Escolar Documentos
Profissional Documentos
Cultura Documentos
Diagnostic Approach To Hypercoagulable States: Bratislavske Lekarske Listy February 2006
Enviado por
envadDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Diagnostic Approach To Hypercoagulable States: Bratislavske Lekarske Listy February 2006
Enviado por
envadDireitos autorais:
Formatos disponíveis
See
discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/6673289
Diagnostic approach to hypercoagulable states
Article in Bratislavske lekarske listy February 2006
Impact Factor: 0.44 Source: PubMed
CITATIONS
READS
77
1 author:
Anna Remkov
Slovak Medical University in Bratislava
62 PUBLICATIONS 291 CITATIONS
SEE PROFILE
All in-text references underlined in blue are linked to publications on ResearchGate,
letting you access and read them immediately.
Available from: Anna Remkov
Retrieved on: 14 July 2016
292
Bratisl Lek Listy 2006; 107 (8): 292 295
TOPICAL REVIEW
Diagnostic approach to hypercoagulable states
Remkova A
1st Department of Internal Medicine, Faculty of Medicine, Comenius University, Bratislava,
Slovakia. anna.remkova@fmed.uniba.sk
Abstract
The primary hypercoagulable states are inherited thrombotic disorders, resulting from mutations in
genes encoding a plasma protein component of one of the coagulation mechanisms. The anticoagulant
pathways most frequently involved include antithrombin III, protein C, and protein S deficiencies and
activated protein C (APC) resistance. Around 80 % of all individuals with APC resistance carry a
mutation of the factor V gene. Abnormalities in procoagulant pathways mostly concern elevated levels
and/or function of procoagulant factors. Elevation in plasma prothrombin (FII) levels is associated with
a FII gene mutation. Hyperhomocysteinemia as a risk factor for thrombosis is determined by genetic
or dietary factors. The acquired or secondary hypercoagulable states consist of a heterogeneous group
of disorders with an increased risk for developing thrombosis. Many underlying conditions (e.g., malignancies) may induce changes in the coagulation system. The risk of thrombosis is increased in individuals with antiphospholipid antibodies. They are found in about one-half of patients with systemic
lupus erythematosus, but also in the course of infections, neoplastic diseases, and sometimes in apparently normal subjects. A definite molecular abnormality of hypercoagulable states can be identified in
the special coagulation laboratory, using two types of molecular risk factors for thrombosis (genetic
factors and abnormal laboratory phenotypes). Its recognition is useful for a prevention and/or therapy
of thrombosis (Tab. 4, Ref. 10).
Key words: coagulation factors, hypercoagulation, thrombophilia, thrombosis, antiphospholipid syndrome.
The pathogenesis of venous and arterial thrombosis is complex and multifactorial. Virchow (1865) identified three risk factors of thrombosis: damage to the vessel wall, reduction in the
blood flow and alterations in the blood components. The interactions between these factors play role in the activation of hemostatic system and thrombus formation.
The function of hemostatic system depends on complex reactions among its components: the platelets, vessel wall, coagulation factors with their inhibitors, and the fibrinolytic proteins
with their inhibitors. Disturbance in the balance between coagulation and fibrinolysis is prone to thrombosis. Patients with a
propensity to develop thrombosis are frequently labeled as having a hypercoagulable or prethrombotic state. In humans,
several of the conditions that predispose to thrombosis involve
the hypercoagulable states. Hypercoagulable state is a disorder
of the blood coagulation, with a shift of the hemostatic balance
towards the enhancement of procoagulant forces. When the hypercoagulability surpasses a certain threshold, thrombus formation will occur (1 6).
The body possesses natural antithrombotic protective mechanisms to counteract the initial thrombotic processes. One of them
is inactivation of the coagulation esterases by physiologic inhibitors such as antithrombin III, protein C, and protein S. Individuals with reduced activities of these inhibitors have a propensity for developing thrombosis. Disorders of these homeostatic
mechanisms can lead to an imbalance of coagulation (prothrombotic) over anticoagulation (antithrombotic) activities.
In some of the hypercoagulable patients, a definite molecular abnormality can be identified in the coagulation laboratory.
1st Department of Internal Medicine, Faculty of Medicine, Comenius
University, Bratislava, Slovakia
Address for correspondence: A. Remkova, MD, PhD, DSc, 1st Dept
of Internal Medicine, Faculty of Medicine, Comenius University,
Mickiewiczova 13, SK-813 69 Bratislava 1, Slovakia.
Phone: +421.2.57290249
Acknowledgement. This work was supported by Slovak Ministry of
Education grant VEGA No 1/2290/05.
Remkova A. Diagnostic approach to hypercoagulable states
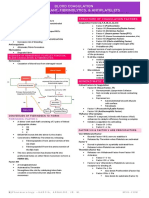
Tab. 1. Classification of hypercoagulable states.
Inherited (Primary) Hypercoagulable States
Antithrombin III deficiency
Protein C deficiency
Protein S deficiency
Activated protein C resistance due to factor V gene mutation
Prothrombin gene mutation
Dysfibrinogenemia (rare)
Acquired (Secondary) Hypercoagulable States
Antiphospholipide syndrome
In association with physiologic or other thrombogenic stimuli
(e.g., pregnancy and the post-partum period, estrogen use, advancing age, immobilization, injury, postoperative state etc.)
In association with some clinical disorders (e.g., malignancy,
nephrotic syndrome, congestive heart failure etc.)
Mixed Hypercoagulation States
Hyperhomocysteinemia
Disorders of these homeostatic mechanisms can lead to an imbalance of coagulation (prothrombotic) over anticoagulation
(antithrombotic) activities (14).
Multiple genetic and environmental factors contribute to the
development of thrombosis. According to this concept, thrombosis is either a congenital disorder of the natural anticoagulant
pathways or an acquired disorder, which triggers the mechanism
of coagulation and/or reduces the natural anticoagulant activity
(Tab. 1). Two types of molecular risk factors for thrombosis can
be recognized: genetic factors and abnormal laboratory phenotypes (4).
Primary hypercoagulable states
The primary hypercoagulable states are inherited thrombotic
disorders, resulting from mutations in genes encoding a plasma
protein component of one of the coagulation mechanisms (3).
The term of inherited thrombophilia is applied to individuals with
atendency to thrombosis due to predisposing genetic defects.
The inherited thrombotic disorders are almost exclusively asso-
293
ciated with venous thrombosis. It is currently possible to define
several genetic risk factors. The anticoagulant pathways most
frequently involved include antithrombin III (AT), protein C (PC),
and protein S (PS) deficiencies and activated PC (APC) resistance. APC-resistance is a defect in the protein C anticoagulant
pathway, resulting in the poor anticoagulant response of plasma
to activated protein C. Around 80 % of all individuals with APCresistance carry a mutation of the factor V gene (factor V Leiden).
Factor V (FV) Leiden is due to replacement of arginine-506 to
glutamine-506 (Arg506Gln) in one of the cleavage sites for APC.
The mutation in the gene of FV delays inactivation of the activated FV. Abnormalities in procoagulant pathways, which result
in enhanced fibrin formation, mostly will concern elevated levels and /or function of procoagulant factors. These can be genetically determined or be the result of an interaction with the
environment. Elevated levels of factor II, factor VIII, and fibrinogen are associated with an increased risk of thrombosis. Elevation in plasma prothrombin (FII) levels is associated with a FII
gene mutation, due to a G A transition in nucleotide 20210 in
the 3' untranslated region. Hyperhomocysteinemia, as a common
risk factor for both venous and arterial thrombosis, is determined
by genetic as well as by dietary factors. A common genetic cause
is the variant of the methylene tetrahydrofolate reductase
(MTHFR) gene that leads to a thermolabile variant of the enzyme and mildly elevated homocysteine levels. Genetic risk factors for thrombosis comprise all gene mutations that results in a
loss or gain function of the encoded protein. Loss of function is
responsible for hereditary deficiencies, like AT, PC, and PS deficiency. Such mutations prevent the synthesis of a normal protein
(type I deficiency) or result in the synthesis of an abnormal, functionally defective protein (type II deficiency). Laboratory diagnosis relies on the measurement of protein concentrations and/
or function in plasma. Mutations that result in a gain of function
include FV Leiden and FII gene mutation. DNA analysis seems
to be the method of choice for the determination of these molecular risk markers (4).
Examples of abnormal laboratory phenotypes as risk factors
for thrombosis include APC-resistance, mild hyperhomocystei-
Tab. 2. Differential diagnosis of hypercoagulable states.
Clinical characteristics
Laboratory tests
Personal history of proven venous thromboembolism
The hemostatic profile of AT, PC, PS, FV Leiden and FII gene mutation
should be investigated. The measurement of antiphospholipid antibodies
should also be performed.
Age at the first thromboembolic episode
A first episode before 40 45 years of age is frequent in patients with AT, PC,
PS deficiency. A first episode at an older age (over 60 years) without any
systemic disease (e.g. cancer) may be associated with FV Leiden.
Recurrence of thromboembolic episodes
In about 50 % of patients with thrombophilia due to AT, PC, PS deficiency.
Family history of venous thromboembolism
The hemostatic profile of AT, PC, PS, FV Leiden and FII gene mutation
should be investigated.
Personal or family history of fetal loss
In AT deficiency and in combined congenital coagulation abnormalities as
well as in FV Leiden. An antiphospholipid syndrome should be suspected in
subject with recurrent fetal loss.
294
Bratisl Lek Listy 2006; 107 (8): 292 295
Tab. 3. Screening laboratory evaluation for hypercoagulable states.
Clotting assay for resistance to activated protein C
Genetic test for factor V Leiden
Genetic test for prothrombin gene mutation (G20210A)
Functional assay of antithrombin III
Functional assay of protein C
Functional assay of protein S
Immunological assays of total and free protein S. Screen for dysfibrinogenemias (immunologic and functional assays of fibrinogen,
thrombin time)
Measurement of total plasma homocysteine
Clotting assay for lupus anticoagulant
Serologic tests for antiphospholipid antibodies
nemia, and elevated factor VIII levels. The molecular basis for
some of these plasma phenotypes is incompletely known.
While hereditary deficiencies of AT, PC, or PS will be found
in fewer than 5 % of unselected patients presenting with venous
thromboembolism, the likelihood of identifying these defects is
increased several-fold by screening patients with the initial thrombosis occurring prior to age of 50 years, a family history of venous
thromboembolism, and recurrent venous thrombosis. FV Leiden,
FII gene mutation (FII G20210A), and hyperhomocysteinemia
are more prevalent defects, and can be found in significant numbers of patients with first episodes of idiopathic venous thrombosis (i.e., no apparent precipitating factor) after age 50 years in
the absence of a positive family history. Thrombotic episodes
can be triggered by various stimuli (e.g., pregnancy, estrogen
use, surgery) in perhaps 50 % of individuals with hereditary defects (6 9). Selection of patients for the laboratory investigation
of molecular risk markers is indicated in Table 2.
A diagnostic approach to patients suspected of having a biologic defect predisposing to thrombosis is based on screening
laboratory evaluation (Tab. 3).
The laboratory evaluation for a natural anticoagulant deficiency is performed by functional and immunological assays.
Functional tests are based either on amidolytic or clotting methods. They are the best screening tests for deficiencies of AT, PC,
and PS because they can detect both quantitative and qualitative
defects. Immunologic (antigenic) assays detect only quantitative
deficiencies of these proteins. They are recquired when functional tests are abnormal for classification in types I (quantitative) or type II (qualitative) deficiencies. The FV Leiden and FII
gene mutation can be performed by DNA analysis. Coagulation
assays for the FV Leiden mutation are based on the resistance of
the activated mutant FV molecule to inactivation by APC. To
screen for a dysfibrinogenemia, the thrombin time is recommended along with measurements of plasma fibrinogen by clotting and immunologic assay. Testing for hyperhomocysteinemia
should be done after an overnight fast and on normal diet.
For the laboratory diagnosis of primary hypercoagulable states
careful interpretation of the results aims toward the exclusion of
disseminated intravascular coagulation (DIC), or elimination of
another acquired hypercoagulable state or acquired natural anticoagulants deficiencies. The existence of underlying conditions
that influence normal hemostasis (such as pregnancy, oral contraception, hormonal replacement therapy, cancer, chemotherapy, liver
disease, oral anticoagulation should be taken in consideration.
Secondary hypercoagulable states
The acquired or secondary hypercoagulable states consist of
a heterogenous group of disorders with an increased risk for developing thrombotic complications (2, 5, 6). Hyperhomocysteinemia is a common abnormality that results in an increased risk
of venous as well as arterial thrombosis. Plasma homocysteine
levels are determined by genetic as well as by environmental
factors, the latter including dietary intake and absorption of folic
acid and vitamins B12 and B6. Many underlying conditions (e.g.,
malignancies) may induce changes in the coagulation system and
lead to a hypercoagulable state. Cancer cells may have direct
procoagulant effects by the production of tissue factor and of
cancer procoagulant. Certain acquired conditions (e.g., elevated
factor VIII levels, lupus anticoagulant, pregnancy, oral contraceptive use) could result in the laboratory phenotype of APCresistance. This type of APC-resistance is not associated with
FV Leiden. It seems to be also a risk factor for thrombosis, although less strong. The origin and molecular basis of APC-resistance in the absence of FV Leiden is not well known and is
likely to be of mixed genetic and acquired origin.
The risk of thrombosis is increased in individuals with antiphospholipid antibodies (APA). This abnormal plasma phenotype is found in about one-half of patients with systemic lupus
erythematosus, but also in the course of infections, neoplastic
diseases, administration of certain drugs, and sometimes in apparently normal subjects (10). The APA are directed against a variety
of phospholipid (PL) binding-proteins of which 2-glycoprotein I
(2GPI) is considered to be the major antigen. Some of these antibodies prolong PL-dependent clotting reactions and are termed
lupus anticoagulants (LA). Autoimmune APA which are bound
through 2GPI to cardiolipin are called anticardiolipin antibodies
(ACA). The origin of APA is unknown. Some arise as a response
to infections, other may occur as a result of cellular injury or
apoptosis. Among patients with venous thrombosis, a LA has been
reported in 5 % to 15 %. It can lead to a nine-fold increased risk of
thrombosis. It seems that LA is a stronger risk factor for thrombosis than ACA. The thrombosis recurrence rate in patients with APA
is exceedingly high. Thrombogenic mechanisms remain unclear.
More than one mechanism seems likely since APA are associated
with such a wide spectrum of venous, arterial and microvascular
thromboses. Antiphospholipid syndrome (APS) is an autoimmune
disorder, defined as the association of APA with arterial or venous
thrombosis, recurrent fetal loss or thrombocytopenia (10) (Tab.
4). Pregnancy loss is most likely a result of disruption of placental
blood flow due to vascular thrombosis. About 515 % of women
with recurrent pregnancy loss are found to have evidence of APA.
The APA are clearly linked to myocardial infarction and thrombotic or embolic stroke, particularly in young people.
Two general types of assays are used to identify APA in clinical practice (10). Enzyme-linked immunosorbent assays (ELISA)
Remkova A. Diagnostic approach to hypercoagulable states
Tab. 4. Classification criteria for the antiphospholipid syndrome.
Antiphospholipid syndrome (APS) is established if at least one clinical
and one laboratory criterion is present. Persistent positivity of laboratory tests is important.
Clinical criteria
1. Vascular thrombosis
One or more clinical episodes of arterial, venous, or small vessel
thrombosis, in any tissue or organ.
2. Pregnancy morbidity
One or more unexplained deaths of a morphologically normal fetus, or premature births of a morphologically normal neonate because of eclampsia or severe preeclampsia, or recognized features
of placental insufficiency, or three or more unexplained consecutive spontaneous abortions.
Laboratory criteria
1. Lupus anticoagulant in plasma, on 2 or more occasions at least 12
weeks apart.
2. Anti-cardiolipin antibody IgG and/or IgM in serum or plasma,
present in medium or high titer, on 2 or more occasions, at least 12
weeks apart, measured by a standardized ELISA.
3. Anti-2 glycoprotein-I antibody IgG and/or IgM in serum or plasma,
present on 2 or more occasions, at least 12 weeks apart, measured
by a standardized ELISA.
are used for APA against specific proteins: ACA and anti-2-GPI
antibodies. Lupus anticoagulants (LA) are detected by using coagulation tests. LA are heterogeneous and their reactivity depends on the nature of the assay, the origin and amount of PL in
the coagulation reagents, and their target antigens. More than
one test must be used, because a single test will identify only
60 70 % of patients with lupus inhibitors. Both activated partial
thromboplastin time (APTT)-based assays and dilute Russells
viper venom time (dRVVT) is suitable for LA determination.
Molecular markers of coagulation activation in assessment
of prethrombotic state
Increased plasma levels of coagulation activation markers
indicate an activation of the coagulation system that is also termed
as hypercoagulable state. Under certain conditions, this may
be a prodromal state of thrombosis. Activation of the coagulation system may take place locally at a site of vascular injury, or
systemically, within the entire blood volume. Systemic coagulation activation can be triggered by a variety of mechanisms, leading to the DIC syndrome.
Certain assays reflect the coagulation reactions leading to a
formation of fibrin thrombus. Such tests can reflect the generation of thrombin, which is responsible for the transformation of
fibrinogen into fibrin. During the process of prothrombin to
thrombin activation, measurable prothrombin fragments 1+2
(F1+2) are released. The thrombin-antithrombin (TAT) complexes
measure the interaction between thrombin and its inhibitor. Other
tests reflect the action of thrombin on fibrinogen with fibrin formation. After the release of fibrinopeptides A (FPA) from fibrinogen, the resulting fibrin monomer molecules display an in-
295
tense tendency to polymerize. Soluble fibrin detected in plasma
samples includes a variety of complexes consisting mainly of
fibrin monomer units. The advantage of measuring soluble fibrin over FPA is the considerably longer half-life of soluble fibrin in the circulation. It can be detected by a variety of methods, including paracoagulation and precipitation assays. Finally,
some tests reflect the action of plasmin on fibrinogen and fibrin.
Perhaps the best known of these tests involve fibrinogen/fibrin
degradation products. Tests that are more specific for fibrin digestion may have more potential when evaluating patients with
thrombosis. Markers of this category include the D-dimer, which
is digestion product of cross-linked fibrin. D-dimer is a marker
of fibrin turnover. Plasma measurements of D-dimer are used
routinely in diagnosis of DIC and of venous thromboembolism.
Increased fibrin turnover represents a prothrombotic state, which
might favor not only thrombogenesis but also atherogenesis.
Plasma fibrinogen is a strong and consistent predictor of clinical
ischemic events, most of which are caused by arterial thrombosis.
In general, recognition of hypercoagulable state and coagulation activation using special laboratory methods is useful information for a targeted prevention and /or therapy of thrombosis and thromboembolic complications.
References
1. Bauer KA, Goodnight SH, Ridker PM. Hypercoagulable states translation of risk factors to clinical practice. 255273. In: McArthur
JR (Ed). Hematology. Washington, Amer Soc Hematol, 1998.
2. Ens GE. Disorders leading to thrombosis. 675-681. In: Stiene-Martin EA, Lotspeich-Steininger ChA, Koepke JA (Eds). Clinical Hematology: principles, procedures, correlations. Philadelphia, Lippincott-Raven Publishers, 1998.
3. Mannucci PM. Laboratory detection of inherited thrombophilia: a
historical perspective. Semin Thromb Hemost 2005; 31 (1): 510.
4. Favaloro EJ. Diagnostic issues in thrombophilia: a laboratory scientists view. Semin Thromb Hemost 2005; 31 (1): 1116.
5. Johnson CM, Mureebe L, Silver D. Hypercoagulable states: a review. Vasc Endovascular Surg 2005; 39 (2): 123133.
6. Remkov A. Trombofiln stavy ako rizikov faktor trombz. Intern
Med 2004; 4 (3): 183185.
7. Remkov A, Androv A, Bulas J, Kiov S. Intrakardilna trombza pri zpalovom ochoren reva komplikovanom sepsou. Intern Med
2002; 2 (2): 113115.
8. Remkov A, Reptov A, Holom K, imko J. Trombza jugulrnych l ako komplikcia gravidity po umelom oplodnen. Intern Med
2003; 3 (78): 458460.
9. Remkov A. Trombza aprotrombotick stavy vgynekolgii
aprodnctve 1. as: Rizikov stavy vzniku trombz vgynekolgii
aprodnctve. Intern Med 2005; 5 (10): 529533.
10. Miyakis S, Lockshin MD, Atsumi T et al. International consensus
statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost 2006; 4 (2): 295306.
Received June 14, 2006.
Accepted June 29, 2006.
Você também pode gostar
- Hiperkoagulable StateDocumento4 páginasHiperkoagulable StateNurul NingrumAinda não há avaliações
- Immune Hematology: Diagnosis and Management of Autoimmune CytopeniasNo EverandImmune Hematology: Diagnosis and Management of Autoimmune CytopeniasJenny M. DespotovicAinda não há avaliações
- Inherited Thrombophilias: Michiel Coppens, MD, Stef P. Kaandorp, MD, Saskia Middeldorp, MD, PHDDocumento18 páginasInherited Thrombophilias: Michiel Coppens, MD, Stef P. Kaandorp, MD, Saskia Middeldorp, MD, PHDLuis Carlos Murillo ValenciaAinda não há avaliações
- Disorders Leading To ThrombosisDocumento27 páginasDisorders Leading To ThrombosisFearless AngelAinda não há avaliações
- Ruiz-Iraztorza Et Al (2010) - Antiphospholipid SyndromeDocumento13 páginasRuiz-Iraztorza Et Al (2010) - Antiphospholipid SyndromextraqrkyAinda não há avaliações
- Jadaon - 2011 - Epidemiology of Activated Protein C Resistance and Factor V Leiden Mutation in The Mediterranean RegionDocumento11 páginasJadaon - 2011 - Epidemiology of Activated Protein C Resistance and Factor V Leiden Mutation in The Mediterranean RegionnadaAinda não há avaliações
- APS pdf2Documento6 páginasAPS pdf2Dr Edi HidayatAinda não há avaliações
- Acquired Thrombophilic Syndromes: Daniela Matei, Benjamin Brenner, Victor J. MarderDocumento18 páginasAcquired Thrombophilic Syndromes: Daniela Matei, Benjamin Brenner, Victor J. MarderRahmat SuhitaAinda não há avaliações
- Antiphospholipid Antibody Syndrome and PregnancyDocumento7 páginasAntiphospholipid Antibody Syndrome and PregnancystepepsAinda não há avaliações
- Defectos Del Sist FibrinoliticoDocumento12 páginasDefectos Del Sist FibrinoliticoJACKPGALINDOAinda não há avaliações
- Hema 2 5th Ed SummaryDocumento9 páginasHema 2 5th Ed Summarymonzon.mika1801Ainda não há avaliações
- Acute Thrombotic Disorders: Joanne G. Kuntz MD, Justin D. Cheesman MD, Robert D. Powers MD, MPHDocumento8 páginasAcute Thrombotic Disorders: Joanne G. Kuntz MD, Justin D. Cheesman MD, Robert D. Powers MD, MPHd40sithuiAinda não há avaliações
- Miyata 2006Documento7 páginasMiyata 2006Mestre O ToloAinda não há avaliações
- Aplastic AnemiaDocumento29 páginasAplastic AnemiaGurkamal SinghAinda não há avaliações
- Aplastic Anemia - Pathogenesis, Clinical Manifestations, and Diagnosis - UpToDate PDFDocumento21 páginasAplastic Anemia - Pathogenesis, Clinical Manifestations, and Diagnosis - UpToDate PDFWahyu Dwi NugrohoAinda não há avaliações
- Tep 1Documento16 páginasTep 1Yarlin MontoyaAinda não há avaliações
- Mecanisme Thrombofilie ScurtDocumento3 páginasMecanisme Thrombofilie ScurtGeorgiana BaciuAinda não há avaliações
- Antiphospholipid Thrombosis Syndrome HematoFeb2008, Vol. 22Documento173 páginasAntiphospholipid Thrombosis Syndrome HematoFeb2008, Vol. 22aazizkhanAinda não há avaliações
- Assignment 1 Pathology Aplastic Anemia: Supervisor: DR - Ramez Al-KeelaniDocumento6 páginasAssignment 1 Pathology Aplastic Anemia: Supervisor: DR - Ramez Al-Keelaniameer mousaAinda não há avaliações
- Bahan Bacaan PreeklampsiaDocumento11 páginasBahan Bacaan PreeklampsiaMegan LewisAinda não há avaliações
- Platelet Storage Pool Disorders PDFDocumento4 páginasPlatelet Storage Pool Disorders PDFMano CempakaAinda não há avaliações
- MRCPass Notes For MRCP 1 - HEMATOLOGYDocumento9 páginasMRCPass Notes For MRCP 1 - HEMATOLOGYsabdali100% (1)
- Whiteman 2000Documento23 páginasWhiteman 2000Hashem Essa QatawnehAinda não há avaliações
- Immunological Causes of Bad Obstetric HistoryDocumento14 páginasImmunological Causes of Bad Obstetric HistoryDara Dasawulansari SyamsuriAinda não há avaliações
- Antiphospholipid Syndrome:A Challenging Hypercoagulable Statewithsystemic ManifestationsDocumento8 páginasAntiphospholipid Syndrome:A Challenging Hypercoagulable Statewithsystemic ManifestationsFernando Re TaAinda não há avaliações
- New Developments in The Pathogenesis of Preeclampsia: Mihran V. NaljayanDocumento12 páginasNew Developments in The Pathogenesis of Preeclampsia: Mihran V. NaljayanRaymond FrazierAinda não há avaliações
- Prothrombin Gene Mutation G20210A, Homocysteine, Antiphospholipid Antibodies and Other Hypercoagulable States in Ocular ThrombosisDocumento5 páginasProthrombin Gene Mutation G20210A, Homocysteine, Antiphospholipid Antibodies and Other Hypercoagulable States in Ocular ThrombosisDouglas NoltieAinda não há avaliações
- Antiphospholipid SyndromeDocumento8 páginasAntiphospholipid SyndromeVijeyachandhar DorairajAinda não há avaliações
- Evaluate The Presence of Auto-Antibodies in Subjects With B - Thalassemia Major For Early Intervention To Decrease Morbidity and MortalityDocumento9 páginasEvaluate The Presence of Auto-Antibodies in Subjects With B - Thalassemia Major For Early Intervention To Decrease Morbidity and MortalityCentral Asian StudiesAinda não há avaliações
- Antiphospholipid Syndrome: Antiphospholipid Syndrome or Antiphospholipid Antibody Syndrome (APS orDocumento6 páginasAntiphospholipid Syndrome: Antiphospholipid Syndrome or Antiphospholipid Antibody Syndrome (APS orhikmat sheraniAinda não há avaliações
- Bone Marrow FailureDocumento4 páginasBone Marrow Failuremedicomauro2Ainda não há avaliações
- Disorders Leading To ThrombosisDocumento9 páginasDisorders Leading To ThrombosisGilo IlaganAinda não há avaliações
- Circulation 2014 Piazza 283 7Documento6 páginasCirculation 2014 Piazza 283 7arthoclaseAinda não há avaliações
- Urea and Protein Carbamylation in ESRD: Surrogate Markers or Partners in Crime?Documento3 páginasUrea and Protein Carbamylation in ESRD: Surrogate Markers or Partners in Crime?m29hereAinda não há avaliações
- Acquired Factor V Inhibitor RéviséDocumento7 páginasAcquired Factor V Inhibitor RéviséImen KrichenAinda não há avaliações
- Aplastic Anemia: Review of Etiology and TreatmentDocumento7 páginasAplastic Anemia: Review of Etiology and TreatmentCleber MaiaAinda não há avaliações
- ThrombophiliaDocumento37 páginasThrombophiliaapi-272740672Ainda não há avaliações
- DR Tejaswi Mekala PulDocumento26 páginasDR Tejaswi Mekala Pulnanichinni1436Ainda não há avaliações
- English For Medical Ii Plenary I: "Aplastic Anemia"Documento13 páginasEnglish For Medical Ii Plenary I: "Aplastic Anemia"Kang Wisit TheaAinda não há avaliações
- Pulmonary Hypertension: Advances in Pathogenesis and TreatmentDocumento12 páginasPulmonary Hypertension: Advances in Pathogenesis and Treatmentbdalcin5512Ainda não há avaliações
- M 105Documento8 páginasM 105midwfjessica4Ainda não há avaliações
- Antiphospholipid Syndrome A Review PDFDocumento9 páginasAntiphospholipid Syndrome A Review PDFDiah Puspita RiniAinda não há avaliações
- Antiphospholipid Antibody SyndromeDocumento37 páginasAntiphospholipid Antibody SyndromeAhmad Reshad AslamAinda não há avaliações
- Guidelines On The Investigation and Management of Antiphospholipid SyndromeDocumento12 páginasGuidelines On The Investigation and Management of Antiphospholipid Syndromefarish_machyaAinda não há avaliações
- Antiphospholipid Syndrome: Key PointsDocumento10 páginasAntiphospholipid Syndrome: Key PointsNelson CespedesAinda não há avaliações
- Literature Review On Sickle Cell DiseaseDocumento8 páginasLiterature Review On Sickle Cell Diseaseafmzwflmdnxfeb100% (1)
- Medscape Polisitemia VeraDocumento17 páginasMedscape Polisitemia VeraMiftahurrahmah GmsAinda não há avaliações
- Pages 4 7Documento4 páginasPages 4 7andreas_251650Ainda não há avaliações
- Pathogenesis and Management of Essential Thrombocythemia: Philip A. Beer and Anthony R. GreenDocumento8 páginasPathogenesis and Management of Essential Thrombocythemia: Philip A. Beer and Anthony R. GreenHoopmen SilaenAinda não há avaliações
- Antiphospholipid Syndrome: What's New?Documento6 páginasAntiphospholipid Syndrome: What's New?Wahyu Nunggal PramudaAinda não há avaliações
- Familial Hyperlipidaemia Risk AssessmentDocumento7 páginasFamilial Hyperlipidaemia Risk Assessmentdrpiratheepan4274Ainda não há avaliações
- Diet and Thrombosis Risk: Nutrients For Prevention of Thrombotic DiseaseDocumento10 páginasDiet and Thrombosis Risk: Nutrients For Prevention of Thrombotic DiseasemrsilAinda não há avaliações
- Inflammatory Biomarkers in Acute Coronary Syndromes: Clinician UpdateDocumento9 páginasInflammatory Biomarkers in Acute Coronary Syndromes: Clinician UpdateSandi AuliaAinda não há avaliações
- EclampsiaDocumento14 páginasEclampsiaUmi PulunganAinda não há avaliações
- Hematology: Thrombosis and The Antiphospholipid SyndromeDocumento2 páginasHematology: Thrombosis and The Antiphospholipid SyndromeYohanna YohannaAinda não há avaliações
- Antiphospholipid Syndrome and Pregnancy (Dengan Foto Punya DR RositaDocumento9 páginasAntiphospholipid Syndrome and Pregnancy (Dengan Foto Punya DR RositadidongAinda não há avaliações
- 304 Management of Hypertensive Disorders of Pregnancy-4Documento13 páginas304 Management of Hypertensive Disorders of Pregnancy-4anyAinda não há avaliações
- Rabies Menurut Inet MscapehDocumento8 páginasRabies Menurut Inet MscapehenvadAinda não há avaliações
- List AppDocumento1 páginaList AppenvadAinda não há avaliações
- Retinitis Pigmentosa CaseDocumento16 páginasRetinitis Pigmentosa CaseenvadAinda não há avaliações
- Organ Transplant BenefitDocumento7 páginasOrgan Transplant BenefitenvadAinda não há avaliações
- LupusDocumento7 páginasLupusorapoosaAinda não há avaliações
- Haemophilia: DR Y S Vishnu Vardhan, PGDocumento64 páginasHaemophilia: DR Y S Vishnu Vardhan, PGVishnu Vardhan100% (1)
- Disease & Def Patho/Mech Clinical S/S DX/ Tests/Labs TX NotesDocumento11 páginasDisease & Def Patho/Mech Clinical S/S DX/ Tests/Labs TX NotesSara AshurstAinda não há avaliações
- Bleeding Disorders: Hemorrhagic Diathesis: Frederick R. Llanera, MD, FPSP, Ascpi, Amt, RMTDocumento29 páginasBleeding Disorders: Hemorrhagic Diathesis: Frederick R. Llanera, MD, FPSP, Ascpi, Amt, RMTRaymond MalubayAinda não há avaliações
- Bleeding Time PDFDocumento25 páginasBleeding Time PDFKhaled ZatariAinda não há avaliações
- Recombiplastin 2G - 0020002950 (8 ML) : Al For Identification and Resolution of Out-Of-Control SituationsDocumento5 páginasRecombiplastin 2G - 0020002950 (8 ML) : Al For Identification and Resolution of Out-Of-Control SituationsSteffyPérezPioAinda não há avaliações
- CoagulopathyDocumento121 páginasCoagulopathyMegat Mohd Azman AdzmiAinda não há avaliações
- Secondary Hemostasis Activity BACHARODocumento3 páginasSecondary Hemostasis Activity BACHAROGilliana KathrynAinda não há avaliações
- Coagulation of BloodDocumento21 páginasCoagulation of BloodHery StiawanAinda não há avaliações
- Disorders Leading To ThrombosisDocumento9 páginasDisorders Leading To ThrombosisGilo IlaganAinda não há avaliações
- Icsh Hemostasis Critical ValuesDocumento12 páginasIcsh Hemostasis Critical Valuescitometria prolabAinda não há avaliações
- Secondary HemostasisDocumento9 páginasSecondary HemostasisMedicah Simon PeligrinoAinda não há avaliações
- Blood Coagulation Anticoagulant, Fibrinolytics, & AntiplateletsDocumento19 páginasBlood Coagulation Anticoagulant, Fibrinolytics, & AntiplateletsNoelle Grace Ulep BaromanAinda não há avaliações
- Clotting Factor Lesson Plan Recovered)Documento5 páginasClotting Factor Lesson Plan Recovered)Rebecca Jolie100% (1)
- Automated Blood Coagulation Analyzer CA-50: Basic Data Sheet - (Intrinsic Factors)Documento12 páginasAutomated Blood Coagulation Analyzer CA-50: Basic Data Sheet - (Intrinsic Factors)Aahsan Iqbal احسن اقبالAinda não há avaliações
- Disseminated Intravascular CoagulationDocumento5 páginasDisseminated Intravascular CoagulationElenaAinda não há avaliações
- Bleeding Disorders CandraDocumento38 páginasBleeding Disorders CandraDisya CittaAinda não há avaliações
- Module 2.1 - Coagulation TimeDocumento9 páginasModule 2.1 - Coagulation TimeI love dem Coffee (Migz)Ainda não há avaliações
- Hematology 2 SummaryDocumento8 páginasHematology 2 Summarymonzon.mika1801Ainda não há avaliações
- 1 Blood HemostasisDocumento32 páginas1 Blood Hemostasisarlinda noviana100% (1)
- Mechanisms of Hemostasis - Contributions of Platelets, Coagulation Factors, and The Vessel WallDocumento25 páginasMechanisms of Hemostasis - Contributions of Platelets, Coagulation Factors, and The Vessel WallelhierofanteAinda não há avaliações
- Chapter 41 - LEH Function TestDocumento6 páginasChapter 41 - LEH Function TestCha GuingabAinda não há avaliações
- Harrison's Review - Chapter 65 Bleeding and ThrombosisDocumento2 páginasHarrison's Review - Chapter 65 Bleeding and ThrombosisJason CentenoAinda não há avaliações
- Biochemistry A (RKTP, RMT) - Blood ChemistryDocumento10 páginasBiochemistry A (RKTP, RMT) - Blood ChemistryGaelle Lisette MacatangayAinda não há avaliações
- Blood Mbbs 12Documento28 páginasBlood Mbbs 12GITANSHU GALGATAinda não há avaliações
- 10-Platelet Structure and Function PDFDocumento21 páginas10-Platelet Structure and Function PDFAnil SharmaAinda não há avaliações
- Qualitative Analysis of How Certain Plant Products Can Increase The Rate of Blood Coagulation in HumansDocumento3 páginasQualitative Analysis of How Certain Plant Products Can Increase The Rate of Blood Coagulation in HumansInternational Journal of Innovative Science and Research TechnologyAinda não há avaliações
- ECL - EN - FinalDocumento2 páginasECL - EN - Finalmaroun machaalanyAinda não há avaliações
- Bloody Easy Coagulation SimplifiedDocumento24 páginasBloody Easy Coagulation SimplifiedIlyasHasanAinda não há avaliações
- HEMOPHILIADocumento70 páginasHEMOPHILIAtoyyibAinda não há avaliações
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNo EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNota: 5 de 5 estrelas5/5 (2)
- The Age of Magical Overthinking: Notes on Modern IrrationalityNo EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityNota: 4 de 5 estrelas4/5 (28)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNo EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNota: 4 de 5 estrelas4/5 (404)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNota: 2 de 5 estrelas2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNo EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNota: 5 de 5 estrelas5/5 (81)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNo EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaNota: 4.5 de 5 estrelas4.5/5 (266)
- Gut: the new and revised Sunday Times bestsellerNo EverandGut: the new and revised Sunday Times bestsellerNota: 4 de 5 estrelas4/5 (393)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNo EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNota: 5 de 5 estrelas5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNo EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNota: 4.5 de 5 estrelas4.5/5 (42)
- The Obesity Code: Unlocking the Secrets of Weight LossNo EverandThe Obesity Code: Unlocking the Secrets of Weight LossNota: 4 de 5 estrelas4/5 (6)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsAinda não há avaliações
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNo EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNota: 3.5 de 5 estrelas3.5/5 (3)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningNo EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningNota: 4 de 5 estrelas4/5 (3)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)No EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Ainda não há avaliações
- Why We Die: The New Science of Aging and the Quest for ImmortalityNo EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityNota: 4 de 5 estrelas4/5 (4)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisNo EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisNota: 3.5 de 5 estrelas3.5/5 (2)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryNo EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryNota: 4 de 5 estrelas4/5 (44)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeNo EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeNota: 4.5 de 5 estrelas4.5/5 (253)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.No EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Nota: 4.5 de 5 estrelas4.5/5 (110)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisNo EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisNota: 4 de 5 estrelas4/5 (1)
- The Marshmallow Test: Mastering Self-ControlNo EverandThe Marshmallow Test: Mastering Self-ControlNota: 4.5 de 5 estrelas4.5/5 (58)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsNo EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsNota: 4.5 de 5 estrelas4.5/5 (170)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingNo EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingNota: 4 de 5 estrelas4/5 (1138)