Escolar Documentos
Profissional Documentos
Cultura Documentos
Final Burst Abdomen in Pregnancy
Enviado por
saryindrianyDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Final Burst Abdomen in Pregnancy
Enviado por
saryindrianyDireitos autorais:
Formatos disponíveis
Case report
Burst abdomen in pregnancy: A proposed management algorithm
Amalachukwu M. Okpala1, Samuel A. Debrah2 and Mohammed Mouhajer3
Ghana Med J 2016; 50(2): 115-118 DOI: http://dx.doi.org/10.4314/gmj.v50i2.10
1
Department of Plastic Surgery, Leeds General Infirmary, Leeds, United Kingdom 2Department of Surgery,
School of Medical Sciences, University of Cape Coast, Cape Coast, Ghana 3Department of Obstetrics and
Gynaecology, Korle Bu Teaching Hospital, Accra, Ghana
Corresponding author: Amalachukwu M. Okpala
E-mail: drmaluski@yahoo.com
Conflict of interest: None declared
SUMMARY
Management of the burst abdomen is complex due to the co-morbidities associated with it. When coupled with intraabdominal sepsis and pregnancy, it becomes even more difficult due to the ethical issues that have to be considered
when managing both mother and child. Due to the paucity of literature on this subject, a management algorithm has
been proposed which aims at tackling this delicate issue. However, the major consideration in the management of
these cases is that decisions are to be made based on optimization of the condition of the mother.
Keywords: Burst abdomen, pregnancy, management, algorithm, intra-abdominal sepsis
INTRODUCTION
Acute abdomen in pregnancy, and thus management of
its complications, remains one of the most challenging
diagnostic and therapeutic dilemmas of today despite
advancements in medical technology.1 Wound dehiscence following intra - abdominal sepsis in pregnancy is
rare, and the management of such a complex case is a
conundrum to both the surgeon and the obstetrician.
Whether to close or not to close the abdomen, or when
and how to deliver the fetus depends on both maternal
and fetal factors which must be considered to have the
most optimal outcome.
Case report
Eighteen-year-old Miss CN was referred from a hospital
in the district to the Central Regional Hospital as a case
of intestinal obstruction post laparotomy for typhoid
perforation in pregnancy at 23 weeks gestation. Patient
had undergone surgery 3 days prior to referral, and intra
operative findings were faeculent peritoneal fluid, and a
single large ileal perforation 15 cm from the ileo-caecal
junction. A simple closure had been done. Three days
post operatively, abdominal distension was noticed,
associated with bilious vomiting, hence the referral from
the district hospital.
On initial assessment at the emergency unit, a young,
very ill looking female with marked pallor and a temperature of 38.o C was noted. She was tachypnoeic and
tachycardic, with a blood pressure of 100/64 mmHg.
115
Her abdomen was distended, with pus oozing out from a
sub-umbilical midline incision, which was held, together by non-absorbable sutures. Obstetric examination
(abdomino-pelvic ultrasound) revealed a viable fetus at
23 weeks gestation.
Laboratory investigations showed a haemoglobin level
of 6.6 g/dl and a white cell count of 14.6 x 10 9 /L. A
diagnosis of deep surgical site infection post laparotomy
with severe anaemia was made. Patient was admitted
and resuscitated with intravenous fluids, intravenous
antibiotics and blood transfusions. A wound swab was
taken for culture and sensitivity. Skin sutures were removed to facilitate drainage of pus, and patient was
managed on a high protein/calorie enteral diet. On the
tenth day of admission, the patient developed a burst
abdomen. A Bogota bag was provided for closure of the
abdomen due to the finding of a septic hostile abdomen
in an anaemic malnourished patient.
The surgical wound granulated over rapidly, and the
foetus was monitored regularly via abdominal ultrasound and daily foetal kick counts. Seven weeks after
admission (gestational age 31 weeks) and after a course
of steroids to promote foetal lung maturation, patient
went into preterm labour and delivered a live male infant via spontaneous vaginal delivery. The neonate was
taken to the neonatal intensive care unit for further monitoring.
www.ghanamedj.org Volume 50 Number 2 June 2016
Case report
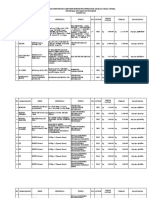
Management algorithm for burst abdomen in pregnancy
Burst abdomen in pregnancy (post laparotomy; post incisional hernia etc)
-----------------------------------------------------------------------------------------------
<24 weeks
> 24 weeks
Intra-abdominal sepsis
Intra-abdominal sepsis
Yes ------------------------------------------- No
No ------------------------------------------------------ Yes
Foetus alive
Foetus alive
Yes --------------------------------------------------------- No
Foetus alive
Foetus alive
Yes --------------------------------No
SM
SM
NPWT/BB
C/S
TOP
CS/SVD with
1o mesh repair
NPWT/BB + EHR
Mesh repair
NPWT/BB
SVD/CS when possible
EHR
Yes ------- --------- No
NPWT/BB
Mesh repair
No -----------------
SM
C/S
NPWT/BB
EHR
--------------------Yes
SM
NPWT/BB
SVD/CS when possible
EHR
SVD Spontaneous Vaginal Delivery; NPWT Negative Pressure Wound Therapy; CS Caesarean Section;
TOP Termination of pregnancy
SM -Surgical management involves laparotomy and peritoneal lavage if required; BB Bogota bag;
EHR Elective hernia repair
Patient was discharged with a healthy neonate to be
reviewed on an outpatient basis. The wound subsequently healed with secondary intention, with future consideration of incisional hernia repair.
DISCUSSION
Typhoid fever is a distinctive acute systemic febrile
infection caused by several serotypes of the Gramnegative bacillus Salmonella (primarily Salmonella
choleraesuis serotypes typhi and paratyphi).2 A study
carried out in a hospital in Pakistan showed that nonpregnant women with typhoid fever were more likely to
develop complications as compared to the pregnant
women.2 The authors of that study also derived the hypothesis that disease complications in typhoid fever are
related to host immunity and less likely to occur with
the immunological changes associated with pregnancy.2
Having said this, when complications due to typhoid
perforation do occur, the lives of the mother and the
foetus are at stake.
116
TOP + 10 mesh repair
CS/SVD
Fetal losses, especially when typhoid perforation occurs
during the first and second trimester, are high .3 Maternal mortality rate is also high and this is probably due to
the physiological changes in pregnancy coupled with
the stress of typhoid infection and intra-abdominal sepsis.3
Surgery is the gold standard for the treatment of typhoid
perforation after adequate resuscitation, correction of
electrolyte imbalance and commencement of appropriate antibiotic therapy.2 Multiple local, regional, and systemic factors can contribute to post-laparotomy wound
dehiscence as occurred in our case.4 The patient had
wound infection with ongoing intra-abdominal sepsis
due the gross peritoneal contamination; bowel distension due to a combination of bowel edema, paralytic
ileus and a gravid uterus; and severe anaemia with malnutrition.
www.ghanamedj.org Volume 50 Number 2 June 2016
Case report
There are different modalities available for the management of wound dehiscence post laparotomy, which
range from primary repair with sutures/mesh reinforcement, to entero-atmospheric treatment.5 However, in the
presence of intra-abdominal sepsis and a gradually enlarging uterus, the management option with the best
outcome for both mother and foetus becomes more difficult to choose due to fewer viable options. An online
search for the management of similar cases revealed 3
cases of burst abdomen during pregnancy, 2 due to incisional hernias, and the third due to surgical site infection
post laparotomy.6,7,8 The first case had a burst abdomen
due to an incisional hernia at a gestational age of 28
weeks which was initially managed with a mesh hernia
repair and tension sutures. The baby was subsequently
delivered by Caesarean section at 34 weeks with a concurrent surgical repair of the hernia.6 The second case of
burst abdomen due to an incisional hernia occurred at
35 weeks gestation, and underwent a Caesarean section
with concurrent hernia repair without a mesh.7 These
cases had no overt on-going intra-abdominal sepsis,
hence the choice of management. The third case developed an intra-abdominal abscess with wound failure at a
gestational age of 27 weeks post small bowel resection,
and was managed on Negative Pressure Wound Therapy
(NPWT). The wound was healed in 4 weeks, and the
baby was delivered vaginally at 39 weeks.
The advantage of NPWT post wound dehiscence is well
documented in literature.4There is no evidence of randomized controlled trials involving use of NPWT in
gravid patients. This may be due to the rarity of such
cases. However, the two cases in which NPWT were
used in gravid patients reported excellent outcomes for
both mother and baby.8,10
Due to the paucity of literature on the management of
wound dehiscence due to intra-abdominal sepsis in
pregnant patients, the authors have suggested a management algorithm (Figure 1). It takes a broad look at
the management of the burst abdomen in pregnancy
according to the presence of intra-abdominal sepsis and
the gestational age of viability which is 24 weeks according to WHO guidelines.9 Those who present with
intra-abdominal sepsis usually undergo an elective incisional hernia repair after management of the pregnancy
and the sepsis.
2.
Important points to consider are:
1. The availability of neonatal intensive care units
for resuscitation and management of preterm
deliveries.
2. Management decisions must be made based on
the health of the mother, not of the foetus.
3. Gestational age of viability differs among different countries, depending on the quality of
their neonatal intensive care units. The suggested algorithm can be adapted to suit the selected gestational age of viability for whichever health care system it is implemented in.
117
CONCLUSION
Management of the acute abdomen, and the sequelae of
complications that may arise in pregnancy is a challenge
even for the best equipped facilities. There is a paucity
of literature on the management of wound dehiscence in
pregnancy with/without intra-abdominal sepsis. A management algorithm for such cases has been suggested.
Although no adverse effects have been reported in the
cases in which NPWT was used in the gravid patient,
randomized controlled trials and long term follow up
would be necessary to confirm its overall safety in
pregnancy and absence of long term effects on the foetus. Decisions on management of these cases must be
made based on the health of the mother.
REFERENCES
1.
3.
4.
5.
6.
7.
8.
Goran Augustin, Mate Majerovic. Non-obstetric
acute abdomen during pregnancy. Eur J Obstet Gynecol Reprod Biol 2007; 131: 4 12.
Sulaiman K, Sarwari AR; Culture-confirmed typhoid fever and pregnancy. Int J Infect Dis 2007;
11:337 341.
Naaya HU, Eni UE, Chama CM. Typhoid Perforation in Maiduguri, Nigeria. Ann Afr Med 2004;
3(2): 69 -72.
Heller L, Levin S, Butler C. Management of abdominal wound dehiscence using vacuum assisted
closure in patients with compromised healing. Am J
Surg 2006; 191(2): 165 172.
Lopez-Cano M, Pereira J, Armengol-Carrasco M.
Acute postoperative open abdominal wall: Nosological concept and treatment implications. World J
Gastrointest Surg 2013; 5(12):314 -320.
Kumar R, Sonika A, Kaberi B, Sunesh K, Charu C.
Gravid Uterus in an incisional hernia leading to
burst abdomen. The Internet Journal of Gynecology
and Obstetrics 2004; 5 (1).
Dubey C, Gupta N, Gupta C, Arora R, Sachdeva P.
Successful pregnancy outcome in a case of gravid
uterus in an incisional hernia leading to burst abdomen. The Internet Journal of Gynecology and
Obstetrics 2009; 13 (1).
Shapiro S, Mumme D. Use of Negative Pressure
Wound Therapy in the Management of Wound De-
www.ghanamedj.org Volume 50 Number 2 June 2016
Case report
9.
118
hiscence in a Pregnant Patient. Wounds 2008; 20
(2):46 48.
Ikechebelu JI, Eleje GU, Ugochukwu EF, Edokwe
ES. Should we re-define age of Fetal Viability in
Nigeria? A Case Report of Newborn Survival from
pre-viable pre-labor rupture of membranes. J Womens Health Issues Care 2014; 3:3.
10. Asukai K, Kashiwazaki M, Koizumi K, Nobunaga
T, Yano H. A case report of a 19-week gravid patient with a dehisced abdominal wound and treated
with V.A.C. ATS Therapy System. Int Wound J
2014; doi:10.1111/iwj.12352
www.ghanamedj.org Volume 50 Number 2 June 2016
Você também pode gostar
- Nelson2013 Ajog PDFDocumento7 páginasNelson2013 Ajog PDFsaryindrianyAinda não há avaliações
- Acute Fatty Liver of Pregnancy: Letter To EditorDocumento2 páginasAcute Fatty Liver of Pregnancy: Letter To EditorsaryindrianyAinda não há avaliações
- Pregnancy-Related Liver Disorders: Seminar Journal of Clinical and Experimental HepatologyDocumento12 páginasPregnancy-Related Liver Disorders: Seminar Journal of Clinical and Experimental HepatologysaryindrianyAinda não há avaliações
- Birth After Previous Caesarean Section (C Obs 38) Re Write July 2015 1Documento27 páginasBirth After Previous Caesarean Section (C Obs 38) Re Write July 2015 1saryindrianyAinda não há avaliações
- Acute Fatty Liver of Pregnancy: Better Understanding of Pathogenesis and Earlier Clinical Recognition Results in Improved Maternal OutcomesDocumento8 páginasAcute Fatty Liver of Pregnancy: Better Understanding of Pathogenesis and Earlier Clinical Recognition Results in Improved Maternal OutcomessaryindrianyAinda não há avaliações
- ACG Clinical Guideline: Liver Disease and Pregnancy: Practice GuidelinesDocumento19 páginasACG Clinical Guideline: Liver Disease and Pregnancy: Practice GuidelinessaryindrianyAinda não há avaliações
- 3881825Documento30 páginas3881825saryindrianyAinda não há avaliações
- Calculation of Ratios For Fetal Venous Blood Flow WaveformsDocumento1 páginaCalculation of Ratios For Fetal Venous Blood Flow WaveformssaryindrianyAinda não há avaliações
- Causes and Management of Surgical Wound Dehiscence: Department of General SurgeryDocumento10 páginasCauses and Management of Surgical Wound Dehiscence: Department of General SurgerysaryindrianyAinda não há avaliações
- Post Caesarean Surgical Site Infections 2Documento6 páginasPost Caesarean Surgical Site Infections 2saryindrianyAinda não há avaliações
- 1 s2.0 S0889854515001163Documento18 páginas1 s2.0 S0889854515001163saryindrianyAinda não há avaliações
- Rupture of Membranes Guideline For The Management of Preterm PrelabourDocumento10 páginasRupture of Membranes Guideline For The Management of Preterm PrelaboursaryindrianyAinda não há avaliações
- Risk Factors For Wound Dehiscence After Laparotomy - Clinical Control TrialDocumento9 páginasRisk Factors For Wound Dehiscence After Laparotomy - Clinical Control TrialsaryindrianyAinda não há avaliações
- Technical Series 2 Using PartographDocumento5 páginasTechnical Series 2 Using PartographsaryindrianyAinda não há avaliações
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Module 2Documento7 páginasModule 2karthik karti100% (1)
- Ward 7Documento14 páginasWard 7Financial NeedsAinda não há avaliações
- Rab Sikda Optima 2016Documento20 páginasRab Sikda Optima 2016Julius Chatry UniwalyAinda não há avaliações
- Scrum Handbook: Scrum Training Institute PressDocumento66 páginasScrum Handbook: Scrum Training Institute PressFranky RiveroAinda não há avaliações
- VLSI Implementation of Floating Point AdderDocumento46 páginasVLSI Implementation of Floating Point AdderParamesh Waran100% (1)
- Windows System Shortcut CommandsDocumento2 páginasWindows System Shortcut CommandsVenkatesh YerraAinda não há avaliações
- ProbDocumento10 páginasProbKashif JawaidAinda não há avaliações
- Flowrox Valve Solutions Catalogue E-VersionDocumento16 páginasFlowrox Valve Solutions Catalogue E-Versionjavier alvarezAinda não há avaliações
- Heirs of Vinluan Estate in Pangasinan Charged With Tax Evasion For Unsettled Inheritance Tax CaseDocumento2 páginasHeirs of Vinluan Estate in Pangasinan Charged With Tax Evasion For Unsettled Inheritance Tax CaseAlvin Dela CruzAinda não há avaliações
- Vintage Airplane - May 1982Documento24 páginasVintage Airplane - May 1982Aviation/Space History LibraryAinda não há avaliações
- Shaqlawa Technical College: IT DepartmentDocumento20 páginasShaqlawa Technical College: IT Departmentbilind_mustafaAinda não há avaliações
- Dash 3000/4000 Patient Monitor: Service ManualDocumento292 páginasDash 3000/4000 Patient Monitor: Service ManualYair CarreraAinda não há avaliações
- Steel Price Index PresentationDocumento12 páginasSteel Price Index PresentationAnuj SinghAinda não há avaliações
- Case Study To Find Tank Bulging, Radial Growth and Tank Settlement Using API 650Documento15 páginasCase Study To Find Tank Bulging, Radial Growth and Tank Settlement Using API 650Jafer SayedAinda não há avaliações
- 2 - Sample Kids Can Read and Write 2 and 3 Letter Words - Step 2 Final Downloadable Version For Website PDFDocumento18 páginas2 - Sample Kids Can Read and Write 2 and 3 Letter Words - Step 2 Final Downloadable Version For Website PDFsantoshiAinda não há avaliações
- Module 2 TechnologyDocumento20 páginasModule 2 Technologybenitez1Ainda não há avaliações
- Thermodynamic c106Documento120 páginasThermodynamic c106Драгослав БјелицаAinda não há avaliações
- Yarn HairinessDocumento9 páginasYarn HairinessGhandi AhmadAinda não há avaliações
- Reproduction in PlantsDocumento12 páginasReproduction in PlantsAnand Philip PrasadAinda não há avaliações
- BA 4722 Marketing Strategy SyllabusDocumento6 páginasBA 4722 Marketing Strategy SyllabusSri GunawanAinda não há avaliações
- Ransomware: Prevention and Response ChecklistDocumento5 páginasRansomware: Prevention and Response Checklistcapodelcapo100% (1)
- Angelo (Patrick) Complaint PDFDocumento2 páginasAngelo (Patrick) Complaint PDFPatLohmannAinda não há avaliações
- 1st Problem Solving Assignment - Barrels of Apples - M383 Sp22.docx-2Documento4 páginas1st Problem Solving Assignment - Barrels of Apples - M383 Sp22.docx-2Kor16Ainda não há avaliações
- Shift in Business Strategy of 10 Minute School - B2B To B2CDocumento40 páginasShift in Business Strategy of 10 Minute School - B2B To B2CSadiaAinda não há avaliações
- Barista Skills Foundation Curriculum enDocumento4 páginasBarista Skills Foundation Curriculum enCezara CarteșAinda não há avaliações
- R15 Understanding Business CyclesDocumento33 páginasR15 Understanding Business CyclesUmar FarooqAinda não há avaliações
- Stochastic ProcessesDocumento264 páginasStochastic Processesmanosmill100% (1)
- Helipal Tbs Powercube ManualDocumento29 páginasHelipal Tbs Powercube Manualoualid zouggarAinda não há avaliações
- Lab 2 - Permeability TestDocumento9 páginasLab 2 - Permeability TestAinur NasuhaAinda não há avaliações
- Catalog Tu ZG3.2 Gian 35kV H'MunDocumento40 páginasCatalog Tu ZG3.2 Gian 35kV H'MunHà Văn TiếnAinda não há avaliações