Escolar Documentos
Profissional Documentos
Cultura Documentos
Patho. Reviewer. Thromboembolic Diseases
Enviado por
Seff CausapinDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Patho. Reviewer. Thromboembolic Diseases
Enviado por
Seff CausapinDireitos autorais:
Formatos disponíveis
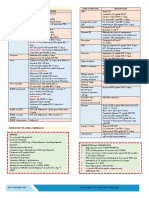
HEMODYNAMIC DISORDERS: THROMBOSIS AND SHOCK
Dr. WALTER
PATHOLOGY REVIEWER
If superficial: varicose veins saphenous veins local
congestion, pain, rarely embolize
1. Advanced age, bed rest and immobilization
2. CHF
3. Trauma, surgey, burns
4. Puerperal and post- partum
5. tumor
Disseminated intravascular coagulation
- not a dse but a complication
o microthrombi diffuse circulatory insufficiency
o rapid concurrent consumption of platelet and
coagulation factors serious bleeding
o
Deep vein thrombosis occurs in
Refers to the widespread fibrin thrombi in the
microcirculation, caused by variety of disorders
******* NOTHING FOLLOWS********
PATHOLOGY REVIEWER
How alterations of the normal blood flow can
cause thrombus formation?
This factor is important in causing thrombosis in
veins, cardiac chambers and arterial aneurysms;
hyperviscosity syndromes or deformed
erythrocytes.
Defined as any alteration of the coagulation
pathways that predisposes to thrombosis; occurs
less frequently
What is the most common heritable
hypercoagulable states?
Administration of the unfractionated heparin
induces circulating antibodies that cause platelet
activation and endothelial cell injury
Platelet activation of patients with antibodies
against anionic, phospholipids
Common morphology of thrombus
Thrombi that may also form on heart valves
Fate of thrombus
Deep veins thrombus
Arterial thrombi
Venous thrombi
HEMODYNAMIC DISORDERS: THROMBOSIS AND SHOCK
Dr. WALTER
a. Disrupts laminar flow and bring platelets into contact
with the endothelium
b. Prevents dilution of the activated clotting factors by
free- flowing blood
c. Retard inflow of clotting factor inhibitors and permit
build- up of thrombi
d. Promote endothelial cell activation
stasis
Hypercoagulability
Factor V gene mutations
Heparin- induced thrombocytopenia syndrome
Anti- phospholipid antibody syndrome
a.
b.
c.
d.
Aortic or cardiac thrombi- typically non- occlusive
Smaller arterial thrombi- usually occlusive
All begins at site of endothelial injury
Venous thrombi- occur is sites of stasis and are
occlusive
e. At sites of origin- firmly attached
f. Arterial thrombi- extend retrograde from attachment
point; venous extend following the direction of the
blood flow
g. May create an embolus
h. Cardiac and arterial thrombi are gray- red and tend to
have gross and microscopic laminations (lines of
Zahn) produced by pale layers of platelets and fibrin
alternating with red- cell rich lines.
i. Venous thrombosis- red- blue cast of vein lumen
Infective endocarditis- caused by bacteria or fungi
(vegetation)
Sterile vegetation- non- bacterial
Verrucous endocarditis (libman- Sacks)
If the patient survives the immediate effects;
a. Propagation- causing complete vessel obstruction
b. Embolization- esp. the lungs
c. Dissolution- by fibrinolytic activity
d. Organization and recanalization- re- establishing blood
flow
e. Bacterial seeding (rarely) of the thrombus resulting to
mycotic aneurysm
Willl cause only congestion and edema of the lower
extremities, but once it becomes an emboli, it can cause death
Are less likely to embolize, local obstruction is more important
o Usually occurs in superficial or deep veins
PATHOLOGY REVIEWER
HEMODYNAMIC DISORDERS: THROMBOSIS AND SHOCK
Dr. WALTER
Why plasmin activity is restricted to sites of
thrombosis?
Plasmin activator inhibitors are increased by?
Anticoagulants that are activated by thrombin.
Anticoagulant that is activated by plasmin
Anticoagulant that is activated by
Anticoagulant that is activated by heparin- like
molecules on the endothelium
This anticoagulant converts inactive circulating
plasminogen into active plasma
This anticoagulant breaks down fibrin and
interferes with its polymerization
Acts as weak anticoagulants
Inhibits thrombin and other serine proteasesfactors 9a,10a,11a,12a
Inactivates factors 5a and 8a
Procoagulant that is activated by released platelet
granules
Activated by vWf
Activated by exposed collagen
Activated by thrombin
Thrombin and well as certain cytokines
This procoagulant catalyzes the final steps of the
cascade leading to the production of fibrin
This procoagulant release cytokines and other
procoagulant substaces
This refers to the inappriorate activation of blood
clotting in uninjured
Composed the Virchow triad? (primary influences
on thrombus formation)
b. Anti- thrombins in the presence of heparin- like
molecules on the endothelium inhibit thrombin and
other serine proteases- factors 9a, 10a, 11a and 12a
c. In the presence of thrombomodulin, thrombin activates
proteins C and S which in turn inactivates factors 5a
and 8a
d. Thrombin induces endothelial release of tissue
plasminogen activator (t- PA) which convert inactive
circulating plasminogen into active plasmin. Plasmin
breaks down the fibrin and interferes with its
polymerization resulting to fibrin split products that
also act as weak anticoagulants
e. Endothelium regulates anti-coagulation by releasing
plasminogen activator inhibitors; these block
fibrinolysis by inhibiting t- PA binding to fibrin
1. t- PA activates plasminogen when bound to a fibrin
meshwork
2. free plasmin is rapidly neutralized by serum alpha2
plasmin inhibitor
3. t-PA activity is blocked by plasminogen activator
inhibitor
Thrombin as well as certain cytokines cause intravascular
thrombosis accompanying severe inflammation
Protein C and S, t- PA
Fibrin split producst
t- PA
antithrombins
t- PA
Plasmin
Fibrin split products
Antithrombins
Protein C and S
Calcium, ADP, phospholipid complex
Platelet granules
Von willebrand factor
Fibrin
Thrombin
vWf
Thrombosis
1. Endothelial injury
2. Alteration =s in normal blood flow
3. Hypercoagulability
PATHOLOGY REVIEWER
HEMODYNAMIC DISORDERS: THROMBOSIS AND SHOCK
Dr. WALTER
The lining of the blood vessels that modulates
several, frequently opposing aspects of
hemostasis
The properties exhibited by a normal endothelium.
The properties exhibited by the endothelium after
an injury.
What determines whether the thrombus formation,
propagation or dissolution occurs
This blood component plays a central role in
normal hemostasis and thrombosis.
When platelet is activated, it involves the ___
This process acts as bridge between platelet
surface receptors and exposed collagen
The process adhesion is mediated by what
factor?
The genetic deficiency dse of vWf or to in a
platelet receptor
What are the two types of granules that occurs
secretion
Endothelium
A vitamin that is important factor in coagulation
cascade
This provides a site for calcium and coagulation
factor binding in the intrinsic clotting cascade
What do you call the the platelet adhering to other
platelets
The mechanism of platelet aggregation.
Calcium (result)
This refers to the sequence of conversions of
inactive proenzymes into activated enzymes
culminating in the generation of insoluble fibrin
from the soluble plasma protein fibrinogen
The intrinsic and extrinsic pathway converge at
what factor?
The intrinsic pathway is traditionally initiated by
activation of what factor?
What activates the extrinsic pathway?
Each step of the intrinsic and extrinsic pathways
result from _____
What enzyme catalyzes the final steps of the
cascade?
Most of the effects of thrombin are induced
What are the control mechanism of hemostasis
and thrombosis?
Exhibit anti- platelet, ant- coagulant and fibrinolytic properties
Exhibit procoagulation function
The balance between the anti- thrombotic and pro- thrombotic
activities
Platelet
shape change, secretion and aggregation
Adhesion
Adhesion
Bernard- sullier syndrome
a. Alpha granule expresses the molecule P- selectin and
contained coagulation and growth factors
b. Delta bodies or delta granules- contains adenosine
nucleotides (ATP, ADP)
Phospholipid comples
Platelet aggregation
Promoted by: ADP and the platelet vasoconstrictor product
Thromboxane A2
Creates: the primary hemostatic plug which is reversible
Coagulation cascade
Factor 10 (X)
Factor 12 (Hageman Factor)
Tissue factor
Complex composed of an enzyme, a substrate and a cofactor
(reaction accelerator) all held together by calcium ions on a
phospholipid complex
Thrombin
via thrombin receptors, very potent, even in a small amount
a. Factor activation is restricted to sites of exposed
phospholipids, factors are diluted by flow at sites
distant from the original injury and cleared by the liver
and tissue macrophages
PATHOLOGY REVIEWER
Moderate infections and higher LPS levels
Severe infection
2nd mediators in severe infection may cause
Organs affected most often
Organs and the corresponding morphology in
shock.
3 general phases of shock
HEMODYNAMICS.PART 2
What is hemostasis?
A pathologic state wherein there is inappropriate
activation of hemostatic mechanisms in uninjured
vasculature or thrombotic occlusion of a vessel
after relatively minor injury.
Thrombosis and hemostasis depends on three
components which are ___
Summary of the normal hemostasis.
Considered as the first response of the
endothelial tissue to injury.
The stage of coagulation cascade where exposed
endothelial ECM allows platelet adhesion and
activation which secrete products attracting more
platelet to forma temporary hemostatic plug.
The stage where tissue factor exposed by the site
of injury activates the coagulation cascade
thrombin generation conversion of fibrin into
insoluble fibrin solid, permanent plug
HEMODYNAMIC DISORDERS: THROMBOSIS AND SHOCK
Dr. WALTER
Cytokine- induced secondary effectors become significant like
systemic effects of TNF and IL- 1
Septic shock, high- dose cytokines and secondary mediators
a. Systemic vasodilation
b. Diminished myocardial contractility
c. Widespread endothelial injury and activation ARDS
d. Activation of coagulation system DIC
Heart, brain, lungs, kidney, adrenals, GIT
Brain= hypoxic encephalopathy
Heart= areas of coagulation necrosis with subendocardial
hemorrhage, contraction- band necrosis or both kinds
Kidneys= extensive tubular ischemic injury causing oliguria,
anuria, and electrolyte imbalance
1. Initial non- progressive phase- reflex comepensatory
pathways are activated and perfusion of vital organs is
maintained
2. Progressive stage- tissue hypoperfusion and
metabolic imbalances etc
* peripheral pooling worsens cardiac output e
exacerbates endothelial anoxia DIC
3. Irreversible stage- the body has incurred cellular and
tissue injury that even if hemodynamics are corrected,
survival is not possible.
It is the normal physiologic process maintaining blood in a
fluid, clot- free state in normal vessels and inducing a rapid
and localized hemostatic plug at sites of vascular injury.
Thrombosis
1. Vascular endothelium
2. Platelets
3. Coagulation cascade
Endothelial injury platelet adhesion to the site of injury
(primary hemostasis) and recruit other platelets secrete
secretory granules recruit more platelet coagulation
cascade thrombin generation fibrinogen fibrin solid
permanent plug
Transient reflex neurogenic arteriolar vasoconstriction
augmented by endothelin (constrictor)
Primary hemostasis
Secondary hemostasis
PATHOLOGY REVIEWER
HEMODYNAMIC DISORDERS: THROMBOSIS AND SHOCK
Dr. WALTER
Factors that influence the development of an
infarct.
In infarct that is considered as an after shock or
systemic hypoperfusion
A morphology of infarct that occurs in venous
occlusions, loose tissues, tissues with dual
circulation and tissues previously congested
because of the sluggish venous outflow.
Observed in solid organs with end arterial
circulation.
In an infarct that is wedged- shape, what serves
as the base and apex?
The most dominant histologic characteristic of an
infarct.
Initial inflammatory responses is usually followed
by ___
What specific morphology is seen in a brain
infarct?
This infarction occur with embolization of infected
heart valve vegetations or when microbes seed
an area of necrosis.
What is shock?
Shock is the result of?
This is considered as the final common pathway
of many lethal events.
3 major categories of shock
Septic shock
This is released when cell walls are degraded and
this consist of toxic fatty acid (lipid A) core and a
complex of polysaccharide coat
Septic shock at low doses
a. Anatomic pattern of vascular supply- dual circulation
may tend to develop a collateral circulation, but with
end- arterial vessel, it may cause vessel obstruction
and eventually lead to infarction.
b. Rate of development of occlusion- slowly developing
occlusion may allow more time to develop collateral
circulation and the damage is less
c. Vulnerability to hypoxia- neurons for example, 3-4
mins of lack of blood supply may caused irreversible
damage, 20- 30 mins for the myocardium ad
fibroblasts in the myocardium is several hours
d. Oxygen content of the blood- conditions like anemia,
cyanosis or CHF can cause infarction
Watershed infarcts (necrosis at the places farthest from the
arterial supply)
Red infarcts
White infarcts
Apex is the occluded blood vessel; the base is the organ
periphery
Ischemic coagulative necrosis
A reparative response that in most cases eventually replaced
by a scar tissue
Liquefactive necrosis
Septic infarctions
A systemic hypoperfusion resulting from reduction in either
cardiac output or the effective circulating blood volume
Hypotension followed by impaired tissue perfusion and cellular
hypoxia
Shock
1. Low cardiac output- cardiogenic and hypovolemic
shock
2. Septic shock- caused by gm (-) bacteria
3. Neurogenic shock- with loss of vascular tone and
peripheral pooling
25- 75 % mortality
main cause of death in the ICU
70% is caused by gm (-) bacteria
Bacterial lipopolysaccharides (LPS)
Activates complement and monocytes macrophages
bacterial eradication
PATHOLOGY REVIEWER
HEMODYNAMIC DISORDERS: THROMBOSIS AND SHOCK
Dr. WALTER
This emboli causes decompression sickness,
obstetric complications
The morphology of this embolism are the
adipocytes within blood vessels
Complications of this embolism are pulmonary
disseminated intravascular coagulopathy
How many % of the pulmonary thromboembolism
is clinically silent?
Embolic obstruction of medium- sized arteries
may result to ____
When 60% of the pulmonary circulation is
obstructed with emboli may result to ___
This refers to the emboli in the arterial circulation
80% of systemic thromboembolism is from ___
How many percent of the systemic
thromboembolism is caused by MI and dilated
atria?
The 2nd most common cause of embolism
Occurs after fracture of the long bone
This syndrome is fatal in 10% causing sudden
pulmonary insufficiency 1- 3 days after injury with
20- 50% of the patients diffuse petechial rash
Describe the pathogenesis of the fat embolism
syndrome
Hallmark of diagnosing fat embolism.
Presence of air bubbles within the circulation that
causes obstruction.
For the air to be clinically significant, it should be
___ ml
This sickness is caused by sudden changes in
atmospheric temp
Mechanism of decompression sickness
The gas bubbles in skeletal muscle and joint
Gas bubbles in lungs
Treatment for decompression sickness
More chronic form of decompression sickness
This embolism is caused by the infusion of
amniotic fluid into maternal circulation
The classic findings of amniotic fluid embolism
If patient survives the initial crisis, what probably
might result to the patient?
An area of ischemic necrosis usually caused by
occlusion of the arterial supply (97% of the cases)
If venous drainage is the one occluded, what
might result?
Gas
Fat
Amniotic fluid
60- 80%
Pulmonary hemorrhage but not usually cause pulmonary
infarction due to collateral blood flow
Sudden death, right heart failure or cardiovascular collapse
Systemic thromboembolism
Cardiac mural thrombi
2/3 from the MI, 25% from the dilated atria, and the rest is
caused by aortic aneurysm, ulcerated atherosclerotic plaques,
valvular vegetations and parodixal emboli
Fat embolism
Microscopic fat globules
Fat embolism syndrome
Mechanical obstruction local platelet and erythrocyte
aggregation and release of the fatty acid toxic injury to
endothelium
Identifying microvascular fat globules
Air embolism
100 ml
Decompression sickness
Air breathed from a atmp. pressure high amount of gas
dissolved in blood and tissues rapid ascent
(depressurization) gasses bubble out of solution
The bends
The chokes
Repressurizing the individual followed by slow decompression
Caisson dse; ischemic necrosis
Amniotic fluid embolism
Fetal squamous cells, mucin, lanugo hair, venix caseosa fat in
the maternal pulmonary microcirculation
Pulmonary edema occurs
Infarction
It may cause infarction but more often only congestion due to
opening of bypass channels
PATHOLOGY REVIEWER
HEMODYNAMIC DISORDERS: THROMBOSIS AND SHOCK
Dr. WALTER
Mechanism of edema in decreased osmotic
pressure
Microscopic morphology of the edema.
Edema of what organ results to increased size
and weight and separation of parenchymal
elements
This edema morphology is typical in in leftventricular failure
This edema is often prominent in loose connective
tissue matrix e.g. eyelids
Localized to sites of injury (abscess, neoplasm) or
may generalized
Generalized brain edema
Refers to the extravasation of blood because of
vessel rupture
This type of hemorrhage is usually due to
vascular injury such as trauma, atherosclerosis, or
inflammatory/ neoplastic erosion of the vessel
This bleeding occurs with chronic congestion
Groups of hemorrhage
Larger (> 3mm) hemorrhages associated with
similar pathologies as well as trauma, vasculitis
and increased vascular fragility
Minute 1- 2 mm hemorrhages of the skin, mucous
membranes or serosal surfaces, with increased
intravascular pressure, low platelet count,
defective fxn and clotting factors deficits
These are subcutaneous hematomas (>1-2 cm)
commonly known as bruise and follows after a
trauma
Erythrocytes are degraded by
Illustrate how bruise develops
Clinically, hemorrhage depends on ___
Refers to aby intravascular solid, liquid, or
gaseous mass carried by the blood to a site
distant from its point or origin
How many % of thrombi becomes an emboli?
Common embolus materials
4 types of embolism
Type of embolism that has a morphology of fetal
squames, lanugo hairs within blood vessels
Reduces the movement of fluid into vessels due to loss of
albumin such as nephrotic syndrome. Exacerbated by salt and
water retention and net movement is into the interstitium
Subtle cell swelling with separation of ECM
Edema of the solid organs
Pulmonary edema (lungs enlarged by 2- 3x)
Subcutaneous edema
Brain edema
Brain is grossly swollen with narrowed sulci and distended gyri
flattened against the skull.
Hemorrhage
Rupture of the large artery and veins
Capillary bleeding
1. Petechiae
2. Purpura
3. Ecchymoses
4. Large accumulations of blood in the body
Purpura
petechiae
ecchymoses
Macrophages
Hemoglobin bilirubin and biliverdin hemosiderin (goldenbrown) changes of color of the bruise
volume and rate of blood loss
Embolism
99%
Fat, gas bubbles, atherosclerotic debris, tumor fragments,
bone marrow, foreign bodies
1. Thromboembolism
2. Fat
3. Gas
4. Amniotic fluid
Amniotic fluid
HEMODYNAMIC DISORDERS: THROMBOSIS AND SHOCK
Dr. WALTER
PATHOLOGY REVIEWER
.
QUESTIONS
The active process with augmented blood flow
caused by arteriolar dilatation.
What happens to tissue with hyperemia?
What is congestion?
Isolated venous obstruction may cause ____
Systemic venous obstruction causes _____
What is cyanosis?
Stasis of deoxygenated blood long enough can
cause?
Morphology of hyperemia and congestion.
This morphology is commonly associated with
edema
Chronic congestion is characterized by ____
In chronic congestion of the lungs, it typically
involves ___
Differentiate acute and chronic lung congestion
Congestion of the liver usually involves ____
Differentiate acute and chronic congestion of the
liver.
The condition of increased in fluid in the interstitial
tissue spaces or body cavities
What are the two pathologic categories of
edema?
Non- inflammatory causes
Increased hydrostatic pressure causes fluid to __
this obstruction blocks the removal of the
interstitial fluid
ANSWERS
hyperemia
Tissues are redder owing to engorgement with oxygenated
blood
The passive process caused by impaired outflow from a tissue.
local congestion
CHF
The red blue color of the tissue when by prolonged and
deoxygenated hemoglobin accumulates
Hypoxia cell death
a. Acute congestion
b. Capillary bed congestion
c. Chronic congestion
Capillary bed congestion
Capillary rupture hemorrhage
Breakdown of RBC hemosiderin- laden macrophages
Tissue appears: BROWN
Parenchymal cell atrophy or death with scaring may be
present
Common in: LIVER and LUNGS
Left- sided heart failure
Acute: engorged capillaries and septal edema with transudate
in the air spaces
Chronic: edematous to fibrotic septa, presence of hemosiderinladen macrophages which are considered as heart- failure
cells
Right- sided heart failure or with hepatic vein or SVC
obstuction
Acute: distention of central veins and sinusoids
Chronic: red- brown central region of hepatic lobules (nutmeg
liver)
Microscopic: cenrilobular necrosis
With severe long- standing congestion: hepatic fibrosis
(cardiac cirrhosis)
Edema (may be localized or systemic)
Non- inflammatory (yields protein- poor transudate)
Inflammatory (yields protein- rich exudate)
a. Increased hydrostatic pressure
b. Decreased osmotic pressure
c. Primary sodium retention
d. Lymphatic obstruction
Fluid to get out of the vessels, CHF is the most common cause
of systemic edema
Lymphatic obstruction
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Being Mortal: Medicine and What Matters in The EndDocumento15 páginasBeing Mortal: Medicine and What Matters in The EndEsteban0% (19)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- MNLG 4Documento2 páginasMNLG 4Kanchana Venkatesh39% (18)
- Introduction To Professional School Counseling Advocacy Leadership and Intervention Ebook PDF VersionDocumento62 páginasIntroduction To Professional School Counseling Advocacy Leadership and Intervention Ebook PDF Versionmary.krueger918100% (50)
- ArticlesOfConfederation Constitution 3.0Documento6 páginasArticlesOfConfederation Constitution 3.0ChristinaAinda não há avaliações
- Dem Tickler NotesDocumento1 páginaDem Tickler NotesSeff CausapinAinda não há avaliações
- Altitude IllnessDocumento4 páginasAltitude IllnessSeff CausapinAinda não há avaliações
- Thyroid 2Documento58 páginasThyroid 2Seff CausapinAinda não há avaliações
- Anterior Pituitary Tumor SyndromesDocumento10 páginasAnterior Pituitary Tumor SyndromesSeff CausapinAinda não há avaliações
- Urinary Tract ObstructionDocumento2 páginasUrinary Tract ObstructionSeff CausapinAinda não há avaliações
- Disorders of The Female Reproductive System PDFDocumento4 páginasDisorders of The Female Reproductive System PDFSeff CausapinAinda não há avaliações
- Glomerular Diseases: Pathogenesis of Glomerular Diseases Progression of Glomerular DiseasesDocumento6 páginasGlomerular Diseases: Pathogenesis of Glomerular Diseases Progression of Glomerular DiseasesSeff CausapinAinda não há avaliações
- Disturbances in Respiratory FunctionDocumento6 páginasDisturbances in Respiratory FunctionSeff CausapinAinda não há avaliações
- Approach To Patient With Endocrine DisordersDocumento2 páginasApproach To Patient With Endocrine DisordersSeff CausapinAinda não há avaliações
- Physical Diagnosis of The ThoraxDocumento3 páginasPhysical Diagnosis of The ThoraxSeff Causapin100% (1)
- Pathophysiology of SLEDocumento16 páginasPathophysiology of SLESeff CausapinAinda não há avaliações
- Complete Guide To Physical ExamDocumento19 páginasComplete Guide To Physical ExamSeff Causapin100% (2)
- Medicine (Dr. Pedroza) Copd 14 FEBRUARY 2018Documento3 páginasMedicine (Dr. Pedroza) Copd 14 FEBRUARY 2018Seff CausapinAinda não há avaliações
- LeptospirosisDocumento2 páginasLeptospirosisSeff CausapinAinda não há avaliações
- Vasoactive PeptidesDocumento8 páginasVasoactive PeptidesSeff CausapinAinda não há avaliações
- Vasoactive PeptidesDocumento8 páginasVasoactive PeptidesSeff CausapinAinda não há avaliações
- Eicosanoids: Arachidonic Acid & Other Polyunsaturated PrecursorsDocumento6 páginasEicosanoids: Arachidonic Acid & Other Polyunsaturated PrecursorsSeff CausapinAinda não há avaliações
- Sympathomimetic Agents: CLIN. PHARM (Dr. Salvador) Asthma 05 SEPT 2017Documento3 páginasSympathomimetic Agents: CLIN. PHARM (Dr. Salvador) Asthma 05 SEPT 2017Seff Causapin100% (1)
- SONA ReactionDocumento4 páginasSONA ReactionSeff CausapinAinda não há avaliações
- Test Bank On GI PathologyDocumento14 páginasTest Bank On GI PathologySeff CausapinAinda não há avaliações
- HEAD AND NECK 1.robbins & Cotran Pathologic Basis of Disease ReviewerDocumento14 páginasHEAD AND NECK 1.robbins & Cotran Pathologic Basis of Disease ReviewerSeff Causapin100% (1)
- History of AIDocumento27 páginasHistory of AImuzammalAinda não há avaliações
- Appendix H Sample of Coded Transcript PDFDocumento21 páginasAppendix H Sample of Coded Transcript PDFWahib LahnitiAinda não há avaliações
- Theology and Pipe Smoking - 7pDocumento7 páginasTheology and Pipe Smoking - 7pNeimar HahmeierAinda não há avaliações
- Effect of Employee Loyalty On Customer S PDFDocumento37 páginasEffect of Employee Loyalty On Customer S PDFShailendra DasariAinda não há avaliações
- Catibayan Reflection AR VRDocumento6 páginasCatibayan Reflection AR VRSheina Marie BariAinda não há avaliações
- Eurokids Parent Manual (ECity) - PDF-EJ and ESDocumento18 páginasEurokids Parent Manual (ECity) - PDF-EJ and ESsabarin_72100% (2)
- Student Health Services - 305 Estill Street Berea, KY 40403 - Phone: (859) 985-1415Documento4 páginasStudent Health Services - 305 Estill Street Berea, KY 40403 - Phone: (859) 985-1415JohnAinda não há avaliações
- Creativity & Innovation Brainstorming TechniquesDocumento50 páginasCreativity & Innovation Brainstorming TechniquesFirdhaus SakaffAinda não há avaliações
- RCPI V VerchezDocumento2 páginasRCPI V VerchezCin100% (1)
- Episode 5 The Global TeacherDocumento8 páginasEpisode 5 The Global TeacherEllieza Bauto SantosAinda não há avaliações
- Exam3 Buscom T F MC Problems FinalDocumento23 páginasExam3 Buscom T F MC Problems FinalErico PaderesAinda não há avaliações
- Software Development Life CycleDocumento70 páginasSoftware Development Life CycleChaitanya MalikAinda não há avaliações
- CardiologyDocumento83 páginasCardiologyAshutosh SinghAinda não há avaliações
- CNS Drugs Pharmaceutical Form Therapeutic Group: 6mg, 8mgDocumento7 páginasCNS Drugs Pharmaceutical Form Therapeutic Group: 6mg, 8mgCha GabrielAinda não há avaliações
- Yahoo Tab NotrumpDocumento139 páginasYahoo Tab NotrumpJack Forbes100% (1)
- Occupant Response To Vehicular VibrationDocumento16 páginasOccupant Response To Vehicular VibrationAishhwarya Priya100% (1)
- Long Range Plans ReligionDocumento3 páginasLong Range Plans Religionapi-266403303Ainda não há avaliações
- Finding Roots of Equations Bracketing MethodsDocumento11 páginasFinding Roots of Equations Bracketing MethodsmebrahtenAinda não há avaliações
- The Palatability, and Potential Toxicity of Australian Weeds To GoatsDocumento163 páginasThe Palatability, and Potential Toxicity of Australian Weeds To Goatsalshokairsaad513Ainda não há avaliações
- Biology Chapter 23.1Documento2 páginasBiology Chapter 23.1Carlos Enrique Altamar BorjaAinda não há avaliações
- LabDocumento11 páginasLableonora KrasniqiAinda não há avaliações
- Calculation For Service Platform & Pump Shelter StructureDocumento36 páginasCalculation For Service Platform & Pump Shelter Structuretrian33100% (1)
- ECON 4035 - Excel GuideDocumento13 páginasECON 4035 - Excel GuideRosario Rivera NegrónAinda não há avaliações
- They Cried MonsterDocumento13 páginasThey Cried MonstermassuroAinda não há avaliações
- Erythrocyte Sedimentation RateDocumento16 páginasErythrocyte Sedimentation Rateapi-3823785100% (2)
- Cyrano de BergeracDocumento209 páginasCyrano de BergeracKayleeAinda não há avaliações