Escolar Documentos
Profissional Documentos
Cultura Documentos
American Thoracic Society - Interpretation of Arterial Blood Gases (ABGs)
Enviado por
humberto_2Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
American Thoracic Society - Interpretation of Arterial Blood Gases (ABGs)
Enviado por
humberto_2Direitos autorais:
Formatos disponíveis
16/7/2016
AmericanThoracicSocietyInterpretationofArterialBloodGases(ABGs)
Clinical Education
Home (/) Professionals (../../../index.php) Clinical Resources (../../index.php) Critical Care (../index.php) Clinical
Education (index.php) Interpretation of ABGs
Submenu
Interpretation of ABGs
Interpretation of Arterial Blood Gases (ABGs)
David A. Kaufman, MD
Chief, Section of Pulmonary, Critical Care & Sleep Medicine
Bridgeport Hospital-Yale New Haven Health
Assistant Clinical Professor, Yale University School of Medicine
(Section of Pulmonary & Critical Care Medicine)
Introduction:
Interpreting an arterial blood gas (ABG) is a crucial skill for physicians, nurses, respiratory therapists,
and other health care personnel. ABG interpretation is especially important in critically ill patients.
The following six-step process helps ensure a complete interpretation of every ABG. In addition, you
will nd tables that list commonly encountered acid-base disorders.
Many methods exist to guide the interpretation of the ABG. This discussion does not include some
methods, such as analysis of base excess or Stewarts strong ion dierence. A summary of these
techniques can be found in some of the suggested articles. It is unclear whether these alternate
methods oer clinically important advantages over the presented approach, which is based on the
anion gap.
6-step approach:
Step 1: Assess the internal consistency of the values using the Henderseon-Hasselbach equation:
[H+] = 24(PaCO2)
[HCO3-]
If the pH and the [H+] are inconsistent, the ABG is probably not valid.
pH
https://www.thoracic.org/professionals/clinicalresources/criticalcare/clinicaleducation/abgs.php?platform=hootsuite
1/7
16/7/2016
AmericanThoracicSocietyInterpretationofArterialBloodGases(ABGs)
Approximate [H+]
(mmol/L)
7.00
100
7.05
89
7.10
79
7.15
71
7.20
63
7.25
56
7.30
50
7.35
45
7.40
40
7.45
35
7.50
32
7.55
28
7.60
25
7.65
22
Step 2: Is there alkalemia or acidemia present?
pH < 7.35 acidemia
pH > 7.45 alkalemia
This is usually the primary disorder
Remember: an acidosis or alkalosis may be present even if the pH is in the normal range (7.35
7.45)
https://www.thoracic.org/professionals/clinicalresources/criticalcare/clinicaleducation/abgs.php?platform=hootsuite
2/7
16/7/2016
AmericanThoracicSocietyInterpretationofArterialBloodGases(ABGs)
You will need to check the PaCO2, HCO3- and anion gap
Step 3: Is the disturbance respiratory or metabolic? What is the relationship between the direction of
change in the pH and the direction of change in the PaCO2? In primary respiratory disorders, the pH
and PaCO2 change in opposite directions; in metabolic disorders the pH and PaCO2 change in the same
direction.
Acidosis
Respiratory
pH
PaCO2
Acidosis
Metabolic&
pH
PaCO2
Alkalosis
Respiratory
pH
PaCO2
Alkalosis
Metabolic
pH
PaCO2
Step 4: Is there appropriate compensation for the primary disturbance? Usually, compensation does
not return the pH to normal (7.35 7.45).
Disorder
Expected compensation
Correction
factor
Metabolic acidosis
PaCO2 = (1.5 x [HCO3-]) +8
Acute respiratory acidosis
Increase in [HCO3-]= PaCO2/10
Chronic respiratory acidosis (3-5
Increase in [HCO3-]= 3.5( PaCO2/10)
Metabolic alkalosis
Increase in PaCO2 = 40 + 0.6(HCO3-)
Acute respiratory alkalosis
Decrease in [HCO3-]= 2( PaCO2/10)
Chronic respiratory alkalosis
Decrease in [HCO3-] = 5( PaCO2/10) to
days)
7( PaCO2/10)
If the observed compensation is not the expected compensation, it is likely that more than one acidbase disorder is present.
Step 5: Calculate the anion gap (if a metabolic acidosis exists): AG= [Na+]-( [Cl-] + [HCO3-] )-12 2
https://www.thoracic.org/professionals/clinicalresources/criticalcare/clinicaleducation/abgs.php?platform=hootsuite
3/7
16/7/2016
AmericanThoracicSocietyInterpretationofArterialBloodGases(ABGs)
A normal anion gap is approximately 12 meq/L.
In patients with hypoalbuminemia, the normal anion gap is lower than 12 meq/L; the normal
anion gap in patients with hypoalbuminemia is about 2.5 meq/L lower for each 1 gm/dL decrease
in the plasma albumin concentration (for example, a patient with a plasma albumin of 2.0 gm/dL
would be approximately 7 meq/L.)
If the anion gap is elevated, consider calculating the osmolal gap in compatible clinical situations.
Elevation in AG is not explained by an obvious case (DKA, lactic acidosis, renal failure
Toxic ingestion is suspected
OSM gap = measured OSM (2[Na+] - glucose/18 BUN/2.8
The OSM gap should be < 10
Step 6: If an increased anion gap is present, assess the relationship between the increase in the anion
gap and the decrease in [HCO3-].
Assess the ratio of the change in the anion gap (AG ) to the change in [HCO3-] ([HCO3-]): AG/
[HCO3-]
This ratio should be between 1.0 and 2.0 if an uncomplicated anion gap metabolic acidosis is present.
If this ratio falls outside of this range, then another metabolic disorder is present:
If AG/[HCO3-] < 1.0, then a concurrent non-anion gap metabolic acidosis is likely to be present.
If AG/[HCO3-] > 2.0, then a concurrent metabolic alkalosis is likely to be present.
It is important to remember what the expected normal anion gap for your patient should be, by
adjusting for hypoalbuminemia (see Step 5, above.)
Table 1: Characteristics of acid-base disturbances
Disorder
pH
Primary problem
Compensation
Metabolic acidosis
in HCO3-
in PaCO2
Metabolic alkalosis
in HCO3-
in PaCO2
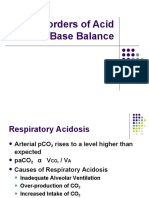
Respiratory acidosis
in PaCO2
in [HCO3-]
Respiratory alkalosis
in PaCO2
in [HCO3-]
Table 2: Selected etiologies of respiratory acidosis
Airway obstruction
https://www.thoracic.org/professionals/clinicalresources/criticalcare/clinicaleducation/abgs.php?platform=hootsuite
4/7
16/7/2016
AmericanThoracicSocietyInterpretationofArterialBloodGases(ABGs)
- Upper
- Lower
COPD
asthma
other obstructive lung disease
CNS depression
Sleep disordered breathing (OSA or OHS)
Neuromuscular impairment
Ventilatory restriction
Increased CO2 production: shivering, rigors, seizures, malignant hyperthermia, hypermetabolism,
increased intake of carbohydrates
Incorrect mechanical ventilation settings
Table 3: Selected etiologies of respiratory alkalosis
CNS stimulation: fever, pain, fear, anxiety, CVA, cerebral edema, brain trauma, brain tumor, CNS
infection
Hypoxemia or hypoxia: lung disease, profound anemia, low FiO2
Stimulation of chest receptors: pulmonary edema, pleural eusion, pneumonia, pneumothorax,
pulmonary embolus
Drugs, hormones: salicylates, catecholamines, medroxyprogesterone, progestins
Pregnancy, liver disease, sepsis, hyperthyroidism
Incorrect mechanical ventilation settings
Table 4: Selected causes of metabolic alkalosis
Hypovolemia with Cl- depletion
GI loss of H+
Vomiting, gastric suction, villous adenoma, diarrhea with chloride-rich uid
Renal loss H+
Loop and thiazide diuretics, post-hypercapnia (especially after institution of
mechanical ventilation)
Hypervolemia, Cl- expansion
Renal loss of H+: edematous states (heart failure, cirrhosis, nephrotic syndrome),
https://www.thoracic.org/professionals/clinicalresources/criticalcare/clinicaleducation/abgs.php?platform=hootsuite
5/7
16/7/2016
AmericanThoracicSocietyInterpretationofArterialBloodGases(ABGs)
hyperaldosteronism, hypercortisolism, excess ACTH, exogenous steroids, hyperreninemia,
severe hypokalemia, renal artery stenosis, bicarbonate administration
Table 5: Selected etiologies of metabolic acidosis
Elevated anion gap:
Methanol intoxication
Uremia
Diabetic ketoacidosisa, alcoholic ketoacidosis, starvation ketoacidosis
Paraldehyde toxicity
Isoniazid
Lactic acidosisa
Type A: tissue ischemia
Type B: Altered cellular metabolism
Ethanolb or ethylene glycolb intoxication
Salicylate intoxication
a
Most common causes of metabolic acidosis with an elevated anion gap
Frequently associated with an osmolal gap
Normal anion gap: will have increase in [Cl-]
GI loss of HCO3Diarrhea, ileostomy, proximal colostomy, ureteral diversion
Renal loss of HCO3proximal RTA
carbonic anhydrase inhibitor (acetazolamide)
Renal tubular disease
ATN
Chronic renal disease
Distal RTA
Aldosterone inhibitors or absence
NaCl infusion, TPN, NH4+ administration
Table 6: Selected mixed and complex acid-base disturbances
Disorder
Respiratory acidosis with
metabolic acidosis
Characteristics
Selected situations
Cardiac arrest
Intoxications
Multi-organ failure
https://www.thoracic.org/professionals/clinicalresources/criticalcare/clinicaleducation/abgs.php?platform=hootsuite
6/7
16/7/2016
AmericanThoracicSocietyInterpretationofArterialBloodGases(ABGs)
in pH
in HCO3
in PaCO2
Respiratory alkalosis with
in pH
metabolic alkalosis
in HCO3-
in PaCO2
Cirrhosis with diuretics
Pregnancy with vomiting
Over ventilation of COPD
Respiratory acidosis with
pH in normal range
metabolic alkalosis
in PaCO2,
in HCO3-
COPD with diuretics, vomiting, NG
suction
Severe hypokalemia
Respiratory alkalosis with
pH in normal range
metabolic acidosis
in PaCO2
in HCO3
Metabolic acidosis with
pH in normal range
metabolic alkalosis
HCO3- normal
Sepsis
Salicylate toxicity
Renal failure with CHF or
pneumonia
Advanced liver disease
Uremia or ketoacidosis with
vomiting, NG suction, diuretics, etc.
Suggested additional reading:
Rose, B.D. and T.W. Post. Clinical physiology of acid-base and electrolyte disorders, 5th ed. New York:
McGraw Hill Medical Publishing Division, c2001.
Fidkowski, C And J. Helstrom. Diagnosing metabolic acidosis in the critically ill: bridging the anion
gap, Stewart and base excess methods. Can J Anesth 2009;56:247-256.
Adrogu, H.J. and N.E. Madias. Management of life-threatening acid-base disordersrst of two
parts. N Engl J Med 1998;338:26-34.
Adrogu, H.J. and N.E. Madias. Management of life-threatening acid-base disorderssecond of
two parts. N Engl J Med 1998;338:107-111.
https://www.thoracic.org/professionals/clinicalresources/criticalcare/clinicaleducation/abgs.php?platform=hootsuite
7/7
Você também pode gostar
- MEDICINE DAMS: A CONCISE OVERVIEW OF THE CARDIOVASCULAR SYSTEMDocumento657 páginasMEDICINE DAMS: A CONCISE OVERVIEW OF THE CARDIOVASCULAR SYSTEMSubhashAinda não há avaliações
- Interpretation of Arterial Blood GasesDocumento5 páginasInterpretation of Arterial Blood GasesRiska PashaAinda não há avaliações
- Arterial Blood Gas InterpretationsDocumento7 páginasArterial Blood Gas InterpretationsErin TraversAinda não há avaliações
- Interpreting ABGs in 6 stepsDocumento16 páginasInterpreting ABGs in 6 stepsRuby Ann Cañero HigoyAinda não há avaliações
- Interpretation of Arterial Blood Gases (ABGs)Documento6 páginasInterpretation of Arterial Blood Gases (ABGs)afalfitraAinda não há avaliações
- Interpreting ABGs: A 6-Step ApproachDocumento7 páginasInterpreting ABGs: A 6-Step ApproachGaby FernándezAinda não há avaliações
- Critical Care Clinical Education: Interpretation of ABGsDocumento8 páginasCritical Care Clinical Education: Interpretation of ABGsRumela Ganguly ChakrabortyAinda não há avaliações
- Interpretation of Arterial Blood Gases (Abgs) I David A. Kaufman, MD DDocumento17 páginasInterpretation of Arterial Blood Gases (Abgs) I David A. Kaufman, MD DingridpuspitaAinda não há avaliações
- ABG Interpretation - ATSDocumento5 páginasABG Interpretation - ATSHAMMYER ALROKHAMIAinda não há avaliações
- American Thoracic Society - Interpretation of Arterial Blood Gases (ABGs)Documento8 páginasAmerican Thoracic Society - Interpretation of Arterial Blood Gases (ABGs)muhammadridhwanAinda não há avaliações
- Interpretation of ABGs ATSDocumento6 páginasInterpretation of ABGs ATSjayson2708Ainda não há avaliações
- Acid-Base Made EasyDocumento14 páginasAcid-Base Made EasyMayer Rosenberg100% (10)
- Abg InterpretationDocumento7 páginasAbg InterpretationPreetha PAAinda não há avaliações
- Interpretasi AGDDocumento129 páginasInterpretasi AGDIta SobaAinda não há avaliações
- Interpretasi ABGDocumento5 páginasInterpretasi ABGNella Rosyalina DamayantiAinda não há avaliações
- Acid Base Disorders JAPIDocumento5 páginasAcid Base Disorders JAPIVitrag_Shah_1067Ainda não há avaliações
- H + Hco H Co H Ol + CO (G) : Acid-Base BalanceDocumento7 páginasH + Hco H Co H Ol + CO (G) : Acid-Base BalanceAndreas NatanAinda não há avaliações
- Arterial Blood Gas AnalysisDocumento28 páginasArterial Blood Gas Analysishendra_darmawan_4Ainda não há avaliações
- 2014-02-17 Acid Base Physiology and ABG Interpretation PDFDocumento149 páginas2014-02-17 Acid Base Physiology and ABG Interpretation PDFIva Dewi Permata PhilyAinda não há avaliações
- Arterial Blood Gas Interpretation: Joseph Brian L. Costiniano, MD, DPCPDocumento39 páginasArterial Blood Gas Interpretation: Joseph Brian L. Costiniano, MD, DPCPevbptrprnrmAinda não há avaliações
- Arterial Blood Gas Interpretation: Joseph Brian L. Costiniano, MD, DPCPDocumento39 páginasArterial Blood Gas Interpretation: Joseph Brian L. Costiniano, MD, DPCPGio Tamaño BalisiAinda não há avaliações
- Acid Base BalanceDocumento9 páginasAcid Base BalanceNawarajendra MunakarmiAinda não há avaliações
- Michael Chansky Acid Base Made Easy HandoutDocumento18 páginasMichael Chansky Acid Base Made Easy HandoutTeguh RamadhanAinda não há avaliações
- Interpretation of Abgs: Sophie TatishviliDocumento14 páginasInterpretation of Abgs: Sophie Tatishvilimashe1Ainda não há avaliações
- Acid-Base Regulation and Disorders: Key ConceptsDocumento54 páginasAcid-Base Regulation and Disorders: Key ConceptsPaolo Uccello100% (1)
- 4 Acid Base Disorder 2021Documento81 páginas4 Acid Base Disorder 2021SHIKUR YASINAinda não há avaliações
- Pneumonia - Kyphoscoliosis - Morbid Obesity - Drug OverdoseDocumento3 páginasPneumonia - Kyphoscoliosis - Morbid Obesity - Drug OverdoseJessica nonyeAinda não há avaliações
- Acid Base Disorders Peter SehaDocumento29 páginasAcid Base Disorders Peter SehaPeter SehaAinda não há avaliações
- Acid-Base Homeostasis: Dr. Abeer KhurshidDocumento42 páginasAcid-Base Homeostasis: Dr. Abeer Khurshidسلة فواكة100% (2)
- ABG ANALYSISDocumento74 páginasABG ANALYSISArunAinda não há avaliações
- So What Does The Blood Gas Analysis Actually Measure?Documento12 páginasSo What Does The Blood Gas Analysis Actually Measure?Veterinarska Bolnica Zavetišče BrežiceAinda não há avaliações
- Blood Gas Analysis CMEDocumento12 páginasBlood Gas Analysis CMEpierhot_11Ainda não há avaliações
- Nikko Angelo P. Alcala, MD 2 Year ARODDocumento8 páginasNikko Angelo P. Alcala, MD 2 Year ARODAnna MarieAinda não há avaliações
- Blood Gas TestDocumento6 páginasBlood Gas TestyudhafpAinda não há avaliações
- Background: Henderson-Hasselbalch Approach To Acid/base PhysiologyDocumento11 páginasBackground: Henderson-Hasselbalch Approach To Acid/base PhysiologyErida Prifti100% (1)
- Overview of Acid-Base and Electrolyte Disorders: The Right Clinical Information, Right Where It's NeededDocumento14 páginasOverview of Acid-Base and Electrolyte Disorders: The Right Clinical Information, Right Where It's NeededNelvinBaezMelendrezAinda não há avaliações
- BiochemistryDocumento33 páginasBiochemistryamhhospital0Ainda não há avaliações
- Acid Base DisordersDocumento5 páginasAcid Base DisordersMillenial VoiceAinda não há avaliações
- Interpreting ABG - An Interative Session: Dr. Manjunath Patil Professor, Dept. of Anaesthesiology J.N.Medical CollegeDocumento31 páginasInterpreting ABG - An Interative Session: Dr. Manjunath Patil Professor, Dept. of Anaesthesiology J.N.Medical CollegeMadhan Mohan Reddy KatikareddyAinda não há avaliações
- Asidosis Metabolik PDFDocumento6 páginasAsidosis Metabolik PDFafifurrahman_rizalAinda não há avaliações
- Basics of Acid-Base Balance: When It Comes To Acids and Bases, The Difference Between Life and Death IsDocumento5 páginasBasics of Acid-Base Balance: When It Comes To Acids and Bases, The Difference Between Life and Death IsAyaz Ahmed BrohiAinda não há avaliações
- 66 Part 1Documento10 páginas66 Part 1Dinu Tiberiu GeorgeAinda não há avaliações
- Abg PPT NewDocumento69 páginasAbg PPT NewMalaka Atapattu100% (2)
- Acid Base BalanceDocumento45 páginasAcid Base BalanceSameer Ul BashirAinda não há avaliações
- Detect and correct acid-base imbalancesDocumento6 páginasDetect and correct acid-base imbalancesjohnkuysAinda não há avaliações
- Understanding acid-base balance: Interpret values and steady a disturbed equilibriumDocumento3 páginasUnderstanding acid-base balance: Interpret values and steady a disturbed equilibriumYuniParaditaDjunaidi100% (1)
- Acid BaseDocumento33 páginasAcid BaseParvathy R NairAinda não há avaliações
- "Blood Gas Analysis in A Nutshell: DR Anshuman MishraDocumento28 páginas"Blood Gas Analysis in A Nutshell: DR Anshuman MishraMinaz PatelAinda não há avaliações
- How To Interpret Arterial Blood Gas ResultsDocumento9 páginasHow To Interpret Arterial Blood Gas ResultsteleasadgramAinda não há avaliações
- Acidosis Metabolica 2015 PDFDocumento18 páginasAcidosis Metabolica 2015 PDFGUADALUPE ARANDA OSORIOAinda não há avaliações
- Acid Base BalanceDocumento11 páginasAcid Base BalancePrince Rener Velasco PeraAinda não há avaliações
- Acid Base PhysiologyDocumento4 páginasAcid Base PhysiologyGhadeer EbraheemAinda não há avaliações
- The Acid Base Balance: Faculty of Medicine Anesthesia and Intensive Care DepartmentDocumento36 páginasThe Acid Base Balance: Faculty of Medicine Anesthesia and Intensive Care DepartmentCamelia A. ParuschiAinda não há avaliações
- LRP CriticalCare Sample2Documento46 páginasLRP CriticalCare Sample2Aniket ChoudharyAinda não há avaliações
- BSAVA - Interpretation of Arterial Blood Gas - VINDocumento5 páginasBSAVA - Interpretation of Arterial Blood Gas - VINvetthamilAinda não há avaliações
- Acido BaseDocumento10 páginasAcido Basebenitez1228Ainda não há avaliações
- Metabolic Acid-Base DisordersDocumento14 páginasMetabolic Acid-Base DisordersAlan Espíndola CruzAinda não há avaliações
- Arterial Blood Gas Analysis ExplainedDocumento52 páginasArterial Blood Gas Analysis Explainedimranqazi11Ainda não há avaliações
- 12-Lead ECG Placement GuideDocumento9 páginas12-Lead ECG Placement GuideFalusi Blessing OlaideAinda não há avaliações
- Semen AnalysisDocumento2 páginasSemen AnalysisSabir KamalAinda não há avaliações
- Anemia: Differential DiagnosisDocumento7 páginasAnemia: Differential DiagnosisZaman MigozaradAinda não há avaliações
- Congenital Talipes Equino-Varus (Congenital Clubfoot) : Prof. Sohail Iqbal Sheikh Hod/Orthopaedics Iimct/PrhDocumento66 páginasCongenital Talipes Equino-Varus (Congenital Clubfoot) : Prof. Sohail Iqbal Sheikh Hod/Orthopaedics Iimct/Prhawaisjinnah100% (1)
- 12-Channel ECG SpecsDocumento5 páginas12-Channel ECG SpecsNai PaniaiAinda não há avaliações
- New 5Documento37 páginasNew 5rishi gupta100% (1)
- Asymptomatic BacteriuriaDocumento23 páginasAsymptomatic BacteriuriaSabita PaudelAinda não há avaliações
- 3 Azarpour Et Al. JNBR 4 (1) 2015 PDFDocumento9 páginas3 Azarpour Et Al. JNBR 4 (1) 2015 PDFKamailAinda não há avaliações
- Notice Application Form For SRDocumento4 páginasNotice Application Form For SRPankaj PrasadAinda não há avaliações
- Training of Top US Distance SwimmersDocumento45 páginasTraining of Top US Distance SwimmersMel HarbourAinda não há avaliações
- Awilda Prignano Weebly ResumeDocumento2 páginasAwilda Prignano Weebly Resumeapi-497064105Ainda não há avaliações
- CM Lecture NotesDocumento30 páginasCM Lecture NotesJefferson SorianoAinda não há avaliações
- Margaret Moore Bob Tschannen-Moran Erika JacksonDocumento201 páginasMargaret Moore Bob Tschannen-Moran Erika JacksonBella100% (18)
- Meier Et Al, 1996Documento4 páginasMeier Et Al, 1996boni_sebayangAinda não há avaliações
- List of Firms Having Who (Own)Documento1 páginaList of Firms Having Who (Own)Ksusha ChernobrovaAinda não há avaliações
- Aeromedical Transport TPDocumento8 páginasAeromedical Transport TPgalib20Ainda não há avaliações
- What Is HumorDocumento5 páginasWhat Is HumorWan Sek ChoonAinda não há avaliações
- Classi Fications of Adverse Drug Reactions: 1. EidosDocumento6 páginasClassi Fications of Adverse Drug Reactions: 1. Eidosdolemite4Ainda não há avaliações
- Tension PneumothoraxDocumento13 páginasTension PneumothoraxAbdullahAinda não há avaliações
- Buklet Amt 01 EnglishDocumento13 páginasBuklet Amt 01 Englishaemrana100% (1)
- Emergency Room InstrumentsDocumento2 páginasEmergency Room InstrumentsEduardo AnerdezAinda não há avaliações
- Chapter 4intestinal NematodesDocumento41 páginasChapter 4intestinal Nematodesdeneke100% (1)
- Advances in Psychological and Social Support After DisastersDocumento149 páginasAdvances in Psychological and Social Support After DisastersjprewittdiazAinda não há avaliações
- Punjab Healthcare Commission: CG-09RM-Ed2Documento168 páginasPunjab Healthcare Commission: CG-09RM-Ed2saimaAinda não há avaliações
- NCPDocumento3 páginasNCPCharles Mallari Valdez100% (1)
- DreamsDocumento1 páginaDreamsiammarcanthonyAinda não há avaliações
- The Sacred Mushroom "Reishi"-A ReviewDocumento4 páginasThe Sacred Mushroom "Reishi"-A ReviewDinesh Babu PugalenthiAinda não há avaliações
- Module 2 Case Analysis JohnDocumento8 páginasModule 2 Case Analysis Johnkimwei clintonAinda não há avaliações
- Reasoning BookDocumento38 páginasReasoning BookAshish Sharma100% (1)
- Human Papillomavirus (HPV) Test and PAP Smear As Predictors of Outcome in Conservatively Treated Adenocarcinoma in Situ (AIS) of The Uterine CervixDocumento7 páginasHuman Papillomavirus (HPV) Test and PAP Smear As Predictors of Outcome in Conservatively Treated Adenocarcinoma in Situ (AIS) of The Uterine CervixodivarAinda não há avaliações