Escolar Documentos
Profissional Documentos
Cultura Documentos
C & L How Far Have We Come Curr Psych Rep
Enviado por
Adriana MendozaDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
C & L How Far Have We Come Curr Psych Rep
Enviado por
Adriana MendozaDireitos autorais:
Formatos disponíveis
Consultation-Liaison Psychiatry:
How Far Have We Come?
Sherese Ali, MD, FRCPC, Carrie Ernst, MD,
Manuel Pacheco, MD, and Gregory Fricchione, MD
Corresponding author
Gregory Fricchione, MD
Associate Chief of Psychiatry, Massachusetts General Hospital,
Warren 605, 55 Fruit Street, Boston, MA 02114, USA.
E-mail: gfricchione@partners.org
Current Psychiatry Reports 2006, 8:215 222
Current Science Inc. ISSN 1523-3812
Copyright 2006 by Current Science Inc.
This article takes stock of how far the eld of consultation-liaison psychiatry has come since its inception in the
20th century. In order to do this, we review its past in
terms of its knowledge base in psychosomatic medicine
and in terms of its practice at the bedside in the general
hospital setting. We also offer a contemporary account
of the eld and nish with a subjective view of the
opportunities and pitfalls faced during the next phase of
consultation-liaison psychiatry in the 21st century.
Introduction
Consultation-liaison (CL) psychiatry is the practical arm
of the eld called psychosomatic medicine. It has gone
through several phases in its existence and enters the 21st
century with a recognized place in the world of subspecialty medicine, with a list of accomplishments behind it,
and with a series of challenges ahead. This article reviews
where CL psychiatry came from, where it is now, and
where it is going.
CL Psychiatry in the Past
From the time of Hippocrates, there have been attempts
to integrate the mind and the body. Views of illness
were more religious or mystical during the Middle Ages,
whereas quasi-biological views came into vogue during
the Renaissance period [1]. The interest in the relationship between the mind and the body re-emerged in the
19th century. Important early gures included Johann
Heinroth, who rst used the term psychosomatic in
1818 to describe certain causes of insomnia, and William
Beaumont, who made empirical observations in 1833
about the effect of psychological factors on the gastric
mucosa [1]. Inuential research by Pavlov and Cannon
in the early 20th century, publications by Dunbar and
Alexander on the psychosomatic disorders in the 1940s
and 1950s, and the increasingly popular American psychoanalytic movement gave recognition to the role of
emotional processes in causing somatic symptoms [1].
The eld of psychosomatic medicine was formalized by
the founding of the Academy of Psychosomatic Medicine
in 1954. Over the past half-century, the eld of psychosomatic medicine has expanded and has become a truly
focused discipline.
The terms consultation-liaison psychiatry and
psychosomatic medicine have at times been used interchangeably, but historically, important distinctions have
been made between the two terms. In 1967, Lipowski [2]
dened CL psychiatry as that area of clinical psychiatry
which includes all diagnostic, therapeutic, teaching, and
research activities of psychiatrists in the non-psychiatric
parts of a general hospital. Called by some the clinical
arm [1] or an applied form [3] of psychosomatic medicine, CL psychiatry has been described as an organized
subspecialty of psychiatry. Psychosomatic medicine, on
the other hand, has traditionally been conceptualized
as a nonclinical discipline concerned with ideas such as
the interplay of biological and psychosocial factors in
the development, course, and outcome of all disease [3].
In order to understand where CL psychiatry is headed, it
is useful to review the history of the eld.
Lipowski and Wise [3] argue that CL psychiatry
developed out of the organizational movement of general-hospital psychiatry and the theoretical movement
of psychosomatic medicine. Until the late 19th century, organized psychiatry was restricted to the setting
of the asylum [4]. The medical revolution that began in
the late 19th century created both the opportunity and
the need for an organized general-hospital psychiatry
movement. With the explosion in number of hospitals, medical schools, and scientic discoveries came
a change in view of the general hospital, now thought
of as a place for biomedical treatment, clinical teaching, and scientic research. The presence of psychiatric
patients within the general hospital revealed a need for
a psychiatric presence.
216
Medicopsychiatric Disorders
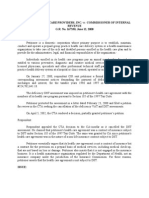
Table 1. Phases in the history of CL psychiatry
Years
Phases
Key events
Pre-1900
to 1930
Preliminary phase [5]
Medical revolution, new role for hospital and medical school
World War I, shell shock
1902: First true general-hospital psychiatry unit at Albany Hospital
1929: First clinical consultation psychiatry paper [6]
1930s to
late 1950s
Organization phase [3],
Pioneering phase [5]
19351935: Rockefeller grants establish psychiatric divisions in 5 general hospitals
1936: Billings introduces term liaison psychiatry into the literature
Early studies on cost/benet
1953: Academy of Psychosomatic Medicine founded
CL services established in many hospitals, using many different models
Psychoanalytic movement popular
Late 1950s
to 1980
Developmental phase [5]
Post-World War II: Many rejected or discharged for psychiatric reasons;
work on stress done
19601975
Conceptual-Development More research, publications, and organizations devoted to CL psychiatry
phase [3]
19751980s
Rapid-Growth phase [3]
Rapid growth in number of CL services
More formal organizational models and training programs
1967: Lipowski [2] published 3-part review detailing scope and function of a
CL service
1974: NIMH training grants for CL programs begin
Medicine shifts to primary care emphasis in context of rising costs, third-party payers
1980 to
present
Consolidation/
Retrenchment [5]
Consultation vs liaison debates
Rethinking objectives: no more proselytizing
NIMH training grants reduced, reimbursement limited
Liaison nurses and behavioral medicine
Desire to document cost effectiveness of CL psychiatry made difcult by
various factors such as shortened length of stay
CLconsultation-liaison; NIMHNational Institute of Mental Health.
The history of CL psychiatry can be divided into several
chronological periods (Table 1). Schwab [5] calls the period
from the late 19th century through 1930 the preliminary
phase. This phase was characterized by the opening of the
early general-hospital psychiatry departments. In 1872,
James Jackson Putnam, a neurologist at Massachusetts
General Hospital, who ironically is often thought of as the
rst consultation psychiatrist, was given the title of Chief
Electrician. In this role, he saw patients with functional
disorders and in 1903 got two hospital beds for the care
of neuropsychiatric patients [4]. Pavilion F, the rst generalhospital psychiatry unit, opened in 1902 at Albany Hospital.
Other prominent gures who advocated for a greater role for
psychiatry within the general hospital included Adolf Meyer
and William Alanson White.
The task of introducing psychiatry into the general
hospital proved challenging, in part because of limited
interest on the part of other physicians. Over the next 20
years, only a few hospitals opened psychiatry units or had
consultation psychiatrists [5]. World War I was important
in revealing the need for general-hospital psychiatry, as
many soldiers were either rejected or discharged for neuropsychiatric reasons and required specialized treatment
during their hospital stays [4]. The end of the preliminary
phase was marked by the publication of the rst clinical
paper in consultation psychiatry. Appearing in the American Journal of Psychiatry in 1929, George Henrys paper,
Some Modern Aspects of Psychiatry in General Hospital
Practice, [6] addressed issues such as the clinical indications for psychiatric consultations and the value of the
general-hospital psychiatrist.
Lipowski and Wise [3] designated an organization
phase (1935 to 1960) that paralleled Schwabs [5] pioneering phase (early 1930s to late 1950s). This period
was characterized by the establishment of psychiatric
services in many hospitals, made possible by substantial
grants in 1934 and 1935 from the Rockefeller Foundation.
The rst formal division of CL psychiatry was established
Consultation-Liaison Psychiatry
in 1934 by Edward Billings at Colorado General Hospital.
Clinical service, teaching, and research were all integral
to this Psychiatric Liaison Department. [3]. Billings, who
was something of a visionary, was also the rst to conduct
studies on the cost effectiveness of consultation psychiatry services. Services at Massachusetts General Hospital,
Johns Hopkins, the University of Rochester, and Mount
Sinai followed.
As there was not yet a formal structure, the organization and operation of each individual psychiatric service
depended on the hospital or practitioners. For example,
at the University of Rochester the psychiatrists were often
trained rst as internists and only later got their psychiatric education. From this tradition came George Engels
biopsychosocial approach to medicine. In contrast, at
Mount Sinai, psychiatrists were dispersed throughout the
hospital with the goal of teaching, consulting, and fostering collaboration [3].
Unlike the early years, when consultations were
predominantly patient-oriented and the goal of the consultant was to provide useful services when requested,
this period (which coincided with the increasing
popularity of the psychoanalytic movement) saw the
emergence of the liaison psychiatrist. The liaison
psychiatrists main objective was didacticthat is, to
demonstrate to other physicians the value of the biopsychosocial point of view. In many cases, this included
evaluation of the staff s behavior, looking for the effects
of transference and countertransference, and better
approaches to illness behavior [7]. However, some liaison psychiatrists thought of themselves as critical role
models for the hospital, with superior truths to impart
to others [8]. Some even optimistically predicted that
psychiatrists would soon be required in all hospital
wards and clinics [9]. Dubbed proselytiz[ing] [10],
indoctrination and inltration [11], conversion [8],
or professional fanaticism and salesmanship [2] by
some, this approach not surprisingly engendered strong
resistance from nonpsychiatrists.
From the 1950s onward, consultation psychiatry
moved into a rapid period of development. Labeled the
developmental phase (late 1950s to 1980) by Schwab
[5] and the conceptual-development phase (1960 to
1975) and rapid-growth phase (1975 to 1980s) by Lipowski and Wise [3], this time saw a large increase in the
number of psychiatry departments, the establishment of
formal CL psychiatry fellowships, and an explosion in
the number of publications and research activities. The
eld began to dene itself as a true subspecialty, and
much attention was focused on organizational issues.
Various formal models for consultation were proposed,
the balance between consultation and liaison activities
was debated, and specic roles were dened. In 1967,
Lipowski [2] published the historic three-part Review of
Consultation Psychiatry and Psychosomatic Medicine,
which laid out the organizational and strategic aspects
Ali et al.
217
of psychiatric consultation and pointed out some of the
challenges faced by this young eld. During this period,
consultation psychiatry became more integrated into
residency training and fellowships were established. In
the United States, both were supported by training grants
to CL programs given in 1974 by the National Institute of
Mental Health [9].
The consolidation/retrenchment phase [5] brought
CL psychiatry from 1980 to the present. Inuenced by the
overall favorable economic, political, and social climate of
the period, CL psychiatry enjoyed a period of some stability [8]. However, an increasing emphasis on the nancial
bottom line, hastened by the adoption of a business
model in American medicine, has begun to threaten the
homeostasis of CL services, which have never been cash
cows in psychiatry departments. The psychiatry departments themselves have been threatened by an every boat
on its own bottom ethos, to mix metaphors.
This nancial challenge led to an opportunity for the
subspecialty. A focus on outpatient primary care medicine returned in the context of the governments growing
concerns about the escalating cost of health care and
the emergence of third-party payers. Consultation psychiatrists were viewed as perfectly suited to help prepare
primary care clinicians for the many psychiatric patients
they were likely to see. Additionally, with the increasing
biomedical sophistication in intensive care units and
other hospital settings, busy physician specialists began
deferring to hospital-based psychiatrists to assume some
of the traditional roles of the primary clinical caretaker
for their patients [11].
Economic forces during this period made the liaison
model increasingly difcult to sustain, so a more consultation-oriented model began to prevail. Nonphysician
clinicians such as nurses and social workers began to
take on a role in this new climate, new treatments such as
behavioral medicine were sometimes used, and research
in cost effectiveness and outcomes as well as in psychosomatics and disease mechanisms increased. Certain
inherent difculties, such as an already shortened hospital length of stay, create a problem in showing a cost
offset of psychiatric consultation [12]. Cost effectiveness
measures that include patient satisfaction variables may
be more likely to show improvement.
As CL psychiatry emerged as a true subspecialty with
its own identity, body of knowledge, research, and literature, the question of whether the eld should get formal
subspecialty status was raised.
CL Psychiatry in the Present
Today, CL psychiatry enjoys status as an accredited
subspecialty in the eld of psychiatry under the name
Psychosomatic Medicine. In 2003 the American Board
of Psychiatry and Neurology (ABPN) unanimously
supported the decision to present CL psychiatry to the
218
Medicopsychiatric Disorders
American Board of Medical Subspecialties for accreditation, a proposal also supported by Accreditation Council
for Graduate Medical Education (ACGME), making it the
seventh accredited subspecialty in the eld of psychiatry.
CL psychiatry is currently served by three national subspecialty organizations and supports at least three major
subspecialty journals. Fellowship examinations are now
a requirement for certication as a specialist in psychosomatic medicine. Adding this subspecialty certication
opportunity to fellowship training and the formal
2-month requirement with outlined objectives for CL
psychiatry in psychiatry residency training programs certainly reects the strides that the subspecialty has made
in securing its place as a separate entity encompassing a
signicant area of specialized knowledge and research.
Research in CL psychiatry has made major contributions in the eld of medicine, drawing attention to the
psychiatric sequelae of many medical disorders, the
treatment of psychiatric disorders in comorbid medical
illnesses, drug interactions with psychotropics, and the
effect of nonpsychotropic medications on psychiatric
symptoms. In many instances, studies have identied
signicant clinical implications of stress and allostatic
loading and issues of the prognostic value and symptom burden of psychiatric illness in those with medical
illnesses. These have included several landmark studies
in diabetes, HIV/AIDS, coronary artery disease, cancer,
and stroke. The eld has become so vast that focused
areas in burn, intensive care, and transplant psychiatry
and psycho-oncology have evolved as the signicance of
psychiatric disorders in the various medical disciplines is
increasingly recognized.
Depression after myocardial infarction (MI), for
example, represents a rich area of research in psychosomatic medicine and CL psychiatry. There is now good
evidence for signicantly greater risk for all-cause mortality at 5 years post-MI in patients who have depressive
symptoms at the time of hospitalization for acute coronary
syndrome with or without conrmed MI [13]. Depression
has also been found to be associated with increased risk
of mortality and morbidity in patients with acute MI complicated by heart failure; in fact, depression was a stronger
predictor for all-cause mortality than left ventricular ejection fraction [14]. These ndings have raised the issue of
the effects of depression on cardiovascular physiology.
There is now good evidence for pathogenic mechanisms
in depression, such as increased platelet reactivity [15] and
decreased heart rate variability [16].
The possible effects of selective serotonin reuptake
inhibitors (SSRIs) on the above biologic factors and on
cardiac outcomes remain in question. Some frequently
cited trials, including SADHART [17], ENRICHD [18],
and MIND-IT [19], have investigated the effect on cardiovascular outcomes of treating depression. Although
the ENRICHD study did not demonstrate change in
cardiovascular outcome from using cognitive-behavioral
therapy for treatment of depression, SADHART showed a
trend toward improvement in cardiac outcomes using the
SSRI sertraline, and it is hoped that MIND-IT will help
to clarify whether this effect is truly signicant. Even if
these studies show equivocal results, they have at least
led to the recognition of depression as an important cause
of cardiac morbidity and mortality, and CL psychiatrists
are on the front lines of mobilizing efforts to address this
clinical challenge.
The prevalence of depression in patients with diabetes
has been found to be twice that in the general population [20]. Several studies have investigated the impact
of depression on glycemic control, symptom burden,
and compliance with behavioral interventions. Associations have been found between depression and glycemic
control and microvascular and macrovascular complications [21], through mechanisms not fully understood.
Although improvement in affective outcome with treatment has been reported, the effects on glycemic control
have been mixed [22]. Studies looking at the symptom
burden in depressed diabetic patients have found that
after controlling for disease severity measures, patients
with depression are two to ve times more likely to report
symptoms of diabetes [23]. Depressed patients are also
less likely to adhere to behavioral interventions such as
diet, exercise, and blood sugar monitoring, and they have
been shown to be less compliant in taking oral hypoglycemic agents [24]. These studies suggest that recognition
and management of depression are integral parts of care
of the diabetic patient and need to be improved in primary care settings, with the help of CL psychiatry.
Extensive research in the eld of psycho-oncology has
identied key points during the illness when the incidence
of depression is very high, 35% to 45%: 1) from diagnosis
to treatment, 2) at termination of treatment, 3) during survivorship, 4) on recurrence, and 5) during palliation [25].
Studies have consistently documented high prevalence
of symptoms of distress such as fatigue (49%), anxiety
(24%), and depression (24%) [26]. Such patients are
more likely to seek medical care and be offered third- and
fourth-line, intensive medical treatments for what may
be psychiatric symptoms [27]. On the other hand, studies
have demonstrated the effectiveness of psychiatric and
psychosocial interventions for symptoms of distress in
cancer patients [28]. A recent review of the literature [29]
showed positive associations on 15 of 24 variables linking depression with cancer progression and mortality,
especially earlier mortality [30]. Although a meta-analysis of 14 studies [31] was inconclusive regarding the effect
of treatment of depression on survival, vibrant debates
about this topic have been stimulated, and there is good
evidence that depression is the leading predictor of global
quality of life at baseline and at the end of treatment in
patients with cancer. This nding has highlighted the
need for intervention by CL psychiatry to screen for and
manage depression in this population.
Consultation-Liaison Psychiatry
A collaborative care intervention (the IMPACT trial
[32]) has shown clear benets in medical populations
aged 60 years and older over usual care for depression.
Teams including a depression care manager, primary
care doctor, and psychiatrist offer education, behavioral activation, antidepressants, brief behavior-based
psychotherapy (problem-solving treatment), and relapse
prevention geared to each patients needs and preferences. Tailored collaborative care actively engages older
adults in treatment for depression and delivers substantial and persistent long-term benets, including
less depression, better physical functioning, and an
enhanced quality of life [32].
CL psychiatry has continued to contribute signicantly
to other major aspects of medicine, including recognition
and management of delirium, poststroke depression, and
psychiatric symptoms in epilepsy, Alzheimers disease,
Parkinsons disease, and HIV infection. A reection of
how far CL psychiatry has come is seen in the increase in
neuropsychiatric studies and the greater use of neuroimaging scans by psychosomatic medicine psychiatrists and
behavioral neurologists in an attempt to better understand brain and behavior. The crosstalk between the
CL psychiatrists and their neurology colleagues around
cases at the mind-brain interface is beginning to pay off,
and organizations like the American Neuropsychiatric
Association have fostered this linkage. Even to initiate
the closing of the gap between neurology and psychiatry is a major step away from the over-reliance years ago
on the use of esoteric psychological theories to explain
neuropsychiatric disease. One suspects that Freud the
neurologist would be pleased with this development, and
the eld of psychosomatic medicine is contributing to it.
Of course, the fact that the internal psychological environment is biological in its effect does not detract from
the importance of psychological mechanisms. Indeed, it
elevates them into the ranks of other physical risk factors
for diseases of all types.
Kornfeld [33] recently offered an elegant summary
of the contributions of CL psychiatry to medical care in
general hospitals. Among other work, he discussed the
major contributions of Hackett and Cassem, FrasureSmith and Lesperance, and Reich in cardiac psychiatry;
his own service at Columbia in helping to uncover why
some patients seek to sign out against medical advice;
the work of Sutherland, Holland, Oken, and Speigel in
psycho-oncology; the work of Abrams, Denour, Levy,
and Vierderman in psychonephrology; and the contributions of Robinson in poststroke syndromes, Perry in
HIV care, and Musselman on the relationship between
interferon and depression. Kornfeld [33] then remarked
on the effects of CL psychiatry on cost-benet analyses,
medical teaching, clinical ethics, end-of-life care, and
clinical genetics. He concluded that, through CL psychiatry, psychosomatic medicine has improved medical
practice, and, paradoxically, he predicted that the eld
Ali et al.
219
will ourish even more as medicine becomes more and
more technological.
But how bright is the future of the eld?
CL Psychiatry in the Future
Most psychiatric care in the United States is now delivered
in the general-hospital psychiatry setting, as the number
of stand-alone inpatient psychiatric beds in state, Veterans Administration, and private institutions dwindles. In
this context, psychosomatic medicine has emerged as the
de facto face of psychiatry presented to clinicians in all
other areas of medicine and to most of the patients who
receive their treatment in academic hospital settings.
Paralleling this decrease in the absolute number of
inpatient psychiatric beds is the decreasing length of stay
of inpatient psychiatric admissions; the average inpatient
length of stay for all diagnoses is now less than 5 days
[34]. Accordingly, the percentage of patient encounters
for consultation psychiatrists that will occur in the outpatient arena is likely to mount. Primary care providers
and other nonpsychiatrists write the vast majority of
prescriptions for psychotropic drugs, with lower rates
of diagnostic accuracy and poorer treatment outcomes
than psychiatrists [35]. Visits solely for the prescription
of psychotropic medications comprise more than 6% of
outpatient ofce visits across all specialties [36]. These
realities underscore the fact that current collaborative
efforts in the nonpsychiatric outpatient setting should
continue to grow. The main rate-limiting step in this
clinical expansion of CL psychiatric services is the relative lack of behavioral health reimbursement. Changing
this disparity will continue to be a challenge.
At Massachusetts General Hospital, CL psychiatric
services are an active area of expansion in the Division of
Psychiatry and Medicine. An increasing number of psychiatrists are embedded in primary care clinics and such
subspecialty clinics as HIV, gastroenterology, and oncology, where they are available for consultation to both
attendings and trainees. We have been able to provide this
service only by insisting on subsidies from our colleagues
so that we dont wind up losing money on the services we
provide; we cant make up our losses in volume when we
collect only about 30 cents on every dollar we bill.
Often it is physically impossible to practice in situ
when colleagues in need of consultation are situated in
remote locales. Telemedicine has arisen as a means to
address this need. A meta-analysis of telemedicine psychiatric consultations has found them to be both cost
effective and efcacious [37]. Recently this technology
has been applied successfully across a variety of diagnoses and populations, such as rural jails [38], victims
of domestic violence [39], and patients with alcoholism
[40]. In the future, CL psychiatrists will naturally be
drawn to the use of telemedicine, which will increase services to distant settings.
220
Medicopsychiatric Disorders
CL psychiatrists may someday be called upon to direct
cases to such new treatment modalities as vagus nerve
stimulation (VNS), deep brain stimulation (DBS), and
transcranial magnetic stimulation (TMS). VNS has been
approved by the US Food and Drug Administration since
1997 for treatment of refractory partial seizures in patients
over the age of 12. Since then, it has been shown to have
efcacy in reducing the frequency of generalized seizures
and the dosage and number of antiepileptic medications
to which patients are exposed [41]. Results of studies on
the efcacy of VNS for the treatment of depression have
been mixed, however [42]. DBS is well established for the
surgical treatment of essential tremor, dystonia, parkinsonian tremor, multiple sclerosis tremor, and even chronic
pain [4345], but its usefulness in psychiatric disorders
will require much future study. Similarly, the application
and efcacy of TMS in major depression, schizophrenia,
and anxiety disorders is not yet well delineated and will
require renement and more research [46]. Nevertheless, we should contemplate future applications for these
modalities in our patient populations. At the same time,
new medical technologies, although potentially life-saving, will sometimes lower the threshold for psychiatric
morbidity in their recipients. For example, having cardiac
electrophysiologic studies, proceeding to the implantation
of an automatic implantable cardioverter-debrillator,
and then having the device randomly discharge appears
to put certain patients at risk for panic-phobic anxiety
and for post-traumatic stress disorder [47].
Certain clinical conditions will present CL psychiatrists with signicant opportunities to be of service.
Among others, these include those who have survived
cancer, the elderly with medical illnesses, those with metabolic syndrome and diabetes, patients with heart disease
with depression and anxiety, the HIV-infected population living under conditions of stress and depression, and
those patients in need of physical rehabilitation. Many of
these patients may benet from the adjunctive treatment
of behavioral medicine specialists equipped to provide
relaxation training and cognitive-behavioral therapy. At
Massachusetts General Hospital, we have a Behavioral
Medicine Service that works alongside the CL psychiatrists
in outpatient venues. Translation into clinical practice of
the vast amount of data generated by the National Institute of Mental Health and other research enterprises can
be difcult. Most patients do not t neatly into the tidy
categories studied in most federally funded research. CL
psychiatrists will therefore continue to be called upon to
use psychiatric research ndings in creative ways.
Thus, treatment innovations will continue to present future challenges for CL psychiatry. The uses of
intravenous haloperidol for the agitation of acute encephalopathy, lorazepam in the treatment of catatonia, and
psychostimulants for depressed medically ill patients are
all examples of clinical research done on a consultation
psychiatry service with little or no outside funding. These
approaches are now widely used throughout medicine
and represent important contributions from this eld.
Although we should continue this rich tradition of
nding pragmatic solutions for our patients conditions,
we must also do a better job of lobbying for funding for
the research we will need to do on patients with comorbid medical-surgical and psychiatric conditions. This will
require an overhaul of present narrow angle constituencies and will require the devotion of CL psychiatrists to
more rigorous research training in an effort to hone in
on the kinds of skills rewarded with funding. Competition in the near future will, if anything, become stiffer in
the face of a shrinking research dollar. Nevertheless, we
should consider encouraging more of our junior faculty
to apply for training awards from the National Institute
of Mental Health and awards from other funding sources
such as the National Cancer Institute and the National
Heart, Lung, and Blood Institute.
Perhaps the most far-reaching research for future CL
psychiatrists will take them into the realm of public health.
Knowledge of psychosomatic medicine, stress physiology
and allostatic loading, attachment style, and resiliency will
be essential in planning large-scale behavioral health promotion and illness prevention programs aimed at modern
epidemics such as the metabolic syndrome.
The recent initiative by the Academy of Psychosomatic
Medicine to build a research consortium eventually will
allow the gathering of large enough samples of subjects
to power studies dealing with questions of comorbidity
and may help to attract the funding necessary to carry
out such large-scale studies.
Most medical schools in the United States require a
psychiatry clerkship rotation as part of their third-year
curriculum. Although in many traditional curricula this
is composed primarily of a core clerkship experience
in an inpatient locked unit, psychosomatic medicine is
now emerging in many programs as an additional exposure for these medical students. This seems like a logical
point of contact for the vast majority of students who will
choose to practice in an area of medicine other than psychiatry. A rotation that includes CL psychiatry presents
an opportunity for them to become aware of the utility of
psychiatric consultation in all areas of the general hospital. As they continue in their professional development,
they may then retain their familiarity with the scenarios
in which psychiatric input is warranted.
In the 2005 National Residency Matching Program,
653 (4.7%) of the total of 13,798 graduating US medical
school seniors entered into ACGME-accredited residencies in general adult psychiatry [48]. Since 1961, residents
have been required to complete rotations in consultation
psychiatry at some point during their residency training. Questions still exist as to the appropriate timing for
this rotation. Should it take place during PGY-2, when
outpatient clinic demands are less time-consuming, or
in PGY-3, when residents possess more clinical experi-
Consultation-Liaison Psychiatry
ence? Whatever is decided for each residency, the place of
psychosomatics in these programs has been cemented in
place for the good of patient care.
Of the current 5900 postgraduate psychiatric trainees in the United States, only 33 (0.6%) have been
reported to be fellows in psychosomatic medicine
programs [49]. Though this gure may not be entirely
accurate, much work is still needed to increase the
attractiveness of the eld. Psychosomatic medicines
recent recognition as a subspecialty by the ABPN thrusts
new issues to the fore. The impact of ABPN accreditation
was touched upon during a presentation of the results
of a recent survey of Psychosomatic Medicine fellowship
training directors during the 2005 annual meeting of
the Academy of Psychosomatic Medicine [50]. Prior to
accreditation, board-eligible fellows in some programs
were considered junior attendings fully credentialed by
their respective institutions and capable of independent
billing for services rendered. Accreditation will therefore
adversely affect the revenue stream for some fellowships
and will require the pursuit of other funding sources
when a Medicare hospital slot is not reserved for a CL
fellow. The same survey also found that the fellowship
training directors were not unanimous in feeling that
the quality of education would necessarily improve with
accreditation. Of 25 survey respondents, eight thought
otherwise. To make the most of fellowship accreditation, its future effects on fellowship quality and practice
must be monitored.
Conclusions
Psychosomatic medicine has a rich tradition, as evidenced by its accumulated knowledge base and by the
role its practical armCL psychiatryhas traditionally
played in the general hospital and in outpatient settings.
Medicine in the 21st century will present a host of new
clinical challenges, many of which will open up opportunities for CL involvement and contribution. Recent
accomplishments such as ABPN recognition as a subspecialty and ACGME accreditation status for fellowships
have brought new energy, if not resources, to the eld.
These developments may be viewed as maturation in the
process of training these subspecialists. Nevertheless,
we will need to track the outcomes of these changes to
ensure that they are actually improving the ability of CL
psychiatry to provide the best care possible for patients
and the best education possible for trainees.
Research advances in our understanding of stress and
allostasis will enable us to contribute to public health
efforts, but our clinical research efforts will need to be
bolstered by commitment to improved research skills, by
research career trajectories for junior faculty members,
and by changes in the way research in clinical psychosomatic medicine is assessed and supported.
Ali et al.
221
References and Recommended Reading
Papers of particular interest, published recently,
have been highlighted as:
Of importance
Of major importance
Rogers MP, Fricchione G, Reich P: Psychosomatic medicine and consultation-liaison psychiatry. In The Harvard
Guide to Psychiatry. Edited by Nicholi AM, Jr. Cambridge,
MA: Belknap Press; 1999:362389.
2.
Lipowski ZJ: Review of consultation psychiatry and
psychosomatic medicine. I. General principles. Psychosom
Med 1967, 29:153171.
3.
Lipowski ZJ, Wise TN: History of consultation-liaison
psychiatry. In Textbook of Consultation Liaison Psychiatry.
Edited by Wise MG, Rundell JR. Washington, DC: American
Psychiatric Publishing; 2002:311.
4.
Friedman RS, Molay F: A history of psychiatric consultation in America. Psychiatr Clin North Am 1994, 17:667681.
5.
Schwab JJ: Consultation-liaison psychiatry: a historical
overview. Psychosomatics 1989, 30:245254.
6.
Henry GW: Some modern aspects of psychiatry in general hospital practice. Am J Psychiatry 1929, 86:481499.
7.
Neill JR: Once more into the breach: doubts about liaison
psychiatry. Gen Hosp Psychiatry 1983, 5:205208.
8.
Lipowski ZJ: Consultation-liaison psychiatrypast failures
and new opportunities. Gen Hosp Psychiatry 1979, 1:310.
9.
Lipowski ZJ: Liaison psychiatry, liaison nursing, and
behavioral medicine. Compr Psychiatry 1981, 22:554561.
10.
Strain JJ: Liaison psychiatry and its dilemmas. Gen Hosp
Psychiatry 1983, 5:209212.
11.
Greenhill, MH: The development of liaison programs. In
Psychiatric Medicine. Edited by Usdin G. New York: Brunner/Mazel; 1977:115191.
12.
Borus JF, Barsky AJ, Carbone LA, et al.: Consultationliaison cost offset: searching for the wrong grail.
Psychosomatics 2000, 41:285288.
13.
Grace SL, Abbey SE, Kapral MK, et al.: Effect of depression
on ve-year mortality after an acute coronary syndrome.
Am J Cardiol 2005, 96:11791185.
14.
Rumsfeld JS, Jones PG, Whooley MA, et al.: Depression
predicts mortality and hospitalization in patients with
myocardial infarction complicated by heart failure. Am
Heart J 2005, 150:961967.
15.
Serebruany VL, Glassman AH, Malinin AI, et al.; Sertraline
AntiDepressant Heart Attack Randomized Trial Study
Group: Platelet/endothelial biomarkers in depressed
patients treated with the selective serotonin reuptake
inhibitor sertraline after acute coronary events: the
Sertraline AntiDepressant Heart Attack Randomized
Trial (SADHART) Platelet Substudy. Circulation 2003,
108:939944.
16.
Chrapko WE, Jurasz P, Radomski MW, et al.: Decreased
platelet nitric oxide synthase activity and plasma nitric
oxide metabolites in major depressive disorder. Biol
Psychiatry 2004, 56:129134.
17.
Shapiro PA, Lesperance F, Frasure-Smith N, et al.: An
open-label preliminary trial of sertraline for treatment
of major depression after acute myocardial infarction
(the SADHART Trial). Sertraline Anti-Depressant Heart
Attack Trial. Am Heart J 1999, 137:11001106.
Landmark study addressing the importance of recognizing and
treating post-myocardial infarction depression with a serotoninspecic reuptake inhibitor.
18.
ENRICHD investigators: Enhancing Recovery in Coronary
Heart Disease (ENRICHD) study intervention: rationale
and design. Psychosom Med 2001, 63:747755.
1.
222
Medicopsychiatric Disorders
van den Brink RH, van Melle JP, Honig A, et al.: Treatment of
depression after myocardial infarction and the effects on
cardiac prognosis and quality of life: rationale and outline
of the Myocardial Infarction and Depression-Intervention
Trial (MIND-IT). Am Heart J 2002, 144:219225.
First study to directly examine the effect of treatment of post
myocardial infarction depression on cardiac prognosis.
20. Williams JW, Jr, Katon W, Lin EHB, et al. for the IMPACT
investigators: The effectiveness of depression care management on diabetes-related outcomes in older patients.
Ann Intern Med 2004, 140:10151024.
Large, randomized controlled trial demonstrating the benets of
collaborative care with psychiatry in older patients with diabetes
and depression with poor glycemic control.
21.
de Groot M, Anderson R, Freedland KE, et al.: Association
of depression and diabetes complications: a meta-analysis. Psychosom Med 2001, 63:619630.
22.
Lustman PJ, Grifth LS, Clouse RE, et al.: Effect of nortriptyline on depression and glycemic control on diabetes,
results of a double-blind, placebo-controlled trial. Psychosom Med 1997, 59:241250.
23.
Ludman EJ, Katon W, Russo J, et al.: Depression and diabetes
symptom burden. Gen Hosp Psychiatry 2004, 26:430436.
24.
Ciechanowski PS, Katon WJ, Russo JE: Depression and
diabetes: impact of depressive symptoms on adherence,
function and costs. Arch Intern Med 2000, 160:32783285.
25.
Carlson LE, Angen M, Cullum J, et al.: High levels of
untreated distress and fatigue in cancer patients. Br J
Cancer 2004, 90:22972304.
26.
Bultz BD, Carlson LE: Emotional distress: the sixth vital
sign in cancer care. J Clin Oncol 2005, 23:64406441.
27.
Ashbury FD, Findlay H, Reynolds B, et al.: A Canadian
survey of cancer patients experiences: Are their needs
being met? J Pain Symptom Manage 1998, 16:298306.
28.
Newell SA, Sanson-Fisher RW, Savolainen NJ: Systematic
review of psychological therapies for cancer patients:
overview and recommendations for future research. J
Natl Cancer Inst 2002, 94:558584.
29.
Spiegel D, Giese-Davis J: Depression and cancer: mechanisms and disease progression. Biol Psychiatry 2003,
54:269282.
30.
Akaho R, Sasaki T, Mori S, et al.: Psychological factors and
survival after bone marrow transplantation in patients
with leukemia. Psychiatry Clin Neurosci 2003, 57:9196.
31.
Smedslund G, Ringdal GI: Meta-analysis of the effects of
psychosocial interventions on survival time in cancer
patients. J Psychosom Res 2004, 57:123131.
32.
Hunkeler EM, Katon WJ, Tang L, et al.: Long-term outcomes
from the IMPACT randomised trial for depressed elderly
patients in primary care. Br Med J 2006, 332:259263.
33. Kornfeld DS. Consultation-liaison psychiatry: contributions to medical practice. Am J Psychiatry 2002,
159:19641972.
An elegant summary of the major contributions of CL psychiatry
to medical care in general hospitals.
34.
DeFrances CJ, Hall MJ, Podgornik MN: National Hospital
Discharge Survey. Advance data from Vital and Health Statistics
2003, no. 359. Hyattsville, MD: US Department of Health
and Human Services, CDC, National Center for Health
Statistics; 2005.
19.
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
Hohmann AA, Larson DB, Thompson JW, et al.: Psychotropic medication prescription in U.S. ambulatory medical
care. DICP 1991, 25:8599.
Pincus HA, Tanielian TL, Marcus SC, et al.: Prescribing trends
in psychotropic medications: primary care, psychiatry, and
other medical specialties. JAMA 1998, 279:526531.
Hyler SE, Gangure DP, Batchelder ST: Can telepsychiatry
replace in-person psychiatric assessments? A review and
meta-analysis of comparison studies. CNS Spectr 2005,
10:403413.
Manfredi L, Shupe J, Batki SL: Rural jail telepsychiatry: a
pilot feasibility study. Telemed J E Health 2005, 11:574577.
Thomas CR, Miller G, Hartshorn JC, et al.: Telepsychiatry
program for rural victims of domestic violence. Telemed J
E Health 2005, 11:567573.
Frueh BC, Henderson S, Myrick H: Telehealth service
delivery for persons with alcoholism. J Telemed Telecare
2005, 11:372375.
Schachter, SC: Vagus nerve stimulation therapy summary:
ve years after FDA approval. Neurology 2002, 59(6 Suppl
4):S15S20.
Nahas Z, Marangell LB, Husain MM, et al.: Two-year
outcome of vagus nerve stimulation (VNS) for treatment of major depressive episodes. J Clin Psychiatry 2005,
66:10971104.
Piper M, Abrams GM, Marks WJ, Jr: Deep brain stimulation for the treatment of Parkinsons disease: overview
and impact on gait and mobility. Neuro Rehabilitation
2005, 20:223232.
Tagliati M, Shils J, Sun C, et al.: Deep brain stimulation for
dystonia. Expert Rev Med Devices 2004, 1:3341.
Lefaucheur JP: Transcranial magnetic stimulation in
the management of pain. Suppl Clin Neurophysiol 2004,
57:737748.
Lisanby SH, Kinnunen LH, Crupain MJ: Applications of
TMS to therapy in psychiatry. J Clin Neurophysiol 2002,
19:344360.
Fricchione GL, Vlay SC: Neuropsychiatric aspects of
arrhythmia evaluation and management. In Manual of
Cardiac Arrhythmias: A Practical Guide to Clinical Management, Vol. 2. Edited by Vlay, SC. Boston: Little Brown;
1996:438450.
American Association of Medical Colleges: AAMC Data Book:
Statistical Information Related to Medical Education. Washington, DC: American Association of Medical Colleges; 2005.
American Psychiatric Association: Resident Census: Characteristics
and Distribution of Psychiatry Residents in the U.S. 20042005.
Arlington, VA: American Psychiatric Association, Ofce of
Graduate and Undergraduate Education; 2005.
Joseph RC, Fricchione GL, Bonds CL, et al.: Fellowship
training in psychosomatic medicineWhere are we
headed? Presentation at the 52nd Annual Meeting of the
Academy of Psychosomatic Medicine. Santa Ana Pueblo,
NM; November 1620, 2005.
Você também pode gostar
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Psychosomatic MedicineDocumento1.115 páginasPsychosomatic MedicineAndreea Bocirnea89% (18)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Anne Rice - Bibliography and Book DescriptionsDocumento10 páginasAnne Rice - Bibliography and Book DescriptionsAdriana Mendoza100% (2)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Staffing: Presentation TranscriptDocumento4 páginasStaffing: Presentation TranscriptagelesswapAinda não há avaliações
- Simon LeVay - The Sexual BrainDocumento156 páginasSimon LeVay - The Sexual BrainAdriana MendozaAinda não há avaliações
- NEDA Core Competencies With Cops Chart PDFDocumento1 páginaNEDA Core Competencies With Cops Chart PDFskydivaAinda não há avaliações
- Clinical Manual of Psychosomatic Medicine Rundell - Wise HandbookDocumento351 páginasClinical Manual of Psychosomatic Medicine Rundell - Wise HandbookAdriana Mendoza67% (3)
- Anne Rice - Lestat The Musical (16 Page Book)Documento8 páginasAnne Rice - Lestat The Musical (16 Page Book)Adriana MendozaAinda não há avaliações
- Psychiatric NursingDocumento12 páginasPsychiatric NursingLloyd Rafael Estabillo100% (1)
- Anne Rice - Short Story - Interlude With The Vampire - Armand's LessonDocumento5 páginasAnne Rice - Short Story - Interlude With The Vampire - Armand's LessonAdriana MendozaAinda não há avaliações
- Implementation of A Laboratory Information Management System at LRHDocumento7 páginasImplementation of A Laboratory Information Management System at LRHUdara Senarathne100% (1)
- Auerbachs Wilderness Medicine 7Th Edition Paul S Auerbach Et Al Full ChapterDocumento67 páginasAuerbachs Wilderness Medicine 7Th Edition Paul S Auerbach Et Al Full Chapterruby.nicholson732100% (7)
- China Health System..Documento40 páginasChina Health System..chandan singhAinda não há avaliações
- Preoperative Anesthesia and PremedicationDocumento10 páginasPreoperative Anesthesia and PremedicationFlorida Siregar0% (1)
- Phil. Health Care v. CirDocumento2 páginasPhil. Health Care v. CirPixie Dust100% (2)
- Anne Rice - Short Story - Interlude With The Vampire - Armand's LessonDocumento4 páginasAnne Rice - Short Story - Interlude With The Vampire - Armand's LessonAdriana MendozaAinda não há avaliações
- About Anne RiceDocumento22 páginasAbout Anne RiceAdriana MendozaAinda não há avaliações
- Derby NHS List of Suppliers 2012-13 & 2013 To DateDocumento97 páginasDerby NHS List of Suppliers 2012-13 & 2013 To DateVAinda não há avaliações
- Sedation ConceptsDocumento105 páginasSedation ConceptsSreejith SreekumarAinda não há avaliações
- YUGANDHARDocumento4 páginasYUGANDHARyugandhar reddyAinda não há avaliações
- Ankle Dislocations Health Conference 2010Documento16 páginasAnkle Dislocations Health Conference 2010Aswan IsmailAinda não há avaliações
- An Analysis of The Causes of Adverse Events From The Quality in Australian Health Care StudyDocumento7 páginasAn Analysis of The Causes of Adverse Events From The Quality in Australian Health Care StudyaxramosAinda não há avaliações
- Judicial RulingDocumento12 páginasJudicial RulingChaitanya SharmaAinda não há avaliações
- Products For PCNL BrochureDocumento8 páginasProducts For PCNL Brochuremusic43562981Ainda não há avaliações
- Company ProfileDocumento5 páginasCompany Profileganguly_ajayAinda não há avaliações
- Decide To Live Second Edition SoftcoverDocumento263 páginasDecide To Live Second Edition SoftcoverRod CzlonkaAinda não há avaliações
- Life Flora Hospital Johannesburg Life HealthcareDocumento1 páginaLife Flora Hospital Johannesburg Life HealthcareameerahAinda não há avaliações
- Registration Form For HCEs PDFDocumento3 páginasRegistration Form For HCEs PDFFarhan SyedAinda não há avaliações
- CHN-RLE Module 2 (Home Visits)Documento5 páginasCHN-RLE Module 2 (Home Visits)Ems Rio Bal100% (1)
- Global Perspectives On Mental HealthDocumento21 páginasGlobal Perspectives On Mental Health4127297Ainda não há avaliações
- Health CareDocumento1 páginaHealth CareMikeAinda não há avaliações
- Basic Life SupportDocumento4 páginasBasic Life Supportraven_claw25Ainda não há avaliações
- The Essential Anatomical Subunit Approximation Unilateral Cleft Lip RepairDocumento4 páginasThe Essential Anatomical Subunit Approximation Unilateral Cleft Lip Repairanggita ningratAinda não há avaliações
- Application CoopMED Health Insurance Plan BarbadosDocumento2 páginasApplication CoopMED Health Insurance Plan BarbadosKammieAinda não há avaliações
- Data Extraction Ulfasylvia Yudia PramanaDocumento3 páginasData Extraction Ulfasylvia Yudia PramanaMuhammad Ja'far ShadiqAinda não há avaliações
- Care Provision For Older AdultsDocumento7 páginasCare Provision For Older AdultsiamELHIZAAinda não há avaliações
- Letter of Complaint To Massachusetts Department of Public HealthDocumento4 páginasLetter of Complaint To Massachusetts Department of Public HealthGreg SaulmonAinda não há avaliações
- Total Quality Management: A Study On Implementation of Affinity Diagram' in Apollo HospitalDocumento10 páginasTotal Quality Management: A Study On Implementation of Affinity Diagram' in Apollo HospitalVindhya Mounika PatnaikAinda não há avaliações
- Introduction To Hospital Pharmacy: OutlineDocumento12 páginasIntroduction To Hospital Pharmacy: OutlinePrincess TiongsonAinda não há avaliações