Escolar Documentos
Profissional Documentos
Cultura Documentos
Tytytt
Enviado por
ProbioticsAnywhereTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Tytytt
Enviado por
ProbioticsAnywhereDireitos autorais:
Formatos disponíveis
Fatima et al.
SpringerPlus 2012, 1:70
http://www.springerplus.com/content/1/1/70
RESEARCH
a SpringerOpen Journal
Open Access
Antimicrobial susceptibility pattern of clinical
isolates of Pseudomonas aeruginosa isolated from
patients of lower respiratory tract infections
Anab Fatima2*, Syed Baqir Naqvi1, Sheikh Abdul Khaliq2, Shaheen Perveen3 and Sabahat Jabeen1
Abstract
The present study was conducted to determine the antibiotic susceptibility pattern of Pseudomonas aeruginosa
from sputum samples of lower respiratory tract infection patients admitted to different hospitals of Karachi. Most of
the hospitals are hampered with high frequency of nosocomial infections generally caused by multiresistant
nosocomial pathogen. Among Gram-negative pathogens Pseudomonas aeruginosa considered as most challenging
pathogen. The objective of the study was to determine frequency of Pseudomonas aeruginosa from sputum
samples and to find out susceptibility pattern against four antibiotics widely used for treatment. The sputum
samples from 498 patients were collected consecutively between January 2010 and March 2011 and were cultured
and identified. According to CLSI (Clinical Laboratory Standards Institute) guidelines antimicrobial susceptibility
testing was performed by disc diffusion method. Pseudomonas aeruginosa were isolated from 24% (120/498) of the
lower respiratory tract patient. A higher resistance to Pseudomonas aeruginosa isolate was observed with
piperacillin/tazobactam and cefipime i.e. 42% and 40% respectively. Imipenem was found to be most effective
antibiotic against Pseudomonas aeruginosa (76% sensitivity) but amikacin resistance was continuously increasing. In
conclusion the frequency of Pseudomonas aeruginosa was also higher among lower respiratory tract infection
patients with alarmingly high rate of resistance among widely used antibiotics. These findings focused on careful
consideration for monitoring and optimization of antimicrobial use in order to reduce occurrence and spread of
antimicrobial resistant pathogen.
Introduction
In general practice bronchitis and pneumonia were most
common lower respiratory tract infections and were
related to considerable mortality and morbidity worldwide (Macfarlane et al. 2001). According to statistics
4.4% of hospital admissions and 6% of general practitioner consultations were related to lower respiratory
tract infections (Anderson et al. 1993). A wide variety of
antimicrobial agents with anti-pseudomonal activity
along with advancement in medical and surgical care
has been developed but Pseudomonas aeruginosa
causing life threatening infections continue to cause
complications in hospitals acquired infections (Mayhall
1996). Pseudomonas aeruginosa is a Gram-negative
aerobic rod belong to family Pseudomonadaceae. It
* Correspondence: anabfatima@hotmail.com
2
Department of Pharmaceutics, Faculty of Pharmacy, Hamdard University,
Karachi, Pakistan
Full list of author information is available at the end of the article
become considered as an opportunistic pathogens and a
major cause of nosocomial infections. It was also considered as most challenging pathogen globally because of
its high rate of resistance to antimicrobial agents (Hugbo
and Olurinola 1992; Trilla 1994). The Pseudomonas aeruginosa had very minimal nutritional requirement that
expedited its growth in hospital environment (Gilligan
1995). Resistance to multiple antimicrobial agents displayed by Pseudomonas aeruginosa and only few
antibiotics found to be effective against Pseudomonas
aeruginosa (Carmeli et al. 1999). A high resistance
pattern of Pseudomonas aeruginosa measured as cause
of higher mortality rate by Pseudomanal infections
(Samporn et al. 2004). Different geographical locations
and hospital environments showed variation in susceptibility pattern of Pseudomonas aeruginosa isolates
therefore idiosyncrasy of isolate susceptibility pattern
2012 Fatima et al.; licensee Springer. This is an Open Access article distributed under the terms of the Creative Commons
Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction
in any medium, provided the original work is properly cited.
Fatima et al. SpringerPlus 2012, 1:70
http://www.springerplus.com/content/1/1/70
required for chemotherapeutic approach of Pseudomonal infections for better achievement of results.
In this study we aimed to determine the prevalence of
Pseudomonas aeruginosa in lower respiractory tract infection patients and to compare their antibiotic susceptibility pattern.
Materials and Methods
Study setting
A total number of 498 sputum samples were collected
from adult patients attended/admitted in pulmonary department of various hospitals and clinics suffered from
lower respiratory tract infections in 14 months period
from January 2010 to March 2011. Out of 498 samples
120 samples were Pseudomonas aeruginosa.
Microbiology/sample processing
The samples were transferred to microbiology laboratory
and were analyzed within 30 min to 1 hour of collection.
Nutrient agar, MacConkey agar and blood agar (Oxoid
UK) used for streaking of sample and then incubated at
37C for 24 hours as described by chessborough (Cheesborough 2002). After incubation Pseudomonas isolation
agar media (Oxoid UK) used for sub-culturing of isolate
obtained. The pure isolates of Pseudomonas aeruginosa
were transferred to 1% nutrient agar slant and stored in
the refrigerator at 4 1C. Diifferent identification tests
were performed on suspected Pseudomonas aeruginosa
and were characterized and identified i.e. Gram-stain,
colonial morphology, positive oxidase reaction, production of pyocyanin on Mueller-Hinton agar (Oxoid UK),
citrate utilization and growth at 42C.
Antibiotic susceptibility test
By disk diffusion technique antibiotic susceptibility pattern of isolates on commonly used antibiotics was performed on Mueller-Hinton agar medium according to
Clinical Laboratory Standard Institute (CLSI) guidelines
(NCCLS 1995). Paper disk were impregnated with antibiotics (Sigma chemicals): imipenem (10 g), Amikacin
(30 g), piperacillin / tazobactam (100/10 g) and cefipime (30 g) respectively and incubated at 37C for
24 hours in 510% CO2 enriched environment. The
medium containing antibiotic disks were quality controlled daily by standard culture. After defined incubation period the diameter of zone of inhibition was
measured and interpretation of result based on CLSI
guidelines was performed (NCCLS 1995).
Result
In 14 months period a total of 498 sputum specimens
were collected consecutively from different hospitals of
Karachi and a total of 120 Pseudomonas aeruginosa
strains (24%) were isolated of which 85 samples (70.8%)
Page 2 of 4
and 35 samples (29.1%) were reported from males and
females respectively (Figure 1).
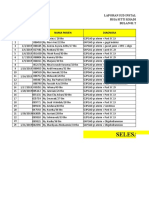
The antibiotic resistance pattern of isolates presented
in Figure 2. The most effective antibiotic was from Carbapenem i.e. imipenem and its resistance rate was
detected as 24%.
Piperacillin/tazobactam and cefipime showed more resistance i.e. 42% and 40% respectively. Amikacin also
showed 35% resistance. Graphically Figure 2 clearly reflect antibiotic susceptibility profile of Pseudomonas aeruginosa isolates and showed that imipenem was most
sensitive then all other antibiotics used.
Discussion
The main objective of this study was to investigate epidemiological data of Pseudomonas aeruginosa strains in
lower respiratory tract infection patients and to determine the antimicrobial resistance pattern of bacteria
against some commonly used antibiotics. The predominance of Pseudomonas aeruginosa resistance considered
as serious problem in many countries (Agarwal et al.
2006; Ako-Nai et al. 2006; Balkhy et al. 2006; Lizioli
et al. 2003). It was also reported that Pseudomonas aeruginosa is one of the most common nosocomial pathogen
and a leading cause of nosocomial respiratory tract infection (Gilligan 1995; Jarvis and Martone 1992; Jarlier
et al. 1996).
From previous literature high rate of resistance against
carbapenem, quinolones and third generation cephalosporin had been detected in Pseudomonas aeruginosa
(Hancock 1998; Quinn 1998; Sader et al. 1998). In our
study resistance rate against imipenem from carbapenem
group was determined as 24% which was considerably
accelerating towards higher side in Pakistan and this was
in agreement with previous study conducted by Akhtar
N which showed resistance rate of 26.1% (Akhtar 2010).
It was reported that resistance to imipenem was 14% in
Spain (Bouza et al. 1999), 19.3% in Italy (Bonfiglio et al.
1998) and was 68% in Saudi Arabia (Rotimi et al. 1998).
29.10%
Males
Females
70.80%
Figure 1 % occurrence of lower respiratory tract infections in
males and females by Pseudomonas aeruginosa.
Fatima et al. SpringerPlus 2012, 1:70
http://www.springerplus.com/content/1/1/70
Page 3 of 4
respiratory tract infection an ultimate and detailed bacteriological diagnosis and susceptibility testing required
to overcome global problem of antibiotic resistance
and by encouraging greater understanding of this problem different solutions can be planned by health care
providers.
76%
80%
70%
60%
50%
40%
30%
20%
10%
0%
65%
58%
42%
60%
40%
35%
24%
S
R
Figure 2 Resistance rate of Pseudomonas aeruginosa. IMP:
imipenem, AMIK: amikacin, PIP/TAZO: piperacillin/tazobactam, CFP:
cefipime.
In a previous hospital study resistance rate among
Pseudomonas aeruginosa was only 59% against amikacin (Bouza et al. 1999; Gerding et al. 1991). In the
present study the rate of amikacin resistance was found
to be relatively high i.e. 35% however it may in accordance with Friedland et al. who reported that amikacin
resistance related to more intensive usage of amino glycosides (Friedland et al. 1992). The increasing rate of
amikacin in Pakistan was also reported by Akhtar N i.e.
21.3 against Pseudomonas aeruginosa (Akhtar 2010). It
was further investigated that when amikacin used in
combination with impenem i.e. as combination therapy
resistance rate among Pseudomonas aeruginosa was
reduced to 10% (Bustamante et al. 1987).
Piperacillin/tazobactam resistance rate was 7% in a nationwide in Spain (Bouza et al. 1999). Contrary to this
resistance rate in isolates was higher in our study (42%).
In a previous study equivalent safety and efficacy of
intravenous Piperacillin/tazobactam with intravenous
imipenem/cilastatin was reported for intra-abdominal
infections caused by Pseudomonas aeruginosa but presently resistance was different for both antibiotics which
might be due to extensive usage of this combination in
our hospitals as life saving antibiotics (Erasmo et al.
2004).
In the present study resistance rate of Pseudomonas
aeruginosa against cefepime observed was deviated from
reported data as it showed 40% resistance while in previous reported data it did not exceed 17% (Bouza et al.
1999).
The data obtained from our study in Pakistan it was
probable that application of conventional agents for the
empirical treatment become complicated by the respiratory pathogens with accelerating resistance to antibiotics. Therefore for an effective management of lower
Competing interests
The authors declare that they have no competing interests.
Authors contributions
AF: carried out main research work as she was research fellow. SBN: He was
research supervisor, performed continuous vigilance via out research work.
SAK: Involved in searching and validation of method. SP: Carried out data
compilation, did drafting of manuscript. SJ: She did verification and
identification of clinical isolates. All authors read and approved the final
manuscript.
Author details
1
Department of Pharmaceutics, Faculty of Pharmacy, University of Karachi,
Karachi, Pakistan. 2Department of Pharmaceutics, Faculty of Pharmacy,
Hamdard University, Karachi, Pakistan. 3Department of Pharmaceutics, Faculty
of Pharmacy, Jinnah University for Women, Karachi, Pakistan.
Received: 18 October 2012 Accepted: 6 December 2012
Published: 18 December 2012
References
Agarwal R, Gupta D, Ray P (2006) Epidemiology, risk factors and outcome of
nosocomial infections in a respiratory intensive care unit in north India. J
Infect 53(2):98105
Akhtar N (2010) Hospital acquired infections in a medical intensive care unit. J
Coll Physicians Surg Pak 20(6):386390
Ako-Nai AK, Ikem IC, Akinloye OO, Aboderin AO, Ikem RT, Kassim OO (2006)
Characterization of bacterial isolates from diabetic foot infections in Ile-Ife,
south western Nigeria. Foot 16(3):158164
Anderson H, Esmail A, Hollowell J, Littlejohns P, Strachen D (1993)
Epidemiologically based needs assessment: lower respiratory disease. DHA
Project Research Programme, Government publication Publisher: NHS
Management Executive, 1993.report 16, pp 612
Balkhy HH, Cunningham G, Chew FK (2006) Hospital- and community-acquired
infections: a point prevalence and risk factors survey in a tertiary care center
in Saudi Arabia. Int J Infect Dis 10(4):326333
Bonfiglio G, Carciotto V, Russo G et al (1998) Antibiotic resistance in
pseudomonas aeruginosa: an Italian survey. Antimicrob Chemother 41:307
310
Bouza E, Garcia-Gorrote F, Cercenado E, Marin M, Diaz MS (1999) Pseudomonas
aeruginosa: a survey of resistance in 136 hospitals in Spain. The Spanish
pseudomonas aeruginosa study group antimicrob agents chemother, 43rd
edn., pp 981982
Bustamante CI, Drusano GI, Wharton RC, Whade GC (1987) Synergism of the
combinations of imipenem plus ciprofloxacin and imipenem plus Amikacin
against pseudomonas aeruginosa and other bacterial pathogens. Antimicrob
Agents Chemother 31(4):632634
Carmeli Y, Troillet N, Eliopoulos GM, Samore MH (1999) Emergence of antibioticresistant pseudomonas aeruginosa: comparison of risks associated with
different anti pseudomonal agents. Antimicrob Agents Chemother 43:1379
1382
Cheesborough M (2002) Medical laboratories manual for trocountries. Tropical
Health Technol. Butterworth London 2:479
Erasmo AA, Crisostomo AC et al (2004) Randomized comparison of piperacillin/
tazobactam versus imipenem/cilastatin in the treatment of patients with
intra-abdominal infections. Asian J Surg 27(3):227235
Friedland IR, Funk E, Khoosal M, Klugman KP (1992) Increased resistance to
Amikacin in a neonatal unit following intensive Amikacin usage. Antimicrob
Agents Chemother 36(8):15961600
Gerding DN, Larson TA, Hughes RA et al (1991) Amino glycoside resistance and
amino glycoside usage: ten years of experience in one hospital. Antimicrob
Agents Chemother 35(7):12841290
Fatima et al. SpringerPlus 2012, 1:70
http://www.springerplus.com/content/1/1/70
Page 4 of 4
Gilligan PH (1995) Pseudomonas and Burkholderia. In: Murray RR, Baron EJ, Pfaler
MA, Tenover FC, Yolken RH (eds) Manual of clinical microbiology. American
Society for Microbiology, Washington DC, pp 509519
Hancock REW (1998) Resistance mechanism in pseudomonas aeruginosa and
other nonfermentative gram-negative bacteria. Clin Infect Dis 27:289299
Hugbo PG, Olurinola PF (1992) Resistance of pseudomonas aeruginosa to
antimicrobial agents: implications in medicine and pharmacy. Nig J Pharm
Sci 4:110
Jarlier V, Fosse T, Philippon A (1996) Antibiotic susceptibility in aerobic gramnegative bacilli isolated in intensive care units in 39 French teaching
hospitals (ICU study). Intensive Care Med 22:10571065
Jarvis WR, Martone WJ (1992) Predominant pathogens in hospital infections. J
Antimicrob Chemother 29(A):1924
Lizioli A, Privitera G, Alliata E (2003) Prevalence of nosocomial infections in Italy:
result from the Lombardy survey in (2000). J Hosp Infect 54(2):141148
Macfarlane J, Holmes W, Gard P, Macfarlane R, Rose D, Weston V, Leinonen M,
Saikku P, Myint S (2001) Prospective study of the incidence, aetiology and
outcome of adult lower respiratory tract illness in the community. Thorax 56
(2):109114
Mayhall CG (1996) Nosocomial burn wound infection. In: Mayhall GC (ed)
Hospital epidemiology and infection control. William and Wilkins Co,
Baltimore, MD, USA, pp 225236
National Committee for Clinical Laboratory Standards (1995) Approved standard
M2 A7 NCCLS. In: Villanova PA (ed) Performance standards for antimicrobial
disk susceptibility tests., p 15, NCCLS T 940 West Valley Road T Suite 1400 T
Wayne, PA 19087 T USA, T PHONE 610.688.0100
Quinn JP (1998) Clinical problems posed by multiresistant nonfermenting gramnegative pathogens. Clin Infect Dis 27:117124
Rotimi VO, Al-Sweih NA, Feteih J (1998) The prevalence and antibiotic
susceptibility pattern of gram-Negative bacterial isolates in two ICUs in Saudi
Arabia and Kuwait. Diagn Microbiol Infect Dis 30:5359
Sader HS, Jones RN, Gales AC et al (1998) Antimicrobial susceptibility patterns for
pathogens isolated from patients in Latin American medical centers with a
diagnosis of pneumonia: analysis of results from the SENTRY antimicrobial
surveillance program (1997). SENTRY Latin American study group. Diagn
Microbiol Infect Dis 32:289301
Samporn S, Chuntima T, Thitiya Y, Chertask D (2004) Prevalence and antimicrobial
susceptibility of pseudomonas aeruginosa mucoid and non-mucoid type. SE
Asian J Trop Med 35:893894
Trilla A (1994) Epidemiology of nosocomial infections in adult in care units.
Intensive Care Med 20(3):14, 1
doi:10.1186/2193-1801-1-70
Cite this article as: Fatima et al.: Antimicrobial susceptibility pattern of
clinical isolates of Pseudomonas aeruginosa isolated from patients of
lower respiratory tract infections. SpringerPlus 2012 1:70.
Submit your manuscript to a
journal and benet from:
7 Convenient online submission
7 Rigorous peer review
7 Immediate publication on acceptance
7 Open access: articles freely available online
7 High visibility within the eld
7 Retaining the copyright to your article
Submit your next manuscript at 7 springeropen.com
Você também pode gostar
- M!L!H!SD! !!!!:!! ® 'I F ! A!m W Ew!!!p!!!!!!!!!!!! A!! F!!!!!!!!! ! ! !!! LLLTLLDocumento77 páginasM!L!H!SD! !!!!:!! ® 'I F ! A!m W Ew!!!p!!!!!!!!!!!! A!! F!!!!!!!!! ! ! !!! LLLTLLProbioticsAnywhere100% (1)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Food Microbiology ScopeDocumento2 páginasFood Microbiology ScopeProbioticsAnywhere50% (2)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Real-Time PCR:: Quantifying The QPCR MarketplaceDocumento12 páginasReal-Time PCR:: Quantifying The QPCR MarketplaceProbioticsAnywhereAinda não há avaliações
- Practical - Turbidimetric MethodsDocumento9 páginasPractical - Turbidimetric MethodsProbioticsAnywhere100% (1)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Virology - Isolation & Cultivation of BacgteriophageDocumento12 páginasVirology - Isolation & Cultivation of BacgteriophageProbioticsAnywhereAinda não há avaliações
- Bacteriology - Determining Bacterial CFU by Miles & Misra MethodDocumento2 páginasBacteriology - Determining Bacterial CFU by Miles & Misra MethodProbioticsAnywhereAinda não há avaliações
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Multiple-Antibiotic Resistance Mediated by Plasmids and Integrons in Uropathogenic Escherichia Coli and Klebsiella PneumoniaeDocumento5 páginasMultiple-Antibiotic Resistance Mediated by Plasmids and Integrons in Uropathogenic Escherichia Coli and Klebsiella PneumoniaeProbioticsAnywhereAinda não há avaliações
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- EwswsawnDocumento5 páginasEwswsawnProbioticsAnywhereAinda não há avaliações
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- XXXXXXXXXXX BGDocumento5 páginasXXXXXXXXXXX BGProbioticsAnywhereAinda não há avaliações
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- HJNHNNDocumento9 páginasHJNHNNProbioticsAnywhereAinda não há avaliações
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Essential Article On CancerDocumento10 páginasEssential Article On CancerProbioticsAnywhereAinda não há avaliações
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Mycology PresentationDocumento3 páginasMycology PresentationProbioticsAnywhereAinda não há avaliações
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- Useful Article On CancerDocumento7 páginasUseful Article On CancerProbioticsAnywhereAinda não há avaliações
- Sutured Wound Care InstructionsDocumento2 páginasSutured Wound Care InstructionsPreet Inder SinghAinda não há avaliações
- MSDS PDFDocumento5 páginasMSDS PDFdang2172014Ainda não há avaliações
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Body Image: Marika Tiggemann, Kristy HageDocumento7 páginasBody Image: Marika Tiggemann, Kristy HageRachel VictorianaAinda não há avaliações
- Best Supplements For ADHD and Focus Support For Kids - GNC IndiaDocumento3 páginasBest Supplements For ADHD and Focus Support For Kids - GNC IndiaTrần Thị UyênAinda não há avaliações
- Health and Welfare Committee ReportDocumento4 páginasHealth and Welfare Committee ReporttncircuitriderAinda não há avaliações
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- Stroke PamphletDocumento12 páginasStroke Pamphletapi-232971337Ainda não há avaliações
- Proforma For College - Information Regarding Fee, Bond - Conditions EtcDocumento2 páginasProforma For College - Information Regarding Fee, Bond - Conditions EtcThe Indian DentistAinda não há avaliações
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Case Report MyelopathyDocumento29 páginasCase Report MyelopathyNurul Hasanah SururyAinda não há avaliações
- SHARON SCHULTZ, ET AL. v. JANOS GUOTH, M.D. AND KHALED F. RABIE, M.D. (Parish of Rapides)Documento18 páginasSHARON SCHULTZ, ET AL. v. JANOS GUOTH, M.D. AND KHALED F. RABIE, M.D. (Parish of Rapides)wstAinda não há avaliações
- Medical Terminology Worksheet-2Documento4 páginasMedical Terminology Worksheet-2pumpiepumpkin12Ainda não há avaliações
- Grade 2 Edema On Arms and Legs (Grade 2 Periorbital Edema: Additional Not From The Searched Case StudyDocumento3 páginasGrade 2 Edema On Arms and Legs (Grade 2 Periorbital Edema: Additional Not From The Searched Case StudyKim Glaidyl BontuyanAinda não há avaliações
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Eeh455 Assignment2b MaharpDocumento22 páginasEeh455 Assignment2b Maharpapi-267478292Ainda não há avaliações
- Cold Cryotherapy NotesDocumento6 páginasCold Cryotherapy Notesakheel ahammedAinda não há avaliações
- Forensic Aspects of Dissociative Identity DisorderDocumento240 páginasForensic Aspects of Dissociative Identity DisorderDeath Tiscat100% (1)
- Shape Up BusyBee CarysDocumento16 páginasShape Up BusyBee CarysElena HorodincaAinda não há avaliações
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Polscience 6th SemDocumento16 páginasPolscience 6th Semritam1994paulAinda não há avaliações
- Anti ParasiteDocumento4 páginasAnti ParasiteVörös Bálint100% (1)
- Book of Best Practices Trauma and The Role of Mental Health in Post-Conflict RecoveryDocumento383 páginasBook of Best Practices Trauma and The Role of Mental Health in Post-Conflict RecoveryDiego Salcedo AvilaAinda não há avaliações
- VE4 Sem 1 Student Packet (25 July)Documento187 páginasVE4 Sem 1 Student Packet (25 July)Dwayne June GetiganAinda não há avaliações
- Sample Massage Therapy Business Plan TemplateDocumento8 páginasSample Massage Therapy Business Plan Templatewealth nwaiwuAinda não há avaliações
- Nutritional Interventions PDFDocumento17 páginasNutritional Interventions PDFLalit MittalAinda não há avaliações
- Business Ethics and Corporate Social Responsibility: Analyze Complex Issues in CSR and Corporate GovernanceDocumento6 páginasBusiness Ethics and Corporate Social Responsibility: Analyze Complex Issues in CSR and Corporate GovernanceDime PierrowAinda não há avaliações
- WRAS MarinasDocumento4 páginasWRAS MarinasAdam ReesAinda não há avaliações
- Laporan Iud 2019Documento91 páginasLaporan Iud 2019Yuli AntiAinda não há avaliações
- Break The Cycle Activity GuidesDocumento19 páginasBreak The Cycle Activity GuidesJuanmiguel Ocampo Dion SchpAinda não há avaliações
- Homoeopathic Perspective of Thyroid DisordersDocumento20 páginasHomoeopathic Perspective of Thyroid DisordersSaurav AroraAinda não há avaliações
- Settle Plate SamplingDocumento3 páginasSettle Plate SamplingFilipa PereiraAinda não há avaliações
- Concept PaperDocumento2 páginasConcept PaperAngel CoAinda não há avaliações
- APLS Scenario OSCE PDFDocumento5 páginasAPLS Scenario OSCE PDFNikita JacobsAinda não há avaliações
- Postharvest Technology-Importance: Eufemio G. Barcelon, PHDDocumento56 páginasPostharvest Technology-Importance: Eufemio G. Barcelon, PHDJohanna Amor L. AdaoAinda não há avaliações
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNo EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNota: 5 de 5 estrelas5/5 (3)