Escolar Documentos
Profissional Documentos
Cultura Documentos
Belle Preterm Birth
Enviado por
Rashed ShatnawiDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Belle Preterm Birth
Enviado por
Rashed ShatnawiDireitos autorais:
Formatos disponíveis
PRETERM BIRTH
Significance
Pathogenesis
A birth that occurs before 37
Clinical and laboratory
Taken together with its
Approximately 70 to
completed weeks of gestation.
evidence suggest that a
sequelae,
PTB
is
by
far
80
percent
of
PTBs
Subclassifications of PTB are
number of pathogenic
the leading cause of
occur spontaneously.
variably and inconsistently
processes can lead to a final
infant mortality in the
preterm labor (PTL)
defined as:
common pathway that results
United
States.
accounts
for
40
to
50
Late preterm = 34 to 36 weeks
in preterm labor and delivery.
percent of all PTBs
Moderately preterm = 32 to 34 PTB is also a major
determinant of shortand preterm
weeks
The four primary processes
and
long-term
premature rupture of
Very preterm = <32 weeks
are:
morbidity in infants and
membranes (PPROM)
Extremely preterm = <28
children.
accounts for 20 to 30 1. Activation of the maternal
weeks
or fetal hypothalamicpercent.
INCIDENCE
In
the
PTB can also be defined by
pituitary-adrenal axis
United States, 12.8
The remaining 20 to
birth weight (BW):
percent of births in
30 percent of PTBs are 2. Infection
Low birth weight (LBW) BW
2006 occurred preterm
due to intervention for 3. Decidual hemorrhage
less than 2500 g
4. Pathological uterine
and 3.66 percent were
maternal or fetal
Very low birth weight (VLBW)
distention
less than 34 weeks of
problems
BW less than 1500 g
gestation
Extremely low birth weight
(ELBW) BW less than 1000 g
RISK FACTOR, CLINICAL MANIFESTATIONS AND DIAGNOSIS FACTORS
PTL is one of the most common reasons for
Uterine contractions are a normal finding at all stages of
hospitalization of pregnant women.
pregnancy, thereby adding to the challenge of distinguishing true
from false labor. The frequency of contractions increases with
In one systematic review, approximately 30
gestational age, the number of fetuses, and at night.
percent of preterm labors spontaneously
resolved.
The diagnosis of PTL is generally based upon clinical criteria of
Signs and symptoms of early PTL include
regular painful uterine contractions accompanied by cervical
menstrual-like cramping, constant low back
dilation and/or effacement. Specific criteria, which were initially
ache, mild uterine contractions at infrequent
developed to select subjects in research settings, include
and/or irregular intervals, and bloody show.
However, these signs and symptoms are nonspecific and often noted in women whose
pregnancies go to term.
Initial evaluation of women
with suspected PTL should
determine:
1. The presence and
frequency of uterine
contractions
2. Whether there is
uterine bleeding
3. Whether the fetal
membranes have
ruptured
4. Gestational age
5. Fetal well-being
Physical examination
The uterus is examined to
assess firmness,
tenderness, fetal size, and
fetal position.
A sterile speculum
examination is performed
to rule out ruptured
membranes, to visually
examine the vagina and
cervix
Obtain specimens for
laboratory testing .
A digital examination to
assess cervical dilatation
and effacement is
performed after placenta
previa and PPROM have
been excluded
persistent uterine contractions (four every 20 minutes or eight
every 60 minutes) with documented cervical change or cervical
effacement of at least 80 percent, or cervical dilatation greater
than 2 cm.
Digital cervical examination has limited reproducibility between
examiners, especially when changes are not pronounced;
therefore, some centers evaluate the cervix via transvaginal
ultrasound to confirm the diagnosis A short cervix has been
variously defined as a cervical length less than 2.0 cm, 2.5 cm, or
3.0 cm.
Lab tests
Urine culture, since
bacteriuria and
pyelonephritis are
associated with PTB.
Rectovaginal group B
streptococcal culture, to
determine need for
antibiotic prophylaxis.
Tests for gonorrhea and
chlamydia.
Testing for gonorrhea and
chlamydia may be omitted
if previously performed, the
results were negative, and
the patient is not at high
risk of acquiring sexually
transmitted infections.
Fetal fibronectin (fFN),a
swab for fFN on all
symptomatic patients
considered at high risk for
PTB.
Perform transvaginal
sonographic measurement
of cervical length.
We only send the swab to
the laboratory for FFN
determination if the
cervical length is 20 to 30
mm
Given the link between
cocaine use and placental
abruption, perform drug
testing in patients with
risk factors for drug abuse
TRIAGE BASED UPON CERVICAL LENGTH
Cervical length >30 mm These women are at low risk
of PTB,
Regardless of fFN result. Discharge the patients home
after an observational period of four to six hours during
which confirm fetal well-being
Exclude the presence of an acute precipitating event
(eg, an abruption or overt infection),
Follow-up in one to two weeks
Cervical length 20 to 30 mm PTB is more likely in
women with cervices 20 to 30 mm than in women with
longer cervices, but most women in this group do not
deliver preterm. Therefore, send the swab for fFN testing
in this subgroup of women. If the test is positive (level
greater than 50 ng/mL), then actively manage the
pregnancy to prevent morbidity associated with PTB.
Cervical length <20 mm .These women are at high risk
of PTB regardless of fFN result. Therefore, we do not
send their swabs for fFN testing to the laboratory and
actively manage them to prevent morbidity associated
with PTB.
MANAGEMENT OF WOMEN WITH PRETERM LABOR
Hospitalize women diagnosed with PTL at less than 34
weeks of gestation and initiate the following treatments:
Antenatal glucocorticoids to reduce neonatal morbidity and
mortality associated with PTB
Appropriate antibiotics for GBS chemoprophylaxis
Tocolytic drugs for up to 48 hours to delay delivery so that
glucocorticoids given to the mother can achieve their
maximum effect.
Appropriate antibiotics to women with positive urine culture
results or positive tests for gonorrhea or chlamydia.
MANAGEMENT OF ASYMPTOMATIC WOMEN AT HIGH RISK OF PTB
Interventions to prevent PTB generally have not been successful, with some exceptions (eg, supplemental
progesterone).
Women with risk factors for PTB are sometimes followed with serial ultrasound measurement of cervical length. A cervical
length 35 mm is generally considered normal and reassuring; as cervical length decreases below 35 mm, the risk of PTB
increases
We manage asymptomatic patients at high risk of PTB similar to the way we manage symptomatic patients, but with a
higher cervical length threshold for intervention. This minimizes overtreatment of high risk asymptomatic patients and
undertreatment of symptomatic patients. Surveillance with serial cervical length measurements is begun at 22 weeks.
Cervical length 35 mm - The risk of PTB is low. See these patients in routine follow-up in one to two weeks.
Cervical length 25 to 34 mm - obtain a fFN concentration. If the test is positive (level greater than 50 ng/mL), then actively
manage the pregnancy to prevent morbidity associated with PTB.
Cervical length <25 mm - The risk of PTB is increased. We actively manage the pregnancy to prevent morbidity associated
with PTB, as described above.
PREMATURE RUPTURE OF MEMBRANE (PROM)
Etiology & RF
Outcome
Refers to membrane
rupture before the
onset of uterine
contractions; preterm
PROM (PPROM) is the
term used when the
pregnancy is less than
37 completed weeks of
gestation.
PPROM occurs in 3
percent of pregnancies
and is responsible for,
or associated with,
approximately onethird of preterm births.
In management of PPROM,
Points of contention
include:
1. Expectant
management versus
intervention
2. Use of tocolytics
3. Duration of
administration of
antibiotic prophylaxis
4. Timing of
administration of
antenatal
glucocorticoids
The pathogenesis of
PPROM is not
completely understood.
There are multiple
etiologies, mechanical
and physiological, that
probably share a final
common pathway
leading to membrane
rupture.
Risk factors for PPROM
are similar to those for
preterm labor
A history of PPROM in a
previous pregnancy
Genital tract infection
Antepartum bleeding
Cigarette smoking have a
particularly strong
association with PPROM
Although a small
randomized trial suggested
vitamin C
supplementation might
lower the risk of PPROM , a
larger randomized trial in
which both vitamin C and E
were given refuted this
finding and suggested the
risk of PPROM may actually
1.
2.
3.
4.
5.
Approximately one-third of
women with PPROM develop
potentially serious infections,
such as intraamniotic
infection (chorioamnionitis),
endometritis, or septicemia.
Endometritis is more common
after cesarean than vaginal
delivery.
The fetus and neonate are at
greater risk of PPROM-related
morbidity and mortality than
the mother.
The majority of pregnancies
with PPROM deliver preterm
and within one week of
membrane rupture.
Preterm infants are especially
vulnerable to a variety of
problems, such as hyaline
membrane disease,
intraventricular hemorrhage,
periventricular leukomalacia
and other neurologic
sequelae, infection (eg,
sepsis, pneumonia,
meningitis), and necrotizing
enterocolitis. The rates of
these morbidities vary with
PPROM is also
associated with
increased risks of
abruptio placentae and
prolapse of the
umbilical cord. Fetal
malpresentation is
common, given the
preterm gestational age
and the frequent
occurrence of reduced
amniotic fluid volume.
The risk of cord
prolapse is especially
high (11 percent in one
study) in the setting of
both nonvertex fetal
presentation and
PPROM.
Early, severe, prolonged
oligohydramnios can be
associated with
pulmonary hypoplasia,
facial deformation, and
orthopedic
abnormalities. Such
complications are most
likely when membrane
rupture occurs at less
than 23 weeks of
5. Methods of testing for
maternal/fetal infection
6. Timing of delivery.
RF for Pre-term birth
be increased with
antioxidant
supplementation .
gestational age and are
higher in the setting of
chorioamnionitis
gestation.
1. Stress Single women, Low socioeconomic status, Anxiety,
Depression, Life events (divorce, separation,
death)Abdominal surgery during pregnancy
2. Occupational fatigue Upright posture, Use of industrial
machines, Physical exertion, Mental or environmental stress
3. Excessive or impaired uterine distention Multiple
gestationPolyhydramniosUterine anomalyUterine
leiomyomaDiethylstilbestrol
4. Cervical factors History of second trimester
abortionHistory of cervical surgeryPremature cervical
dilatation or effacement
Clinical Manifestation & Dx
5. Infection Sexually transmitted infections,
Pyelonephritis, appendicitis, pneumonia, Systemic
infection, Bacteriuria, Periodontal disease
6. Placental pathology Placenta previa, Abruption,
Vaginal bleeding
7. Miscellaneous Previous preterm delivery, Substance
abuse, SmokingMaternal age (<18 or >40), AfricanAmerican race, Poor nutrition and low body mass index,
Inadequate prenatal care, Anemia (hemoglobin <10
g/dL)Excessive uterine contractility, Low level of
educational achievement, Genotype
8. Fetal factors Congenital anomaly, Growth restriction
History The classic clinical presentation of PPROM is a
sudden "gush" of clear or pale yellow fluid from the vagina.
However, many women describe intermittent or constant
leaking of small amounts of fluid or just a sensation of
wetness within the vagina or on the perineum. A clinical
history suggestive of PPROM should be confirmed by visual
inspection or laboratory tests to exclude other causes of
vaginal/perineal wetness, such as urinary incontinence,
vaginal discharge, and perspiration.
Physical examination The best method of confirming
the diagnosis of PPROM is direct observation of amniotic
fluid coming out of the cervical canal or pooling in the
vaginal fornix. If amniotic fluid is not immediately visible, the
woman can be asked to push on her fundus, Valsalva, or
cough to provoke leakage of amniotic fluid from the cervical
os. Digital examination should be avoided because it may
decrease the latency period (ie, time from rupture of
membranes to delivery) and increase the risk of intrauterine
infection
Nitrazine and fern tests If PROM is not obvious after
visual inspection, the diagnosis can be confirmed by testing
the pH of the vaginal fluid, which is easily accomplished with
nitrazine paper. Amniotic fluid usually has a pH range of 7.0
to 7.3 compared to the normally acidic vaginal pH of 3.8 to4.
False-negative and false-positive nitrazine tests results
occur in up to 5 percent of cases.
False negative tests results can occur when leaking
is intermittent or the amniotic fluid is diluted by other
vaginal fluids. False positive results can be due to the
presence of alkaline fluids in the vagina, such as blood,
seminal fluid, or soap. In addition, the pH of urine can
be elevated to near 8.0 if infected with Proteus species.
In the United Kingdom, an absorbent pad
(AmnioSense) that changes color at pH > 5.2 is used as
a panty liner and marketed to pregnant women. In a
study of 157 pregnant women, the sensitivity and
specificity of this device for diagnosis of membrane
rupture were 98 and 65 percent, respectively
Ultrasonography Ultrasound examination may be
of value in the diagnosis of PPROM. Fifty to 70 percent
of women with PPROM have low amniotic fluid volume
on initial sonography . A mild reduction of amniotic fluid
volume may have many etiologies. On the other hand,
the finding of anhydramnios or severe oligohydramnios,
combined with a characteristic history, is highly
suggestive of rupture of membranes, although renal
agenesis, obstructive uropathy, or severe uteroplacental insufficiency also can cause marked
reductions in amniotic fluid volume.
Instillation of indigo carmine One-half hour later,
the tampon is removed and examined for blue staining,
which indicates leakage of amniotic fluid.
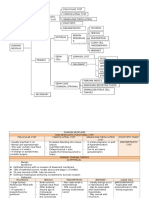
Management
The management of pregnancies complicated by PPROM is based upon
Initial evaluation
Expeditious delivery of women with
consideration of several factors, which are assessed upon presentation
PPROM is indicated if intrauterine
Gestational age
infection, abruptio placentae, repetitive
1. Availability of neonatal intensive care
FHR decelerations, or a high risk of cord
2. Presence or absence of maternal/fetal infection
prolapse is present or suspected
3. Presence or absence of labor
In each of these conditions, fetal well4. Fetal presentation (Breech and transverse lies are unstable and may
being can deteriorate with expectant
increase the risk for cord prolapse)
management, and there are no
5. Fetal heart rate (FHR) tracing pattern
therapeutic interventions available other
6. Likelihood of fetal lung maturity
than delivery.
7. Cervical status (by visual, not digital, inspection unless induction is
planned or the woman is in labor)
Our simplified algorithm for management of other women with PPROM is shown in the
Antenatal glucocorticoids
Maternal surveillance
Antibiotics
Fetal surveillance
Treatment of overt infections
Timing of delivery
Tocolysis
Gestational age <34 weeks In general, prematurity
is the greatest risk to the fetus with PPROM. As
Hospitalization
discussed above, we administer a course of antenatal
Tissue sealants (A variety of tissue sealants (eg, fibrin
glucocorticoids, prophylactic antibiotics for seven
glue, gelatin sponge) have shown some success in
days, and tocolytics for 48 hours, as indicated.
stopping leakage in case reports. Neither the safety nor
the efficacy of these sealants has been established ).
Gestational age greater than 34 weeks
Method of delivery Cesarean delivery is performed
Supplemental progesterone (There is no evidence that
for standard indications; otherwise labor is induced.
administration of supplemental progesterone has any
Favorable Cervix vs Unfavorable cervix
beneficial effects in women with PPROM )
Você também pode gostar
- Ractice Essentials: Reference - Ids - Tool - Tip Reference - IdsDocumento3 páginasRactice Essentials: Reference - Ids - Tool - Tip Reference - IdsYoan Caroline Saron KapressyAinda não há avaliações
- Tocolytics (Also Called Anti-Contraction Medications or Labor Represents) AreDocumento2 páginasTocolytics (Also Called Anti-Contraction Medications or Labor Represents) AreEric RothAinda não há avaliações
- 3.1 Pprom ShangrilaDocumento31 páginas3.1 Pprom Shangrilaintan.obgAinda não há avaliações
- PREMATURITASDocumento34 páginasPREMATURITASperiAinda não há avaliações
- PRETERM DELIVERY With NARRATIONDocumento23 páginasPRETERM DELIVERY With NARRATIONamanda deonananAinda não há avaliações
- Preterm Premature Rupture of Membranes (PPROM) - Assessment and Management GuidelineDocumento6 páginasPreterm Premature Rupture of Membranes (PPROM) - Assessment and Management GuidelineAlexis LambertAinda não há avaliações
- Premature Rupture of MembranesDocumento33 páginasPremature Rupture of MembranesSarang Lee100% (1)
- PPROMDocumento63 páginasPPROMSaraMohammedAinda não há avaliações
- Postterm PregnancyDocumento27 páginasPostterm PregnancyChayanika KumarAinda não há avaliações
- INTRODUCTIO1Documento10 páginasINTRODUCTIO1Diane ChuAinda não há avaliações
- Rupture of Membranes Preterm Premature Pprom 220719Documento5 páginasRupture of Membranes Preterm Premature Pprom 220719MuathAinda não há avaliações
- Diagnosis of Preterm Labor and Overview of Preterm BirthDocumento15 páginasDiagnosis of Preterm Labor and Overview of Preterm BirthKenny IncsAinda não há avaliações
- Management Ectopic Pregnancy SLCOGDocumento9 páginasManagement Ectopic Pregnancy SLCOGMelissa Aina Mohd YusofAinda não há avaliações
- Prom 1Documento48 páginasProm 1Tesfahun TekleAinda não há avaliações
- Preterm Labour: Introduction and Causes by Humna AnisDocumento19 páginasPreterm Labour: Introduction and Causes by Humna AnisManjunath VankadariAinda não há avaliações
- 18 PromDocumento8 páginas18 PromRyubusa HayabusaAinda não há avaliações
- Longitud CervicalDocumento5 páginasLongitud CervicalSaul Ignacio SuarezAinda não há avaliações
- 8) PROM - and PTBDocumento38 páginas8) PROM - and PTBmameekasim75Ainda não há avaliações
- Elizabeth G. Querubin BSN 3E1-9 - Group 195 A Ectopic PregnancyDocumento16 páginasElizabeth G. Querubin BSN 3E1-9 - Group 195 A Ectopic PregnancyLizeth Querubin97% (38)
- Preterm LaborDocumento62 páginasPreterm LaborAstri Sri Widiastuty100% (1)
- Protocol Book For OBGYNDocumento41 páginasProtocol Book For OBGYNShabir BadakhshAinda não há avaliações
- High Risk PregnancyDocumento44 páginasHigh Risk PregnancyKavipriyaAinda não há avaliações
- 1 MiscarriageDocumento34 páginas1 Miscarriagezxcvbzaki123Ainda não há avaliações
- Premature Rupture of MembraneDocumento5 páginasPremature Rupture of MembraneEspiritu, ChriscelAinda não há avaliações
- Preterm LaborDocumento29 páginasPreterm LaborBer AnneAinda não há avaliações
- Prolonged PregnancyDocumento40 páginasProlonged Pregnancyjan caraAinda não há avaliações
- Current Concepts in The Management of Premature Rupture of The MembranesDocumento21 páginasCurrent Concepts in The Management of Premature Rupture of The MembranesWike UbayAinda não há avaliações
- Preterm LaborDocumento19 páginasPreterm LaborPrily RillyAinda não há avaliações
- Prolonged PregnancyDocumento41 páginasProlonged PregnancyArif Febrianto100% (1)
- Lecture IV IIIDocumento32 páginasLecture IV IIIMohamad Alsayed AlasaasAinda não há avaliações
- Postterm Pregnancy and IUFDDocumento24 páginasPostterm Pregnancy and IUFDNejib M/AminAinda não há avaliações
- 10 The Role of Routine Cervical Length Screening in Selected High - and Low-Risk Women For Preterm Birth PreventionDocumento6 páginas10 The Role of Routine Cervical Length Screening in Selected High - and Low-Risk Women For Preterm Birth PreventionWailea Faye SalvaAinda não há avaliações
- Causes of Fetal DeathDocumento3 páginasCauses of Fetal DeathRene Cordova InapanAinda não há avaliações
- EctopicDocumento42 páginasEctopicSafana NazeerAinda não há avaliações
- Gyno... PTL & PRODocumento30 páginasGyno... PTL & PROhailemichael chekolAinda não há avaliações
- Antepartum & Postpartum HemorrhageDocumento68 páginasAntepartum & Postpartum HemorrhageZee YongAinda não há avaliações
- Preterm Labor-1Documento28 páginasPreterm Labor-1tajfaiz779Ainda não há avaliações
- Preterm Labor and Prelabor Rupture of Membranes (Documento35 páginasPreterm Labor and Prelabor Rupture of Membranes (Gendis Giona SudjaAinda não há avaliações
- Pelvic Inflammatory Disease (PID) Chlamydia GonorrheaDocumento19 páginasPelvic Inflammatory Disease (PID) Chlamydia GonorrheaanneAinda não há avaliações
- 14 Abortion Noted PDFDocumento37 páginas14 Abortion Noted PDFmohammed farajiAinda não há avaliações
- Rcog PpromDocumento7 páginasRcog PpromDevi SyamAinda não há avaliações
- Preterm LaborDocumento41 páginasPreterm LaborAdistri Kim100% (3)
- PediatriDocumento7 páginasPediatriKijang 2018Ainda não há avaliações
- Premature Ruptured of Membrane: Ferdian GunawanDocumento29 páginasPremature Ruptured of Membrane: Ferdian GunawanSandra SudargoAinda não há avaliações
- Prolonged PregnancyDocumento41 páginasProlonged PregnancyPratiwi Anggun LestariningrumAinda não há avaliações
- BRN MN 21 01 Guideline 2013 Eng Management Preterm Prelabour Rupture MembranesDocumento3 páginasBRN MN 21 01 Guideline 2013 Eng Management Preterm Prelabour Rupture Membranesd99452727Ainda não há avaliações
- Ectopic Pregnancy: N Engl J Med 2009 361:379-87Documento25 páginasEctopic Pregnancy: N Engl J Med 2009 361:379-87Muhammad AbeeshAinda não há avaliações
- Assigment د امل خليفهDocumento5 páginasAssigment د امل خليفهShimaa Abdel hameedAinda não há avaliações
- Ob AbbrevDocumento12 páginasOb Abbrevth233Ainda não há avaliações
- S Preterm Birth and PromDocumento6 páginasS Preterm Birth and PromThembeka MbathaAinda não há avaliações
- Premature Rupture of MembranesDocumento38 páginasPremature Rupture of MembranesArwa QishtaAinda não há avaliações
- Obgyn Ob PRPM Pt1 13Documento6 páginasObgyn Ob PRPM Pt1 13SalmonteAinda não há avaliações
- AsdasfasfvDocumento7 páginasAsdasfasfvPulseWangminAinda não há avaliações
- Abortion ZeleDocumento49 páginasAbortion ZeleZelalem DawitAinda não há avaliações
- Case Presentation OnppromDocumento44 páginasCase Presentation Onppromocean329100% (1)
- Preterm LaborDocumento9 páginasPreterm LaborMelonie VIAinda não há avaliações
- IUFDDocumento29 páginasIUFDfasyanneshaAinda não há avaliações
- USMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsNo EverandUSMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsNota: 5 de 5 estrelas5/5 (9)
- Treatment Strategy for Unexplained Infertility and Recurrent MiscarriageNo EverandTreatment Strategy for Unexplained Infertility and Recurrent MiscarriageKeiji KurodaAinda não há avaliações
- Obsandgyne Tables 200pagesDocumento221 páginasObsandgyne Tables 200pagesRashed ShatnawiAinda não há avaliações
- Belle-Premature Rupture of MembraneDocumento5 páginasBelle-Premature Rupture of MembraneRashed ShatnawiAinda não há avaliações
- Belle Vaginal DischargeDocumento12 páginasBelle Vaginal DischargeRashed ShatnawiAinda não há avaliações
- Belle RH IsoimmunizationDocumento3 páginasBelle RH IsoimmunizationRashed ShatnawiAinda não há avaliações
- Belle-Fetal Growth AssessmentDocumento10 páginasBelle-Fetal Growth AssessmentRashed ShatnawiAinda não há avaliações
- IM NotesDocumento74 páginasIM NotesRashed ShatnawiAinda não há avaliações
- Belle STDDocumento8 páginasBelle STDRashed ShatnawiAinda não há avaliações
- Belle Sga IugrDocumento6 páginasBelle Sga IugrRashed ShatnawiAinda não há avaliações
- Belle PuerperiumDocumento11 páginasBelle PuerperiumRashed ShatnawiAinda não há avaliações
- Belle PreTerm Labor PROMDocumento3 páginasBelle PreTerm Labor PROMRashed ShatnawiAinda não há avaliações
- Belle Shoulder DystociaDocumento2 páginasBelle Shoulder DystociaRashed ShatnawiAinda não há avaliações
- Belle Prolonged PregnancyDocumento2 páginasBelle Prolonged PregnancyRashed ShatnawiAinda não há avaliações
- Belle PuerperiumDocumento10 páginasBelle PuerperiumRashed ShatnawiAinda não há avaliações
- Belle Infertility Management ARTDocumento6 páginasBelle Infertility Management ARTRashed ShatnawiAinda não há avaliações
- (Belle) MalpresentationDocumento4 páginas(Belle) MalpresentationAray Al-AfiqahAinda não há avaliações
- Belle-Preterm Labour ManagementDocumento4 páginasBelle-Preterm Labour ManagementRashed ShatnawiAinda não há avaliações
- Belle PPHDocumento4 páginasBelle PPHRashed ShatnawiAinda não há avaliações
- Belle Ovarian NeoplasmDocumento6 páginasBelle Ovarian NeoplasmRashed ShatnawiAinda não há avaliações
- Belle Malignant Lesions of The Body of UterusDocumento2 páginasBelle Malignant Lesions of The Body of UterusRashed ShatnawiAinda não há avaliações
- Belle Preinvasive Invasive Cervical DiseaseDocumento5 páginasBelle Preinvasive Invasive Cervical DiseaseRashed ShatnawiAinda não há avaliações
- Belle PIDDocumento2 páginasBelle PIDRashed ShatnawiAinda não há avaliações
- Belle Medical Disorders in PregnancyDocumento4 páginasBelle Medical Disorders in PregnancyRashed ShatnawiAinda não há avaliações
- Belle Multiple GestationsDocumento2 páginasBelle Multiple GestationsRashed ShatnawiAinda não há avaliações
- Belle MenopauseDocumento7 páginasBelle MenopauseRashed ShatnawiAinda não há avaliações
- Belle-Drugs in PregnancyDocumento17 páginasBelle-Drugs in PregnancyRashed ShatnawiAinda não há avaliações
- Belle Hypertensive Disorders in PregnancyDocumento6 páginasBelle Hypertensive Disorders in PregnancyRashed ShatnawiAinda não há avaliações
- Belle Induction of LaborDocumento5 páginasBelle Induction of LaborRashed ShatnawiAinda não há avaliações
- Belle Instruments For OGDocumento1 páginaBelle Instruments For OGRashed ShatnawiAinda não há avaliações
- Belle-Gestational Diabetes MellitusDocumento4 páginasBelle-Gestational Diabetes MellitusRashed ShatnawiAinda não há avaliações
- Translations Telugu To English A ClassifDocumento111 páginasTranslations Telugu To English A ClassifGummadi Vijaya KumarAinda não há avaliações
- Net Pert: Cable QualifierDocumento4 páginasNet Pert: Cable QualifierAndrés Felipe Fandiño MAinda não há avaliações
- White Cataract What To AssesDocumento2 páginasWhite Cataract What To Assesalif andraAinda não há avaliações
- Note Hand-Soldering eDocumento8 páginasNote Hand-Soldering emicpreampAinda não há avaliações
- Types of Intermolecular ForcesDocumento34 páginasTypes of Intermolecular ForcesRuschan JaraAinda não há avaliações
- Kamal: Sales and Marketing ProfessionalDocumento3 páginasKamal: Sales and Marketing ProfessionalDivya NinaweAinda não há avaliações
- State Farm Claims: PO Box 52250 Phoenix AZ 85072-2250Documento2 páginasState Farm Claims: PO Box 52250 Phoenix AZ 85072-2250georgia ann polley-yatesAinda não há avaliações
- Resa Auditing Theorydocx - CompressDocumento64 páginasResa Auditing Theorydocx - CompressMaeAinda não há avaliações
- Phenomenology of The SelfDocumento5 páginasPhenomenology of The SelfGuilherme CastelucciAinda não há avaliações
- Understanding Culture Society, and PoliticsDocumento3 páginasUnderstanding Culture Society, and PoliticsVanito SwabeAinda não há avaliações
- Review and Basic Principles of PreservationDocumento43 páginasReview and Basic Principles of PreservationKarl Marlou Bantaculo100% (1)
- A Tall Order - Cooling Dubai's Burj Khalifa: FeatureDocumento2 páginasA Tall Order - Cooling Dubai's Burj Khalifa: FeatureMohsin KhanAinda não há avaliações
- Teambinder Product BrochureDocumento7 páginasTeambinder Product BrochurePrinceAinda não há avaliações
- Dashboard - Reveal Math, Grade 4 - McGraw HillDocumento1 páginaDashboard - Reveal Math, Grade 4 - McGraw HillTijjani ShehuAinda não há avaliações
- Small Business and Entrepreneurship ProjectDocumento38 páginasSmall Business and Entrepreneurship ProjectMădălina Elena FotacheAinda não há avaliações
- Learning Module - Joints, Taps and SplicesDocumento9 páginasLearning Module - Joints, Taps and SplicesCarlo Cartagenas100% (1)
- 2012 Conference NewsfgfghsfghsfghDocumento3 páginas2012 Conference NewsfgfghsfghsfghabdAinda não há avaliações
- Landcorp FLCC Brochure 2013 v3Documento6 páginasLandcorp FLCC Brochure 2013 v3Shadi GarmaAinda não há avaliações
- Programming MillDocumento81 páginasProgramming MillEddy ZalieAinda não há avaliações
- Exercise-3 (B) : Linear EquationsDocumento3 páginasExercise-3 (B) : Linear EquationsVRUSHABHAinda não há avaliações
- Assignment 4 Job Order Costing - ACTG321 - Cost Accounting and Cost ManagementDocumento3 páginasAssignment 4 Job Order Costing - ACTG321 - Cost Accounting and Cost ManagementGenithon PanisalesAinda não há avaliações
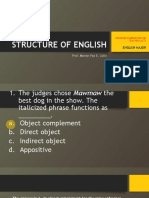
- LET-English-Structure of English-ExamDocumento57 páginasLET-English-Structure of English-ExamMarian Paz E Callo80% (5)
- Volcano Lesson PlanDocumento5 páginasVolcano Lesson Planapi-294963286Ainda não há avaliações
- Early Christian ArchitectureDocumento38 páginasEarly Christian ArchitectureInspirations & ArchitectureAinda não há avaliações
- Alto Hotel Melbourne GreenDocumento2 páginasAlto Hotel Melbourne GreenShubham GuptaAinda não há avaliações
- Pepperberg Notes On The Learning ApproachDocumento3 páginasPepperberg Notes On The Learning ApproachCristina GherardiAinda não há avaliações
- Categories of Cargo and Types of ShipsDocumento14 páginasCategories of Cargo and Types of ShipsVibhav Kumar100% (1)
- Course Outline Cbmec StratmgtDocumento2 páginasCourse Outline Cbmec StratmgtskyieAinda não há avaliações
- General Characteristics of Phonemes: Aspects of Speech SoundsDocumento8 páginasGeneral Characteristics of Phonemes: Aspects of Speech SoundsElina EkimovaAinda não há avaliações
- Fall 3050 SyllabusDocumento6 páginasFall 3050 Syllabustaher91Ainda não há avaliações