Escolar Documentos
Profissional Documentos
Cultura Documentos
Appendicits Surgery Os The Best Option 2011
Enviado por
Hugo0 notas0% acharam este documento útil (0 voto)
6 visualizações2 páginasapendicitis
Título original
Appendicits Surgery Os the Best Option 2011
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoapendicitis
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
6 visualizações2 páginasAppendicits Surgery Os The Best Option 2011
Enviado por
Hugoapendicitis
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
Você está na página 1de 2
Comment
Appendicitis: is surgery the best option?
The need to surgically remove the appendix in patients
with acute appendicitis is so entrenched in the minds
of surgeons, patients, and physicians alike that nonoperative management is almost never considered or
oered to patients. In The Lancet, Corinne Vons and
colleagues1 present data from a randomised noninferiority trial that compared antibiotics (amoxicillin
plus clavulanic acid) with emergency appendicectomy.
In their study, 243 patients were randomised in ve
French hospitals and the primary endpoint, 30-day
postintervention peritonitis, was more frequent in
the antibiotic group (8% vs 2%, treatment dierence
58, 95% CI 03121). However, 68% of patients with
uncomplicated appendicitis assigned to the antibiotic
group did not need an appendicectomy. This incidence of
unnecessary appendicectomy was similar to four earlier
randomised trials25 comparing antibiotic therapy with
appendicectomy for the treatment of uncomplicated
appendicitis (table). Yet Vons and colleagues could not
show non-inferiority of antibiotic treatment compared
with appendicectomy, owing perhaps to study design
and choice of antibiotic.
Vons and colleagues1 compared the 30-day posttherapeutic occurrence of an intra-abdominal infectious
complication between antibiotic and appendicectomy
groups with a non-inferiority margin of 10%. A 10%
margin is usual in comparisons of dierent drug treatments, but is probably too narrow when comparing a
surgical option with a non-surgical option, with very
dierent riskbenet ratios.6 There is no guidance in the
literature for the appropriate non-inferiority margin to
use when comparing a non-surgical with a surgical group.
If a 15% margin had been chosen, which in my view is not
unreasonable considering the risks associated with surgery,
non-inferiority would have been shown. Furthermore,
the overall rate of Escherichia coli non-susceptibility to
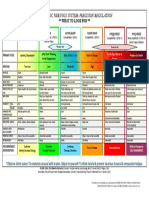
Number of patients in antibiotic group
amoxicillin-clavulanic acid is substantially greater than the
non-inferiority margin chosen.7 E coli is the most common
organism isolated from patients with appendicitis, and
resistance of E coli to aminopenicillins in Europe can
reach 66%.8 For this reason, amoxicillin-clavulanic acid
is not recommended in the non-operative treatment
of appendicitis.9 In fact, in the four other published
comparisons,25 amoxicillin-clavulanic acid was never used.
The most appropriate way to analyse missing data
continues to be a challenge for researchers. Vons
and colleagues rst imputed missing data points
as successes, and in a secondary analysis excluded
these data. However, in the webappendix when the
missing data were imputed as failures, the incidence
of a primary event in the antibiotic group was 108%
(13 of 120 patients) compared with 58% (seven of 119)
in the appendicectomy group, which is statistically
consistent with similarity between antibiotic therapy
and appendicectomy (Pearson =191, p=0167).
Localised thickness of the digestive tract walls with
free uid present at operation, subjectively determined
by the surgeon, was a primary endpoint in the antibiotic
group having surgery (see protocol section 7-1). A similar
determination of densication of soft tissue with or
without organised uid collection could not be assessed
in patients in the surgery group, because they did not
routinely have a CT scan at follow-up, and were assessed
1 week later than patients in the antibiotic group. In my
experience, intestinal thickening and postoperative uid
would have been detected in some surgical patients
after appendicectomy if they had been followed up at
day 8 and if all patients with symptoms had a CT scan,
as was done for patients in the antibiotic group. Use of
dierent follow-up procedures between groups biases
the data, and potentially changes the outcome. I would
suggest that patients in both groups should have had a
Eriksson (1995)2
Styrud (2006)5
Hansson (2009)3
Malik (2009)4
Vons (2011)1
20
128
202
40
120
Antibiotic failure needing appendicectomy
15
105
14
Normal appendix
Recurrence requiring appendicectomy
16
11
30
Normal appendix with recurrence
Did not need appendicectomy
0
13/20 (65%)
0
98/128 (77%)
0
89/202 (44%)
0
34/40 (85%)
See Articles page 1573
For the study protocol see
http://www.medecine.u-psud.fr/
modules/resources/download/
ufrmedecine/Recherche/
Publications/Appendop_
biomedical_resarch_protocol_C_
VONS_et_al.pdf
4
81/120 (68%)
Table: Summary of randomised trials comparing antibiotics with appendicectomy
www.thelancet.com Vol 377 May 7, 2011
1545
Comment
day 8 follow-up with mandatory abdominal imaging,
irrespective of symptoms, to eliminate bias.
The success of source control surgery or antibiotic
treatment of appendicitis is determined by resolution of
the condition strictly by means of the assigned treatment.
Patients who developed postoperative peritonitis in
the antibiotic group were correctly included as failed
treatments, even though this complication arose from
surgery. The same stringent criteria were not applied
in the surgery group, since 21 (18%) of these patients
had complicated appendicitis and received antibiotics
postoperatively, but were not considered treatment
failures. Some of the patients in the surgery group would
probably have developed postoperative peritonitis
without antibiotics.8 These patients should be classied
as treatment failures because appendicectomy alone did
not provide adequate source control. Equivalence might
have been shown if the patients undergoing surgery had
not received this preferential treatment.
The incidence of post-treatment peritonitis is
interesting and as yet unaccounted for. When the
management of appendicitis with antibiotics was
successful, the incidence of post-treatment peritonitis
was zero. However, if antibiotics failed, the organ
space surgical site infection rate was very high, at 14%
(two of 14 patients) compared with 17% (two of 120)
in the appendicectomy group.
Finally, an alternative to appendicectomy in patients
who did not respond to initial treatment with antibiotics
and those who had recurrent appendicitis could be
another course or dierent antibiotic, since the cause
of failure could be antibiotic resistance. This acceptable
alternative strategy3 is analogous to the present standard
of care for recurrent uncomplicated diverticulitis.10
I congratulate Vons and colleagues for tackling this
important, controversial, and relevant topic. Hopefully
their conclusion, once the biases have been considered,
will not overshadow major advances that have been made
in the past 15 years towards the conservative treatment of
appendicitis. The fact that two-thirds of patients can be
spared an operation deserves more attention.
Rodney J Mason
University of Southern California, Keck School of Medicine,
Division of General and Laparoscopic Surgery, Los Angeles,
CA 90033, USA
rjmason@med.usc.edu
I declare that I have no conicts of interest.
1
2
3
4
5
10
Vons C, Barry C, Maitre S, et al. Amoxicillin plus clavulanic acid versus
appendicectomy for treatment of acute uncomplicated appendicitis:
an open-label, non-inferiority, randomised controlled trial. Lancet 2011;
377: 157379.
Eriksson S, Granstrom L. Randomised controlled trial of appendicectomy
versus antibiotic therapy for acute appendicitis. Br J Surg 1995; 82: 16669.
Hansson J, Korner U, Khorram-Manesh A, Solberg A, Lundholm K.
Randomised clinical trial of antibiotic therapy versus appendicectomy as
primary treatment of acute appendicitis in unselected patients.
Br J Surg 2009; 96: 47381.
Malik AA, Bari SU. Conservative management of acute appendicitis.
J Gastrointest Surg 2009; 13: 96670.
Styrud J, Eriksson S, Nilsson I, et al. Appendectomy versus antibiotic
treatment in acute appendicitis. a prospective multicenter randomized
controlled trial. World J Surg 2006; 30: 103337.
Powers JH, Ross DB, Brittain E, Albrecht R, Goldberger MJ. The United
States Food and Drug Administration and noninferiority margins in clinical
trials of antimicrobial agents. Clin Infect Dis 2002; 34: 87981.
Oteo J, Campos J, Lazaro E, et al. Increased amoxicillin-clavulanic acid
resistance in Escherichia coli blood isolates, Spain. Emerg Infect Dis 2008;
14: 125962.
Andersen BR, Kallehave FL, Andersen HK. Antibiotics versus placebo for
prevention of postoperative infection after appendicectomy.
Cochrane Database Syst Rev 2005; 3: CD001439.
Solomkin JS, Mazuski JE, Bradley JS, et al. Diagnosis and management of
complicated intra-abdominal infection in adults and children: guidelines
by the Surgical Infection Society and the Infectious Diseases Society of
America. Surg Infect (Larchmt) 2010; 11: 79109.
Chautems RC, Ambrosetti P, Ludwig A, Mermillod B, Morel P, Soravia C.
Long-term follow-up after rst acute episode of sigmoid diverticulitis:
is surgery mandatory?: a prospective study of 118 patients.
Dis Colon Rectum 2002; 45: 96266.
Improving treatment outcome for children with HIV
Published Online
April 20, 2011
DOI:10.1016/S01406736(11)60363-2
See Articles page 1580
1546
Over 2 million children are infected with HIV, and around
700 children die of HIV/AIDS-related causes every
day. Almost all children with HIV infection have been
infected through perinatal transmission, and without
antiretroviral treatment over half will die before the age
of 2 years.1
Antiretrovirals have had a dramatic eect on the
course of HIV/AIDS in children. Trials show excellent
long-term outcomes with protease inhibitors and
non-nucleoside reverse-transcriptase inhibitors,2
and current guidelines recommend starting antiretroviral therapy in children as soon as possible
after diagnosis of HIV infection.3 Poor availability of
ecient antiretroviral regimens, unclear strategies for
optimum drug sequencing, and maintenance of high
adherence from infancy and throughout adolescence
to adulthood are important challenges to long-term
treatment success.4
www.thelancet.com Vol 377 May 7, 2011
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The American Association For Thoracic Surgery Consensus Guidelines For The Management of EmpyemaDocumento18 páginasThe American Association For Thoracic Surgery Consensus Guidelines For The Management of EmpyemaHugo100% (2)
- Colorectal Cancer Lancet 2010 PDFDocumento18 páginasColorectal Cancer Lancet 2010 PDFHugoAinda não há avaliações
- Mitral Valve ProlapseDocumento19 páginasMitral Valve ProlapseHugoAinda não há avaliações
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Abdominoperineal Resection MilesDocumento17 páginasAbdominoperineal Resection MilesHugoAinda não há avaliações
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Inhalation Injury-Epidemiology, Pathology, Treatment StrategiesDocumento15 páginasInhalation Injury-Epidemiology, Pathology, Treatment StrategiesHugo100% (1)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Endocrine SystemDocumento32 páginasEndocrine Systemlee bon hukAinda não há avaliações
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- Stretch To Win (2017) PDFDocumento241 páginasStretch To Win (2017) PDFmmpersonal2010100% (4)
- Summary of AB236 AmendmentsDocumento9 páginasSummary of AB236 AmendmentsMichelle Rindels100% (1)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Schedule of Charges-Holy Family - Sep 08Documento64 páginasSchedule of Charges-Holy Family - Sep 08Quirinevv100% (1)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- Hardy Et Al-2018-Australian and New Zealand Journal of Public HealthDocumento5 páginasHardy Et Al-2018-Australian and New Zealand Journal of Public HealthAnggita RifkyAinda não há avaliações
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- 20190305190022636Documento94 páginas20190305190022636Subhi MohamadAinda não há avaliações
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- MEM05052A Apply Safe Welding Practices - Learner GuideDocumento14 páginasMEM05052A Apply Safe Welding Practices - Learner Guidequestionbank.com.au100% (1)
- Capa SopDocumento23 páginasCapa SopHaroon Rasheed100% (3)
- Qi - Magazine Nº48Documento41 páginasQi - Magazine Nº48Carvalho100% (4)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Health10 - Q4 - Mod1 (Lessons 1-4)Documento40 páginasHealth10 - Q4 - Mod1 (Lessons 1-4)Merjie A. NunezAinda não há avaliações
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Female Foeticide in India A Bitter Truth FinalDocumento22 páginasFemale Foeticide in India A Bitter Truth Finalaman manderAinda não há avaliações
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Sistema NervosoDocumento1 páginaSistema NervosoPerisson Dantas100% (2)
- Rizal's Visit To The United States (1888Documento23 páginasRizal's Visit To The United States (1888Dandy Lastimosa Velasquez57% (7)
- Yoga and Pregnancy Pre and Postnatal Resources PDFDrive ComDocumento63 páginasYoga and Pregnancy Pre and Postnatal Resources PDFDrive ComsilverbirddudeAinda não há avaliações
- Journal Club: A Step Towards Evidence Based Practice: January 2011Documento6 páginasJournal Club: A Step Towards Evidence Based Practice: January 2011Jommy ChawalaAinda não há avaliações
- TASSDocumento11 páginasTASSNike KeketAinda não há avaliações
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Centaur CortisolDocumento12 páginasCentaur CortisolMohamed AliAinda não há avaliações
- Economics Assignment (AP)Documento20 páginasEconomics Assignment (AP)Hemanth YenniAinda não há avaliações
- Tugas 2Documento17 páginasTugas 2NuretikaSalmiaAinda não há avaliações
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Haad 3 Questions GiDocumento16 páginasHaad 3 Questions GiPatpat De Guzman67% (3)
- ED Produk KF - KF (Nama Apotek)Documento19 páginasED Produk KF - KF (Nama Apotek)Eko FebryandiAinda não há avaliações
- HPA 14 Assignemnt Due November 16thDocumento5 páginasHPA 14 Assignemnt Due November 16thcAinda não há avaliações
- Monkeypox: VirusDocumento18 páginasMonkeypox: Virusdiela dwi lestariAinda não há avaliações
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Punjab General Industries Private Limited: Hazard Identification and Risk Assessment (HIRA)Documento9 páginasPunjab General Industries Private Limited: Hazard Identification and Risk Assessment (HIRA)Rohit VishwakarmaAinda não há avaliações
- Plazma Ionizarot CP 212 Eng ManualDocumento1 páginaPlazma Ionizarot CP 212 Eng ManualVladimirDulaAinda não há avaliações
- Promethazine (Phenergan)Documento1 páginaPromethazine (Phenergan)Adrianne BazoAinda não há avaliações
- Invasive and Non-Invasive Site Investigation and Understand Permitting Process For Constructing LandfillDocumento12 páginasInvasive and Non-Invasive Site Investigation and Understand Permitting Process For Constructing LandfillKessler BiatingoAinda não há avaliações
- Medical Informatics - Concepts, Methodologies, Tools, and Applications (Premier Reference Source) (PDFDrive)Documento2.593 páginasMedical Informatics - Concepts, Methodologies, Tools, and Applications (Premier Reference Source) (PDFDrive)tinanoAinda não há avaliações
- E Chlas Feb16Documento20 páginasE Chlas Feb16dkhatriAinda não há avaliações
- SAFH - Sqe.001 SAFH's Clinical Privileging Process - Revised 12.1.21Documento6 páginasSAFH - Sqe.001 SAFH's Clinical Privileging Process - Revised 12.1.21joy chiaAinda não há avaliações