Escolar Documentos
Profissional Documentos
Cultura Documentos
Chapter 3 - Introduction To Nuclear Medicine
Enviado por
unknownxemTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Chapter 3 - Introduction To Nuclear Medicine
Enviado por
unknownxemDireitos autorais:
Formatos disponíveis
Linda K.
Petrovich, MD, and
E. Scott Pretorius, MD
Chapter
Introduction to Nuclear Medicine
1. How is a nuclear medicine test performed?
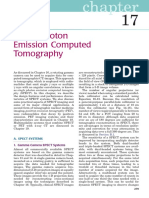
A radiopharmaceutical agent, which is a radioactively tagged compound, is administered to a patient. Many
radiopharmaceutical agents act like analogues of natural biologic compounds and localize to specific organs. Photons
are emitted from the radiopharmaceutical agent in the
Photomultiplier tubes
Computer
patient, and a gamma camera is used to detect the
tracer distribution. An image is created by a computer
system (Fig. 3-1).
2. What is the difference between the
x-rays used in plain films and computed
tomography (CT) and the gamma rays
used in nuclear medicine?
X-rays are produced from the interaction of bombarding
photons or electrons within an atom. Gamma rays are
produced when an unstable nucleus transitions to a
more stable state. Diagnostic x-ray imaging is referred
to as transmission imaging. This term is used because
images are formed as x-ray photons from an external
source traverse tissue and emerge to form the image.
Nuclear medicine is referred to as emission imaging
because photons are emitted from inside the patient and
subsequently detected by the gamma camera imaging
system.
Sodium
iodide
crystal
Collimator
Monitor
Source
3. How does nuclear medicine differ
from other imaging modalities used in
radiology, such as plain film, ultrasound
Figure 3-1. Line drawing showing the flow of information of a
(US), CT, and magnetic resonance
typical nuclear medicine study, such as a bone scan, obtained with
imaging (MRI)?
a gamma camera.
Plain films, US, CT, and MRI produce anatomic images
with very high spatial resolution. A viewer can see
anatomy very well, but function generally is not assessed. Nuclear medicine studies sacrifice spatial resolution, but in
return offer information about organ function.
Key Points: How Nuclear Medicine Differs from Other Imaging Modalities
1.
2.
3.
4.
5.
Radiopharmaceutical agents are administered to the patient before imaging.
Images are indicative of the functional status of an organ.
The spatial resolution in nuclear medicine is less than that of x-rays, US, CT, and MRI.
Photons are emitted from the patient and detected by a gamma camera.
The total time for a nuclear medicine test may range from minutes to days, depending on the half-life and distribution
of the radiopharmaceutical agent.
4. List some common clinical indications for performing
nuclear medicine imaging.
. .
To rule out pulmonary embolism, a ventilation-perfusion (V/Q) scan may be performed.
To evaluate for acute cholecystitis, a hepato-iminodiacetic acid (HIDA) scan may be performed.
To detect a potential gastrointestinal (GI) bleed, a bleeding scan may be performed.
To evaluate for osteomyelitis, a three-phase bone scan may be performed.
19
Downloaded from ClinicalKey.com at Rutgers University - NERL June 05, 2016.
For personal use only. No other uses without permission. Copyright 2016. Elsevier Inc. All rights reserved.
20
Introduction to Nuclear Medicine
. .
5. What
. . radiopharmaceutical agents are used in a V/Q scan?
A V /Q scan attempts to identify regions of lung that are aerated lung but not perfused (such regions are suspicious
for pulmonary embolism). The scan consists of two parts: a ventilation phase where the aerated lung is imaged, and
a perfusion phase that maps blood flow to the lungs. The two sets of images are compared for discrepancies. For the
ventilation portion of the study, xenon-133 and technetium (Tc)-99m diethylenetriaminepentaacetic acid (DTPA) are the
most commonly used agents. For the perfusion portion of the study, Tc-99m macroaggregated albumin (MAA) is used.
. .
6. How is a V/Q scan performed?
The ventilation portion is performed using either radioactive gas (xenon) or radioactive aerosol (Tc-99m DTPA). When
radioactive gas is used, the study is accomplished in three phases: single-breath/wash-in phase, equilibrium phase,
and washout phase. For studies that use radioaerosols, the radiopharmaceutical agent is placed in a special nebulizer
system, and the patient breathes through the mouthpiece until sufficient radioaerosol is delivered to the lungs. Tc-99m
remains in the lung long enough to obtain multiple views with a gamma camera. Tc-99m MAA is injected into a
peripheral vein to assess perfusion. The particles travel to the right side of the heart and then to the lungs, where they
are filtered or trapped in the pulmonary vascular bed. The emissions from the trapped particles are imaged with a
gamma camera.
. .
7. How are the results of a V/Q scan interpreted?
If an acute pulmonary embolism is present, the thrombus in the blood vessel prevents radiotracer from reaching the
portion of lung supplied by the vessel, and a perfusion defect results. An acute thrombus does not prevent air from
being distributed to the lung via bronchi, however, and the results of the ventilation scan are normal. This
. combination
.
of a perfusion defect without a corresponding ventilation defect is called a mismatch. The results of a V /Q scan are
classified as low, intermediate, or high probability for a pulmonary embolism. The classification is based on the number
and size ofdefects, with higher numbers and sizes resulting in greater probability that an embolus is present.
8. What radiopharmaceutical agent is used in HIDA scan?
Tc-99mlabeled iminodiacetic acid (IDA) compounds are used. They share biologic activity with bilirubin and are also
taken up, transported, and excreted by hepatocytes.
9. How is HIDA scan performed?
The patient is required to fast for at least 4 hours, but not longer than 24 hours. If the test is performed after a recent meal,
the gallbladder may still be contracted, and this could lead to false-positive test results. After a prolonged fast, the gallbladder
may be filled with concentrated bile, and this may also lead to false-positive test results by preventing tracer accumulation in
the gallbladder. Tc-99m IDA is injected into a peripheral vein, followed by immediate imaging of the right upper quadrant.
10. How are the results of HIDA scan interpreted?
Because the tracer behaves similar to bilirubin, it should be taken up by hepatocytes and excreted into the bile ducts.
The liver should be visualized first, followed by visualization of the bowel and gallbladder. The appearance of tracer in
the bowel and gallbladder by 60 minutes after administration is defined as normal. Nonvisualization of the gallbladder
by 60 minutes is diagnostic of acute cholecystitis because this implies a functional obstruction of the cystic duct. Falsepositive results can be caused by chronic cholecystitis, hepatic insufficiency, and fasting for less than 4 hours or more
than 24 hours as previously described.
Key Points: Common Clinical Indications for a Nuclear Medicine Study
1.
2.
3.
4.
5.
6.
7.
To rule out pulmonary embolism (ventilation-perfusion scan)
To rule out acute cholecystitis, bile duct obstruction, or biliary leak (HIDA scan)
To rule out lower GI bleed (Tc-99m sulfur colloid or Tc-99mlabeled red blood cells)
To rule out infection (bone scan, indium-111labeled white blood cells, gallium 67)
To evaluate for metastatic disease (bone scan, positron emission tomography (PET) scan)
To evaluate for thyroid pathologic conditions (iodine-123)
To evaluate for renal pathologic conditions, such as obstruction, hypertension, reflux, and transplant (Tc-99mlabeled
compounds)
11. What radiopharmaceutical agents are used for GI bleeding scan?
Tc-99m sulfur colloid or Tc-99mlabeled red blood cells (RBCs) are used. Tc-99mlabeled RBCs are more difficult
toprepare, but have a longer plasma half-life and are able to detect a GI bleed over a longer period.
12. How do you tell whether the results of the bleeding scan are positive?
An abnormal radiotracer hot spot appears and conforms to bowel anatomy. The activity should increase over time and
move through the GI tract. Because blood acts as an intestinal irritant, movement can be rapid and bidirectional.
Downloaded from ClinicalKey.com at Rutgers University - NERL June 05, 2016.
For personal use only. No other uses without permission. Copyright 2016. Elsevier Inc. All rights reserved.
introduction to imaging modalities
13. What are some indications for performing a renal scan?
Renal scans have various clinical applications, including evaluating renal transplants, differentiating between obstructed
and dilated collecting systems, and diagnosing reflux and renovascular hypertension.
14. What are the four major renal functions that can be evaluated with radionuclide imaging?
Renal scans are helpful in evaluating blood flow to the kidney, glomerular filtration, tubular function (resorption and
secretion), and drainage of the collecting systems.
15. What are the main radiopharmaceutical agents used in renal scans? How do they
differ?
Tc-99m DTPA is a glomerular agent, meaning that it is cleared primarily by glomerular filtration and is neither
reabsorbed nor secreted by the renal tubules. It can be used to measure the glomerular filtration rate. Tc-99m
mertiatide (MAG3) is a tubular agent, meaning that its mechanism of renal clearance is solely tubular secretion. Tc-99m
dimercaptosuccinic acid (DMSA) is a cortical agent, meaning that it binds to tubular cells in the renal cortex, making
possible static imaging of the renal parenchymal cortex.
16. What three main factors should be examined when interpreting a renal scan?
Blood flow, radiotracer uptake, and radiotracer excretion should be examined.
17. What radiopharmaceutical agents are used in thyroid imaging?
Iodine-123 is the diagnostic agent of choice for imaging the thyroid. Iodine is administered orally. It is absorbed from
the GI tract and trapped and organified (incorporated into thyroglobulin molecules) in the thyroid. Tc-99m pertechnetate
is used if imaging has to be performed within 1 hour or if the patient is unable to ingest orally. Iodine-131 is used for
whole-body scans after thyroidectomy for thyroid cancer and for therapeutic purposes.
18. Describe the appearance of Graves disease, thyroiditis, and tumor on a nuclear
imaging study.
Graves disease is manifested by an enlarged gland that shows diffusely increased uptake. Thyroiditis appears as
diffusely decreased uptake. Thyroid cancer tends to appear as a focal area of decreased activity (a solitary cold nodule)
rather than showing increased activity on a nuclear medicine study.
19. What radiopharmaceutical agents are used in bone scanning?
Tc-99mlabeled diphosphonates are injected intravenously to perform a bone scan. The radiotracer distribution is
representative of osteoblastic activity and regional blood flow to bone. Dynamic blood flow imaging is performed immediately
after the injection of radiotracer. Static imaging is performed 2 to 4 hours after injection and is indicative of osteoblastic activity.
20. What are the two types of bone scans that can be performed, and what are the
indications for each?
Focal three-phase imaging and whole-body imaging are the two types of bone scans. Focal three-phase imaging is used
to differentiate cellulitis from osteomyelitis. The three phases are the flow phase (1 minute after injection), the blood pool
(5 minutes after injection), and the skeletal phase (2 to 4 hours after injection). Cellulitis and osteomyelitis have increased
uptake in the first two phases of the bone scan; however, only osteomyelitis shows increased activity in the third phase.
Whole-body imaging consists of static images obtained 2 to 4 hours after injection. It is used for detection of metastatic
and metabolic diseases and bone dysplasia.
21. If you are concerned about an infection outside the skeletal system, what nuclear
imaging studies can you perform?
Indium (In)-111labeled white blood cells (WBCs) and gallium-67 citrate can be used to detect occult infection. To label
WBCs with In-111, the cells must be removed from plasma. Blood is taken from the patient, labeled, and reinjected.
Imaging is performed 24 hours after the injection. The normal distribution of WBCs is spleen, liver, and bone marrow.
Activity seen outside the normal expected distribution is evidence of a focus of infection. Gallium, the other agent useful
in locating sources of infection, binds to iron-binding molecules. Its normal distribution is liver and bone marrow. It is
excreted by the kidneys for the first 24 hours and through the large bowel after 24 hours. As with an In-111 WBC scan,
activity seen outside the expected normal organs of uptake is evidence of infection.
22. What is a PET scan?
PET stands for positron emission tomography. A tracer that emits positrons is injected into the patient. After the positrons
are emitted from the nucleus of an atom, they travel through surrounding tissue and collide with electrons. This collision
between positrons and electrons is called annihilation and produces gamma rays. The gamma rays are detected by a PET
Downloaded from ClinicalKey.com at Rutgers University - NERL June 05, 2016.
For personal use only. No other uses without permission. Copyright 2016. Elsevier Inc. All rights reserved.
21
22
Introduction to Nuclear Medicine
scanner and analyzed by a computer to form an image. Because positronic decay produces two 511-keV photons that
travel in exactly opposite directions, acquisition of PET data is sometimes called coincidence detectiononly photons
of the correct energy that are detected simultaneously by detectors 180 degrees from each other are registered as true
events, and the rest are assumed to be noise.
23. What radiopharmaceutical agent is used in PET? What type of pathologic conditions
can it detect?
Fluorodeoxyglucose (FDG) is used in PET. This is a radionuclide combined with glucose, which is the currency of
metabolism for malignant and benign cells. Because malignant cells tend to grow and metabolize glucose faster than
healthy tissue, however, malignant cells use more of the tracer. PET uses the difference in metabolism to differentiate
normal from abnormal tissue.
Key Points: Main Radionuclides Used in Nuclear Medicine
1.
2.
3.
4.
5.
6.
Tc-99m (most common)
Iodine-123
Gallium-67
Thallium-201
In-111
FDG (for PET imaging)
24. What is SUV?
SUV is standardized uptake value. It is a very important concept in interpretation of PET and PET/CT scans, and is a
measurement of the activity seen in a region of interest relative to the body as a whole. By definition, if the activity of an
injected dose were normalized over the entire body, the SUV everywhere would be 1.
25. What types of cancer are best detected on PET?
PET scans can be used to detect malignant tumors, determine cancer stage, and judge the effectiveness of cancer
treatment. They are most often used in patients with head and neck tumors, colorectal cancer, lymphoma, melanoma,
and lung cancer.
26. Should PET/CT be done with or without an intravenous contrast agent?
There is increasing evidence that the use of an intravenous contrast agent for the CT portion of PET/CT increases
detection of liver lesions and allows for more accurate characterization of the lesions detected.
Bibliography
[1] S. Badiee, B.L. Franc, E.M. Webb, et al., Role of IV iodinated contrast material in 18F-FDG PET/CT of liver metastases, AJR Am. J. Roentgeol.
191 (2008) 14361439.
[2] J.H. Thrall, Nuclear Medicine: The Requisites, second ed., Mosby, St. Louis, 2001.
Downloaded from ClinicalKey.com at Rutgers University - NERL June 05, 2016.
For personal use only. No other uses without permission. Copyright 2016. Elsevier Inc. All rights reserved.
Você também pode gostar
- Atlas of Hybrid Imaging Sectional Anatomy for PET/CT, PET/MRI and SPECT/CT Vol. 2: Thorax Abdomen and Pelvis: Sectional Anatomy for PET/CT, PET/MRI and SPECT/CTNo EverandAtlas of Hybrid Imaging Sectional Anatomy for PET/CT, PET/MRI and SPECT/CT Vol. 2: Thorax Abdomen and Pelvis: Sectional Anatomy for PET/CT, PET/MRI and SPECT/CTAinda não há avaliações
- Nuclear Medicine GuideDocumento3 páginasNuclear Medicine GuidejeffsunilAinda não há avaliações
- Nuclear Medicine Tehnologist or Lead Nuclear Medicine TechnologiDocumento2 páginasNuclear Medicine Tehnologist or Lead Nuclear Medicine Technologiapi-78955179Ainda não há avaliações
- Advances in Biological and Medical Physics: Volume 1No EverandAdvances in Biological and Medical Physics: Volume 1Ainda não há avaliações
- Senior Radiographer Nuclear MedicineDocumento1 páginaSenior Radiographer Nuclear Medicinetafi66Ainda não há avaliações
- Angiographic Phases/ Phases of Normal FaDocumento9 páginasAngiographic Phases/ Phases of Normal FaWesley Kent Copioso0% (1)
- Nuclear Medicine Inc.'s Iodine Value Chain AnalysisDocumento6 páginasNuclear Medicine Inc.'s Iodine Value Chain AnalysisPrashant NagpureAinda não há avaliações
- Nuclear Medicine Instrumentation QC GUIDELINES Maria Lyra Et Al 2007Documento69 páginasNuclear Medicine Instrumentation QC GUIDELINES Maria Lyra Et Al 2007knno87Ainda não há avaliações
- Basic Considerations in Nuclear MedicineDocumento12 páginasBasic Considerations in Nuclear Medicinechberg13Ainda não há avaliações
- F-18 NaFDocumento47 páginasF-18 NaFLadipo Temitope AyodejiAinda não há avaliações
- 4Documento247 páginas4Tanpreet SinghAinda não há avaliações
- CT ANGIOGRAPHY - DETAILED IMAGES OF BLOOD VESSELSDocumento1 páginaCT ANGIOGRAPHY - DETAILED IMAGES OF BLOOD VESSELSsreejithAinda não há avaliações
- Fluroscopy & Iitv SystemDocumento87 páginasFluroscopy & Iitv SystemMunish DograAinda não há avaliações
- Contrast Media and Adverse Effects - Vijay KumarDocumento41 páginasContrast Media and Adverse Effects - Vijay KumarTapshi SohalAinda não há avaliações
- P8-9 CoverStory CT-HistoryDocumento2 páginasP8-9 CoverStory CT-Historyalem87Ainda não há avaliações
- Evaluation and Routine Testing in Medical Imaging DepartmentsDocumento18 páginasEvaluation and Routine Testing in Medical Imaging DepartmentsRankie Choi100% (1)
- Rtog 0813 Marina CousinsDocumento22 páginasRtog 0813 Marina Cousinsapi-426094285Ainda não há avaliações
- 200+ TOP RADIOLOGY Online Quiz Questions - Exam Test 2023Documento24 páginas200+ TOP RADIOLOGY Online Quiz Questions - Exam Test 2023Ayub Alam100% (1)
- Diagnostic Reference Level in Lumbar Radiography in Abidjan, Côte D'ivoireDocumento5 páginasDiagnostic Reference Level in Lumbar Radiography in Abidjan, Côte D'ivoiretheijesAinda não há avaliações
- Contrast MediaDocumento6 páginasContrast MediardmdelarosaAinda não há avaliações
- Week 9 C Chapter 40 Radiation Protection, Chapter 31 QC 84Documento84 páginasWeek 9 C Chapter 40 Radiation Protection, Chapter 31 QC 84chicken66Ainda não há avaliações
- Radiology Notes (1-36)Documento83 páginasRadiology Notes (1-36)el spin artifactAinda não há avaliações
- Emergency Radiology PDFDocumento41 páginasEmergency Radiology PDFRobiul AlamAinda não há avaliações
- Iodinated Contrast Media GuidelineDocumento41 páginasIodinated Contrast Media GuidelineN Aa100% (1)
- OpenMrs Radiology Module User GuideDocumento33 páginasOpenMrs Radiology Module User GuideSkaksAinda não há avaliações
- Star Primer 2014 InvitationDocumento4 páginasStar Primer 2014 InvitationBhavik ChopdaAinda não há avaliações
- Final Qa ChartDocumento9 páginasFinal Qa Chartapi-299270003Ainda não há avaliações
- AAPM 34 - MRI Acceptance TestDocumento16 páginasAAPM 34 - MRI Acceptance TestmahbodsedAinda não há avaliações
- Viner 2005 Forensic Radiography in South AfricaDocumento24 páginasViner 2005 Forensic Radiography in South Africah8517Ainda não há avaliações
- Introduction To Nuclear Medicine: Sania Rahim PGY 4 BCM C/o 2008Documento28 páginasIntroduction To Nuclear Medicine: Sania Rahim PGY 4 BCM C/o 2008asfadsi23Ainda não há avaliações
- Cherenkov RadiationDocumento17 páginasCherenkov RadiationMayank GargAinda não há avaliações
- 2 Fundamental Principles of RadiobiologyDocumento28 páginas2 Fundamental Principles of RadiobiologyAngelo RamosAinda não há avaliações
- Icru 82Documento67 páginasIcru 82Aditya DisdusAinda não há avaliações
- The Safe Use of Fluoroscopy: Radiation Protection Ala' ThawabtehDocumento41 páginasThe Safe Use of Fluoroscopy: Radiation Protection Ala' ThawabtehDiaa AyobAinda não há avaliações
- Principles of Exposure Ch.8Documento42 páginasPrinciples of Exposure Ch.8abdulsalam khalaf100% (1)
- Basic Stroke ImagingDocumento73 páginasBasic Stroke ImagingjoeiradAinda não há avaliações
- Final MIT Logbook JamilDocumento15 páginasFinal MIT Logbook Jamilammar-nasir3314Ainda não há avaliações
- X-Ray Intensifying Screens: Prof. J.K Tonui, PHDDocumento42 páginasX-Ray Intensifying Screens: Prof. J.K Tonui, PHDLajja Parikh PatelAinda não há avaliações
- Ge-68 - Ga-68 Generators - John K. Amartey, MS, PhD-508 PDFDocumento19 páginasGe-68 - Ga-68 Generators - John K. Amartey, MS, PhD-508 PDFDhika FazrianAinda não há avaliações
- Barium Swallow (Cine Oesophagram) : Hyelhirra P. MsheliaDocumento25 páginasBarium Swallow (Cine Oesophagram) : Hyelhirra P. MsheliaJameeluh TijjanyAinda não há avaliações
- Interpretation of Magnetic Resonance Imaging of Orbit: Simplifi Ed For Ophthalmologists (Part I)Documento7 páginasInterpretation of Magnetic Resonance Imaging of Orbit: Simplifi Ed For Ophthalmologists (Part I)Abid AliAinda não há avaliações
- Radionuclide Production Methods and ApplicationsDocumento21 páginasRadionuclide Production Methods and ApplicationsFeby Kusuma DewiAinda não há avaliações
- Chapter 17 Single Photon Emission Computed TomographyDocumento28 páginasChapter 17 Single Photon Emission Computed TomographyJohnnie LópezAinda não há avaliações
- 103manual QAP Radiologi Pindaan Januari 2019Documento115 páginas103manual QAP Radiologi Pindaan Januari 2019UMGC Sri RampaiAinda não há avaliações
- Grids and Scatter ReductionDocumento79 páginasGrids and Scatter ReductionMondiaal Financial ServicesAinda não há avaliações
- Basics of Diffusion and Perfusion MRIDocumento11 páginasBasics of Diffusion and Perfusion MRIPudhiavan AruviAinda não há avaliações
- 2012 ASTRO Radiation and Cancer Biology Practice Examination and Study Guide PDFDocumento193 páginas2012 ASTRO Radiation and Cancer Biology Practice Examination and Study Guide PDFKoustav Majumder100% (2)
- Personnel Monitoring DevicesDocumento63 páginasPersonnel Monitoring DevicesPramod Tike100% (1)
- EAU ESUR ESTRO SIOG Guidelines On Prostate Cancer Large Text V2Documento145 páginasEAU ESUR ESTRO SIOG Guidelines On Prostate Cancer Large Text V2DellaAinda não há avaliações
- Essential Guidelines for Trauma RadiographyDocumento69 páginasEssential Guidelines for Trauma RadiographySyuhada AzmiAinda não há avaliações
- Physics Lecture on Mammography X-Ray SystemsDocumento42 páginasPhysics Lecture on Mammography X-Ray SystemsLajja Parikh PatelAinda não há avaliações
- Nuclear MedicineDocumento2 páginasNuclear MedicineRadlinkSingaporeAinda não há avaliações
- Proton Therapy for Cancer Treatment Using High-Energy ProtonsDocumento48 páginasProton Therapy for Cancer Treatment Using High-Energy ProtonsSUBHA100% (1)
- Basic QA RadiologyDocumento55 páginasBasic QA RadiologyWahyu Widhianto100% (10)
- Finals Rad ProtectDocumento7 páginasFinals Rad ProtectNicko PerezAinda não há avaliações
- Radio BiologyDocumento26 páginasRadio BiologyMAN MedanAinda não há avaliações
- 10 Intraoperative RadiotherapyDocumento11 páginas10 Intraoperative RadiotherapyDgek LondonAinda não há avaliações
- Radiology Morning 5 TH Sep 2018Documento10 páginasRadiology Morning 5 TH Sep 2018Arshad AliAinda não há avaliações
- MRI Lecture NotesDocumento33 páginasMRI Lecture NotesBrandon44Ainda não há avaliações
- High Yield Psychiatry Shelf ReviewDocumento43 páginasHigh Yield Psychiatry Shelf Reviewconfusedmage90% (10)
- Learn The Brachial Plexus in Five Minutes or LessDocumento21 páginasLearn The Brachial Plexus in Five Minutes or LesskavithaAinda não há avaliações
- BF Nutrition 3 RD Ed Pocket GuideDocumento94 páginasBF Nutrition 3 RD Ed Pocket GuideengkjAinda não há avaliações
- Inpatient ConstipationDocumento14 páginasInpatient ConstipationunknownxemAinda não há avaliações
- AAMC - Education Debt ManagerDocumento56 páginasAAMC - Education Debt ManagerunknownxemAinda não há avaliações
- USMLE Step I - Lab ValuesDocumento2 páginasUSMLE Step I - Lab ValuesunknownxemAinda não há avaliações
- PE Final Notes - AbdomenDocumento2 páginasPE Final Notes - AbdomenunknownxemAinda não há avaliações
- Pulm ChartsDocumento4 páginasPulm ChartsunknownxemAinda não há avaliações
- Pharm Drug FileDocumento46 páginasPharm Drug FileunknownxemAinda não há avaliações
- Latin Anatomy TermsDocumento5 páginasLatin Anatomy TermsunknownxemAinda não há avaliações
- Chapter 11 - Signal TransductionDocumento19 páginasChapter 11 - Signal TransductionunknownxemAinda não há avaliações
- CD Molecules ReferenceDocumento25 páginasCD Molecules ReferenceunknownxemAinda não há avaliações
- #End of Life - Helping With Comfort and Care (NIH)Documento72 páginas#End of Life - Helping With Comfort and Care (NIH)unknownxemAinda não há avaliações
- Aorta, Branches, and Related VesselsDocumento1 páginaAorta, Branches, and Related VesselsunknownxemAinda não há avaliações
- Carbohydrate Metabolism ReviewDocumento21 páginasCarbohydrate Metabolism Reviewunknownxem100% (3)
- Chapter 11 - Signal TransductionDocumento19 páginasChapter 11 - Signal TransductionunknownxemAinda não há avaliações
- The Liver and The Biliary SystemDocumento4 páginasThe Liver and The Biliary SystemunknownxemAinda não há avaliações
- Latin Anatomy TermsDocumento5 páginasLatin Anatomy TermsunknownxemAinda não há avaliações
- Scholarships and Grants For Med StudentsDocumento7 páginasScholarships and Grants For Med StudentsunknownxemAinda não há avaliações
- Columbia GSAS - Drug Absorption, Distribution, and EliminatinoDocumento38 páginasColumbia GSAS - Drug Absorption, Distribution, and EliminatinounknownxemAinda não há avaliações
- Chapter 11 - Signal TransductionDocumento19 páginasChapter 11 - Signal TransductionunknownxemAinda não há avaliações
- Reproductive MedicineDocumento330 páginasReproductive MedicineunknownxemAinda não há avaliações
- MCAT2015 PreviewguideDocumento153 páginasMCAT2015 PreviewguideMiao JingyaAinda não há avaliações
- α and ß carbohydrates PDFDocumento2 páginasα and ß carbohydrates PDFunknownxemAinda não há avaliações
- Glycolysis PDFDocumento2 páginasGlycolysis PDFunknownxemAinda não há avaliações
- Transferable Skills in MedicineDocumento4 páginasTransferable Skills in MedicineunknownxemAinda não há avaliações
- AMSA - Diversifying Your Pool of Potential Medical SchoolsDocumento4 páginasAMSA - Diversifying Your Pool of Potential Medical SchoolsunknownxemAinda não há avaliações
- Healthcare Policy - The BasicsDocumento66 páginasHealthcare Policy - The BasicsunknownxemAinda não há avaliações
- Race, Money, and MedicinesDocumento5 páginasRace, Money, and MedicinesunknownxemAinda não há avaliações
- QCU Student Group Documents Mary and Christ Clinic's Manual SystemDocumento4 páginasQCU Student Group Documents Mary and Christ Clinic's Manual SystemChris ValduezaAinda não há avaliações
- Comorbidities of Hearing Loss and The Implications of Multimorbidity For Audiological Care. Hearing Research - 10.1016:j.heares.2018.06.008Documento12 páginasComorbidities of Hearing Loss and The Implications of Multimorbidity For Audiological Care. Hearing Research - 10.1016:j.heares.2018.06.008ALEIRAMGONZALEZAinda não há avaliações
- Introduction To Artificial Respiration and Cardiopulmonary ResuscitationDocumento21 páginasIntroduction To Artificial Respiration and Cardiopulmonary ResuscitationMark Kenneth CeballosAinda não há avaliações
- Continuous Positive Airway PressureDocumento19 páginasContinuous Positive Airway PressureBFKHOAinda não há avaliações
- LP2 MAJOR EXAM 4 Files Merged 2 Files MergedDocumento285 páginasLP2 MAJOR EXAM 4 Files Merged 2 Files MergedBianca ArceAinda não há avaliações
- Ra-031103 - Professional Teacher - Secondary (Tle) - Tacloban - 10-2022Documento135 páginasRa-031103 - Professional Teacher - Secondary (Tle) - Tacloban - 10-2022AILENAinda não há avaliações
- 00 Medical-Imaging-Preface-Waleed-AltalabiDocumento5 páginas00 Medical-Imaging-Preface-Waleed-Altalabiمحمدعبدالخالق العلوانيAinda não há avaliações
- Complications of Blood TransfusionsDocumento4 páginasComplications of Blood TransfusionsZain Hadi100% (1)
- Patient Scenario, Chapter 19, Nutritional Needs of A NewbornDocumento3 páginasPatient Scenario, Chapter 19, Nutritional Needs of A NewbornNobiliary ortizAinda não há avaliações
- SAGO Pharma Inc Rev2.1Documento17 páginasSAGO Pharma Inc Rev2.1wafaa mustafaAinda não há avaliações
- CHRONIC WOUND EVALUATION AND MANAGEMENTDocumento36 páginasCHRONIC WOUND EVALUATION AND MANAGEMENTEdwar RusdiantoAinda não há avaliações
- New Classification of General Hospitals in The Philippines Based On Functional CapacityDocumento5 páginasNew Classification of General Hospitals in The Philippines Based On Functional CapacityVer Bautista100% (1)
- Is It An Abortion or A D&C - Medically Speaking, - The Steps Are The SameDocumento9 páginasIs It An Abortion or A D&C - Medically Speaking, - The Steps Are The SamesiesmannAinda não há avaliações
- Module 1 To 5 QM Training For Blood Transfusion Services WHO PDFDocumento182 páginasModule 1 To 5 QM Training For Blood Transfusion Services WHO PDFRose jane Tambasen100% (1)
- Renal Calculi Lesson PlanDocumento14 páginasRenal Calculi Lesson PlanVeenasravanthiAinda não há avaliações
- Long-Term Results of the Kumamoto Study on Optimal Diabetes Control in Type 2 Diabetic PatientsDocumento19 páginasLong-Term Results of the Kumamoto Study on Optimal Diabetes Control in Type 2 Diabetic PatientsCarlosZamAinda não há avaliações
- Bipolar 1 Disorder NCPDocumento3 páginasBipolar 1 Disorder NCPJoy-Rena Sabinay OchondraAinda não há avaliações
- Henrietta Lacks: Dr. Roz Iasillo Trinity High School River Forest, ILDocumento13 páginasHenrietta Lacks: Dr. Roz Iasillo Trinity High School River Forest, ILRoz IasilloAinda não há avaliações
- Versed dosing guideDocumento4 páginasVersed dosing guideintrovert ikonAinda não há avaliações
- Essential Nursing Procedures Assignment - 092039Documento14 páginasEssential Nursing Procedures Assignment - 092039IRA MONIQUE CABADENAinda não há avaliações
- Excerpt From "Diabetes: A Lifetime of Being Too Sweet"Documento9 páginasExcerpt From "Diabetes: A Lifetime of Being Too Sweet"waltcrockerAinda não há avaliações
- Multimodal Early Onset Stimulation (MEOS) in Rehabilitation After Brain InjuryDocumento10 páginasMultimodal Early Onset Stimulation (MEOS) in Rehabilitation After Brain InjuryVendiAinda não há avaliações
- Parenteral Nutrition CalculationsDocumento62 páginasParenteral Nutrition CalculationsaqeelaadnanAinda não há avaliações
- NCP Knowledge Deficit (FINAL)Documento8 páginasNCP Knowledge Deficit (FINAL)Nikki Ricafrente89% (9)
- Evmlu Uganda.2020Documento124 páginasEvmlu Uganda.2020ALINOMUGASHA EMMANUELAinda não há avaliações
- An Analysis of Ethical Issues in Pharmaceutical IndustryDocumento19 páginasAn Analysis of Ethical Issues in Pharmaceutical IndustrySuresh KodithuwakkuAinda não há avaliações
- Chapter 03: Health Policy and The Delivery SystemDocumento11 páginasChapter 03: Health Policy and The Delivery SystemStephany ZatarainAinda não há avaliações
- Homeopathic Remedy Pictures Alexander Gothe Julia Drinnenberg.04000 1Documento6 páginasHomeopathic Remedy Pictures Alexander Gothe Julia Drinnenberg.04000 1BhargavaAinda não há avaliações
- Medicine JC-SC WCS Summary (Neurology)Documento6 páginasMedicine JC-SC WCS Summary (Neurology)Peter LeeAinda não há avaliações
- Kelompok 7 - 4b - Buku Saku Antibiotik Dan AntivirusDocumento62 páginasKelompok 7 - 4b - Buku Saku Antibiotik Dan AntivirusWidya PratiwiAinda não há avaliações
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNo EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNota: 4 de 5 estrelas4/5 (402)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessNo EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessNota: 4.5 de 5 estrelas4.5/5 (327)
- The Age of Magical Overthinking: Notes on Modern IrrationalityNo EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityNota: 4 de 5 estrelas4/5 (13)
- The Ultimate Guide To Memory Improvement TechniquesNo EverandThe Ultimate Guide To Memory Improvement TechniquesNota: 5 de 5 estrelas5/5 (34)
- Techniques Exercises And Tricks For Memory ImprovementNo EverandTechniques Exercises And Tricks For Memory ImprovementNota: 4.5 de 5 estrelas4.5/5 (40)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNo EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNota: 3.5 de 5 estrelas3.5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeAinda não há avaliações
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNo EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNota: 5 de 5 estrelas5/5 (78)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisNo EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisNota: 4 de 5 estrelas4/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityNo EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityNota: 3.5 de 5 estrelas3.5/5 (2)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNo EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsAinda não há avaliações
- The Obesity Code: Unlocking the Secrets of Weight LossNo EverandThe Obesity Code: Unlocking the Secrets of Weight LossNota: 5 de 5 estrelas5/5 (3)
- The Happiness Trap: How to Stop Struggling and Start LivingNo EverandThe Happiness Trap: How to Stop Struggling and Start LivingNota: 4 de 5 estrelas4/5 (1)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingNo EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingNota: 5 de 5 estrelas5/5 (4)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingNo EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingNota: 3.5 de 5 estrelas3.5/5 (31)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsNo EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsNota: 4.5 de 5 estrelas4.5/5 (169)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNo EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsAinda não há avaliações
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNo EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNota: 4.5 de 5 estrelas4.5/5 (41)
- The Tennis Partner: A Doctor's Story of Friendship and LossNo EverandThe Tennis Partner: A Doctor's Story of Friendship and LossNota: 4.5 de 5 estrelas4.5/5 (4)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisNo EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisNota: 5 de 5 estrelas5/5 (3)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.No EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Nota: 4.5 de 5 estrelas4.5/5 (110)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisNo EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisNota: 5 de 5 estrelas5/5 (8)