Escolar Documentos
Profissional Documentos
Cultura Documentos
ESBL
Enviado por
Jonathan WelchDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
ESBL
Enviado por
Jonathan WelchDireitos autorais:
Formatos disponíveis
Available online at
http://jurnal.permi.or.id/index.php/mioline
DOI: 10.5454/mi.9.4.2
MICROBIOLOGY
INDONESIA
ISSN 1978-3477, eISSN 2087-8575
Vol.9, No.4, December 2015, p 150-156
Antibiotic Use Is Not a Risk Factor of Infection by Extended-Spectrum
Beta-Lactamase Producing Bacteria in Dr. Soetomo Hospital Surabaya
1
NADHYA NUR FITRI *, MUSOFA RUSLI , AND MANIK RETNO WAHYUNITISARI
1
Departement of Medical Microbiology, Faculty of Medicine, Universitas Airlangga,
Jalan Mayjen Prof. Dr. Moestopo 47 Surabaya 60131, Indonesia;
2
Departement of Internal Medicine, Faculty of Medicine, Universitas Airlangga,
Jalan Mayjen Prof. Dr. Moestopo 47 Surabaya 60131, Indonesia
Infection by Extended-Spectrum Beta-Lactamase (ESBL) producing bacteria confers a major challenge for
clinicians due to limited treatment options and poor prognosis. Inappropriate antibiotic use is thought to cause the
emergence of this resistant strain through selective pressure mechanisms. This study aims to describe the
proportion of ESBL-producing bacteria and characteristics of patients with ESBL-producing bacterial infection,
and to analyze the risk factors of infection by ESBL-producing bacteria in Dr. Soetomo Hospital, Surabaya. A
cross-sectional study was conducted on medical records of inpatients of Internal Medicine Ward of Dr. Soetomo
Hospital. Samples were classified into ESBL-positive or ESBL-negative groups. Demographic data, clinical
data and previous antibiotic use of 66 samples (33 in each group) were retrospectively obtained. As many as 30
patients (45.5%) were male. Mean age of patients in the ESBL-positive and negative group were 53.57 (16.77)
and 54.27 (14.88) years, respectively (p>0.05). The median pre-infection length of stay was 4 and 3 days for
ESBL-positive and negative group, respectively (p>0.05). Type 2 diabetes mellitus was the most common
comorbid disease (33.3%). The most frequent bacteria obtained from clinical isolates was Escherichia coli
(49.3%). Proportion of ESBL producers amongst E.coli and K. pneumoniae isolates were 75% and 38.5%,
respectively. The most frequently prescribed empirical antibiotic was ceftriaxone. None of the antibiotic used
were risk factors for infection by ESBL-producing bacteria. Although none of the assessed variables were risk
factors for ESBL-infection was discovered, this study finds a significantly larger proportion of ESBL-E. coli
compared to non-ESBL producing E. coli. Further studies should include larger sample size and quantitatively
measured antibiotic use.
Key words: antibiotic resistance, antibiotic use, ESBL, Escherichia coli
Infeksi oleh bakteri penghasil Extended-Spectrum Beta-Lactamase (ESBL) menjadi sebuah tantangan bagi
klinisi karena terbatasnya pilihan terapi antibiotic dan prognosis pasien yang buruk. Penggunaan antibiotik
secara tidak tepat diduga menyebabkan berkembangnya melalui tekanan seleksi. Penelitian ini bertujuan untuk
mendeskripsikan prevalensi bakteri penghasil ESBL dan karakteristik pasien yang terinfeksi oleh bakteri
penghasil ESBL serta menganalisis faktor risiko infeksi oleh bakteri penghasil ESBL di RSUD Dr. Soetomo,
Surabaya. Sebuah studi cross-sectional dilakukan menggunakan rakam medic pasien rawat inap di instalasi
rawat inap medik penyakit dalam RSUD. Dr. Soetomo, Surabaya. Sampel dikelompokkan menjadi kelompok
ESBL-positif dan ESBL-negatif. Data demografis, klinis dan riwayat penggunaan antibiotik dari 66 sampel (33
sampel pada masing-masing kelompok) dilihat secara retrospektif. Sebanyak 30 (45.5%) pasien berjenis
kelamin laki-laki. Rata-rata usia pada kelompok ESBL-positif ialah 53.57(16.77) tahun, sedangkan pada
kelompok ESBL-negatif ialah54.27 (14.88) tahun (p>0.05). Nilai median lama rawat inap sebelum infeksi pada
kelompok ESBL-positif dan ESBL-negatif masing-masing 4 dan 3 hari (p>0.05). Penyakit komorbid tersering
yang dijumpai pada pasien adalah diabetes mellitus (33.3%). Bakteri yang terbanyak didapatkan pada isolat
klinis ialah Escherichia coli (49.3%). Prevalensi E. coli penghasil ESBL adalah 75% dan 38.5% pada Klebsiella
pneumoniae. Antibiotik yang paling sering diberikan pada pasien ialah cephalosporin generasi-3 (ceftriaxon).
Tidak didapatkan hubungan antara penggunaan antibiotik dengan infeksi oleh bakteri penghasil ESBL. Isolat E.
coli yang menghasilkan ESBL secara signifikan lebih banyak daripada isolat yang tidak menghasilkan ESBL.
Penelitian berikutnya diharapkan dapat melibatkan sampel yang lebih besar serta mengukur penggunaan
antibiotik secara kuantitatif.
Kata kunci: ESBL, Escherichia coli, penggunaan antibiotik, resistensi antibiotik.
Extended-Spectrum Beta-Lactamase (ESBL) is a
group of enzymes responsible for the resistance of
gram negative bacteria towards beta-lactam
*Corresponding author; Phone: +62-31-5020251, Fax: +6231-5022472; Email: nadhya.nf@gmail.com
antibiotics. These enzymes are mainly produced by
members of the gram negative family
Enterobacteriaceae such as Escherichia coli and
Klebsiella pneumoniae, but other species such as
Acinetobacter baumanii and Pseudomonas aeruginosa
Volume 9, 2015
are also known to produce ESBLs (Dhillon and Clark
2012). ESBLs are able to hydrolize and inactivate betalactam antibiotics, including all penicillins,
cephalosporin, and aztreonam, but has no activity
against cephamycin and carbapenem (Tham 2012).
This strain also commonly shows co-resistance
towards fluoroquinolones and aminoglycosides,
therefore limiting treatment options (Kaya et al. 2013).
Limited susceptible antibiotic options have become the
main challenge in treating infection by ESBL
producing bacteria, causing an increase in medical
costs, morbidity and mortality (Tumbarello et al.
2006).
The prevalence of ESBL producing bacteria varies
among countries; however, an increasing trend is
reported (Shaikh et al. 2015). The prevalence of ESBLproducing bacteria could be as low as 7.5% in North
America to as high as 22% in the Asia-Pacific region
(Dhillon and Clark 2012). Hadi et al. (2013) reported
that the prevalence of ESBL-producing bacteria in
institutions participating in the AMRIN (Antimicrobial
Resistance in Indonesia: Prevalence and Prevention)
Study increased from 22% in 2010 to 53% in 2012.
One of the notorious risk factors for infection by
ESBL-producing bacteria is inappropriate antibiotic
use. Antibiotic use is thought to drive selection
pressure, eliminating susceptible bacteria and enabling
the growth of resistant bacteria (Wright 2010).
However, results obtained from previous studies vary
and analytical studies on this topic are still limited in
Indonesia. This study is conducted to describe the
proportion of ESBL-producing bacteria; the clinical
characteristics of patients with ESBL-producing
bacterial infection, and to analyze the risk factors of
infection by ESBL-producing bacteria in Dr. Soetomo
Hospital, Surabaya. This study is by far the most recent
analytical study on risk factors of infection by ESBL
producing bacteria in a tertiary hospital in Indonesia.
MATERIALS AND METHODS
Study Design and Population. This cross
sectional study involved medical records of patients
with bacterial infection hospitalized at the Internal
Medicine Ward of Dr. Soetomo Hospital, a tertiary
referral hospital in Surabaya, Indonesia. The inclusion
period was October 2014 to May 2015. The eligible
population consists of patients with a diagnosis of
bacterial infection from which clinical specimens have
been collected for bacterial identification and antibiotic
susceptibility testing at the Clinical Microbiology
Microbiol Indones
151
Laboratory of Dr. Soetomo Hospital. The minimum age
of patients included in the study was 18 years old.
Incomplete medical records were excluded. Samples
were selected consecutively and were classified into
two groups, ESBL-negative and ESBL-positive with a
1:1 ratio. Bacterial identification was conducted with
the MicrobactTM System (Medvet diagnostics,
Thebarton, Adelaide, Australia), ESBL-positive group
consisted of patients with confirmed bacterial
identification from clinical specimens, in which the
identified bacteria was confirmed as ESBL-producing,
while ESBL-negative group consisted of patients
infected by a non-ESBL-producing bacteria. ESBL
production by gram negative bacteria screening was
done with disk diffusion testing using cefotaxime or
ceftazidime based on reccomendations of the Clinical
and Laboratory Standards Institute (CLSI) guidelines
or by the BD Phoenix Automated Microbiology System
(BD Diagnostic Systems, Sparks, MD) machine used in
Clinical Microbiology Laboratory of Dr. Soetomo
Hospital.
Data Collection. Medical records were reviewed
to obtain necessary data. Studied variables were patient
age and sex; comorbid disease and length of hospital
stay (LOS) prior to infection; antibiotic use and the type
of clinical specimen collected. Antibiotic use was
defined as any class of antibiotic given to the patient
before date of clinical specimen collection, with a
minimum duration of antibiotic use of 48 h.
Statistical Analysis. Bivariate analysis on
categorical variables was performed with chi square
test or fisher's exact test when appropriate. Independent
samples T-test was used to analyze association of age
with infection by ESBL-producing bacteria.
Independent samples Mann Whitney U Test was used
to compare pre-infection length of hospital stay in the
ESBL-positive and ESBL-negative group. All
statistical analyses are significant at p<0.05; 95%
Confidence Interval. All statistical analysis was
conducted with SPSS version 20.
Ethical Clearance. The study protocol was
approved by the Medical Research Ethics Committee
of Dr. Soetomo Hospital, Surabaya, Indonesia [Komite
Etik Penelitian Kesehatan Rsud Dr. Soetomo] (Ethical
clearance approval number 135/Panke.KKE/II/2015).
RESULTS
Samples that met the inclusion criteria consisted of
66 medical records, 33 in each ESBL-positive and
ESBL-negative group. As many as 30 patients (45.5%)
Microbiol Indones
152 FITRI ET AL.
were male. Demographic and clinical characteristics of
samples are shown (Table 1). There are no significant
differences between the demographic characteristics of
the ESBL-positive and ESBL-negative group
(p>0.05). The most common comorbid diseases in
samples were type 2 diabetes mellitus and malignancy.
None of the comorbidities were found to be risk factors
of infection by ESBL-producing bacteria.
From the 66 patients, 73 clinical specimens were
positive for bacterial cultures. The majority of isolates
were from urinary specimens (63.01%) Other clinical
specimens obtained and ESBL production
characteristics are shown (Table 2).
From 73 bacterial isolates, the most common
species obtained was Escherichia coli (47.95%). From
the 33 ESBL-positive isolates, as many as 27 (81.8%)
isolates were Escherichia coli, five (15,2%) were
Klebsiella pneumonia and one (3%) was Enterobacter
aerogenes (Table 3). The number of ESBL-positive E.
coli is significantly larger than the number of ESBLnegative isolates (p=0.000). The proportion of ESBL-
producing isolates was 75% in Escherichia coli and
38.46% in Klebsiella pneumoniae.
Antibiotics used by patients were classified based
its classes, including cephalosporin, beta-lactam/beta
lactamase inhibitor, fluoroquinolones, and other types
of antibiotics. Patients with combination of antibiotics
is catagorized as those who receive more than one types
of antibiotic simultaneously. The most frequently
prescribed antibiotic is the third generation
cephalosporin, ceftriaxone.
Bivariate analysis of antibiotic uses and infections
by ESBL-producing bacteria shows that none of the
antibiotics were risk factors for infection by ESBLproducing bacteria (Table 4).
DISCUSSION
Infection by Extended-Spectrum Beta-Lactamase
producing bacteria has become a major challenge for
clinicians due to increasing prevalence, limited
antibiotic options, and poor prognosis. It is therefore
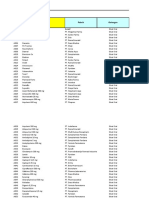
Table 1 Characteristics of samples
ESBL-positive
N=33
ESBL-negative
N=33
Gender (male)
12 (36.37%)
18 (54.54%)
0.138
Mean Age (SD)
53.57 (16.77)
54.27 (14.88)
0.859***
0.547**
Type 2 Diametes Mellitus
4 (12%)
7 (21%)
0.322
Diabetic nephropathy
6 (18%)
4 (12%)
0.492
Malignancy
8 (24%)
9 (27%)
0.778
Renal disease
6 (18%)
4 (12%)
0.492
Liver disease
1 (3%)
2 (6%)
1.000*
Rheumatic diseases
2 (6%)
1 (3%)
1.000*
Characteristics
Demographic
Median pre-infection LOS (days)
Comorbidities
*p value generated with Fisher's exact test
** p value generated with Independent samples Mann Whitney U Test
*** p value generated with Independent samples T Test
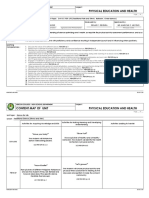
Table 2 Sources of clinical specimens
Clinical Specimens
ESBL
Urine
Sputum
Pus
Blood
ESBL +
26 (56.5%)
5 (41.7%)
1 (10%)
1 (20%)
ESBL -
20 (43.5%)
7 (68.3%)
9 (90%)
4 (80%)
Total
46 (100%)
12 (100%)
10 (100%)
5 (100%)
Microbiol Indones
Volume 9, 2015
Table 3 Distribution of bacteria in the ESBL-positive and ESBL-negative group
Bacteria
ESBL-positive
ESBL-negative
Total (%)
Escherichia coli
27
36 (49.3%)
Klebsiella pneumoniae
13 (17.8%)
Enterobacter aerogenes
3 (4.1%)
Enterobacter cloacae
1 (1.4%)
Proteus mirabilis
1 (1.4%)
Pseudomonas aeruginosa
6 (8.2%)
Acinetobacter baumanii
4 (5.5%)
Acinetobacter iwolfii
1 (1.4%)
Acinetobacter junii
1 (1.4%)
Cedecea lapagei
4 (5.5%)
Pasteurella mucocida
1 (1.4%)
Enterococcus faecalis
1 (1.4%)
Staphylococcus epidermidis
1 (1.4%)
Total
33
40
73 (100%)
Table 4 Analysis of antibiotic use in ESBL-positive and ESBL-negative group
ESBL-positive
ESBL-negative
RR
95%CI
(Lower-upper)
Cephalosporin
27
29
1.000
1.000
0.477-2.094
Ceftriaxone
25
25
1.000
1.000
0.570-1.756
Cefotaxime
1.000*
Cefixime
1.000*
Ceftazidime
1.000*
1.000
0.432-2.315
Beta Lactam-Beta
Lactamase Inhibitor
Amoxicillin-Clavulanic Acid
0.492*
1.000*
Cefoperazone-Sulbactam
1.000*
Fluoroquinolones
14
12
0.614
0.882
0.545-1.429
Ciprofloxacin
0.757
1.098
0.619-1.947
Levofloxacin
0.757
1.098
0.619-1.947
Meropenem
0.495*
Azithromycin
1.000*
Cotrimoxazole
1.000*
1.000
0.245-4.085
10
0.786
Antibiotic
Other classes
Combination of antibiotics
*p value generated with Fisher's exact test
*RR=relative risk
0.535-1.609
153
154 FITRI ET AL.
important to study the epidemiology and risk factors
for acquisition of this resistant strain to provide
adequate infection control in the hospital. A continuous
surveillance should also be conducted because the
prevalence usually changes overtime and differs in
each health centers.
Demographic characteristics of patients obtained
in this study showed that neither gender nor age were
significant risk factors for infection by ESBLproducing bacteria. However, other studies with larger
samples have found differing results. Older age is
found to be a risk factor in a multinational survey on
risk factors for infection by ESBL-producing bacteria
(OR=2.4; 95%CI=1.63.6) (Ben-Ami et al. 2009).
However, a contrasting result was found by Soraas et
al., (2013) that younger age was found to be a risk
factor for infection by ESBL-producing bacteria. Male
sex was found to be a risk factor for infection by ESBLproducing bacteria in a multinational survey (Ben-Ami
et al. 2009) (OR=2.5; 95%CI=1.7-3.7). Another study
by Tuon et al. (2010) in Brazil also reported similar
results (OR=2.62; 95%CI=1.16-5.93). However, Lee
et al. (2010) reported that female sex was a risk factor
for urinary tract infection by ESBL-producing bacteria
(OR=1.44; 95%CI=1.062-1.951; p= 0.019).
Length of hospital stay previous to infection is also
not a risk factor in this study. This is in concert with
studies by Tuon et al., (2011) and Huang et al., (2007)
which did not found that pre- infection length of
hospital stay as risk factors for infection by ESBLproducing bacteria. However a case control study in an
Australian tertiary hospital found that pre-infection
length of hospital stay was a risk factor for colonization
by ESBL producing bacteria (OR=1.2; 95%CI=1.01.3) (Osthoff et al. 2015).
None of the comorbidities were risk factors of
infection by ESBL-producing bacteria. However, Tuon
et al. (2010) reported that diabetes mellitus is a risk
factor for bacteremia by ESBL-producing K.
pneumoniae (p=0.043). Silva et al. (2006) reported in
his study that diabetes mellitus and malignancy are risk
factors for infection by ESBL producing bacteria
(p=0.02). Diabetes mellitus is a well-known risk factor
towards infection. Patients with diabetes have underoptimal immune system function, rendering them
susceptible towards infectious agents (Casqueiro et al.
2012).
An interesting finding in this study is that the
proportion of ESBL-producers among E. coli isolates
reaches 75%. This result differs from a study of
microbial resistance pattern in Dr. Soetomo Hospital
Microbiol Indones
by Kuntaman et al. (2006). The study reported
prevalence of ESBL-producers among E.coli was
34.86% and among K. pneumonia isolates reaches
35.35%. The study involved larger sample size and
isolates from wards other than Internal Medicine;
therefore it represented a larger population. Meanwhile
Pajariu et al. (2010) reported the prevalence of ESBLE. coli was 54.32% and ESBL-K. pneumonia was 50%
in Dr. Kariadi General Hospital, Semarang. Microbial
epidemiology usually varies among health institutes
and changes overtime. However, the small sample size
involved in this study might cause sampling bias and
the results might not accurately describe population
characteristics. Changes of bacterial population might
also be the case, however no report was available and
data on microbial pattern distribution is lacking.
Further surveillance is needed to confirm whether there
is a changing trend in bacterial distribution in Dr.
Soetomo Hospital.
ESBL gene may be harbored in the bacterial
chromosome or in plasmid. Severin et al. (2009)
reported that the most predominant ESBL isolate from
Dr. Soetomo Hospital was the producer of CTX-M-15,
of which the gene is most commonly harbored in
plasmid. Unfortunately, molecular ESBL analysis was
not conducted in this study; hence it is not known
whether the strains of ESBL-producing bacteria in this
study were from clonal spread or horizontal plasmid
transfer.
Finally, none of the classes of antibiotics used by
patients is found to be a risk factor for infection by
ESBL-producing bacteria. Osthoff et al. 2015 and
Huang et al. 2007 reported that the use of third
generation cephalosporin is a risk factor for infection
by ESBL-producing bacteria. The use of beta lactambeta lactamase inhibitor (Chopra et al. 2015; Harris et
al. 2007) and fluoroquinolones (Soraas et al. 2013)
were also found as risk factors for infection by ESBLproducing bacteria. The failure to obtain an association
between antibiotic use and infection by ESBLproducing bacteria in this study might be caused by
involvement of small sample size. Another reason
would be because exposure towards antibiotics in this
study is measured as a categorical variable
(exposed/unexposed) rather than as a continuous
variable such as measuring Defined Daily Dose
(DDD), Length of Therapy (LOT) or Duration of
therapy (DOT). Schechner et al. (2013) reported that
an association of antibiotic use with infection by
resistant organisms is more likely to be obtained if the
antibiotic used was measured as a continuous variable
Microbiol Indones
Volume 9, 2015
rather than a categorical variable.
In conclusion, age, gender, pre-infection length of
hospital stay, comorbidities and antibiotic use were not
risk factors for ESBL-infection was discovered,
However, this study finds a significantly larger
proportion of ESBL-E. coli compared to non-ESBL
producing E. coli. Further studies should include larger
sample size and quantitatively measured antibiotic use.
ACKNOWLEDGMENT
The authors would like to thank the Dean of Faculty
of Medicine Universitas Airlangga and the Director of
Dr. Soetomo Hospital whose support made this study
possible.
REFERENCES
Ben-Ami R, Rodrguez-Bano J, Arslan H, Pitout JDD, Quentin
C, Calbo ES, Azap OK, Arpin C, Pascual A, Livermore
DM, Garau J, Carmeli Y. 2009. A multinational survey of
risk factors for infection with extended-spectrum blactamaseproducing enterobacteriaceae in nonhospitalized patients. Clinl Infect Dis. 49(5):682-690.
doi: 10.1086/604713.
Casqueiro J, Casqueiro J, Alves C. 2012. Infections in
patients with diabetes mellitus: A review of
pathogenesis. Indian J Endocrinol Metab. 16(1) S27S36. doi: 10.4103/2230-8210.94253.
Chopra T, Marchaim D, Johnson PC, Chalana IK, Tamam Z,
Mohammed M, Alkatib S, Tansek R, Chaudhry K, Zhao
JJ, Pogue JM, Kaye KS. 2015. Risk factors for
bloodstream infection caused by extended-spectrum blactamase producing Escherichia coli and Klebsiella
pneumoniae: A focus on antimicrobials including
cefepime. American J Infect Control. 43(7):719-723.
http://dx.doi.org/10.1016/j.ajic.2015. 02.030.
Dhillon RHP, Clark J. 2012. ESBLs: A clear and present
danger? Crit Care Res Practice. 2012:625170.
doi:10.1155/2012/625170.
Hadi U, Kuntaman, Qiptiyah M, Paraton H. 2013. Problem
of antibiotic use and antimicrobial resistance in
Indonesia: Are we really making progress?. Indones J
Trop Infect Dis. 4(4):5-8.
Harris AD, McGregor JC, Johnson JA, Strauss SM, Moore
AC, Standiford HC, Hebden JN, Morris JG. 2007. Risk
factors for colonization with extended-spectrum lactamaseproducing bacteria and intensive care unit
admission. Emerg Infect Dis. 13(8): 11441149. doi:
10.3201/eid1308.070071.
Huang Y, Zhuang S, Du M. 2007. Risk factors of nosocomial
infection with extended-spectrum beta-lactamase-
155
producing bacteria in a neonatal intensive care unit in
China. Infection. 35(5):339-45.
Kaya O, Akcam FZ, Gonen I, Unal O, Ceylan T. 2013. Risk
factors for bacteremia due to extended-spectrum betalactamase-producing Escherichia coli in a Turkish
Hospital. J Infect dev Ctries. 7(7): 507-512. doi:
10.3855/jidc.2788.
Kuntaman, Mertaniasih NM, Usman H. 2006.
Multiresistance Pattern of Extended Spectrum Lactamase (Esbl) Escherichia coli and Klebsiella
pnemoniae Strains. Folia Medica Indonesiana. 42(1):
40 - 46.
Osthoff M, McGuinness SL, Wagen AZ, Aisen DP. 2015.
Urinary tract infections due to extended-spectrum betalactamase- producing Gram-negative bacteria:
identification of risk factors and outcome predictors in
an Australian tertiary referral hospital. Int J Infect Dis.
34:7983. doi:10.1016/j.ijid.2015.03.006.
Pajariu A et al. 2010. Infeksi oleh bakteri penghasil
extended-spectrum beta-lactamase (ESBL) di RSUP
Dr. Kariadi Semarang: Faktor risiko terkait penggunaan
antibiotik. Universitas Diponegoro, Semarang.
Schechner V,Temkin E, Harbarth S, Carmeli &, Schwaber
MJ. 2013. Epidemiological interpretation of studies
examining the effect of antibiotic usage on resistance.
Clin Microbiol Rev. 26(2): 289307. doi: 10.1128/
CMR.00001-13.
Silva N, Mrcio O, Bandeira AC, Brites C. 2006. Risk
factors for infection by extended-spectrum betalactamase producing Klebsiella pneumonia in a tertiary
hospital in Salvador, Brazil. Braz J Infect Dis. 10(3):
191-193.
Sraas A, Sundsfjord A, Sandven I, Brunborg C, Jenum PA.
2013. Risk factors for community-acquired urinary
tract infections caused by ESBL-producing
enterobacteriaceae A casecontrol study in a low
prevalence country. PLoS One. 11 p [on line]. doi:
10.1371/journal.pone.0069581.
Tham J. 2012. Extended-spectrum beta-lactamaseproducing enterobacteriaceae: epidemiology, risk
factors, and duration of carriage. Department of
Clinical Sciences, Infectious Disease Research Unit,
Lund University.
Tumbarello M, Spanu T, Sanguinetti M, Citton R, Montuori
E, Leone F, Fadda G, Cauda R. 2006. Bloodstream
infections caused by extended-spectrum betalactamase-producing Klebsiella pneumoniae: Risk
factors, molecular epidemiology, and clinical outcome.
Antimicrob Agents Chemother. 50(2):498.
Tuon FF, Kruger M, Terreri M, Penteado-Filho SR, Gortz L
2011. Klebsiella ESBL bacteremia-mortality and risk
factors, Braz J Infect Dis. 15(6):594-598. doi:10.1016/
S1413-8670(11)70257-4.
156 FITRI ET AL.
Wright GD. 2010. Q&A: Antibiotic resistance: where does it
come from and what can we do about it? BMC Biology.
8:123. doi: 10.1186/1741-7007-8-123.
Shaikh S, Fatima J, Shakil S, Rizyi SMD, Kamal MA. 2015.
Microbiol Indones
Antibiotic resistance and extended spectrum betalactamases: Types, epidemiology and treatment. Saudi
J Biol Sci. 22(1):90-101. doi: 10.1016/j.sjbs.2014.08.
002.
Você também pode gostar
- ESBL Phenotipic PDFDocumento14 páginasESBL Phenotipic PDFGerardo J. Huerta RoblesAinda não há avaliações
- Praktikum Mikrobiologi Gram NegatifDocumento44 páginasPraktikum Mikrobiologi Gram Negatifrids_Ainda não há avaliações
- HCL Update 2019 PDFDocumento8 páginasHCL Update 2019 PDFHaroon KhanAinda não há avaliações
- Lecture 27-Basic Virology-Dr. Ludhang Pradipta Rizki, M.biotech, SP - MK (2018)Documento45 páginasLecture 27-Basic Virology-Dr. Ludhang Pradipta Rizki, M.biotech, SP - MK (2018)NOVI UMAMI UMAMIAinda não há avaliações
- Respon Imun Terhadap PenyakitDocumento40 páginasRespon Imun Terhadap PenyakitKolor GantengAinda não há avaliações
- Immunity To MicrobesDocumento25 páginasImmunity To MicrobestimcarasAinda não há avaliações
- EsblDocumento16 páginasEsblsharmamaddy32Ainda não há avaliações
- 2-Microscopic IdentificationDocumento24 páginas2-Microscopic IdentificationMunir AhmedAinda não há avaliações
- Pengaruh Intensitas Cahaya Dan Nutrisi Terhadap Pertumbuhan MiseliumDocumento6 páginasPengaruh Intensitas Cahaya Dan Nutrisi Terhadap Pertumbuhan MiseliumPUTRI ZAKY ALVAS SYAHNIARAinda não há avaliações
- Tes Lab Pada Peny Infeksi Dan Tropis (Lebih Singkat)Documento71 páginasTes Lab Pada Peny Infeksi Dan Tropis (Lebih Singkat)Monazzt AsshagabAinda não há avaliações
- EsblDocumento159 páginasEsblArunagiri Subramanian100% (2)
- Multiple Myeloma OverviewDocumento52 páginasMultiple Myeloma OverviewanmegpraAinda não há avaliações
- AFPDocumento4 páginasAFPHassan GillAinda não há avaliações
- What'S New in Treatment Monitoring: Viral Load and Cd4 TestingDocumento2 páginasWhat'S New in Treatment Monitoring: Viral Load and Cd4 TestingRina ErlinaAinda não há avaliações
- Quorum Sensing in Bacteria and A Glance On Pseudomonas Aeruginosa 2327 5073.1000156Documento10 páginasQuorum Sensing in Bacteria and A Glance On Pseudomonas Aeruginosa 2327 5073.1000156Tanjila IslamAinda não há avaliações
- MULTIPLE MYELOMA For Medical Students. Copy - 032148Documento39 páginasMULTIPLE MYELOMA For Medical Students. Copy - 032148Miracle Odenigbo100% (1)
- Para Protein Emi ADocumento14 páginasPara Protein Emi AMohamoud MohamedAinda não há avaliações
- Virology Techniques: Chapter 5 - Lesson 4Documento8 páginasVirology Techniques: Chapter 5 - Lesson 4Ramling PatrakarAinda não há avaliações
- Carbapenem Resistance A ReviewDocumento28 páginasCarbapenem Resistance A ReviewSri IriantiAinda não há avaliações
- Anti-Mutated Citrullinated Vimentin Antibodies in Rheumatoid ArthritisDocumento17 páginasAnti-Mutated Citrullinated Vimentin Antibodies in Rheumatoid ArthritisReda RamzyAinda não há avaliações
- Blind PassagingDocumento1 páginaBlind PassagingsomchaisAinda não há avaliações
- Lab Report 10Documento6 páginasLab Report 10api-301352285Ainda não há avaliações
- Final Announcement MaGEHUp 2022Documento14 páginasFinal Announcement MaGEHUp 2022Teti HendrayaniAinda não há avaliações
- ID Virus Avian Influenza h5n1 Biologi Molek PDFDocumento13 páginasID Virus Avian Influenza h5n1 Biologi Molek PDFArsienda UlmafemaAinda não há avaliações
- Lowenstein Jensen MediumDocumento2 páginasLowenstein Jensen MediumRizal IchwansyahAinda não há avaliações
- Hematology 2Documento58 páginasHematology 2Laboratorium Ansari SalehAinda não há avaliações
- Multiple MyelomaDocumento15 páginasMultiple MyelomaDinda YusditiraAinda não há avaliações
- Oncogenesis Topic by Laraib FiazDocumento23 páginasOncogenesis Topic by Laraib FiazLaraib FiazAinda não há avaliações
- Ca 125Documento3 páginasCa 125डा. सत्यदेव त्यागी आर्यAinda não há avaliações
- 15) Dr. Firdaus, Ph. D - Penjelasan Praktikum REPRODUKSI PALUDocumento35 páginas15) Dr. Firdaus, Ph. D - Penjelasan Praktikum REPRODUKSI PALUcimyAinda não há avaliações
- Acinetobacter Baumannii by Gemechis DejeneDocumento36 páginasAcinetobacter Baumannii by Gemechis DejeneGemechis DejeneAinda não há avaliações
- Alpha FetoproteinDocumento2 páginasAlpha FetoproteinmonimoyAinda não há avaliações
- 1 Introduction SymbiosisDocumento229 páginas1 Introduction Symbiosisbex9gg100% (1)
- Immunofluorescence: Tapeshwar Yadav (Lecturer)Documento23 páginasImmunofluorescence: Tapeshwar Yadav (Lecturer)Raj Kumar SoniAinda não há avaliações
- TB Meningitis Lancet 2022Documento15 páginasTB Meningitis Lancet 2022stephanie bojorquezAinda não há avaliações
- Microcytic Anemia PDFDocumento8 páginasMicrocytic Anemia PDFMargarita TorresAinda não há avaliações
- Gene Expression: Protein Synthesis and Control RNA Synthesis and Control Chromatin Structure and FunctionNo EverandGene Expression: Protein Synthesis and Control RNA Synthesis and Control Chromatin Structure and FunctionBrian F. C. ClarkAinda não há avaliações
- Carbapenamases Facts and DetecctionDocumento68 páginasCarbapenamases Facts and Detecctiontummalapalli venkateswara raoAinda não há avaliações
- Review Article - Mirizzi SyndromeDocumento4 páginasReview Article - Mirizzi SyndromeEvan KristionoAinda não há avaliações
- Comparison TB LAMP, Microscopy, GeneXpert and CultureDocumento24 páginasComparison TB LAMP, Microscopy, GeneXpert and Culturepolosan123Ainda não há avaliações
- FACSDocumento24 páginasFACSMudit MisraAinda não há avaliações
- Pratiwi S Gunawan, BDS., DDS., MDSC, PHDDocumento53 páginasPratiwi S Gunawan, BDS., DDS., MDSC, PHDBima Ewando KabanAinda não há avaliações
- HEMATOPOIESISDocumento44 páginasHEMATOPOIESISviviyanti znAinda não há avaliações
- Mycobacterium Tuberculosis and Tuberculosis - TodarDocumento18 páginasMycobacterium Tuberculosis and Tuberculosis - TodarTanti Dewi WulantikaAinda não há avaliações
- 1.1 Bacterial Morphology Structure and ClassificationDocumento108 páginas1.1 Bacterial Morphology Structure and ClassificationJustine Mel Concepcion IlardeAinda não há avaliações
- Principle of VaccineDocumento10 páginasPrinciple of VaccineRasyid WicaksonoAinda não há avaliações
- Alpha Fetoprotein (Afp)Documento10 páginasAlpha Fetoprotein (Afp)Andi UkengAinda não há avaliações
- Carbapenem Power PointDocumento34 páginasCarbapenem Power PointAbiola Olumuyiwa OlaitanAinda não há avaliações
- New Red Blood Cell and Reticulocyte Parameters and Reference Values For Healthy Individuals and in Chronic Kidney Disease.Documento8 páginasNew Red Blood Cell and Reticulocyte Parameters and Reference Values For Healthy Individuals and in Chronic Kidney Disease.Alberto MarcosAinda não há avaliações
- Tumor Markeri - Eng PDFDocumento79 páginasTumor Markeri - Eng PDFdr_4uAinda não há avaliações
- Pancytopenia As Initial Presentation of Acute Lymphoblastic Leukemia and Its Associationwith Bone MarrowresponseDocumento6 páginasPancytopenia As Initial Presentation of Acute Lymphoblastic Leukemia and Its Associationwith Bone MarrowresponseIJAR JOURNALAinda não há avaliações
- BCCA Febrile Neutropenia GuidelinesDocumento2 páginasBCCA Febrile Neutropenia GuidelinesdenokayuMRAinda não há avaliações
- CBA MouseTh1Th2 Kit ManualDocumento52 páginasCBA MouseTh1Th2 Kit ManualendopetAinda não há avaliações
- Jurnal RubellaDocumento2 páginasJurnal RubellaAlif SpiritAinda não há avaliações
- Cystatin C As An Early Marker of Diabetic Nephropathy in Nigerian Adults With Type 2 DiabetesDocumento9 páginasCystatin C As An Early Marker of Diabetic Nephropathy in Nigerian Adults With Type 2 Diabetesijmb333Ainda não há avaliações
- "Simple Screening Test of Ampc Beta-Lactamases in Clinical Isolates Among MultidrugDocumento15 páginas"Simple Screening Test of Ampc Beta-Lactamases in Clinical Isolates Among MultidrugBhagwat Suryawanshi100% (1)
- Tuberculosis en PDFDocumento307 páginasTuberculosis en PDFAbdullah Khairul AfnanAinda não há avaliações
- Acute-On-Chronic Liver Failure - Controversies and ConsensusDocumento10 páginasAcute-On-Chronic Liver Failure - Controversies and ConsensusPhan Nguyễn Đại NghĩaAinda não há avaliações
- Jurnal Gastroenterology, Hepatology, and Nutrition PediatricDocumento71 páginasJurnal Gastroenterology, Hepatology, and Nutrition PediatricJonathan WelchAinda não há avaliações
- Pediatric Neurology PDFDocumento301 páginasPediatric Neurology PDFJonathan WelchAinda não há avaliações
- Pediatric Gastroenterology Algorithme PDFDocumento118 páginasPediatric Gastroenterology Algorithme PDFJonathan Welch100% (1)
- TB SimulationDocumento15 páginasTB SimulationJonathan WelchAinda não há avaliações
- International Journal of Pathology and Clinical Research Ijpcr 2 023Documento9 páginasInternational Journal of Pathology and Clinical Research Ijpcr 2 023Jonathan WelchAinda não há avaliações
- Glasgow Meningococcal Septicaemia Prognostic Score (GMPS) : Arrival 1 Hour 1 Systolic Blood PressureDocumento1 páginaGlasgow Meningococcal Septicaemia Prognostic Score (GMPS) : Arrival 1 Hour 1 Systolic Blood PressureJonathan WelchAinda não há avaliações
- Antibiotik Pada Anak: Achmad Yudha ApDocumento23 páginasAntibiotik Pada Anak: Achmad Yudha ApJonathan WelchAinda não há avaliações
- Clinical Features, Evaluation, and Diagnosis of Sepsis in Term and Late Preterm Infants PDFDocumento27 páginasClinical Features, Evaluation, and Diagnosis of Sepsis in Term and Late Preterm Infants PDFJonathan WelchAinda não há avaliações
- Causedoutbreak Klebsiella PDFDocumento11 páginasCausedoutbreak Klebsiella PDFJonathan WelchAinda não há avaliações
- Ta Katsuji 1996Documento7 páginasTa Katsuji 1996Jonathan WelchAinda não há avaliações
- Laura M Lamberti, Christa L Fischer Walker, Adi Noiman, Cesar Victora and Robert E BlackDocumento1 páginaLaura M Lamberti, Christa L Fischer Walker, Adi Noiman, Cesar Victora and Robert E BlackJonathan WelchAinda não há avaliações
- Esbl Sepsis India2011Documento8 páginasEsbl Sepsis India2011Jonathan WelchAinda não há avaliações
- Early-Onset Neonatal Sepsis: Kari A. Simonsen, Ann L. Anderson-Berry, Shirley F. Delair, H. Dele DaviesDocumento27 páginasEarly-Onset Neonatal Sepsis: Kari A. Simonsen, Ann L. Anderson-Berry, Shirley F. Delair, H. Dele DaviesJonathan WelchAinda não há avaliações
- MGMTDocumento19 páginasMGMTMakrant MohanAinda não há avaliações
- A656 GR 80 Brochure 06-26-08Documento2 páginasA656 GR 80 Brochure 06-26-08OsmanAinda não há avaliações
- Soft Tissue SarcomaDocumento19 páginasSoft Tissue SarcomaEkvanDanangAinda não há avaliações
- BT HandoutsDocumento4 páginasBT HandoutsNerinel CoronadoAinda não há avaliações
- OBESITY - Cayce Health DatabaseDocumento4 páginasOBESITY - Cayce Health Databasewcwjr55Ainda não há avaliações
- Speaking Topics For Final ReviewDocumento3 páginasSpeaking Topics For Final ReviewNhư ÝAinda não há avaliações
- BDC 6566Documento6 páginasBDC 6566jack.simpson.changAinda não há avaliações
- HDFC Life Insurance (HDFCLIFE) : 2. P/E 58 3. Book Value (RS) 23.57Documento5 páginasHDFC Life Insurance (HDFCLIFE) : 2. P/E 58 3. Book Value (RS) 23.57Srini VasanAinda não há avaliações
- Little Ann and Other Poems by Ann Taylor and Jane TaylorDocumento41 páginasLittle Ann and Other Poems by Ann Taylor and Jane Tayloralexa alexaAinda não há avaliações
- Vocab PDFDocumento29 páginasVocab PDFShahab SaqibAinda não há avaliações
- Bi RadsDocumento10 páginasBi RadsFeiky Herfandi100% (1)
- Data Obat VMedisDocumento53 páginasData Obat VMedismica faradillaAinda não há avaliações
- Starters Flash CardsDocumento28 páginasStarters Flash CardsNara GarridoAinda não há avaliações
- Demolition/Removal Permit Application Form: Planning, Property and Development DepartmentDocumento3 páginasDemolition/Removal Permit Application Form: Planning, Property and Development DepartmentAl7amdlellahAinda não há avaliações
- Plastic Omnium 2015 RegistrationDocumento208 páginasPlastic Omnium 2015 Registrationgsravan_23Ainda não há avaliações
- The Effect OfAdditional Nanoparticles Supplementation of Indonesian Bay Leaf (SyzigiumPolyanthum) On Blood Pressure in Pregnancy HypertensionDocumento4 páginasThe Effect OfAdditional Nanoparticles Supplementation of Indonesian Bay Leaf (SyzigiumPolyanthum) On Blood Pressure in Pregnancy HypertensionInternational Journal of Innovative Science and Research TechnologyAinda não há avaliações
- Dynamic Stretching - Stability - Strength.570239Documento2 páginasDynamic Stretching - Stability - Strength.570239Sylvia GraceAinda não há avaliações
- Learning Guide No 5Documento19 páginasLearning Guide No 5Menal JemalAinda não há avaliações
- Sepsis Management UCLA HealthDocumento23 páginasSepsis Management UCLA HealthKomang_JananuragaAinda não há avaliações
- RDG UNIT 2 Skimming Class A 2021Documento17 páginasRDG UNIT 2 Skimming Class A 2021Yuly Rumondang Wulan SiallaganAinda não há avaliações
- Fortune Falls - Lou VaneDocumento402 páginasFortune Falls - Lou VanetesteAinda não há avaliações
- طبى 145Documento2 páginasطبى 145Yazan AbuFarhaAinda não há avaliações
- Marketing ProjectDocumento82 páginasMarketing ProjectSumit GuptaAinda não há avaliações
- Drake Family - Work SampleDocumento1 páginaDrake Family - Work Sampleapi-248366250Ainda não há avaliações
- Work of Asha Bhavan Centre - A Nonprofit Indian Organisation For Persons With DisabilityDocumento10 páginasWork of Asha Bhavan Centre - A Nonprofit Indian Organisation For Persons With DisabilityAsha Bhavan CentreAinda não há avaliações
- Injection Analyzer Electronic Unit enDocumento67 páginasInjection Analyzer Electronic Unit enmayralizbethbustosAinda não há avaliações
- Material: Safety Data SheetDocumento3 páginasMaterial: Safety Data SheetMichael JoudalAinda não há avaliações
- Tryout Consent Form - 2014 - Sign and ReturnDocumento2 páginasTryout Consent Form - 2014 - Sign and ReturnSanjeevan BaraAinda não há avaliações
- Content Map PE & Health 12Documento12 páginasContent Map PE & Health 12RIZZA MEA DOLOSOAinda não há avaliações
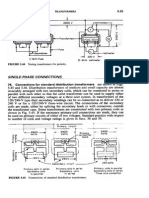
- Transformers ConnectionsDocumento6 páginasTransformers Connectionsgeorgel1980Ainda não há avaliações