Escolar Documentos
Profissional Documentos
Cultura Documentos
Incentive Spirometers
Enviado por
mlbonthelineDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Incentive Spirometers
Enviado por
mlbonthelineDireitos autorais:
Formatos disponíveis
SARASOTA MEMORIAL HOSPITAL
NURSING PROCEDURE
TITLE:
ISSUED
FOR:
INCENTIVE SPIROMETRY
(equ02)
Nursing
7/88
DATE:
11/05
REVIEWED:
1 of 3
PAGES:
RESPONSIBILITY:
RN, LPN, RT
* PCA, Patient Care Specialist
PURPOSE:
To provide a procedure for the delivery of incentive spirometry.
KNOWLEDGE BASE:
1. Incentive spirometry uses a breathing device to encourage
the patient to achieve maximal ventilation. The device
measures respiratory flow or respiratory volume and
induces the patient to take a deep breath and hold it for
several seconds. This exercise establishes alveolar
hyperinflation for a longer time than is possible with a
normal deep breath, thus preventing and reversing the
alveolar collapse that produces atelectasis and
pneumonitis.
2. Incentive spirometry benefits the patient on prolonged bed
rest, especially the postoperative patient who may regain
his normal respiratory pattern slowly because of such
predisposing factors as: abdominal or thoracic surgery,
advanced age, inactivity, obesity, smoking, and a
decreased ability to cough effectively and expel lung
secretions.
3. Incentive spirometry requires a physicians order. The
order will be processed according to established
procedures.
PATIENT EDUCATION:
1. Explain the procedure to the patient, making sure he/she
understands the importance of performing this exercise
regularly to maintain alveolar inflation and help prevent lung
collapse and pneumonia.
2. When possible and appropriate, include incentive
spirometry in preoperative teaching.
INDICATIONS:
To prevent atelectasis and mobilize secretions through deep
inspiratory maneuvers and end-inspiratory breath-holding.
TITLE:
INCENTIVE SPIROMETRY
(equ02)
PAGE: 2 of 3
EQUIPMENT:
1.
2.
3.
4.
Incentive Spirometer (Central Service Cart)
Tissues
Gloves, as appropriate
Noseclips (optional)
PROCEDURE:
1. Read and follow the manufacturers instructions for
spirometer set up and operation. Connect the breathing
tube to the spirometer. The tube and mouthpiece will be
sterile on the first use and clean on subsequent uses.
2. Assist the patient to a comfortable sitting or semi-Fowlers
position to promote optimal lung expansion. If the patient is
unable to assume or maintain this position, perform the
procedure in any position as long as the device remains
upright. Tilting an incentive spirometer decreases the
required patient effort and reduces the exercises
effectiveness.
3. The patients lungs may be auscultated by the nurse or RT
to provide a baseline for comparison with post-treatment
auscultation.
4. Instruct the patient to insert the mouthpiece and to close
his/her lips tightly around it in order to obtain a tight seal.
Noseclips may be used, if necessary.
5. Instruct and encourage the patient to inhale maximally,
following the directions with the incentive spirometer to
maintain inspiratory flow at desired level.
6. Instruct the patient to hold his/her breath for 2 to 3 seconds
and then exhale slowly through the nose.
7. Two to four maximal inspirations should be done per minute
for a period of 5 to 8 minutes.
a. If the patient exhibits light-headedness during the
procedure, stop and allow the patient to rest before
continuing.
b. Stress the importance of patient involvement and the
self-help concept. Involve family.
c. To be continued even after discharge.
d. Procedure should be performed at least every hour
while awake.
8. Instruct the patient to cough to remove accumulated
secretions. Patients should use a small pillow for splinting
chest incisions.
9.
If soiled, wash the mouthpiece in warm water and shake it
dry. Avoid immersing the spirometer itself because this
enhances bacterial growth and impairs the internal filters
effectiveness in preventing inhalation of extraneous
TITLE:
INCENTIVE SPIROMETRY
(equ02)
PROCEDURE (contd):
PAGE: 3 of 3
material.
10. Label the spirometer with the patients name to avoid
inadvertent use by another patient.
11. Provide the patient with the Instructions for Use that are
in the kit. These are helpful as information available in
French and Spanish also.
DOCUMENTATION:
Nursing Reassessment Flowsheet in SCM/CareVISION or
CareVue: Document incentive spriometer frequency and
incentive spirometer volume range.
Education Record: Document the initial procedure, patient
education and patient response. Document any subsequent
patient education, patient response and any other pertinent
information, as appropriate.
REFERENCE(S):
Buchfa, V. (2000). Incentive Spirometry. Nursing Procedure:
Third Edition. (pp 474-476). Springhouse, PA: Springhouse
Corporation
Archer, E. et al., Nursing Procedures and Protocols. (2003).
Lippincott Williams and Wilkins. Philadelphia: PA.
REVIEWING AUTHOR(S):
Cindy Taylor, RN, BSN, CPS, Cardiac
Mark Pellman, RRT, Team Leader, Resp. Therapy
APPROVAL(S):
Nursing Standards & Practice Council 9/1/05
Respiratory Management, 8/26/05
Você também pode gostar
- Incentive SpirometryDocumento6 páginasIncentive SpirometryRiza Angela BarazanAinda não há avaliações
- Nursing Clinical Guide for PreeclampsiaDocumento2 páginasNursing Clinical Guide for PreeclampsiaDummy AccountAinda não há avaliações
- Administering Enema POWERPOINT GIVING ENEMA TO PATIENT, FOR PATIENT WITH GASTROINTESTINAL DISORDERS .. LECTURES, PRINCIPLES AND PROCEDURESDocumento14 páginasAdministering Enema POWERPOINT GIVING ENEMA TO PATIENT, FOR PATIENT WITH GASTROINTESTINAL DISORDERS .. LECTURES, PRINCIPLES AND PROCEDURESPb0% (1)
- ARTHROCENTESISDocumento2 páginasARTHROCENTESISJairene Dave Martinez CambalonAinda não há avaliações
- Endotracheal Tube SuctioningDocumento5 páginasEndotracheal Tube SuctioningArlene DalisayAinda não há avaliações
- Discharge Plan CapDocumento3 páginasDischarge Plan Capalexander abasAinda não há avaliações
- Percutaneous Transhepatic CholangiographyDocumento3 páginasPercutaneous Transhepatic CholangiographyRonel UsitaAinda não há avaliações
- German MeaslesDocumento8 páginasGerman MeaslesYdynn Parejas GavinaAinda não há avaliações
- NCP FeuDocumento2 páginasNCP FeuFejlean Angelica AntineoAinda não há avaliações
- Oropharyngeal and Nasotracheal SuctioningDocumento2 páginasOropharyngeal and Nasotracheal SuctioningZoren CayananAinda não há avaliações
- Code Blue in HospitalDocumento7 páginasCode Blue in HospitalJu Lie AnnAinda não há avaliações
- Leopold S ManeuverDocumento5 páginasLeopold S Maneuverastak ghisingAinda não há avaliações
- Nasopharyngeal Suctioning GuideDocumento6 páginasNasopharyngeal Suctioning GuideJmarie Brillantes PopiocoAinda não há avaliações
- PEG Feeding Procedure GuideDocumento3 páginasPEG Feeding Procedure GuideAlyzza Dagoy100% (1)
- Funda Saved Ms2003Documento103 páginasFunda Saved Ms2003June DumdumayaAinda não há avaliações
- NGT Feeding: by Group 2Documento25 páginasNGT Feeding: by Group 2karl montano100% (1)
- Sudaria Ivy G. AnswerKeysDocumento25 páginasSudaria Ivy G. AnswerKeysDeinielle Magdangal RomeroAinda não há avaliações
- MineDocumento3 páginasMineJM NelsonAinda não há avaliações
- NG Tube Removal ProcedureDocumento2 páginasNG Tube Removal Procedurejoel david knda mjAinda não há avaliações
- Exploratory Appendectomy Procedure DetailsDocumento11 páginasExploratory Appendectomy Procedure DetailsJessica Christine Datuin GustiloAinda não há avaliações
- Sop and Competencies For NG InsertionDocumento4 páginasSop and Competencies For NG InsertionReza ShinodaAinda não há avaliações
- Unit 6. Roles and Functions of A Nurse in The Delivery of Care To A Sick ChildDocumento9 páginasUnit 6. Roles and Functions of A Nurse in The Delivery of Care To A Sick ChildMarlon Glorioso IIAinda não há avaliações
- Skill Performance Evaluation - Measuring Intake and OutputDocumento2 páginasSkill Performance Evaluation - Measuring Intake and OutputLemuel Que100% (1)
- NCP BMDocumento1 páginaNCP BMSourabh MehraAinda não há avaliações
- NGT Feeding ChecklistDocumento1 páginaNGT Feeding ChecklistJoycee BoAinda não há avaliações
- Bernard Narrative Evaluation ReportDocumento4 páginasBernard Narrative Evaluation ReportAldwin Compra QuiñoAinda não há avaliações
- Oral and Nasal Suctioning Procedure GuidelinesDocumento4 páginasOral and Nasal Suctioning Procedure GuidelinesKimberly Ann Santos100% (1)
- Chapter IiDocumento37 páginasChapter Iicoosa liquors100% (1)
- Inserting IV Cannula Utilizing A DummyDocumento6 páginasInserting IV Cannula Utilizing A Dummykhaye_corpusAinda não há avaliações
- Incentive Spirometry 1.1. DefinitionDocumento4 páginasIncentive Spirometry 1.1. DefinitionCristine Mae Libarnes Jaudian100% (1)
- Nso AbdurasadDocumento4 páginasNso AbdurasadNader AbdurasadAinda não há avaliações
- NCPDocumento2 páginasNCPVince John SevillaAinda não há avaliações
- 2.mod Geron 2 DocumentationDocumento43 páginas2.mod Geron 2 Documentationnot your medz duran100% (1)
- QuestionDocumento6 páginasQuestiontravelbeeAinda não há avaliações
- Qualifications of Board of NursingDocumento11 páginasQualifications of Board of NursingKram PerezAinda não há avaliações
- Nursing Assessment, Planning, Implementation and EvaluationDocumento2 páginasNursing Assessment, Planning, Implementation and EvaluationDiana MuañaAinda não há avaliações
- Angiotensin Converting Enzyme (ACE) InhibitorsDocumento4 páginasAngiotensin Converting Enzyme (ACE) InhibitorsPutri Mulia HasibuanAinda não há avaliações
- Silvestri001100Documento55 páginasSilvestri001100lilchibabyAinda não há avaliações
- Checklist On Internal ExaminationDocumento2 páginasChecklist On Internal ExaminationMhel MG100% (1)
- Oropharyngeal and Nasopharyngeal SuctioningDocumento2 páginasOropharyngeal and Nasopharyngeal SuctioningAlana Caballero100% (1)
- Cast CareDocumento1 páginaCast CareCarmelita SaltAinda não há avaliações
- CEUFast Infection Control and Barrier PrecautionsDocumento90 páginasCEUFast Infection Control and Barrier PrecautionsMeg GalauranAinda não há avaliações
- SchistosomiasisDocumento5 páginasSchistosomiasisBryan TarrobalAinda não há avaliações
- PATENTE - Worksheet - Nasogastric Tube Insertion, Feeding, and RemovalDocumento11 páginasPATENTE - Worksheet - Nasogastric Tube Insertion, Feeding, and RemovalSelwynVillamorPatenteAinda não há avaliações
- NSO Gastric LavageDocumento3 páginasNSO Gastric Lavagetry dokkAinda não há avaliações
- Checking The Vital SignsDocumento5 páginasChecking The Vital SignsRoger ViloAinda não há avaliações
- NCP Micu Hascvd Cad - RioDocumento5 páginasNCP Micu Hascvd Cad - RioRio BonifacioAinda não há avaliações
- ThyroidectomyDocumento11 páginasThyroidectomySherina W. EddingAinda não há avaliações
- Tracheostomy CareDocumento3 páginasTracheostomy CareKate Chavez100% (1)
- Sanaani Nur Hathi M. Nso Jugular Venous Oximetry Staff Nurse 1Documento7 páginasSanaani Nur Hathi M. Nso Jugular Venous Oximetry Staff Nurse 1Nur SanaaniAinda não há avaliações
- IV Meds in Volumetric Set C RationaleDocumento2 páginasIV Meds in Volumetric Set C RationalePascal Marie IzhaqAinda não há avaliações
- Nursing Care PlanDocumento3 páginasNursing Care PlanMarielle SorianoAinda não há avaliações
- Chest Tube Reflective EssayDocumento2 páginasChest Tube Reflective EssayAnjae GariandoAinda não há avaliações
- Venn Diagram (Nursing Process vs. Education Process)Documento2 páginasVenn Diagram (Nursing Process vs. Education Process)Maze Jamela Peñaojas ManlogonAinda não há avaliações
- Community Health Nursing Competency Workbook 1: Home VisitDocumento5 páginasCommunity Health Nursing Competency Workbook 1: Home VisitJulianne B. Dela CruzAinda não há avaliações
- Bronchial Asthma Case StudyDocumento52 páginasBronchial Asthma Case StudyYang ChimsAinda não há avaliações
- Water Sealed DrainageDocumento2 páginasWater Sealed DrainagefairwoodsAinda não há avaliações
- Incentive Spirometry (Revised)Documento4 páginasIncentive Spirometry (Revised)Myangel LoiseAinda não há avaliações
- Module 2 - Incentive Spirometry (Student)Documento4 páginasModule 2 - Incentive Spirometry (Student)febie pacheco0% (1)
- Incentive SpirometryDocumento5 páginasIncentive Spirometryrachelmores12Ainda não há avaliações
- Nursing and Midwifery Board FAQ Internationally Qualified Nurses and MidwivesDocumento4 páginasNursing and Midwifery Board FAQ Internationally Qualified Nurses and MidwivesmlbonthelineAinda não há avaliações
- 01Documento3 páginas01mlbonthelineAinda não há avaliações
- Nursing and Midwifery Board FAQ IQNM Criterion 8 Registered NurseDocumento2 páginasNursing and Midwifery Board FAQ IQNM Criterion 8 Registered NursemlbonthelineAinda não há avaliações
- Bcit-Ices Ices ApplicationDocumento8 páginasBcit-Ices Ices ApplicationmlbonthelineAinda não há avaliações
- TracerStudyTheAntoninusJournal 2 PDFDocumento28 páginasTracerStudyTheAntoninusJournal 2 PDFmlbonthelineAinda não há avaliações
- School Codes As of 09-10-2012 PDFDocumento88 páginasSchool Codes As of 09-10-2012 PDFmlbonthelineAinda não há avaliações
- 6th International Symposium On Technology For SustainabilityDocumento1 página6th International Symposium On Technology For SustainabilitymlbonthelineAinda não há avaliações
- Japan VIsa Application SampleDocumento2 páginasJapan VIsa Application SampleBudi Utami Wibawani80% (5)
- ERN Assessment Manual For Applicants 9. Sample Letter of National Endorsement For Healthcare ProvidersDocumento3 páginasERN Assessment Manual For Applicants 9. Sample Letter of National Endorsement For Healthcare ProvidersmlbonthelineAinda não há avaliações
- RadTech Performance of SchoolsDocumento4 páginasRadTech Performance of SchoolsPhilNewsXYZAinda não há avaliações
- Chapter 7: Critical ThinkingDocumento17 páginasChapter 7: Critical ThinkingmlbonthelineAinda não há avaliações
- Nurses' Application FormDocumento2 páginasNurses' Application FormTricia GervacioAinda não há avaliações
- June 2016 Nurse Licensure Examination: Seq. NODocumento17 páginasJune 2016 Nurse Licensure Examination: Seq. NOTheSummitExpressAinda não há avaliações
- June 2007 NursestopDocumento22 páginasJune 2007 Nursestopmaryannrichelle100% (3)
- RadTech Performance of SchoolsDocumento4 páginasRadTech Performance of SchoolsPhilNewsXYZAinda não há avaliações
- Top Performing Schools in The June 2016 Nurse Licensure ExaminationDocumento3 páginasTop Performing Schools in The June 2016 Nurse Licensure ExaminationmlbonthelineAinda não há avaliações
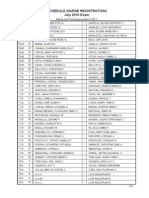
- REVISED Initial Registration Schedule of Nurses - July 2010 (Manila and Pampanga Passers Only)Documento2 páginasREVISED Initial Registration Schedule of Nurses - July 2010 (Manila and Pampanga Passers Only)Coolbuster.NetAinda não há avaliações
- June 2016 Nurse Licensure Examination: Seq. NODocumento17 páginasJune 2016 Nurse Licensure Examination: Seq. NOTheSummitExpressAinda não há avaliações
- Nurs0616se eDocumento248 páginasNurs0616se eTheSummitExpressAinda não há avaliações
- Top Performing Schools in The June 2016 Nurse Licensure ExaminationDocumento3 páginasTop Performing Schools in The June 2016 Nurse Licensure ExaminationmlbonthelineAinda não há avaliações
- Nurs0616se eDocumento248 páginasNurs0616se eTheSummitExpressAinda não há avaliações
- CMO No.5 S. 2008 P1-110Documento110 páginasCMO No.5 S. 2008 P1-110Lanz LlnsAinda não há avaliações
- May 2015 NLE Performance of SchoolsDocumento18 páginasMay 2015 NLE Performance of SchoolsCoolbuster.Net100% (1)
- Professional Regulation Commission: Republic of The Philippines ManilaDocumento2 páginasProfessional Regulation Commission: Republic of The Philippines ManilaNonoyTaclinoAinda não há avaliações
- Dorothy Johnson (Report)Documento24 páginasDorothy Johnson (Report)mlbonthelineAinda não há avaliações
- Nursing Board Exam 2015 ResultsDocumento195 páginasNursing Board Exam 2015 ResultsGMA News Online100% (2)
- List of Successful Examinees in The May 2014 Nurse Licensure ExaminationDocumento225 páginasList of Successful Examinees in The May 2014 Nurse Licensure ExaminationofwwatchAinda não há avaliações
- List of Top Notchers NLE 2015Documento5 páginasList of Top Notchers NLE 2015PhilNewsXYZAinda não há avaliações
- List of Successful Examinees in The May 2014 Nurse Licensure ExaminationDocumento225 páginasList of Successful Examinees in The May 2014 Nurse Licensure ExaminationofwwatchAinda não há avaliações
- Work Method Statement ToolkitDocumento16 páginasWork Method Statement ToolkitKocic BalicevacAinda não há avaliações
- Folleto - Ing - Leoni 2Documento2 páginasFolleto - Ing - Leoni 2Johnny CotzitoAinda não há avaliações
- Acute respiratory failure pathophysiologyDocumento14 páginasAcute respiratory failure pathophysiologyMahmoud KittAinda não há avaliações
- Coagulopathy in Cardiac Surgery1Documento63 páginasCoagulopathy in Cardiac Surgery1Mohammed Abdul ShafiAinda não há avaliações
- PATH-Fit Course SyllabusDocumento7 páginasPATH-Fit Course SyllabusLOUISE DOROTHY PARAISO100% (1)
- Medical Surgical Nursing Test VIIDocumento7 páginasMedical Surgical Nursing Test VIIclobregasAinda não há avaliações
- EkgDocumento67 páginasEkgFendi Rafif Dad'sAinda não há avaliações
- Howard S. Friedman - The Oxford Handbook of Health Psychology (2011, Oxford University Press)Documento935 páginasHoward S. Friedman - The Oxford Handbook of Health Psychology (2011, Oxford University Press)Emill Jayson Caypuno100% (9)
- Vaccination ChartDocumento3 páginasVaccination ChartszawAinda não há avaliações
- Community, Engagement, Solidarity and CitizenshipDocumento14 páginasCommunity, Engagement, Solidarity and CitizenshipCyrrha Fe QuesabaAinda não há avaliações
- Material Safety Data Sheet (MSDS)Documento22 páginasMaterial Safety Data Sheet (MSDS)OladimejiAinda não há avaliações
- Plan Canguro 2020Documento7 páginasPlan Canguro 2020luzhelanapaezAinda não há avaliações
- NICU - Policies, Procedures and ProtocolsDocumento190 páginasNICU - Policies, Procedures and Protocolskrishnasree100% (3)
- Obesity AdimeDocumento2 páginasObesity Adimeapi-3008826400% (1)
- POULTRY FARM OPERATION AND LAB TECHNIQUES REPORTDocumento30 páginasPOULTRY FARM OPERATION AND LAB TECHNIQUES REPORTBakhtawarAinda não há avaliações
- DD 1 2 Practice Ryder CookDocumento3 páginasDD 1 2 Practice Ryder CookJessica IreneAinda não há avaliações
- The Role of Orlistat in Treatment of ObesityDocumento12 páginasThe Role of Orlistat in Treatment of ObesityNoor786110Ainda não há avaliações
- Bladder TrainingDocumento3 páginasBladder TrainingJihan AisyAinda não há avaliações
- Personal Protective Grounding - Training PresentationDocumento31 páginasPersonal Protective Grounding - Training PresentationIrfan UllahAinda não há avaliações
- (Transgênicos) Le Principe de Précaution. Rapport Au Premier Ministre Présenté Par Philippe Kourilsky (Collège de France) & Geneviève Viney (Université Paris I) - 1999.Documento189 páginas(Transgênicos) Le Principe de Précaution. Rapport Au Premier Ministre Présenté Par Philippe Kourilsky (Collège de France) & Geneviève Viney (Université Paris I) - 1999.filosophAinda não há avaliações
- ICS Course Introduces Incident Management SystemDocumento22 páginasICS Course Introduces Incident Management SystemMessias PortoAinda não há avaliações
- Develop Maximum Strength While Staying Fresh For BoxingDocumento3 páginasDevelop Maximum Strength While Staying Fresh For Boxinggtlaau50% (2)
- 11 Emergency Preparedness PlanDocumento6 páginas11 Emergency Preparedness PlanMAHESH SHAWAinda não há avaliações
- C-BSU - at Admission Requirement - 0Documento6 páginasC-BSU - at Admission Requirement - 0DanielleSarahCacheroAinda não há avaliações
- University of Rizal System Cainta Campus Ed1 Name: Chyryz Jewel D. Baldelomar Date: Nov. 5, 2020 PART 1 (50 PTS.)Documento3 páginasUniversity of Rizal System Cainta Campus Ed1 Name: Chyryz Jewel D. Baldelomar Date: Nov. 5, 2020 PART 1 (50 PTS.)Chyryz Jewel BaldelomarAinda não há avaliações
- "The Life and Times of Mr. Nicholls" Michael George Nicholls-Pierce Liberal Studies LIBS 390-01 Intellectual AutobiographyDocumento5 páginas"The Life and Times of Mr. Nicholls" Michael George Nicholls-Pierce Liberal Studies LIBS 390-01 Intellectual Autobiographyapi-573024890Ainda não há avaliações
- 3 2 24 791 PDFDocumento4 páginas3 2 24 791 PDFKeerti PathakAinda não há avaliações
- Nursing Care Plan: Assessment Nursing Diagnosis Planning Intervention EvaluationDocumento2 páginasNursing Care Plan: Assessment Nursing Diagnosis Planning Intervention EvaluationCristoper BodionganAinda não há avaliações
- 2018 CaciDocumento3.268 páginas2018 CaciLiam MaloneAinda não há avaliações
- Observer Application: General Personal InformationDocumento3 páginasObserver Application: General Personal InformationDragomir IsabellaAinda não há avaliações