Escolar Documentos
Profissional Documentos
Cultura Documentos
Managing Geriatric Patients
Enviado por
Sarah KahilDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Managing Geriatric Patients
Enviado por
Sarah KahilDireitos autorais:
Formatos disponíveis
By: Sarah Kahil
Course: ENDO511
19/12/2015
MANAGING GERIATRIC
PATIENTS
PATIENTS MAY BE:
1. Tempered
2. Uncooperative
3. Low dental IQ
2 Types of Patients:
- Relatively healthy older adults: functionally independent
- Unhealthy older patients: have complex conditions and need
assistance
1. Find out the patients daily eating and resting habits to determine
the ideal time for the appointment. Early morning is usually
preferable.
2. Provide pillows for comfortable positioning in the chair.
3. Special needs may require rest room breaks.
4. Eye shades maybe needed to shield patient from intense light.
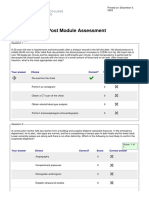
DIAGNOSIS AND TREATMENT PLAN
-
Clinical judgement should be made based on:
Patients complaint
History
Signs
Symptoms
Testing
Radiographs
MEDICAL HISTORY
Page 1 | 8
By: Sarah Kahil
Course: ENDO511
19/12/2015
Dramatic changes to C.V.S, Respiratory System, CNS.
Decline in liver and renal function. When predicting behavior and
interaction of drugs (anesthesia, analgesics, antibiotics)
UPDATE THE MEDICAL HISTORY
- Updating the medical history at each visit is very important.
- It may help to use a standard form listing various diseases
because many diseases of elderly are chronic and these patients
may under estimate the importance of informing you about a 30
years old chronic problem for example.
- Obtain information about drug therapy.
- Sensitivity to medications at every visit.
- Consult the physician for side effects and precautions
- Old patients with vision problems may need help filling out the
form, and you may need consult a family member or physician to
obtain further information.
- Because elder patients rarely present with an acute problem.
Treatment can be postponed until consultations are completed.
- Management of medical emergencies in the dental office is best
directed toward prevention rather than treatment.
CHIEF COMPLAINT
- First step in evaluating the patients condition is encouraging the
patient to talk about the problem.
- This consultation with the patient serves several purposes, not
only you can learn about the complaint but you can evaluate any
handy capping, ability to communicate and dental IQ.
- Most geriatric patients do not complain readily about signs or
symptoms of pulpal and periapical disease and may consider
them to be minor compared with other health concerns and
discomfort.
- A disease process usually arises as an acute problem in children
but assumes a more chronic or less dramatic form in the older
adult.
Page 2 | 8
By: Sarah Kahil
Course: ENDO511
19/12/2015
- Pain associated with vital pulps (referred pain; or pain caused by
heat, cold, or sweets) seems to be reduced with age, and severity
seems to diminish over time.
- Pulpal healing capacity is also reduced, and necrosis may occur
quickly after microbial invasion, again with reduced symptoms.
DENTAL HISTORY
Search patients records
Explore their memories to determine the history of involved teeth or
surrounding area
Subjective symptoms:
Examiner should pursue responses to questions about the chief
complaint, the stimulus or irritant that causes pain, nature of pain and
its relationship to the stimulus or irritant.
Diagnostic procedures:
It is important to remember that pulpal symptoms are usually chronic
in older patients and other sources of oro-facial pain should be ruled
out when pain is not soon localized.
Objective Signs:
- Intraoral and extra oral examination
- Exposures to factors that contribute to oral cancers accumulate
with age
- Many systemic diseases may initially manifest oral signs or
symptoms
- Missing teeth, tilt, rotation, supra eruption of adjacent and
opposing teeth contribute to reduced functional ability.
- Resultant loss of chewing efficiency leads to a higher
carbohydrate diet of softer, more cariogenic foods increasing
susceptibility to caries and periodontal disease.
- Increased sugar intake to compensate for loss of taste and
xerostomia are also factors in the renewed susceptibility to decay.
Page 3 | 8
By: Sarah Kahil
Course: ENDO511
19/12/2015
- Saliva has a significant role in the maintenance of oral and
general health
- Aging has no significant clinical impact on salivary secretion.
- Most common cause of salivary hypofunction in the elderly is
medication use and is most commonly associated with dental
caries and oral fungal infections.
Gingival recession: creates sensitivity which is hard to control,
exposes cementum and dentin that are less resistant to decay
causing root caries
Removal of root caries irritating to the pulp and often results in pulp
exposures or reparative dentin formation that affects the negotiation
of the canal if root canal later is needed.
- Interproximal caries is difficult to restore.
- Restoration failure as a result of continued decay is common.
Attrition, Abrasion and Erosion also exposes dentin through a slower
process that allows the pulp to respond with dentinal sclerosis and
reparative dentin.
Secondary dentin formation may eventually result in complete pulp
obliteration.
In anterior teeth secondary dentin is deposited on the lingual surface
while in molar teeth its deposition occurs on the floor of the pulp
chamber.
PULPAL CHANGES DUE TO AGING
- Decrease in size and number of pulpal cells
- Increase in number of collagen fibers
- Decrease in size of pulpal space due to continued dentin
formation
- Decrease in number of pulpal blood vessels
- Decrease in number of pulpal nerve fibers
Page 4 | 8
By: Sarah Kahil
Course: ENDO511
19/12/2015
- Cellularity of older pulp tissue gradually decreases in size and
number and may disappear at certain areas.
- Canal and chamber volume is inversely proportional to age
- Reparative dentin resulting from restorative procedures, trauma,
attrition and recurrent caries also contribute to diminution of
canal and chamber size
- CDJ moves farther from the radiograph apex with continued
cementum deposition
- Thickness of young apical cementum is 100to 200 micro m and
increases with age to 2-3 times that thickness
- Calcification process associated with aging appears clinically to be
more of linear type than that which occurs in a young tooth in
response to caries, pulpotomy or trauma.
- Dentinal tubules becomes more occluded with advancing age,
decreasing tubular permeability
- Lateral and accessory canals can calcify by age, thus decreasing
their clinical significance.
- Violating principles of cavity design combined with the loss of
resiliency that results from a reduced organic component to the
dentin can increase susceptibility to cracks and cuspal fractures.
- Pulp exposures caused by cracks are less likely to present acute
problems in older patients and often penetrate the sulcus to
create a periodontal defect or even a periapical one.
- High
magnification
available
with
microscopes
and
transillumination during access opening and canal exploration
permits visualization of the extent of cracks in determining
prognosis
- Cracks is of little significance in the absence of complaints.
- Cracks detected while pulp is still vital can offer good prognosis
- Vertically cracked teeth should always be considered when pulpal
or periapical disease is observed and little or no cause for pulpal
irritation can be observed clinically or radiographically.
- Narrow, boney wall defects associated with non-vital pulps are
usually sinus tracts, but they can be resistant to root canal
therapy alone when with time they become chronic periodontal
pockets.
Page 5 | 8
By: Sarah Kahil
Course: ENDO511
19/12/2015
- Patients with diabetes have increased periodontal disease in
endodontic treated teeth and have a reduced likelihood of success
of endodontic treatment in cases with preoperative periradicular
lesions.
PULP TESTING
- Vitality response must correlate with clinical and radiographical
findings and be a supplement in developing clinical judgement
- Slow and gentle testing should be done to determine pulpal
and periapical status and whether palliative or definitive
therapy is indicated.
- Fewer nerve branches are present in older pulps, due to
retrogressive changes resulting from mineralization of the
nerve and nerve sheath.
- Due to reduced neural and vascular response, response to
stimuli and irritants may be lowered. Presence or absence of
response is of limited value and must be correlated with other
tests.
- Extensive restorations, pulp recession and excessive
calcifications are limitations in both performing and interpreting
results of electric and thermal tests. Pulp testers are of little
value.
- Test cavity is generally less useful,
- Viral pulps can sometimes be exposed and even negotiated
with a file with minimal pain; then the root canal becomes part
of the diagnostic procedures.
- So test cavity should be used only when other findings are
suggestive but not conclusive.
- Diffuse pain of vague origin is also uncommon in older pulps
and limits the need for selective anesthesia
- Non-odontogenic sources should be considered when factors
associated with pulpal disease are not readily identified or
when acute pain does not localize within a short time.
- Discoloration of single teeth may indicate pulp death, but this
is uncommon with advanced age, when it occurs discoloration
is usually a result of restorative material following RCT because
Page 6 | 8
By: Sarah Kahil
Course: ENDO511
19/12/2015
dentin is generally thicker in older patients, it is not an
indicator of pulp necrosis.
- Dentin deposition produces a yellow, opaque color that would
indicate progressive calcification in a younger pulp; however
this is common in older teeth.
RADIOGRAPHS
- Digital radiography may be more useful than conventional
radiography in detecting early bone changes.
- Older patient may find difficulty in film placement, holders should
be used.
- Pulp recession by reparative dentin and complicated by pup
stones and dystrophic calcification
- Depth of the chamber should be measured from the occlusal
surface and its mesiodistal position noted.
- Receding pulp horns that are apparent on radiograph may remain
microscopically much higher.
Canals should be examined for:
-
Numbers
Size
Shape
Curvature
Resorption associated with chronic apical periodontitis may
significantly alter the shape of the apex and the anatomy of the
foramen through inflammatory osteoclastic activity.
Hyper cementosis completely obscure the apical anatomy and result in
constriction far from radiographic apex due to continued cementum
deposition.
Page 7 | 8
By: Sarah Kahil
Course: ENDO511
19/12/2015
Lamina dura should be examined in its entirely and anatomic
landmarks distinguished from periapical radiolucencies and radioopacities,
The incidence of some odontogenic and non-odontogenic cysts and
tumors increases with age and should be considered when vitality does
not correlate with radiographic findings.
Dense bone indicate the need for increased exposures times to
improve contrast needed to see the canal and root anatomy.
Page 8 | 8
Você também pode gostar
- Final Version of AdpieDocumento22 páginasFinal Version of Adpieapi-461805331Ainda não há avaliações
- Primary Preventive Dentistry - 6th EdDocumento847 páginasPrimary Preventive Dentistry - 6th EdYasser KamalAinda não há avaliações
- Oral Wound Healing: Cell Biology and Clinical ManagementNo EverandOral Wound Healing: Cell Biology and Clinical ManagementHannu LarjavaAinda não há avaliações
- Ejaculation by Command - Lloyd Lester - Unstoppable StaminaDocumento21 páginasEjaculation by Command - Lloyd Lester - Unstoppable StaminaEstefania LopezAinda não há avaliações
- Atls Pre Test SolvedDocumento18 páginasAtls Pre Test SolvedDr.Mukesh KumarAinda não há avaliações
- Leukoplakia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo EverandLeukoplakia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsAinda não há avaliações
- Demin/Remin in Preventive Dentistry: Demineralization By Foods, Acids, And Bacteria, And How To Counter Using RemineralizationNo EverandDemin/Remin in Preventive Dentistry: Demineralization By Foods, Acids, And Bacteria, And How To Counter Using RemineralizationAinda não há avaliações
- Dental Pulp Lecture 3Documento10 páginasDental Pulp Lecture 3Mohamed Harun B. SanohAinda não há avaliações
- Dental Health Lesson Plan 3Documento4 páginasDental Health Lesson Plan 3api-509225720Ainda não há avaliações
- Oral Histology-Lab-3Documento5 páginasOral Histology-Lab-3Mohamed TawalbeAinda não há avaliações
- 3 - Dentino-Pulp Complex (Mahmoud Bakr)Documento129 páginas3 - Dentino-Pulp Complex (Mahmoud Bakr)MobarobberAinda não há avaliações
- Dentin, Enamel, Pulp StructureDocumento27 páginasDentin, Enamel, Pulp StructureBismah TayyabAinda não há avaliações
- Indices PerioDocumento15 páginasIndices PerioJunaid100% (2)
- Oral Hist1Documento21 páginasOral Hist1saleemshaikh23Ainda não há avaliações
- Docslide - Us Dentogingival-UnitDocumento53 páginasDocslide - Us Dentogingival-UnitarmAinda não há avaliações
- 2 - Enamel (Mahmoud Bakr)Documento133 páginas2 - Enamel (Mahmoud Bakr)MobarobberAinda não há avaliações
- B - en AmelogenesisDocumento23 páginasB - en Amelogenesisapi-371033150% (2)
- 1-Tooth Development & Embryology (DR - Mahmoud Bakr)Documento95 páginas1-Tooth Development & Embryology (DR - Mahmoud Bakr)Mobarobber50% (2)
- Chapter 6 Oral Health and The Aging Population (Geriatric Oral Health)Documento28 páginasChapter 6 Oral Health and The Aging Population (Geriatric Oral Health)dentovitroAinda não há avaliações
- DentineDocumento19 páginasDentineKhalid Mahmud Arifin0% (1)
- Sextant CPITN scores for periodontal examDocumento2 páginasSextant CPITN scores for periodontal examAnthony NguAinda não há avaliações
- 4 - The Periodontium (Mahmoud Bakr)Documento128 páginas4 - The Periodontium (Mahmoud Bakr)MobarobberAinda não há avaliações
- D-Dentin-Lec 1Documento45 páginasD-Dentin-Lec 1api-3710331100% (7)
- Non-Caries Dental DiseaseDocumento61 páginasNon-Caries Dental Diseaseapi-19916399Ainda não há avaliações
- CementumDocumento10 páginasCementumAshish BisaneAinda não há avaliações
- 6 - Eruption, Shedding and Maxillary Sinus (Mahmoud Bakr)Documento136 páginas6 - Eruption, Shedding and Maxillary Sinus (Mahmoud Bakr)Mobarobber100% (2)
- Dental PulpDocumento19 páginasDental Pulpxehd10100% (5)
- Plaque ControlDocumento52 páginasPlaque ControlIbrahim AbdelHadi100% (1)
- Difference Between Primary and Permanent TeethDocumento17 páginasDifference Between Primary and Permanent TeethMohd Tauseef Khan100% (1)
- Dental HygieneDocumento3 páginasDental Hygieneapi-507354264Ainda não há avaliações
- 5 - Oral Mucosa and Salivary Glands (Mahmoud Bakr)Documento115 páginas5 - Oral Mucosa and Salivary Glands (Mahmoud Bakr)MobarobberAinda não há avaliações
- Development and Eruption of The TeethDocumento5 páginasDevelopment and Eruption of The TeethZHAREIGHNEILE C. MAMOLOAinda não há avaliações
- Periodontal Diseases in Children PedoDocumento34 páginasPeriodontal Diseases in Children PedoFourthMolar.comAinda não há avaliações
- 1 Dental IndicesDocumento3 páginas1 Dental IndicesAinun Nur Arifah100% (2)
- Tooth DevelopmentDocumento20 páginasTooth DevelopmentArslan Jokhio0% (1)
- 6.structure and Components of The Smear Layer / Orthodontic Courses by Indian Dental AcademyDocumento6 páginas6.structure and Components of The Smear Layer / Orthodontic Courses by Indian Dental Academyindian dental academyAinda não há avaliações
- Anatomy of PalateDocumento33 páginasAnatomy of Palatekvellingiri0% (1)
- Oral Histo Midterm Review PDFDocumento17 páginasOral Histo Midterm Review PDFHãnëën TwalbehAinda não há avaliações
- Life Cycle of AmeloblastDocumento3 páginasLife Cycle of AmeloblastArun Shalini SinghAinda não há avaliações
- Odontogenic Tumours - (2) L5Documento28 páginasOdontogenic Tumours - (2) L5nooraaaAinda não há avaliações
- PulpDocumento54 páginasPulpAnsh DuttaAinda não há avaliações
- Introduction To Community Dentistry and Dental Public HealthDocumento36 páginasIntroduction To Community Dentistry and Dental Public HealthAnosha RiazAinda não há avaliações
- Diagnosing Benign Jaw Lesions with ImagingDocumento17 páginasDiagnosing Benign Jaw Lesions with ImagingMaria Alejandra AtencioAinda não há avaliações
- Children's Periodontal Problems and TreatmentsDocumento49 páginasChildren's Periodontal Problems and TreatmentsRaksmey PhanAinda não há avaliações
- Principles of Surgery: The Two Principal Requirements (1) Adequate Visibility (2) AssistanceDocumento16 páginasPrinciples of Surgery: The Two Principal Requirements (1) Adequate Visibility (2) AssistanceVijay K PatelAinda não há avaliações
- TMJ & Max SinusDocumento3 páginasTMJ & Max Sinusapi-3738787Ainda não há avaliações
- Tooth DevelopmentDocumento8 páginasTooth DevelopmentKhalid Mahmud Arifin100% (9)
- Dental ErosionDocumento4 páginasDental ErosionmirfanulhaqAinda não há avaliações
- Development of TeethDocumento127 páginasDevelopment of Teethdentistpro.orgAinda não há avaliações
- Odontogenic Tumors of Oral Cavity: Dr. Deepak K. GuptaDocumento44 páginasOdontogenic Tumors of Oral Cavity: Dr. Deepak K. GuptaBinek NeupaneAinda não há avaliações
- Oral Histology Quiz - What Will Happen If (AmCoFam)Documento2 páginasOral Histology Quiz - What Will Happen If (AmCoFam)AmericanCornerFamilyAinda não há avaliações
- Periodicity DentalGuideDocumento52 páginasPeriodicity DentalGuideSalam BataienehAinda não há avaliações
- Slide 14 Diseases of Salivary Glands IDocumento67 páginasSlide 14 Diseases of Salivary Glands IJustDen09Ainda não há avaliações
- Anatomy of Primary TeethDocumento4 páginasAnatomy of Primary Teethaphist87Ainda não há avaliações
- Madhudentinppt 170809045059Documento74 páginasMadhudentinppt 170809045059siyaAinda não há avaliações
- Mounting Dental X-RaysDocumento6 páginasMounting Dental X-RaysZahid AhmadAinda não há avaliações
- Mandibular Condylar and Subcondylar Fractures PDFDocumento16 páginasMandibular Condylar and Subcondylar Fractures PDFWayan Sutresna YasaAinda não há avaliações
- Cyst of Jaws-RadiologyDocumento60 páginasCyst of Jaws-RadiologyshabeelpnAinda não há avaliações
- Developmental Disturbances of TeethDocumento65 páginasDevelopmental Disturbances of Teethisraa0dentist100% (4)
- Basic Level of Dental Resins - Material Science & Technology: 4th Edition, 2nd VersionNo EverandBasic Level of Dental Resins - Material Science & Technology: 4th Edition, 2nd VersionAinda não há avaliações
- Classification of Periodontal DiseaseDocumento18 páginasClassification of Periodontal DiseaseSarah KahilAinda não há avaliações
- Infection Control - MicrobiologyDocumento9 páginasInfection Control - MicrobiologySarah KahilAinda não há avaliações
- Endodontic MicrobiologyDocumento9 páginasEndodontic MicrobiologySarah KahilAinda não há avaliações
- Procedural AccidentsDocumento19 páginasProcedural AccidentsSarah KahilAinda não há avaliações
- CAMBRADocumento5 páginasCAMBRASarah KahilAinda não há avaliações
- Endo Perio ProblemsDocumento8 páginasEndo Perio ProblemsSarah KahilAinda não há avaliações
- Endo Perio ProblemsDocumento8 páginasEndo Perio ProblemsSarah KahilAinda não há avaliações
- Clinical Use of PeriotomesDocumento1 páginaClinical Use of PeriotomesSarah KahilAinda não há avaliações
- Schonert-Reichl-Educating The Heart As Well As The MindDocumento7 páginasSchonert-Reichl-Educating The Heart As Well As The MindnewoldnoneAinda não há avaliações
- HFpEF Management 2023Documento10 páginasHFpEF Management 2023ctsakalakisAinda não há avaliações
- MortuaryDocumento6 páginasMortuaryDr.Rajesh KamathAinda não há avaliações
- Maternal Serum Alpha-Fetoprotein (MSAFP)Documento2 páginasMaternal Serum Alpha-Fetoprotein (MSAFP)Shaells JoshiAinda não há avaliações
- Name: Eric P. Alim Year & Section: CMT-1Documento27 páginasName: Eric P. Alim Year & Section: CMT-1Ariel BobisAinda não há avaliações
- Report On Progress of Professional Portfolio - NFDN 1002Documento2 páginasReport On Progress of Professional Portfolio - NFDN 1002api-317607382Ainda não há avaliações
- 4ps Chapter 1Documento14 páginas4ps Chapter 1Charesmie JuradoMenoza ImperialGicale100% (1)
- Successful Strategy To Decrease Indwelling Catheter Utilization Rates inDocumento7 páginasSuccessful Strategy To Decrease Indwelling Catheter Utilization Rates inWardah Fauziah El SofwanAinda não há avaliações
- Standards For Improving The Quality of Care For Small and Sick Newborns in Health Facilities 2020Documento152 páginasStandards For Improving The Quality of Care For Small and Sick Newborns in Health Facilities 2020Shuaib KauchaliAinda não há avaliações
- DentaPure Sell SheetDocumento2 páginasDentaPure Sell SheetJeff HowesAinda não há avaliações
- Evaluation and Management of Splenic Injury in Blunt Abdominal TraumaDocumento32 páginasEvaluation and Management of Splenic Injury in Blunt Abdominal TraumaImam Hakim SuryonoAinda não há avaliações
- Bombshell by Suzanne Somers - ExcerptDocumento12 páginasBombshell by Suzanne Somers - ExcerptCrown Publishing GroupAinda não há avaliações
- DNP 2021 A Women Justice Legal NeedsDocumento20 páginasDNP 2021 A Women Justice Legal Needsdito1972Ainda não há avaliações
- Internship Reflection PaperDocumento7 páginasInternship Reflection Paperapi-518707218Ainda não há avaliações
- Lower Gastrointestinal Bleeding: Practice EssentialsDocumento28 páginasLower Gastrointestinal Bleeding: Practice EssentialsJohnPaulOliverosAinda não há avaliações
- Oral Glucose Tolerance TestDocumento4 páginasOral Glucose Tolerance TestCyna Jane Yao AlcularAinda não há avaliações
- Health and SafetyDocumento26 páginasHealth and SafetyReza NugrahaAinda não há avaliações
- Traffic Rules LiteracyDocumento11 páginasTraffic Rules LiteracyMaricel AycoAinda não há avaliações
- Nursing Care PlanDocumento10 páginasNursing Care PlanGinel Laquiores100% (1)
- GERD-PPI MisconceptionsDocumento2 páginasGERD-PPI MisconceptionsLie LhianzaAinda não há avaliações
- Children Nutrition Action PlanDocumento64 páginasChildren Nutrition Action PlanpapayAinda não há avaliações
- RM NCC RN 8.0 CHP 21Documento21 páginasRM NCC RN 8.0 CHP 21LonaBrochenAinda não há avaliações
- Skills - Care of The Pregnant Patient ComputationsDocumento5 páginasSkills - Care of The Pregnant Patient ComputationsMichelle HutamaresAinda não há avaliações
- Lesson PlanDocumento3 páginasLesson PlanRenato Torio100% (1)
- Framework Nurafni SuidDocumento2 páginasFramework Nurafni SuidapninoyAinda não há avaliações
- Public Availability of Labeling CBE Guidance PDFDocumento6 páginasPublic Availability of Labeling CBE Guidance PDFMichael wangAinda não há avaliações
- SEHA Blood Bank With DiagramsDocumento15 páginasSEHA Blood Bank With DiagramsShahzaib HassanAinda não há avaliações
- FAO, WHO - Assuring Food Safety and Quality. Guidelines.2003 PDFDocumento80 páginasFAO, WHO - Assuring Food Safety and Quality. Guidelines.2003 PDFAlexandra Soares100% (1)