasCdev 2 Child and Adolescent Development 2Nd Edition Spencer A Rathus Full Chapterdarrell.pace172100% (18)
- Learning For Success (LFS) : Sajeevta FoundationDocumento5 páginasLearning For Success (LFS) : Sajeevta FoundationGautam Patel100% (1)
- Assignment Stuff AssignmentsDocumento11 páginasAssignment Stuff Assignmentsapi-302207997Ainda não há avaliações
- 002LLI Castillo LTDocumento6 páginas002LLI Castillo LTJohnny AbadAinda não há avaliações
- English: Quarter 4 - Module 4: Reading Graphs, Tables, and PictographsDocumento23 páginasEnglish: Quarter 4 - Module 4: Reading Graphs, Tables, and PictographsResica BugaoisanAinda não há avaliações
- Lab 3Documento3 páginasLab 3bc040400330737Ainda não há avaliações
- CE Section - Docx 1.docx EDIT - Docx ReqDocumento7 páginasCE Section - Docx 1.docx EDIT - Docx ReqEdzel RenomeronAinda não há avaliações
- Advice To Young SurgeonsDocumento3 páginasAdvice To Young SurgeonsDorelly MartinezAinda não há avaliações
- Neha Ajay UpshyamDocumento2 páginasNeha Ajay UpshyamSantoshKumarAinda não há avaliações
- Cover LetterDocumento1 páginaCover Letterapi-282527049Ainda não há avaliações
- Shade T' If The Statement Is True and Shade F' If The Statement Is False in The True/false Answer Sheet ProvidedDocumento6 páginasShade T' If The Statement Is True and Shade F' If The Statement Is False in The True/false Answer Sheet ProvidedMUHAMMAD IKMAL HAKIM ABDULLAH100% (1)
- A General Inductive Approach For Analyzing Qualitative Evaluation DataDocumento11 páginasA General Inductive Approach For Analyzing Qualitative Evaluation DataThủy NguyễnAinda não há avaliações
- Biodentine: The Dentine in A Capsule or More?Documento12 páginasBiodentine: The Dentine in A Capsule or More?Razvan DumbraveanuAinda não há avaliações
- Explicit TeachingDocumento8 páginasExplicit TeachingCrisanta Dicman UedaAinda não há avaliações
- Research Process: Presented By:-Aditi GargDocumento12 páginasResearch Process: Presented By:-Aditi Gargpllau33Ainda não há avaliações
- National Strength and Conditioning Association.1Documento19 páginasNational Strength and Conditioning Association.1Joewin EdbergAinda não há avaliações
- 3 - U2L1-The Subject and Content of Art-AAPDocumento5 páginas3 - U2L1-The Subject and Content of Art-AAPFemme ClassicsAinda não há avaliações
- Form Ac17-0108 (Application Form) NewformDocumento2 páginasForm Ac17-0108 (Application Form) NewformEthel FajardoAinda não há avaliações
- 54819adb0cf22525dcb6270c PDFDocumento12 páginas54819adb0cf22525dcb6270c PDFEmaa AmooraAinda não há avaliações
- Key Data Extraction and Emotion Analysis of Digital Shopping Based On BERTDocumento14 páginasKey Data Extraction and Emotion Analysis of Digital Shopping Based On BERTsaRIKAAinda não há avaliações
- Ogl 320 FinalDocumento4 páginasOgl 320 Finalapi-239499123Ainda não há avaliações
- Analytical Solution For A Double Pipe Heat Exchanger With Non Adiabatic Condition at The Outer Surface 1987 International Communications in Heat and MDocumento8 páginasAnalytical Solution For A Double Pipe Heat Exchanger With Non Adiabatic Condition at The Outer Surface 1987 International Communications in Heat and MDirkMyburghAinda não há avaliações
- Differentiated LearningDocumento27 páginasDifferentiated LearningAndi Haslinda Andi SikandarAinda não há avaliações
- The Fourteen Domains of Literacy in The Philippines MTB-MLE CurriculumDocumento32 páginasThe Fourteen Domains of Literacy in The Philippines MTB-MLE CurriculumKaren Bisaya100% (1)
- Topic 9 Remedial and EnrichmentDocumento13 páginasTopic 9 Remedial and Enrichmentkorankiran50% (2)
- 7 Habits in Short 1Documento30 páginas7 Habits in Short 1api-3725164Ainda não há avaliações
- Report DPDocumento4 páginasReport DPHeryien SalimAinda não há avaliações
- Modified Lesson PlanDocumento6 páginasModified Lesson Planapi-377051886Ainda não há avaliações
- Life Skills Lesson 7 Respect Others LessonDocumento4 páginasLife Skills Lesson 7 Respect Others LessonAnonymous QmyCp9Ainda não há avaliações
- MTM Proposal Template (WordDocumento6 páginasMTM Proposal Template (Wordccp16Ainda não há avaliações