Escolar Documentos
Profissional Documentos
Cultura Documentos
Urinary Elimination Issues in Elderly Male
Enviado por
Richard RLTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Urinary Elimination Issues in Elderly Male
Enviado por
Richard RLDireitos autorais:
Formatos disponíveis
koz74686_ch48.
qxd
11/8/06
5:59 PM
Page 1318
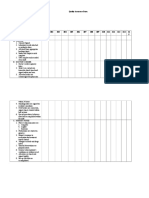
1318 UNIT X / Promoting Physiologic Health
Urinary Elimination
CONCEPT MAP
JB
68 y.o. male
BPH
Shopkeeper, c/o urinary
frequency 2 weeks,
nocturia 23 X/night,
difficulty starting stream,
dribbles, c/o not feeling
like bladder is emptied
assess
Height: 185.4 cm (6' 2")
Weight: 85.7 kg (189 lb)
Temperature: 38.1C (100.6F)
Pulse: 88
Respirations: 20/min
BP: 146/86
Catheterization for residual:
300mL amber urine
Foley left in place for 2 days
CBC normal; UA: amber, clear,
ph 6.5, SpGr 1.025, negative for
glucose, protein, ketones, RBCs,
and bacteria; IVP: enlarged
prostate gland
generate nursing diagnosis
Outcomes partially met:
Following removal of
the Foley catheter,
reported continued
difficulty initiating a
urinary stream but less
dribbling and nocturia
Intermittent
catheterization not
indicated
Intake is about
200 mL > output
Selected an acceptable
undergarment and he
reports more confidence
Impaired Urinary Elimination (Retention and Overflow Incontinence) r/t bladder neck
obstruction by enlarged prostate gland (aeb dysuria, frequency, nocturia, dribbling,
hesitancy, and bladder distention)
evaluation
nursing intervention
outcome
outcome
Urinary Continence
aeb
Able to start and
stop stream
Empties bladder
completely
Knowledge:
Treatment
Regimen aeb
substantial
Description
of self-care
responsibilities
for ongoing care
Description of
self-monitoring
techniques
nursing
intervention
Outcomes met:
Able to discuss
the correlation
between enlarged
prostate and
urinary difficulties
TURP scheduled
in 2 weeks
evaluation
nursing intervention
Urinary Incontinence Care
Urinary Retention Care
Teaching: Disease process
activity
activity
activity
Monitor
urinary
elimination,
including
odor,
volume,
and color
Instruct
client to
limit fluids
for 2 to 3
hours
before
bedtime
activity
Help client
select
appropriate
incontinence
garment or
pad for
short-term
management
while more
definitive
treatment is
designed
activity
Limit
ingestion
of bladder
irritants
(e.g., colas,
coffee, tea,
and
chocolate)
Instruct to
drink a
minimum of
1,500 mL
(six 8-ounce
glasses fluids)
per day
Instruct
client or
family
member
to record
urinary
output
activity
activity
activity
Provide enough
time for bladder
emptying
(10 min)
activity
activity
activity
activity
Explain the
pathophysiology
of the disease
and how it
relates to urinary
anatomy and
function
Implement
intermittent
catheterization;
as appropriate
Instruct in ways
to avoid
constipation or
stool impaction
Appraise
current
level of
knowledge
about
benign
prostatic
hypertrophy
Catheterize
for residual
urine, as
appropriate
activity
Describe the
rationale behind
management,
therapy, and
treatment
recommendations
Instruct on
which signs
and
symptoms to
report to the
primary care
provider (e.g.,
burning on
urination,
hematuria,
olliguria)
Você também pode gostar
- Completed Concept MapDocumento4 páginasCompleted Concept Mapapi-607361848Ainda não há avaliações
- Clinical Log Term II PDFDocumento9 páginasClinical Log Term II PDFPriscilla S100% (1)
- Renal Concept MapDocumento1 páginaRenal Concept MapShaira Ann CalambaAinda não há avaliações
- Nursing Concept MapDocumento2 páginasNursing Concept MapMary MannAinda não há avaliações
- STUDENT-Sepsis - Fundamental - Reasoning Fillable-1Documento5 páginasSTUDENT-Sepsis - Fundamental - Reasoning Fillable-1Laura PoultneyAinda não há avaliações
- CC Concept MapDocumento9 páginasCC Concept Mapapi-606252228Ainda não há avaliações
- FAELDONEA - B. Concept MapDocumento1 páginaFAELDONEA - B. Concept MapPatricia Jean FaeldoneaAinda não há avaliações
- Chest Pain System - DisorderDocumento1 páginaChest Pain System - DisorderAA DDAinda não há avaliações
- Cardiac FT: ResultsDocumento26 páginasCardiac FT: ResultsBillynTarplainAinda não há avaliações
- Chapter 08: Injectable Medications Mulholland: The Nurse, The Math, The Meds, 3rd EditionDocumento13 páginasChapter 08: Injectable Medications Mulholland: The Nurse, The Math, The Meds, 3rd EditionadenAinda não há avaliações
- TMendoza CriticalCareConceptMap2Documento5 páginasTMendoza CriticalCareConceptMap2Theresa Fernandez Mendoza0% (1)
- Peptic Ulcer DiseaseDocumento1 páginaPeptic Ulcer DiseaseEunice CortésAinda não há avaliações
- Care PlanDocumento11 páginasCare PlanAlyssa CardinalAinda não há avaliações
- Nursing Care Plans for Stroke PtDocumento13 páginasNursing Care Plans for Stroke PtJuls Flares SycaycoAinda não há avaliações
- VSIM Clinical Worksheet WORD 06.19Documento6 páginasVSIM Clinical Worksheet WORD 06.19Jackie GriffisAinda não há avaliações
- NSG-430 EcgDocumento19 páginasNSG-430 EcgSarah RealAinda não há avaliações
- Waiters Osteoarthritis PDFDocumento1 páginaWaiters Osteoarthritis PDFmp1757Ainda não há avaliações
- Nursing Clinical Prep SheetDocumento1 páginaNursing Clinical Prep SheetPatty Pasarilla PassehlAinda não há avaliações
- n360 Concept Map Care Plan Week 3 Sheryl SatoDocumento15 páginasn360 Concept Map Care Plan Week 3 Sheryl Satoapi-283363983Ainda não há avaliações
- Fluids and Electrolytes ConceptDocumento31 páginasFluids and Electrolytes ConceptDarwin AndalAinda não há avaliações
- IVY TECH NURSING LAB INFORMATIONDocumento7 páginasIVY TECH NURSING LAB INFORMATIONSethAinda não há avaliações
- Nur411 Syllabus Part 1 Fall 2011Documento21 páginasNur411 Syllabus Part 1 Fall 2011bmccsnresources0% (1)
- Concept MapDocumento1 páginaConcept Mapapi-246466200Ainda não há avaliações
- Concept Map Template NURS 3073Documento4 páginasConcept Map Template NURS 3073Savanna ChambersAinda não há avaliações
- Acute Renal Failure-Student-Rapid ReasoningDocumento4 páginasAcute Renal Failure-Student-Rapid Reasoningapi-268403950Ainda não há avaliações
- CC Concept MapDocumento11 páginasCC Concept Mapapi-546355187Ainda não há avaliações
- Concept Map 1Documento5 páginasConcept Map 1api-396919069Ainda não há avaliações
- Activity - PT - With - Fluid & Lyte ImbalanceDocumento3 páginasActivity - PT - With - Fluid & Lyte ImbalanceAngel Joy CatalanAinda não há avaliações
- CH 39 Acid-Base ElectrolyteDocumento16 páginasCH 39 Acid-Base ElectrolyteJonathan EdieAinda não há avaliações
- C 13Documento11 páginasC 13Jo100% (1)
- Care of Adults 25 Cardiovascular ManagementDocumento39 páginasCare of Adults 25 Cardiovascular ManagementGaras AnnaBerniceAinda não há avaliações
- Chronic Kidney Disease: Prepared by Zakia RogerDocumento27 páginasChronic Kidney Disease: Prepared by Zakia Rogerbene dugaAinda não há avaliações
- CHF Cardiomegaly Volume OverloadDocumento1 páginaCHF Cardiomegaly Volume Overloadnursing concept mapsAinda não há avaliações
- Cumulative Midterm Exam - A&PDocumento16 páginasCumulative Midterm Exam - A&PTran Winner100% (1)
- Understanding CHF and Monitoring Fluid StatusDocumento4 páginasUnderstanding CHF and Monitoring Fluid StatusWeng RamojalAinda não há avaliações
- Assessment and Concept Map Care Plan: Joseph GorospeDocumento5 páginasAssessment and Concept Map Care Plan: Joseph Gorospeapi-497389977Ainda não há avaliações
- Clinical Case Study - Online Discussion Form Fall 2020-1Documento14 páginasClinical Case Study - Online Discussion Form Fall 2020-1Sabrina Odies100% (1)
- Chapter 3 Fluid, Electrolyte and Acid BaseDocumento7 páginasChapter 3 Fluid, Electrolyte and Acid BaseSeverino Valerio100% (2)
- Endocrine MedicationsDocumento47 páginasEndocrine MedicationsAamir AzizAinda não há avaliações
- Exam 3 Review Med SurgDocumento18 páginasExam 3 Review Med SurgCarol ReidAinda não há avaliações
- Case Simu 101Documento5 páginasCase Simu 101Princess Levie CenizaAinda não há avaliações
- Nursing Assessment S - O Pt. May ManifestDocumento4 páginasNursing Assessment S - O Pt. May Manifestk_a1990Ainda não há avaliações
- Nursing Interventions Concept MapDocumento3 páginasNursing Interventions Concept Mapphelenaphie menodiado panlilioAinda não há avaliações
- Chapter 64 - Administration of Injectable MedicationsDocumento11 páginasChapter 64 - Administration of Injectable Medicationskristie donaldAinda não há avaliações
- Handout NSNA Student PresentationDocumento14 páginasHandout NSNA Student PresentationlisaAinda não há avaliações
- STUDENT Sepsis Rapid ReasoningDocumento6 páginasSTUDENT Sepsis Rapid Reasoningghodghod123Ainda não há avaliações
- More Med Surg Practice QuestionsDocumento14 páginasMore Med Surg Practice QuestionsmisscoombsAinda não há avaliações
- Life and DeathDocumento23 páginasLife and DeathJea Joel MendozaAinda não há avaliações
- Medical Surgical Nursing - DiabetesDocumento4 páginasMedical Surgical Nursing - Diabetestripj33100% (2)
- HeartFailure Nursing FIK 2014Documento101 páginasHeartFailure Nursing FIK 2014Putri NurlaeliAinda não há avaliações
- Chapter 11: Parenteral Administration: Intradermal, Subcutaneous, and Intramuscular Routes Test BankDocumento7 páginasChapter 11: Parenteral Administration: Intradermal, Subcutaneous, and Intramuscular Routes Test BankLuna TunaAinda não há avaliações
- System Disorder: Renal CalculiDocumento1 páginaSystem Disorder: Renal CalculiHolly DeckelmanAinda não há avaliações
- Case Study: Congestive Heart FailureDocumento7 páginasCase Study: Congestive Heart FailureXI-E / 21 / MARY TRIANAAinda não há avaliações
- HESI Women's Health:Newborn DrugsDocumento8 páginasHESI Women's Health:Newborn Drugsisapatrick8126Ainda não há avaliações
- Teamworks! Game: Summary ReportDocumento2 páginasTeamworks! Game: Summary ReportAngela May Pustasa AllamAinda não há avaliações
- Brain Dump NUR 213 FINALDocumento37 páginasBrain Dump NUR 213 FINALkelsey jackson100% (1)
- NURSING CARE OF ADULTS II: Passbooks Study GuideNo EverandNURSING CARE OF ADULTS II: Passbooks Study GuideAinda não há avaliações
- O'clock in The Evening at Buhay Na Tubig Covered Court.: Jeffrey Reyes Head OrganizerDocumento1 páginaO'clock in The Evening at Buhay Na Tubig Covered Court.: Jeffrey Reyes Head OrganizerRichard RLAinda não há avaliações
- SolicitationDocumento13 páginasSolicitationRichard RLAinda não há avaliações
- Quality Assurance FormDocumento4 páginasQuality Assurance FormRichard RLAinda não há avaliações
- Vagina CarbunklecaseDocumento10 páginasVagina CarbunklecaseRichard RLAinda não há avaliações
- Kennedy ReflectionDocumento8 páginasKennedy ReflectionRichard RLAinda não há avaliações
- Municipality of Imus, Cavite Office of The MAYOR July 14, 2016Documento2 páginasMunicipality of Imus, Cavite Office of The MAYOR July 14, 2016Richard RLAinda não há avaliações
- Letter To MayorDocumento1 páginaLetter To MayorRichard RLAinda não há avaliações
- Daily CensusDocumento12 páginasDaily CensusRichard RLAinda não há avaliações
- Head Nursing FormDocumento2 páginasHead Nursing FormRichard RLAinda não há avaliações
- 1 Week NoticeDocumento1 página1 Week NoticeRichard RLAinda não há avaliações
- Concept Map Grand CaseDocumento1 páginaConcept Map Grand CaseRichard RLAinda não há avaliações
- Drugs Name 4Documento4 páginasDrugs Name 4Richard RLAinda não há avaliações
- Municipality of Imus, Cavite Office of The MAYOR July 14, 2016Documento2 páginasMunicipality of Imus, Cavite Office of The MAYOR July 14, 2016Richard RLAinda não há avaliações
- Princess Charlyne R. Mabborang November 10,2016 BSN-4ADocumento5 páginasPrincess Charlyne R. Mabborang November 10,2016 BSN-4ARichard RLAinda não há avaliações
- Richard Legaspi Crohn's DiseaseDocumento12 páginasRichard Legaspi Crohn's DiseaseRichard RLAinda não há avaliações
- Osmun Icu LFD 9-1-2016Documento1 páginaOsmun Icu LFD 9-1-2016Richard RLAinda não há avaliações
- Resume Cover Letter NursingDocumento1 páginaResume Cover Letter NursingRichard RLAinda não há avaliações
- Drugs Name 4Documento4 páginasDrugs Name 4Richard RLAinda não há avaliações
- 1 Week NoticeDocumento1 página1 Week NoticeRichard RLAinda não há avaliações
- To Nurses. Nurses Can Give Advice and Can Impart KnoDocumento1 páginaTo Nurses. Nurses Can Give Advice and Can Impart KnoRichard RLAinda não há avaliações
- QuestionnaireDocumento8 páginasQuestionnaireRichard RLAinda não há avaliações
- Zika Virus Thesis CHAP-1-2-3 8-26-16Documento43 páginasZika Virus Thesis CHAP-1-2-3 8-26-16Richard RL100% (3)
- Hemorrhoid Case StudyDocumento13 páginasHemorrhoid Case StudyRichard RLAinda não há avaliações
- Nursing Journal FinalDocumento1 páginaNursing Journal FinalRichard RLAinda não há avaliações
- BSN 2-A field trip to kidney center and home for disabledDocumento1 páginaBSN 2-A field trip to kidney center and home for disabledRichard RLAinda não há avaliações
- BSN 2-A field trip to kidney center and home for disabledDocumento1 páginaBSN 2-A field trip to kidney center and home for disabledRichard RLAinda não há avaliações
- Resume of Avegale S. Javillonar seeking career opportunitiesDocumento1 páginaResume of Avegale S. Javillonar seeking career opportunitiesRichard RLAinda não há avaliações
- BSN 2-A field trip to kidney center and home for disabledDocumento1 páginaBSN 2-A field trip to kidney center and home for disabledRichard RLAinda não há avaliações
- Dermatologic PharmacologyDocumento88 páginasDermatologic PharmacologyAlunaficha Melody KiraniaAinda não há avaliações
- Respiratory Physiology MCQsDocumento25 páginasRespiratory Physiology MCQssk100% (5)
- Fundamental Rationale and AnswersDocumento237 páginasFundamental Rationale and AnswersNorminaKiramAkmadAinda não há avaliações
- DTL Implants-ABDocumento2 páginasDTL Implants-ABananthAinda não há avaliações
- Life Threatening Causes of Pain Abdomen / Acute PancreatitisDocumento27 páginasLife Threatening Causes of Pain Abdomen / Acute PancreatitisDr. Rajesh Padhi100% (1)
- Skill Checklist Applying An Extremity RestraintDocumento2 páginasSkill Checklist Applying An Extremity RestraintAsep BageurAinda não há avaliações
- Dosages and SolutionDocumento68 páginasDosages and SolutionRuan MarchessaAinda não há avaliações
- Ovarian Cyst Treatment 1Documento5 páginasOvarian Cyst Treatment 1Helcio FerreiraAinda não há avaliações
- Ischemic optic neuropathy: causes, diagnosis, and managementDocumento10 páginasIschemic optic neuropathy: causes, diagnosis, and managementScerbatiuc CristinaAinda não há avaliações
- Stroke Reports Following Covid VaccineDocumento9 páginasStroke Reports Following Covid VaccineJosh Singer100% (2)
- SBRT Pulmon Presentacion - TIPs and TricksDocumento197 páginasSBRT Pulmon Presentacion - TIPs and TricksDavid GarciaAinda não há avaliações
- THYROID PROFILE REPORTDocumento7 páginasTHYROID PROFILE REPORTSaujanyaSengarAinda não há avaliações
- Icmr PPT (1) VidhiDocumento32 páginasIcmr PPT (1) VidhiVidhi GuptaAinda não há avaliações
- Edukasi Kesehatan di Bulan RamadhanDocumento10 páginasEdukasi Kesehatan di Bulan RamadhanDiki MulyadiAinda não há avaliações
- 7th Lecture Physics of Cardiovascular System1Documento12 páginas7th Lecture Physics of Cardiovascular System1Asfoor gake1Ainda não há avaliações
- Efficacy of Topical Tacrolimus 0.05% Suspension in Steroid-Resistant and Steroid-Dependent Vernal KeratoconjunctivitisDocumento11 páginasEfficacy of Topical Tacrolimus 0.05% Suspension in Steroid-Resistant and Steroid-Dependent Vernal KeratoconjunctivitiselhambabaieAinda não há avaliações
- Emedica MRCGP AKT Curriculum ChecklistDocumento42 páginasEmedica MRCGP AKT Curriculum ChecklistSana Mustafa100% (1)
- Ocd, Normal IntrusionsDocumento3 páginasOcd, Normal Intrusionscitalac69Ainda não há avaliações
- G-CFA Instructor Tab 6-2 Handout 2 Sample Adequate Nursing Care Plan-R6Documento2 páginasG-CFA Instructor Tab 6-2 Handout 2 Sample Adequate Nursing Care Plan-R6SriMathi Kasi Malini ArmugamAinda não há avaliações
- 2022 - CCR8 Treg Cells in Tumor Tissues With Long-Lasting MemoryDocumento12 páginas2022 - CCR8 Treg Cells in Tumor Tissues With Long-Lasting Memory1262615286Ainda não há avaliações
- Eye - Blur Vision Part IIDocumento56 páginasEye - Blur Vision Part IIStaporn Kasemsripitak100% (2)
- Internship Manual 20-21 PDFDocumento19 páginasInternship Manual 20-21 PDFMsalik1Ainda não há avaliações
- Immunology and Serology Lecture HistoryDocumento3 páginasImmunology and Serology Lecture HistoryLyka ReyesAinda não há avaliações
- Very Early Signs and SymptomsDocumento3 páginasVery Early Signs and SymptomsMichelle TeodoroAinda não há avaliações
- TLE Beauty Care Pretest Grade910Documento4 páginasTLE Beauty Care Pretest Grade910KENT REEVE ROSALAinda não há avaliações
- (Endocrinology) Paolo Vitti, Laszlo Hegedus (Eds.) - Thyroid Diseases - Pathogenesis, Diagnosis and Treatment-Springer International Publishing PDFDocumento478 páginas(Endocrinology) Paolo Vitti, Laszlo Hegedus (Eds.) - Thyroid Diseases - Pathogenesis, Diagnosis and Treatment-Springer International Publishing PDFOktahermoniza TanjungAinda não há avaliações
- The Longevity Diet: Discover The New Science Behind Stem Cell Activation and Regeneration To Slow Aging, Fight Disease, and Optimize Weight - Valter LongoDocumento5 páginasThe Longevity Diet: Discover The New Science Behind Stem Cell Activation and Regeneration To Slow Aging, Fight Disease, and Optimize Weight - Valter Longozyrybosi20% (5)
- Slit Skin SmearDocumento12 páginasSlit Skin SmearRam ManoharAinda não há avaliações
- Basic First Aid Course OverviewDocumento10 páginasBasic First Aid Course OverviewHariz Bin Hussien GmanabilangAinda não há avaliações
- Advances in PsoriasisDocumento415 páginasAdvances in PsoriasisMantas GrigonisAinda não há avaliações