Escolar Documentos
Profissional Documentos
Cultura Documentos
DELTA 2016 DR Ghazy MY IMPLANT LECTURE PDF
Enviado por
Mohamed Hamed GhazyTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
DELTA 2016 DR Ghazy MY IMPLANT LECTURE PDF
Enviado por
Mohamed Hamed GhazyDireitos autorais:
Formatos disponíveis
2016-08-06
Level Five Class summer 2016
IMPLANTSUPPORTED
FIXED PROSTHESIS
BY Dr
Mohamed H. GHAZY
August 6, 2016
What is your 1st line of treatment to
restore this missing tooth
2016-08-06
Implant prosthodontics :
The phase of prosthodontics
concerning with replacement of
missing teeth and/or associated
structures by restorations that
are attached to dental implants
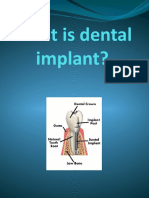
What is a dental implant ?
A
prosthetic
device
of
alloplastic material implanted
into the oral tissue beneath
the mucosal or/and periosteal
tissue for fixed or removable
prosthesis.
2016-08-06
Indication & contraindication
Indications
Contraindications
Lack of operator experience
Smoking
Pregnancy
Psychiatric disorders
Tumoricidal radiation to implant site
Antimetabolic treatment
Uncontrolled cardiovascular problems
Single tooth loss
Inability to wear a removable P.D.
Free end distal extension
Need for long span FPD with
questionable prognosis
Unfavorable number and location
of potential natural tooth abutment
Immunosuppression (chemotherapy,
HIV, etc)
Bone diseases, such as Histiocytosis X,
Paget's Disease and Fibrous Dysplasia
Uncontrolled hematologic disorders
such as Generalized Anemias,
Hemophilia
Endocrine disorders, such as
uncontrolled Diabetes Mellitus, Pituitary
and Adrenal insufficiency and
Hypothyroidism
2016-08-06
Treatment planning for implant patient
Indication &contraindication
Clinical evaluation
Adequate bone and anatomic structure
Visual inspection & palpation
Flabby excess tissues
Bony ridges
Sharp underlining osseous formations and undercuts
Radiographic evaluation
Panoramic view with small radio opaque reference
Cephalometric film to evaluate bone width
CT scan to locate inferior alveolar canal & maxillary sinuses
Diagnostic casts
Study the remaining dentition
Evaluate residual bone
Analyze maxillo-mandibular relationship
Diagnostic waxing and surgical templates
Bone sounding
With probe judging the soft tissue thickness and bone soundness
Subperiosteal
Endosteal plate
form
Transosteal
Endosteal
root form
2016-08-06
To the left you can
see a typical modern
Root form Implant
and to the right of
the implant is a
picture of a natural
tooth.
One can see how the
implant is designed
to replace the root of
a tooth by the
somewhat apparent
similarity.
Implant supported
prosthesis may be
Screw Retained
Transocclusal
Screw Retained
Transversal
Cemented
Fixed Partial Denture
2016-08-06
OSSEOINTEGRATION
A direct structural and functional
connection between ordered living bone
and the surface of a load carrying implant
Swedish professor of orthopedics
named Per-Ingvar Branemark
in 1965 he used the first titanium
dental implant into a human
volunteer
Implant most commonly used from
*Commercially pure (CP) titanium
*Titanium-aluminum-vanadium alloy
(Ti-6Al-4V) - stronger & used w/ smaller diameter
implants
* Ceramic
Why Titanium
High biocompatibility and bonding
ability with the bone
Light weight and high strength
Corrosion resistant
2016-08-06
Principles of Implant location
Anatomic limitation
General guide lines
Ideal bone should be 10 mm
vertical and 6 mm horizontal
Two mm above the superior
aspect of inferior alveolar canal
Five mm anterior to mental
foramen
one mm from the periodontal
ligament of adjacent tooth
Three mm between 2 implant to
ensure bone vitality.
Principles of Implant location
Anatomic limitation
Anterior maxilla
1- Minimum of 1 mm
between the implant apex
and nasal vestibule
2- Implant slightly off
midline on either sides of
incisive foramen.
2016-08-06
Principles of Implant location
Anatomic limitation
Posterior maxilla
Bone less dense, larger narrow spaces, and
thin cortex
1- One implant for every tooth
2- One mm of bone between the floor of
sinus and implant
Principles of Implant location
Anatomic limitation
Anterior mandible
1. One implant placed through the entire
cancellous bone
2. Five mm anterior to the foramen
2016-08-06
Principles of Implant location
Anatomic limitation
Posterior mandible
1.Two mm above the superior
aspect of inferior canal
2. More time required for
integration
3. Attachment of mylohyoid muscle
Principles of Implant location
Restorative consideration
Implant placement
1- Stay 1mm from the adjacent natural tooth but not so far
to for contouring restoration
2016-08-06
Principles of Implant location
Restorative consideration
Implant placement
2- Long axis of implant should be positioned in the central
fosse of the restoration
Less ideal location
Natural
tooth
Ideal
implant
placement
Optimal emergence profile: implant positioned
2-3 mm inferior to emergence position of the restoration
10
2016-08-06
Implant and restoration size
1. Size should be considered during treatment planning
2. 4mm diameter for maxillary central
3. 3mm for mandibular incisors
4. 5-6mm for molars
Template extremely
useful for anterior
implant
Objectives
Surgical guide
1- Delineate the embrasures
2- Locate the implant within
the restoration contour
3- Align the implant within
the long axis of the
restoration
4- Identify the level of CIJ
or tooth emergence from
the soft tissue
11
2016-08-06
Wax model of a tooth to be replaced in the surgical guide
12
2016-08-06
Surgical guide template
Stent used as guide for implant placement
13
2016-08-06
Surgical guide for correct
implant placement
Computer aided
surgical stent
(Stereolithrography)
14
2016-08-06
Implant surgery
Surgical access
Implant placement
Postoperative evaluation
Implant uncover
Implant restorations
Significant factors for success
1- Precise placement
2- A traumatic surgery
3- Unloaded healing
4- Passive restoration
Guide drill / 2mm twist drill / Pilot drill / 3mm twist drill / Countersink
15
2016-08-06
16
2016-08-06
Components of an
implant restoration
Screw- retained implant
restorations consist of
three components.
Restoration
Composite resin
Gutta percha
Retaining screw
Abutment screw
(a) Implant fixture
(b) Abutment
Abutment
(c) Restoration
Implant fixture
- The abutment screw secures
the abutment to the fixture
- The prosthetic retention
screw secures the prosthesis to
the abutment.
Components of an
implant restoration
Screw- retained implant
restorations consist of
three components.
(a) Implant fixture
(b) Abutment
Restoration
Composite resin
Gutta percha
Prosthetic retaining
screw
Abutment retaining
screw
Abutment
(c) Restoration
Implant fixture
- The abutment screw secures
the abutment to the fixture
- The prosthetic retention
screw secures the prosthesis to
the abutment.
17
2016-08-06
Prosthetic Crown
Look and feel of real tooth.
Easily replaced.
Implant Abutment
Secures the crown to the Dental
Implant. Can be straight or angled
depending on implant location
Dental Implant
Should promote bone in-growth.
Structure and geometry differences are
the selling point for most companies.
18
2016-08-06
Lekholm and Zarb bone type classification
Type I bone
homogenous, compact bone
Type II bone
Thick compact bone layer surrounding a
core of dense trabecular bone
Type III bone
Thin cortical bone layer surrounding a
core of dense trabecular bone of good
strength
Type IV bone
Thin cortical bone layer surrounding core
of low density .
Bone density is a key factor when predicting implant stability.
Implant restorations
Impression post
Closed tray
Impression
Imp post & analog
Imp post & analog
connected
Imp post & analog
relocated on the
impression
Polyether soft tissue
injected around
analog before
pouring
19
2016-08-06
Poured cast
Contouring of the
soft tissue material
Impression coping
locates the analog in
the same position in
the cast as the
implant in the mouth
Zirconia abutment
for cement retained
restoration selected
Zirconia abutment
seated on cast
Zirconia abutment
seated in the mouth
20
2016-08-06
Fourth year Class 2013/2014
IMPLANTSUPPORTED FIXED PROSTHESIS
BY Dr
MoHAMeD H. GHAZY
march 18, 2014
Implant insertion into
the prepared socket
21
2016-08-06
Unscrewing the abutment from the implant
fixture, screw covering and suturing
Removal of the cover screw in
the 2nd stage and abutment
attached to the fixture as a
coping ready for impression
22
2016-08-06
The abutment removed from the implant
fixture
Abutment and its implant analog and
repositioned in the impression
23
2016-08-06
Abutment prepared to its final form in the
working cast
Prepared abutment and final restoration
in the patient mouth
24
2016-08-06
Prosthetic Crown
Look and feel of real tooth.
Easily replaced.
Implant Abutment
Secures the crown to the Dental
Implant. Can be straight or angled
depending on implant location
Dental Implant
Should promote bone in-growth.
Structure and geometry
differences are the selling point
for most companies.
Clinical Implant system components
Implant body
Is the component placed within the bone during
1st stage surgery
Titanium screw
Titanium
screw
Hydroxyl
appetite
coated
screw
Hydroxyl
Apatite
coated
cylinder
Titanium plasma
sprayed cylinder
25
2016-08-06
Two images showing two different types of tapered,
cylindrical implants. One looks like a Christmas tree with fins
projecting out to the sides; the other shows a special surface
treatment consisting of spherical titanium beads.
Cover screw
It is the component placed over the dental implant during the
osseointegration phase
to seal the occlusal surface of the implant and prevent tissue from
proliferating into the internal portion of the implant body
It should be of low profile to facilitate the suturing of soft
tissue tension _free.
26
2016-08-06
Healing abutment
Dome shaped 2-10 mm
screw placed on the implant
after the 2nd stage surgery
& before insertion of the
prosthesis
A- screw into implant
B- Screw into abutment
(healing cap)
Healing Abutments
Transgingival Titanium piece which
will form the soft tissue
Selected considering the
Emergence Profile needed for the
restoration and the tissue height
27
2016-08-06
EP (Emergence
Profile)
Healing Abutments
Necessary Information:
Height
Healing Abutment Height
Platform Diameter (normally same as implant
diameter )
Restorative
Platform
Healing Abutment Diameter (EP Profile)
Healing Abutments
28
2016-08-06
Abutment
Component of the implant system that
screw directly into the implant to support
and or retains a prosthesis or implant
superstructure
Abutment
(Screw retained restoration)
Can be either parallel or conical in
shape.
are secured with an abutment
screw that is tightened to 20 Ncm.
Abutment
screw
(green)
Abutment
(red)
(Cemented restoration)
Secured with a square head
screw tightened to 32 Ncm.
29
2016-08-06
15 Pre-Angled
Straight
Engages
Implant
Hex
Click Zone
Impression posts
Component used during the impression procedure
to transfer the intra oral location of the implant
or the abutment the laboratory cast
Abutment type
Fixture type
Two piece
(pick-up) type
30
2016-08-06
Two impression techniques
Closed tray impression
Open tray impression
Closed Tray Impression
Remove The Healing Abutment
Place The Impression Coping
31
2016-08-06
Closed Tray Impression
Syringe around the impression
coping to capture the flat sides
Closed Tray Impression
Remove the impression
Remove the impression post from implant
Mount impression post onto the analog (same color)
Reposition and snap back into the impression
Education
32
2016-08-06
Open tray impression Concept
Implant & impression post
Intraoral situation
Analog & impression
post
Education
Impression procedure
Remove closure screw or healing abutment
Insert impression post and hand tighten screw with
the screwdriver
66
Education
33
2016-08-06
Impression procedure
Take impression with an open tray
Use an elastomeric impression material
67
Education
Impression procedure
When impression material is set,
unscrew and remove the impression
68
Education
34
2016-08-06
Pick-Up Technique
Whats it for:
Single or Multiple units
A MUST in single non-parallel implants
Advantages:
More Precise
30 per
implant
Disadvantages:
Vertical Height (pick up coping is long)
Tray needs a hole in it for impression
screw (customized or standard)
Types of impression posts
A one piece coping
Screw into the abutment
used if the abutment does not
need to be changed on the
lab cast
Two piece coping
Screw into the implant
used if the abutment does
not need to be
changed on the lab
cast
Two piece coping
Screw into the abutment
used to orient the antirotational feature or to
make impression of
very divergent implant
35
2016-08-06
Two piece Impression coping
Impression coping attached to the implant analog
Impression with laboratory analog to make the master cast.
The impression posts attached to the
implants fixtures.
The master cast is that one used to fabricate the
final prosthesis.
36
2016-08-06
Laboratory analogs
Components made to represent the top of
the implant fixture or the abutment in the
laboratory cast
Fixture analog
{Duplicate implant top}
Abutment analog
{Duplicate abtument top}
37
2016-08-06
38
2016-08-06
Attach Analog
39
2016-08-06
Push Analog/Impression Coping Assembly into Impression
Twist and Lock Grooves into Impression
40
2016-08-06
Waxing sleeves
Plastic waxing sleeve tightened
to a laboratory analog
Gold cylinder tightened to a
laboratory analog
Combination
Place screw into waxing sleeve and engage onto
the implant analog in the working model.
Adjust waxing sleeve using a lowspeed handpiece
After the wax-up is complete, remove from
model and mark the gingival margin with a black
marker.
When the abutment is placed back on the model,
the black line will indicate the margin in relation
to the soft tissue. Adjust as required, relieve
undercuts and finalize surface smoothness
41
2016-08-06
Prosthesis retaining
screw
Screw used to secure the
prosthesis to the implant
or the transmucosal
abutment
Prosthetic retaining screw
Prosthetic
retaining screw
Have a slot or hex head
Access is usually covered by a combination of gutta percha
and composite.
Used to retain the prosthesis to the abutment.
Tightened to 10 Ncm.
42
2016-08-06
Components of an implant
restoration
Composite resin
Gutta percha
Screw retained implant restorations
Retaining screw
consist of three components.
Abutment screw
(a) Implant fixture
Abutment
(b) Abutment
(c) Restoration
The abutment retaining screw Implant fixture
secures the abutment to the fixture
The prosthetic retaining screw
secures the prosthesis to the abutment.
Screw retained implant crown
43
2016-08-06
Slot Screw Driver
- Used to remove or replace slotted prosthetic
retention screws.
- Tighten to 10 Ncm
Hex Screw Driver
- Used to remove or replace hex prosthetic
retention screws.
- Tighten to 10 Ncm.
Abutment Screw Driver
- Used to remove or replace abutment screws for
standard or conical (estheticone / mirus cone)
abutments.
- Tighten to 20 Ncm.
Square Screw Driver
- Used to remove or replace Cera One
abutment screw.
- Tighten to 32 Ncm
44
2016-08-06
IMPLANT RESTORATIVE
OPTIONS
Distal-extension Implant Restoration.
Distal-extension Implant Restoration.
Long Edentulous Span Restoration.
Single-tooth Implant Restoration.
Fixed Restoration in the Completely
Edentulous Arch.
1. Tooth-implant supported restoration
One implant distal to the most posterior
natural abutment -------------Fixed
prosthesis connecting the implant with
the natural tooth.
2. Implant supported restoration
Two or more implants posterior to the
most distal natural tooth ----------Completely implant-supported restoration.
45
2016-08-06
IMPLANT RESTORATIVE
OPTIONS
Long Edentulous Span Restoration.
Distal-extension Implant Restoration.
Long Edentulous Span Restoration.
Single-tooth Implant Restoration.
Fixed Restoration in the Completely
Edentulous Arch.
1. Multiple implants placed between the
remaining natural teeth to fabricate a
fully implant-supported restoration.
2. One or two implants can be placed in the
long edentulous span and the final
restoration connected to natural teeth.
When it is necessary to connect implants and the
natural teeth, protecting the teeth with
telescopic copings is recommended .
In this manner, prosthesis retrievability can be
maintained.
Some long edentulous spans require the reconstruction
of soft and hard tissue and teeth. using resin
teeth processed to a metal substructure rather
than a conventional metal-ceramic restoration is
recommended.
Soft tissue esthetics can be more easily and
accurately mimicked with heat-processed resin .
This type of restoration has been called a hybrid
because it combines the principles of conventional
fixed and removable prosthodontics.
IMPLANT RESTORATIVE OPTIONS
Single-tooth Implant Restoration.
Distal-extension Implant Restoration.
Long Edentulous Span Restoration.
Single-tooth Implant Restoration.
Fixed Restoration in the Completely
Edentulous Arch.
Indicated in the following situations:
1. An otherwise intact dentition
2. spaces difficult to treat with conventional fixed
prosthodontics
3. Distally missing teeth.
4. A prosthesis that needs to closely mimic the missing
natural tooth
The requirements for single-tooth implant crowns are:
1. Esthetics
2. Ant rotation to avoid prosthetic component
loosening
3. Simplicity-to minimize the amount of components
used
4. Accessibility-to maintain optimum oral health
5. Variability-to allow the clinician to control the
height, diameter, and angulations of the implant
restoration
46
2016-08-06
Distal-extension Implant Restoration.
Long Edentulous Span Restoration.
Single-tooth Implant Restoration.
Fixed Restoration in the Completely
Edentulous Arch.
IMPLANT RESTORATIVE
OPTIONS
Distal-extension Implant Restoration.
Long Edentulous Span Restoration.
Single-tooth Implant Restoration.
Fixed Restoration in the Completely
Edentulous Arch.
Fixed Restoration in the Completely
Edentulous Arch.
1.The hybrid prosthesis is a cast alloy
framework with processed denture resin and
teeth.
Five implants in the mandible and six in the maxilla.
Suitable for patients who have had moderate
bone loss, the prosthesis restores both bone
and soft tissue contours.
2. The metal-ceramic rehabilitation also
requires five implants in the mandible and six in
the maxilla. Only if minimal bone loss has
occurred and is best suited for patients who
have recently lost their natural teeth (within 5
years).
3. For patients with severe bone loss, there is
Minimal resorption
probably only one option: a removable
Metal ceramic
restoration .
restorations
Moderate
resorptionresin to
metal restorations
sever resorption
Over denture
47
2016-08-06
CEMENT-RETAINED VERSUS SCREWRETAINED IMPLANT CROWNS
Zinc phosphate, glass ionomer, and composite resin
cements have all been suggested for this purpose.
Advantages of cement-retained restorations.
1. Simplicity
2. Less expensive.
3. Allow minor angle correction.
4. More esthetically pleasant
Disadvantages of cement-retained restorations.
1. Require more chair time
2. Have the same propensity to loosen as the
screw retained.
Advantages of screw-retained restorations.
1. Retrievability
Disadvantage of a screw-retained implant
restoration
1. The screw may loosen during function.
2. Cost
CEMENT-RETAINED VERSUS SCREWRETAINED IMPLANT CROWNS
If the screw is sufficiently tightened into
the implant crown to seat it, a clamping load
or preload is developed between the implant
and the crown.
If this clamping force is greater than the
forces trying to separate the joint between
implant and crown, the screw will not loosen.
48
2016-08-06
Screw-Retained Crowns
Screw Retained Transversal
Screw Retained Transocclusal
49
2016-08-06
Cemented Restoration
50
Você também pode gostar
- DR Ghazy 2012 MY IMPLANT LECTURE For 4th Year StudentsDocumento25 páginasDR Ghazy 2012 MY IMPLANT LECTURE For 4th Year StudentsMohamed Hamed GhazyAinda não há avaliações
- DR Ghazy 2013 Implant Lectures For 4th Year StudentsDocumento25 páginasDR Ghazy 2013 Implant Lectures For 4th Year StudentsMohamed Hamed GhazyAinda não há avaliações
- Implant PPT Phase 2 Aseptico ImplantDocumento63 páginasImplant PPT Phase 2 Aseptico Implantapi-152953067Ainda não há avaliações
- IMPLANTOLOGI Compressed Compressed (1) - MinDocumento122 páginasIMPLANTOLOGI Compressed Compressed (1) - MinNayafilahAinda não há avaliações
- Introduction To Dental Implants 2017 PDFDocumento61 páginasIntroduction To Dental Implants 2017 PDFChong Weng Wah100% (2)
- Dental Implant Treatment Planning for New Dentists Starting Implant TherapyNo EverandDental Implant Treatment Planning for New Dentists Starting Implant TherapyNota: 4 de 5 estrelas4/5 (1)
- Catalogue SmallDocumento78 páginasCatalogue SmallAyad Taha100% (1)
- Tuberopterygoid ImplantsDocumento7 páginasTuberopterygoid ImplantsThe SinusLift100% (1)
- Implant Guidelines For The Restorative DentistDocumento165 páginasImplant Guidelines For The Restorative DentistRajab Lil'ronaldo67% (3)
- Dental Implant: Presented byDocumento43 páginasDental Implant: Presented byade ismailAinda não há avaliações
- Ce 420Documento24 páginasCe 420Tupicica GabrielAinda não há avaliações
- EJMCM - Volume 7 - Issue 4 - Pages 1689-1693Documento5 páginasEJMCM - Volume 7 - Issue 4 - Pages 1689-1693Tanushree JainAinda não há avaliações
- Implant Prosthodontics in Complete Edentulous Cases I. Fixed and Removable Prosthodontics QR NelkulDocumento33 páginasImplant Prosthodontics in Complete Edentulous Cases I. Fixed and Removable Prosthodontics QR NelkulЮля КолмаковаAinda não há avaliações
- Dental Implants - Classification, Success and Failure - An OverviewDocumento8 páginasDental Implants - Classification, Success and Failure - An OverviewIOSRjournalAinda não há avaliações
- 1 Overview of ImplantologyDocumento187 páginas1 Overview of ImplantologyTom DienyaAinda não há avaliações
- Endosteal Screw Dental ImplantDocumento5 páginasEndosteal Screw Dental ImplantHUSNAIN ALIAinda não há avaliações
- Treatment Planning Single Maxillary Anterior Implants for DentistsNo EverandTreatment Planning Single Maxillary Anterior Implants for DentistsAinda não há avaliações
- Dental ImplantsDocumento30 páginasDental ImplantsИскен АдылбековAinda não há avaliações
- Implant DentistryDocumento196 páginasImplant DentistryAkanksha MahajanAinda não há avaliações
- 200810110-112 Innova ArticleDocumento2 páginas200810110-112 Innova ArticleMery MerryAinda não há avaliações
- Implant Prosthodontics ParameterDocumento4 páginasImplant Prosthodontics ParameterSorabh JainAinda não há avaliações
- QSD Tapered Implant Manual Art939BDocumento24 páginasQSD Tapered Implant Manual Art939BkhashmiraAinda não há avaliações
- 3i IMPLANTOLOGIADocumento75 páginas3i IMPLANTOLOGIASilke JahnsenAinda não há avaliações
- Poster DisplayDocumento2 páginasPoster Displayscribd710Ainda não há avaliações
- Short ImplantsNo EverandShort ImplantsBoyd J. TomasettiAinda não há avaliações
- Eview: Mini Dental Implants-The Same Day ImplantsDocumento6 páginasEview: Mini Dental Implants-The Same Day ImplantsShaiilly LuthraAinda não há avaliações
- Denture ConversionDocumento11 páginasDenture Conversionaastha dogra100% (1)
- 10867-0 Neoss Anatomical Healing Abutment Manual Hi Res 2009-05-19Documento4 páginas10867-0 Neoss Anatomical Healing Abutment Manual Hi Res 2009-05-19Nate TaylorAinda não há avaliações
- ImplantDocumento9 páginasImplantKhaled Abo ZaidAinda não há avaliações
- Over DentureDocumento19 páginasOver DentureMohammed HassanAinda não há avaliações
- What Is Dental ImplantDocumento14 páginasWhat Is Dental ImplantFaleh ZahrawiAinda não há avaliações
- Immediate Implant Placement in MaxillarDocumento7 páginasImmediate Implant Placement in MaxillarrtyAinda não há avaliações
- Maxillary Anterior Implant PlacementDocumento77 páginasMaxillary Anterior Implant PlacementBasel AlogilyAinda não há avaliações
- Review of Dental ImplantDocumento10 páginasReview of Dental Implantmar100% (1)
- Os SEO IntegrationDocumento7 páginasOs SEO IntegrationAkshay GajakoshAinda não há avaliações
- Marburg Double Crown System For Partial DentureDocumento10 páginasMarburg Double Crown System For Partial DentureAhmad Shoeib100% (1)
- Swing Lock Partial Denture SOWMYADocumento22 páginasSwing Lock Partial Denture SOWMYASanAinda não há avaliações
- The Impact of The Flexible Partial Denture Base On The Alveolar Mucosa in Comparison To Metallic Denture RCT and Histological StudyDocumento7 páginasThe Impact of The Flexible Partial Denture Base On The Alveolar Mucosa in Comparison To Metallic Denture RCT and Histological StudyZachary DuongAinda não há avaliações
- Immediate Implant Placement: Clinical Decisions, Advantages, and DisadvantagesDocumento6 páginasImmediate Implant Placement: Clinical Decisions, Advantages, and DisadvantagesAmaey ParekhAinda não há avaliações
- Immediate Dental ImplantsDocumento13 páginasImmediate Dental ImplantsDevanyNataniaAinda não há avaliações
- Dental Implant DissertationDocumento6 páginasDental Implant DissertationHelpMeWriteAPaperUK100% (1)
- 3i CatalogDocumento79 páginas3i CatalogJulie HollowayAinda não há avaliações
- Prosthetic Aspects of Dental Implants - IIDocumento73 páginasProsthetic Aspects of Dental Implants - IIKomal TalrejaAinda não há avaliações
- Provisional Restoration Options in Implant DentistryDocumento8 páginasProvisional Restoration Options in Implant Dentistrydevendra chhonkarAinda não há avaliações
- Esthetic Oral Rehabilitation with Veneers: A Guide to Treatment Preparation and Clinical ConceptsNo EverandEsthetic Oral Rehabilitation with Veneers: A Guide to Treatment Preparation and Clinical ConceptsRichard D. TrushkowskyAinda não há avaliações
- Chapter 19Documento33 páginasChapter 19Komal TalrejaAinda não há avaliações
- Swing Lock Partial DentureDocumento22 páginasSwing Lock Partial DentureSanAinda não há avaliações
- Immediate DenturesDocumento35 páginasImmediate DenturesPrince AhmedAinda não há avaliações
- KararyDocumento39 páginasKararyوليد خالدAinda não há avaliações
- Oral Implantology: ImplantsDocumento52 páginasOral Implantology: ImplantsDabala Harish Reddy100% (6)
- A Clinical Pathway For Complete Immediate Denture TherapyDocumento18 páginasA Clinical Pathway For Complete Immediate Denture TherapyPragya PandeyAinda não há avaliações
- Fred'S Facts: The Implant Supported OverdentureDocumento4 páginasFred'S Facts: The Implant Supported OverdentureDr. GustaveAinda não há avaliações
- Peri-Implant Bone Loss Around Platform-Switched Morse Taper Connection Implants: A Prospective 60-Month Follow-Up StudyDocumento9 páginasPeri-Implant Bone Loss Around Platform-Switched Morse Taper Connection Implants: A Prospective 60-Month Follow-Up StudyMarco TeixeiraAinda não há avaliações
- Oral ImplantologyDocumento19 páginasOral ImplantologyKariim AhmadAinda não há avaliações
- James J. Sciubba, DMD, PHD: Dental Implants and The Dry Mouth PatientDocumento3 páginasJames J. Sciubba, DMD, PHD: Dental Implants and The Dry Mouth Patientleandrolc01Ainda não há avaliações
- Assignment Implant WelaDocumento3 páginasAssignment Implant WelaWela BaayouAinda não há avaliações
- Extraction of A Maxillary Molar Tooth-Simplified (A Case Report)Documento5 páginasExtraction of A Maxillary Molar Tooth-Simplified (A Case Report)Farizah Aryanti JooAinda não há avaliações
- Treatment Planning of ImplantsDocumento10 páginasTreatment Planning of ImplantsRussia Al ShboulAinda não há avaliações
- The New Alternative To Conventional Dentures-All On 4 Dental Implant Treatment Concept: A Review ArticleDocumento12 páginasThe New Alternative To Conventional Dentures-All On 4 Dental Implant Treatment Concept: A Review Articlesurbhisumanmds2025Ainda não há avaliações
- 2017 DR Ghazy Delta Level 4 Lecture 2 Partial Coverage Restorations 2Documento61 páginas2017 DR Ghazy Delta Level 4 Lecture 2 Partial Coverage Restorations 2Mohamed Hamed GhazyAinda não há avaliações
- Sterilization and DisinfectionDocumento29 páginasSterilization and DisinfectionMohamed Hamed GhazyAinda não há avaliações
- 2017 DR Ghazy DELTA LEVEL4 LECTURE 1 Partial Coverage Crown Preparation PDFDocumento21 páginas2017 DR Ghazy DELTA LEVEL4 LECTURE 1 Partial Coverage Crown Preparation PDFMohamed Hamed GhazyAinda não há avaliações
- IFDEA Dental Anatomy Educational Teaching ResourceDocumento38 páginasIFDEA Dental Anatomy Educational Teaching ResourceaerowongAinda não há avaliações
- Handpieces 320-341Documento22 páginasHandpieces 320-341Mohamed Hamed GhazyAinda não há avaliações
- DR Ghazy 2013 - 2014 Fixed Prosthodontics IntroductionDocumento21 páginasDR Ghazy 2013 - 2014 Fixed Prosthodontics IntroductionMohamed Hamed GhazyAinda não há avaliações
- 2013 2014 Color and Shade SelectionDocumento107 páginas2013 2014 Color and Shade SelectionMohamed Hamed GhazyAinda não há avaliações
- DR Ghazy 2013 - 2014 Fixed Prosthodontics IntroductionDocumento21 páginasDR Ghazy 2013 - 2014 Fixed Prosthodontics IntroductionMohamed Hamed GhazyAinda não há avaliações
- MY NEW CV CompleteDocumento8 páginasMY NEW CV CompleteMohamed Hamed GhazyAinda não há avaliações