Escolar Documentos
Profissional Documentos
Cultura Documentos
Contemporary Nurse Volume 20 Issue 2 2005 (Doi 10.5172 - Conu.20.2.234) Taylor, Beverley Holroyd, Beth Edwards, Paul Unwin, Anna Row - Assertiveness in Nursing Practice - An Action Research and Re
Enviado por
Hendri HariadiTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Contemporary Nurse Volume 20 Issue 2 2005 (Doi 10.5172 - Conu.20.2.234) Taylor, Beverley Holroyd, Beth Edwards, Paul Unwin, Anna Row - Assertiveness in Nursing Practice - An Action Research and Re
Enviado por
Hendri HariadiDireitos autorais:
Formatos disponíveis
This article was downloaded by: [University of Otago]
On: 20 July 2015, At: 20:48
Publisher: Routledge
Informa Ltd Registered in England and Wales Registered Number: 1072954 Registered
office: 5 Howick Place, London, SW1P 1WG
Contemporary Nurse
Publication details, including instructions for authors and
subscription information:
http://www.tandfonline.com/loi/rcnj20
Assertiveness in nursing practice: An
action research and reflection project
a
Beverley Taylor , Beth Holroyd , Paul Edwards PhD Candidate ,
c
Anna Unwin & Joanne Rowley PhD Candidate
Foundation Chair in Nursing Southern Cross University, Lismore
campus, Lismore, New South Wales
b
Mental Health Nurse Coffs Harbour Health Campus, Coffs
Harbour, New South Wales
c
Nurse Educator Coffs Harbour Health Campus, Coffs Harbour,
New South Wales
d
Nurse Researcher Coffs Harbour Health Campus, Coffs Harbour,
New South Wales
Published online: 17 Dec 2014.
To cite this article: Beverley Taylor, Beth Holroyd, Paul Edwards PhD Candidate, Anna Unwin &
Joanne Rowley PhD Candidate (2005) Assertiveness in nursing practice: An action research and
reflection project, Contemporary Nurse, 20:2, 234-247, DOI: 10.5172/conu.20.2.234
To link to this article: http://dx.doi.org/10.5172/conu.20.2.234
PLEASE SCROLL DOWN FOR ARTICLE
Taylor & Francis makes every effort to ensure the accuracy of all the information (the
Content) contained in the publications on our platform. However, Taylor & Francis,
our agents, and our licensors make no representations or warranties whatsoever as to
the accuracy, completeness, or suitability for any purpose of the Content. Any opinions
and views expressed in this publication are the opinions and views of the authors,
and are not the views of or endorsed by Taylor & Francis. The accuracy of the Content
should not be relied upon and should be independently verified with primary sources
of information. Taylor and Francis shall not be liable for any losses, actions, claims,
proceedings, demands, costs, expenses, damages, and other liabilities whatsoever
or howsoever caused arising directly or indirectly in connection with, in relation to or
arising out of the use of the Content.
This article may be used for research, teaching, and private study purposes. Any
substantial or systematic reproduction, redistribution, reselling, loan, sub-licensing,
systematic supply, or distribution in any form to anyone is expressly forbidden. Terms &
Downloaded by [University of Otago] at 20:48 20 July 2015
Conditions of access and use can be found at http://www.tandfonline.com/page/termsand-conditions
Copyright eContent Management Pty Ltd. Contemporary Nurse (2005) 20: 234247.
Assertiveness in nursing practice: An
action research and reflection project
Downloaded by [University of Otago] at 20:48 20 July 2015
ABSTRACT
Key Words
action research;
reflective
practice;
assertiveness;
nursing practice
This article describes an action research project that highlighted reflective
processes, so hospital nurses could work systematically through problem solving
processes to uncover constraints against effective nursing care; and to improve the
quality of their care in light of the identified constraints and possibilities. Four
Registered Nurses (RNs) co-researched their practice with the facilitator and
over the research period identified the thematic concern of the need for
assertiveness in their work.The RNs planned, implemented and evaluated an
action plan and, as a direct result of their reflections and collaborative action,
they improved their nursing practice in relation to becoming more effective in
assertiveness in work situations.
Received 5 August 2005
Accepted 27 October 2005
BEVERLEY TAYLOR
PAUL EDWARDS
Foundation Chair in Nursing
Southern Cross University, Lismore campus
Lismore, New South Wales
PhD Candidate and Mental Health Nurse
Coffs Harbour Health Campus
Coffs Harbour, New South Wales
BETH HOLROYD
ANNA UNWIN
Mental Health Nurse
Coffs Harbour Health Campus
Coffs Harbour, New South Wales
Nurse Educator
Coffs Harbour Health Campus
Coffs Harbour, New South Wales
JOANNE ROWLEY
PhD Candidate and Nurse Researcher
Coffs Harbour Health Campus
Coffs Harbour, New South Wales
234
CN
CN
Volume 20, Issue 2, December 2005
Assertiveness in nursing practice
INTRODUCTION
LITERATURE REVIEW
ursing in hospitals involves negotiating
complex interpersonal relationships and
working in a social and political context within
economic constraints, while balancing a multiplicity of tasks and roles. Nurses are busy clinicians who need to have a broad range of clinical
knowledge and skills, and they are accountable
to many people (Benner 1984; Benner and
Wrubel 1989; Taylor 1997, 2000). Hospital
nurses are caught up in the complexity and
busyness of daily work, but these constraints can
be managed effectively by reflective processes
(Freshwater 2002;Taylor 2000).
This article describes an action research
project that emphasised the value of reflective
practice through which nurses identified the
thematic concern of assertiveness at work.This
article describes the project in terms of its
background, methodology, methods, processes
and insights.The action plan the nurses generated and instituted for practising assertively is also
described.
Assertiveness is an important issue in nursing
practice. After a period of reflective practice,
when the nurses in this project identified their
need for assertiveness at work, the literature
was explored with the intention of assisting in
the creation of the action plan. Nursing literature repeats the call for nurses to become more
assertive (Gaddis 2004; Levesque 2003; Madden 1996; McNally 2002; Milstead 1996; Morris 2004; Kupperschmidt 1994; Larson 1997;
Pacquiao 2000; Pauly-ONeill 1997; Smith
1997). Education programs in assertiveness
knowledge and skills have been in vogue for
some time in nursing because nurses have
recognised the need for assertiveness in quality
nursing care (Benton 1999; Cardillo 2003;
Class 2001; Crouch 2003; Floyd 1999, 2001;
Habel 2004; Lyttle 2001; McCabe & Timmins
2003; Milstead 1996; Pearce 2004; Percival
2005, 2001, 2000; Stein-Parbury 2005;Woods
2003). All of these authors agree that assertiveness is important in nursing practice, but that it
is complex and requires time and practice to
make it effective.
This review describes some recent nursing
research into assertiveness (Addis & Gamble
2004; Jaime et al. 1998; McCartan & Hargie
2004a,b; Timmins & McCabe 2005). Timmins
and McCabe (2005) undertook a preliminary
pilot study to assess how assertive nurses are in
the workplace, in order to develop an instrument and report on the results.The researchers
distributed the 44-item questionnaire to 27 registered nurses and the results showed that nurses in the study responded strongly to items
allowing others to express opinions, complimenting others and saying no (Timmins and
McCabe 2005:61). The researchers concluded
that the nurses behave in a passive, nice way and
were less adept at disagreeing with others
opinions and providing constructive criticism
(Timmins and McCabe 2005:61). Even though
this project has been reported as a preliminary
pilot study, the results should be viewed cau-
Downloaded by [University of Otago] at 20:48 20 July 2015
CN
AIM, OBJECTIVES, SIGNIFICANCE
AND BACKGROUND
This project aimed to facilitate action research
and reflective practice processes in experienced
Registered Nurses in order to:
raise critical awareness of practice problems
they face everyday;
work systematically through problem solving
processes to uncover constraints against
effective nursing care; and
improve the quality of care given by hospital
nurses in light of the identified constraints
and possibilities.
The significance of the project was in improving
nursing care and in educating nurses in a
research process they can use for clinical problems that emerge daily in their practice.
The project originated through collaboration
between a School of Nursing and practice-based
nurses.
Volume 20, Issue 2, December 2005
CN
235
Downloaded by [University of Otago] at 20:48 20 July 2015
CN
Beverley Taylor et al.
tiously because of low sample numbers and the
tendency for questionnaire respondents to indicate nice or self-fulfilling behaviours, even if
they practice in a contrary way, by using active
assertion in their workplace.
Addis and Gamble (2004:452) aimed to
understand what nurses had learned from an
assertive outreach (AO) experience.The project
was informed by the phenomenological concepts of Heidegger and data were collected
through the use of semi-structured interviews
of five rural AO nurses working in one county
in England. The thematic analysis revealed that
nurses understood their experience of assertive
engagement as involving: having time; anticipatory persistence and tired dejection; pressure,
relief and satisfaction; being the human professional confluence; accepting anxiety and fear;
working and learning together; and bringing the
caring attitude. Thus it was shown that being a
rural AO nurse involves contradictory yet
rewarding experiences in practising assertive
behaviours with clients.
McCartan and Hargie (2004a:707) administered The Caring Assessment Instrument and
the Assertion Inventory to a convenience sample
of 94 nurses to find answers to their research
question, Assertiveness and caring: are they
compatible? The background to their project
was that numerous assertion studies suggest
that nurses are generally non-assertive, so they
wanted to determine whether positive and negative assertion behaviours were related to caring
skills. The researchers defined positive assertion as:
other-centred caring type behaviours such as
expressing positive feelings, initiating and
maintaining interactions, giving and receiving
compliments, and conveying empathy.
(McCartan & Hargie 2004a: 707708)
Negative (standard conflict) responses are often
viewed as self-centred skills and may be considered undesirable attributes in nursing (McCar236
CN
tan & Hargie 2004a:708). After analysis of the
nurses responses, they concluded that:
Overall the findings of the study suggest that
positive and negative assertive behaviours are
not related to caring skills The current
findings suggest that the presence of caring
attributes cannot be offered as a possible reason for non-assertion in nurses.
(McCartan & Hargie 2004a:707)
McCartan and Hargie (2004b) distributed the
Bem Sex-Role Inventory and the Assertion
Inventory to a convenience sample of 94 subjects, to determine the effects of nurses sex
role orientation on positive and negative assertion.The researchers reported that contrary to
earlier studies, the findings of the investigation
indicated that there was no significant relationship between assertion measurements and sexrole orientation (McCartan & Hargie 2004b:
45). The findings of the research projects by
McCartan & Hargie (2004a,b) demonstrate difficulties in making exact statements about
assertiveness and suggest that its success is relative to the contexts in which nurses enact it.
The research question posed by Jaime et al.
(1998:98) was whether assertiveness is a characteristic of the nursing profession. Their
descriptive study aimed to determine the
degree of assertiveness in nurses and to assess
the influence of personal characteristics, such as
age, sex, marital status, work experience and
place of employment. A questionnaire measuring the degree of assertiveness in professional
environments was distributed to 75 nurses
working in acute care settings in three Spanish
hospitals.The results showed qualitative differences according to personal characteristics
although these were not statistically significant,
and a high percentage of nursing professionals
showed low degrees of assertiveness (Jaime et
al. 1998:98). The researchers concluded that
given the low degree of assertiveness in the
research sample, assertiveness training was necessary to improve the quality of health care.
Volume 20, Issue 2, December 2005
Downloaded by [University of Otago] at 20:48 20 July 2015
Assertiveness in nursing practice
CN
Their conclusions assume that caring and
assertiveness are linked and that assertiveness is
essential in the provision of quality nursing care.
In summary, nursing research literature
emphasises the need for nurses to become more
assertive and to acquire the necessary knowledge and skills to make nurses assertiveness
more apparent in their workplaces.
water 1999), and education (Anderson &
Branch 2000; Clegg 2000; Cruickshank 1996
Freshwater 1999; Kim 1999; Platzer et al.
2000). Much of the literature focuses on the
work of nursing as practised in clinical contexts
(e.g., Freshwater 1998, 2002; Glaze 1999;
Heath 1998a,b; Johns 2000, 2003;Taylor 2004.
2003, 2002a,b;Wilkin 2002).
METHODOLOGY
Action research
Action research involves four stages of collectively planning, acting, observing and reflecting
(Dick 1995; Stringer 1996).This phase leads to
another cycle of action in which the plan is
revised, and further acting, observing and
reflecting is undertaken systematically to work
towards solutions to problems of a technical,
practical or emancipatory nature (Kemmis &
McTaggart 1988;Taylor 2000).
Nurses have been using action research
successfully in a variety of settings focusing
on differing thematic concerns (e.g., Keatinge
et al. 2000; Koch, Kralik & Kelly 2000;
Chenoweth & Kilstoff 1998). Action research
and reflective processes combine well methodologically because of their common interest
in making sense of experiences, in order to
progress to deeper insights and personal and
professional changes. Research using action
research and reflection has been successful in
giving nurses contextual answers to practice
issues such as dysfunctional nursenurse relationships (Taylor 2001b) and nurses tendencies
towards idealism in palliative care (Taylor et al.
2002).
In qualitative research, methodology usually
means the theoretical assumptions of how
knowledge is generated and validated, which
underlie the choice of methods. Given the collaborative nature of the project, a qualitative
approach was chosen, informed by reflective
practitioner concepts and action research.
Reflective practice
Taylor (2000:3) defines reflection as the throwing back of thoughts and memories, in cognitive
acts such as thinking, contemplation, meditation
and any other form of attentive consideration,
in order to make sense of them and to make
contextually appropriate changes if they are
required. Schn (1983) emphasised the idea
that reflection is a way in which professionals
can bridge the theorypractice gap, based on
the potential of reflection to uncover knowledge in and on action. He referred to tacit
knowledge, or knowing in action, as the kind of
knowledge of which practitioners may not be
entirely aware. When practitioners/clinicians,
such as nurses, are coached to make explicit
their knowing-in-action, they can inevitably use
this awareness to enliven and change their practice (Schn 1987).
Nursing has applied reflective practice ideas
to many of its disciplinary areas. In particular,
nursing has used reflective processes for some
time, for example, to improve practice and
practice development (Johns 2003; Stickley &
Freshwater 2002;Thorpe & Barsky 2001;Taylor
2000, 2002a,b), clinical supervision (Gilbert
2001; Heath & Freshwater 2000;Todd & Fresh-
ACCESSING PARTICIPANTS
Ethical implications
Full ethical clearance from the University and
the Health Campus Research Committee preceded the commencement of the project. As
this research encouraged nurses to share their
practice stories, likely risks were that the privacy and confidentiality of patients may have been
Volume 20, Issue 2, December 2005
CN
237
Downloaded by [University of Otago] at 20:48 20 July 2015
CN
Beverley Taylor et al.
breached and that nurses may have felt vulnerable in sharing their experiences, leading to
embarrassment or possible emotional catharsis,
such as tearfulness or anger. No group member
became emotionally upset beyond the ability of
the group to support them and. although the
project offered professional counselling at no
cost to self, no participant required this service.
Nurses are educated in the need for patient
confidentiality and they practice it daily in their
work. Even so, the researcher ensured that privacy and confidentiality measures were instituted and maintained. Stories written in journals
and shared in group meetings were devoid of
information which could identify patients, relatives and staff. Pseudonyms were used and identifying material was omitted or renamed to
protect the identities of people within the written transcripts of the stories. Reflective journals
remained the personal property of participants
and they were not be read or sighted by the
researcher unless it was a participants expressed
wish that this occurred. Reports and published
material describe the participants stories and
interpretations, according to the issues they
raised and the practice improvements they
caused, rather than to identify specific people,
places and situations.
Participant recruitment
A verbal and written explanation of the project
was given by the researcher at a regular meeting
of the Registered Nurses (RNs) working at the
hospital. Convenience sampling was used to target intentionally RNs interested in reflecting on
their practice in order to improve it. Four RNs
agreed to participate: three females and one
male, from 30 to 45 years of age, with from 10
to 15 years of clinical nursing experience.
The sequence of research activities was based
on previous projects (Taylor 2001a,b).The data
collection activities were embedded in the
group processes and they were that:
RNs were given opportunities to write journal reflections of practice experiences, by
using participant observation during the normal course of their work in ward areas. As
with all nursing care, the details of patients
care were completely confidential.
the reflections were shared in the group
meetings.
the individual and the group critically
analysed the content of all the shared practice
stories and identified common themes and
issues in nursing practice (Taylor 2000).This
means that the participants collectively discussed issues raised in the stories, decided on
the specific nature of issues and named those
issues as research themes.
a theme common to all of the reflections was
identified as the thematic concern (issue) as a
focus for the group. The thematic concern
was the need for assertion in workplace communication.
an action cycle of planning, assessing, observing and reflecting generated an action plan
for addressing and amending the identified
thematic concern.
the action plan was instituted in nursing
practice and the results of the changed
approach to the thematic concern were
noted, through continued planning, acting,
observing and reflecting.
the action plan underwent revision until it
achieved positive changes in successfully
managing the identified thematic concern of
assertion in nursing practice.
RESEARCH PHASES
Data collection and analysis
The research period occurred in five main
Over a 17-week period, the four RNs met phases:
weekly with the researcher/facilitator for one introductory processes;
hour to discuss clinical problems raised by them reflections on practice stories;
in their journal writing and group discussion. locating a thematic concern;
238
CN
Volume 20, Issue 2, December 2005
Assertiveness in nursing practice
Downloaded by [University of Otago] at 20:48 20 July 2015
generating, applying and revising the action
plan; and
improving assertion through reflective practice.
Phase One: Introductory processes
The introductory processes were from the first
to third meeting inclusive. In the first meeting,
each participant received a folder containing
documents relating to the research. Participants
read the Plain Language Statement about the
research and signed the Consent Form. Participants began talking about themselves, especially
where they work and what they hoped to
achieve from the research.The researcher/facilitator gave a brief introduction to the main ideas
within action research and reflective practice
and how the two combine well for research
into nursing practice. Participants discussed the
group processes and agreed that they would like
to be uninterrupted when telling a story, and
expressed the wish for confidentiality in the
group to be maintained to develop trust in the
group and to encourage disclosure. Participants
decided to meet weekly at the same day and
time and to use videoconferencing sometimes,
to reduce the researcher/facilitators road travel.
The second meeting was by videoconferencing and each participant spoke informally about
their week and how they were feeling generally.
This became an informal check-in icebreaker
each week. Participants were concerned about
having relatively little knowledge of research so
they were assured that the process would be
instructive in collaborative research processes.
Participants were asked to reflect on the following questions: Who influenced my childhood
(people, organisations, etc)? What rules for living did I learn? How have these rules for living
influenced my nursing practice? Participants
responded spontaneously to these questions and
they agreed to reflect on these questions during
the week.
In the third meeting, it was reiterated that no
persons name would appear in research reports
CN
of publications and that the use of a split pronoun approach (s/he) to writing would hide
the identity of the only male in the group. Participants read the Agendas and Minutes of the
previous meetings and noted handouts on Some
Background on Research and Reflection, and
the first reflective task of reflecting on childhood influences. Participants shared some of
their thoughts on the introductory reflecting
task. For example: A participant recognised personal difficulty in facing anger, relating to a
work situation in which confrontation of an
aggressive colleague was needed. The participant tried to secure a winwin situation and
remarked that it was important to be assertive
in the situation, especially in light of how nurses
might be perceived by other members of the
multidisciplinary team. It was noted that disciplines have different ways of communicating
and that it is far easier to talk with nurse colleagues than it is with other professionals, such
as teachers.
Phase Two: Reflections on practice
stories
The second phase of reflecting on practice stories was from the fourth to seventh meeting
inclusive. In the fourth meeting, participants
began sharing their practice stories. For example, a participant shared a story of being called
urgently to a medical ward by some nurses and
s/he did not know why, but guessed it related
to a clinical situation.When s/he arrived, there
was a young male patient in distress,in a dreadful situation. He was clammy, pale and had a
tracheostomy. S/he assessed that the mucous
coming copiously through his mouth and tracheostomy tube was indicative of pulmonary
oedema. At first s/he thought: What am I
doing here? I dont know what to do, but the
old ICU nurse kicked in and s/he took control
of the situation and organised the emergency
care and medical assistance. Since that time,
s/he has used that scenario to highlight the
case in the hospital, but s/he has felt powerless
Volume 20, Issue 2, December 2005
CN
239
Downloaded by [University of Otago] at 20:48 20 July 2015
CN
Beverley Taylor et al.
to cause changes as some people have a strangle
hold on the decisions. S/he also commented
that s/he was careful not to blame the nurses in
the situation, but wondered why they were trying to hide their lack of knowledge of what to
do and whether they were scared of getting
into trouble for doing something wrong, even
though they had done nothing wrong.
This led to a conversation of how nurses are
in life/death situations with so much to know in
order to act quickly to be effective clinically.
The researcher/facilitator suggested that the
participant who shared the story raise as many
questions as s/he can about the situation and
personal responses to it, but to leave the questions open-ended and unanswered. Another participant commented that, especially at acute
ward level, nurses are quick to notice other
nurses mistakes but do not tend to give praise
to one another.
In the fifth meeting, participants spoke
briefly about some reflections on the story of
the acutely ill male patient with pulmonary
oedema and other questions that might be asked
about the story. Participants continued sharing
their practice stories. A practice story related to
a busy shift in ICU, when a child with acute
leukaemia was admitted.The participant told of
the terror that s/he feels when a sick child
comes in, relating the sense of responsibility it
creates. The participant was relieved when the
childs care was allocated to a senior nurse who
s/he felt could handle it when the child needed a platelet transfusion. The participant
expressed the need s/he felt to check on the
infusion procedure for platelets, sensing that the
nurse may not have been aware of how to do the
task properly. The information was not in the
ward so s/he went to locate it elsewhere. The
platelets had come from hundreds of kilometres
away, the childs parents were there, the ICU
was fairly silent, the platelets were not going
through and the participant feared the platelets
would soon be coagulating. As the nurse in
charge of that shift, the participant took control
240
CN
of the situation by quietly suggesting to the
nurse that s/he get another filter, while the participant gently moved the platelets in the transfusion bag to minimise coagulation. The
participant expressed feelings of increasing
stress, especially as the parents asked if anything
was wrong, and s/he covered up by replying
that it was a faulty filter. The after hours NUM
was contacted by phone and s/he was not
impressed having to find another filter and
asked why it was necessary. The participant
could not speak out loud on the phone as the
ward was quiet and the parents were listening.
The participant thought: Why couldnt she (the
nurse caring for the child) admit she didnt
know (how to prepare the filter)? What do the
parents think? After the story the participant
asked herself: Why do I take so much responsibility for others? The participant felt so
annoyed at the nurse for not speaking up and
admitting that she did not know how to prepare
the filter, as it would have saved so much time,
energy and worry.
A participant commented that nursing is a
job in which nurses are under scrutiny and
pressure.The researcher/facilitator guided the
storytelling participant through questions as
prompts to get to a deeper level of reflection on
the incident. Where do my ideas come from historically? In other words, what are the values you hold
about nursing practice and from where do your values
come? The participant expressed a belief in the
need for quality care, and for maintaining a professional image of nursing. In the past, s/he has
seen things done badly, incorrectly and s/he
imagined what it might be like to be in the
same predicament. What do I continue to use these
values in my work? Its just me I just want a
good outcome. Whose interests do these values
serve? In other words, who benefits? Me and the
broader image of nursing I guess Im modelling the image (I want for nursing). What power
relations were involved in the story? This nurse is
close to (someone in authority). The participant realised s/he stayed quiet in not asking the
Volume 20, Issue 2, December 2005
Assertiveness in nursing practice
Downloaded by [University of Otago] at 20:48 20 July 2015
nurse in the story if she knew the correct procedure for the filter, because of implicit power
relations, even though the participant was in
charge of the shift and s/he felt it reflected
badly on her/his ability to handle the shift.
In the sixth and seventh meetings, participants continued to share practice stories and to
work through deeper levels of reflection and
meaning by posing questions to themselves
about their personal and professional values and
interests.
Phase Three: Locating a thematic
concern
Phase Three lasted from meetings eight to 11
inclusive. After many practice stories were
shared in the second phase, it was time to locate
a common interest on which all of the participants could reflect and use an action research
approach to explore more deeply. In the eight
and ninth meeting, participants examined a
Table of practice stories to locate issues and
themes within them. Participants discussed
issues and interests that arose: for example,
their reactions to suicide of clients and acquaintances, the relative usefulness of being under
scrutiny and pressure in nursing work, the inexplicability of nurses intuition, and the role of
consumer representatives in bringing about policy changes.
In the tenth meeting, participants listed the
issues/themes generated in the group as: assertion/confrontation/conformity; bullying and
horizontal violence; Aboriginal issues; professional protection of self and others; professional
competency of self and others; slow change;
having a sense of belonging; being under scrutiny and pressure, documentation issues; self
blame and perfection; autonomy versus duty of
care; and role clarification/role valuing.
In the next meeting (11), participants agreed
that they would work as a whole group and
needed to find a thematic concern that was sufficiently generic to their practice so that they
could all see improvements in that area. After
CN
much fruitful discussion, the group decided that
the area most common to them all, with the
best chance of creating practice improvements,
was the thematic concern of assertion/confrontation/conformity. As participants had not
checked their understanding of what each person meant by assertion, they defined it individually so that the group had a working definition.
The responses were that assertion is about:
Participant 1: valuing others opinions while
giving ones own opinion, and not being
scared to do so.
Participant 2: not being passive but not being
aggressive, so there is balance and a middle
ground. It is me challenging myself. I prepare
myself emotionally and usually say: I feel that
...,I would prefer that ...
Participant 3: being at a similar level to make eye
contact, not towering over or being towered
over; with attention to appropriate use of personal space. It involves having an internal conversation to make sense of the concern and to
get it out in the right way. It involves honesty
in what I am saying and feeling, and having self
respect and self esteem, to not let people tread
all over me.
Participant 4: an issue of equality, of feeling valued and of feeling I have an opinion worth
telling others, and having them listen. It reflects
confidence, and the need to let go of emotions,
to find a common ground.
In discussion, participants noted that assertion is
context-specific, in that it depends on the situation as to how nurses react and find voice at
that time. Participants spoke of trying to learn
to listen, taking extra breaths before speaking
and not making preconceived conclusions to
assist assertive communication. We needed to
take a two-week break from meetings so participants agreed to do some homework reflecting
Volume 20, Issue 2, December 2005
CN
241
CN
Beverley Taylor et al.
Downloaded by [University of Otago] at 20:48 20 July 2015
on what is useful and not useful about assertion,
and on practice scenarios when they were
assertive and it went well, and when assertive
attempts did not go well.
ing the previous week at work. For example, a
participant said that s/he experienced an effective assertive episode when s/he confronted a
staff member who used to undermine her.
S/he pulled her aside quietly and privately
told her how s/he felt. The person hearing the
message received it well and expressed surprise
that she had that effect on the participant.
Things have been great since. The participant
reflected that s/he had rehearsed the scenario
and that s/he was pleased it went well.This discussion led to the insight that nurses need not
only to maintain basic courtesies in assertive
attempts, they must also maintain their self
respect and to remind themselves that they are
worthy as nurses and people. Following discussion, the action plan was amended to the second
and final version.
Phase Four: Generating, applying
and revising an action plan
Phase Four lasted from meeting 12 to 14 inclusive. In meeting 12, the group noted that they
often have opportunities in their work to assert
themselves by confronting issues as they occur,
thereby choosing to avoid conformity and not
speaking up. They discussed their reflections
about what is useful and not so useful about
assertion by reflecting on practice situations. As
each person spoke, other participants responded and encouraged openness in a trusting group
process.
For example, a participant said that s/he has
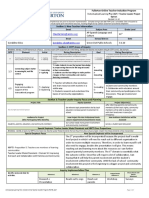
been giving the matter a lot of thought and had ACTION PLAN: Strategies for
realised that assertion is the initiation tool to improving assertion at work
get things started as it is the starting point of 1. Ask: What are the real issues? What do I
collaboration within the multidisciplinary team.
need to communicate effectively?
If the timing is not right, assertion loses its 2. Bring energy to the job. Dont go to work
impact. If the timing of assertion is wrong, the
tired, or sick, or with personal issues getassertive attempt comes off the wrong way.
ting in the way that is, be feeling OK
Courage and timing are needed to get assertive
when you go to work, to give it your full
attempts just right so they have maximal impact.
attention.
This point led to further comments by other 3. Get your emotions under control that is,
group members, such as: In the consultation
be aware of your bodily responses to
role, timing is important ... it is important not
assertive opportunities, such as to note
to patronise. Experienced health care staff
your heart rate is telling you it is important
already have considerable communicative skills,
to speak, wait your turn, and then speak.
and poorly timed or initiated attempts to assert 4. Get the facts ready dont go off halfmay be interpreted as patronising.
cocked.
The group then moved onto the next part of 5. Find a good place to talk if possible, for
the process which was to brainstorm ideas for
example, not on the move and walking in a
strategies for making assertion more effective.
busy and noisy setting. Suggest a time to
Given that brainstorming allows all ideas to be
talk and go aside into a quiet environment.
heard and noted, the original list was unedited 6. If an ideal time and place is not possible for
and it contained some accompanying discussion
effective communication, gauge the responthat arose at the time the ideas were shared.
siveness of the other person and decide
In meeting 13, discussion continued about
whether to speak up at that time, or to wait
the pros and cons of assertion and whether the
until a more conducive moment.
action plan had been helpful to participants dur- 7. Timing is important, so it may be better to
242
CN
Volume 20, Issue 2, December 2005
Downloaded by [University of Otago] at 20:48 20 July 2015
Assertiveness in nursing practice
wait to communicate an assertive position.
For example, in professional group meetings when issues arise, it may be better to
wait, recognising the limitations of the context.
8. Effective assertion requires a listener. The
person to whom you are communicating
needs to know who you are and why they
should listen to you. Introduce yourself and
make sure the person knows who you are,
how you fit into the scheme of things, and
how you have the capacity to represent
clients needs and issues.
9. Recognise the communication style of the
other person, as little may be achieved if
there is aggression and firmly held misconceptions.
10. When meeting with other people who are
not in your immediate disciplinary group,
to minimise misinterpretations based on
lack of understanding of roles and intentions, sit down and begin by asking people
about their priorities, specifically what they
hope to achieve in the meeting that is,
their objectives before conveying your
own. In this way, it is possible to clarify
intentions and expectations, and to see if
objectives match, and thereby ascertain the
angle people are coming from.
11. Be prepared to go it alone without backup
and support, when asserting a position.
12. Maintain basic courtesies, such as conveying
respect, by addressing the person by name
and title.
13. Maintain your self-respect and remind
yourself that you are worthy as a nurse and
person.
14. Remember that communication has many
modes such as face-to-face, emails, letters,
phone calls, etc, and that all of these communication modes are important opportunities for assertion.
15. Use ongoing reflection and educational opportunities to further develop knowledge
and skills in assertion.
CN
By meeting 14, participants were well into the
action research part of the project because they
were actively enlisting the action plan and refining it through practice reflections. For example,
a participant told of a situation involving a student who had been at the hospital for 10 days of
clinical placement and wanted the participant to
write a report on her abilities.The student was
looking pleadingly at the participant. In this
case, the participant asserted that s/he could
not in all fairness write a report based on one
day of observation of her practice, so s/he
referred her to another staff member in a better
position to comment.The participant said that,
at work, s/he was aware of the groups research
discussions and the action plan, and s/he kept
thinking:Assertion!
Phase Five: Improving assertion
through reflective practice
In the last phase from meetings 15 to 17 inclusive, participants continued to share practice
stories and insights related to assertiveness. For
example, a participant shared a practice story of
how s/he applied some principles learned in a
Tai Chi workshop to a clinical situation, specifically to become ready for assertiveness. For
example, a young female patient was in need of
a stay in a clinical support unit before being
allocated support accommodation. Frequent
previous attempts to secure the admission to the
clinical unit had been unsuccessful because of a
huge waiting list. The participant phoned the
doctor and, in a relaxed manner, laid out the
situation and put it in terms of pressure of
beds, and as advantages for the young female
and also for the unit. S/he emphasised
improved outcomes and was successful in securing short-term admission that day, to her/his
amazement. When the group discussed the
story, they focussed on tone of voice on the
phone when transmitting an assertive message.
The relaxed tone was because the participant
thought the situation was hopeless so there was
nothing to lose by another plea. Participants
Volume 20, Issue 2, December 2005
CN
243
CN
Beverley Taylor et al.
see no benefit from doing research I did
not have the experience or maybe I was too
lazy It was so timely when I heard it
was action research action and research! I
thought: That sounds good! I have had experiences and I have something to say. The
meetings have all been valuable I now
have a different spin on research and academic. This research can help my practice. I can
see what I have learned here and I have put it
into practice. I had only known about medical model research and it seemed too long.
This action research is perfect for me,
because of doing it (researching) in a group.
agreed that if they are too earnest in their
requests, the voice can become crackly and does
not sound assertive. In addition, a participant
noted that if s/he is out of breath, confidence
decreases.
The last meeting (17) was by teleconference
and the group shared practice stories and
insights. Finally, the participants shared their
experiences of being involved in the action
research and reflection project, and their
responses were:
Downloaded by [University of Otago] at 20:48 20 July 2015
I found the process interesting especially
in how to go about research ... the steps
involved. I found that I have a lot of stuff
buried inside I remembered practice stories from long ago and they are still stirring
up so much, that is surprising I need to
deal with it (the practice experiences) I
enjoyed talking at a deep level. I can see my
work experiences are full of opportunities
for research. I enjoyed the team work and the
friendship, trust and disclosure. (The participant talks regularly with a critical friend, to
aid reflections on his/her practice.)
I really enjoyed the process. I was surprised
by how I got into the reflection and I continued writing personal reflections. I did a lot of
personal journaling at home and (a family
member) enjoyed the insights into my life
s/he did not know before.When I put pen to
paper I was amazed at how the details came
flooding back the smells, emotions, feelings. It made me sit back and reflect about
work being (myself) I put my head down
and got on with things. I tend to be a happy
person and to dwell on things being
reflective is a positive way of dwelling on
things I enjoyed researching with three
other experienced nurses and fitting in
with the others (participants) and areas of
conversations.
The most valuable aspects of the research for
me has been the focus on practice reflection.
I have used reflective journalling previously
and always found it a useful tool, but in the
day-to-day business I have been forgetting to
incorporate reflection into my self-care. My
wish is for all nurses to give reflective journalling a go at least once, particularly the
analysis of the reflections. The research has
reminded me to reintroduce reflection more
regularly into my practice. The cohesive
group we formed during the research process has been a highlight for me. At all times I
felt safe to disclose my thoughts and the
members discussion and comments have
been both insightful and comforting. I believe
the project has fostered the formation of new
nursing bonds that can only be good for our
profession.
The researcher/facilitator thanked the group
for their comments and suggested that they now
had the knowledge and skills to undertake
action research themselves, whenever they had
practice issues that need deeper attention.
IMPLICATIONS AND CONCLUSION
The implications of the research are that action
research and reflection are practical research
I am very practically minded and value com- processes for nurses to examine their practice
monsense I am not academic and could issues and to improve nursing care. The action
244
CN
Volume 20, Issue 2, December 2005
Downloaded by [University of Otago] at 20:48 20 July 2015
Assertiveness in nursing practice
research and reflective practice approach can be
used in a variety of ways to assist nurses to
reflect on practice issues and care improvements. This project shed light on the need for
assertiveness and ways in which to improve
assertiveness at work.
The nurses in this research generated an
action plan with practical strategies for improving assertiveness at work. The action plan is
available to other nurses who may find it useful
in improving their assertiveness at work. The
implications of this research for nurse teachers
are that assertiveness continues to be a difficult
skill to enact in the immediacy of the workplace. The communication skills within the
action plan from this research can be explored
in experiential teaching sessions.
In conclusion, the nurses in this research
realised that assertiveness is difficult, but that it
is possible when a reflective approach is taken
to practice.The implication of this research for
other nurses with whom it resonates is that they
too can make positive changes to their assertiveness, by paying focused attention to their daily
work practices.
References
Addis J and Gamble C (2004) Assertive outreach
nurses experience of engagement. Journal of
Psychiatric and Mental Health Nursing 11(4):
452460.
Anderson M and Branch M (2000) Storytelling: A
tool to promote critical reflection in the RN
student. Minority Nurse Newsletter (71): 12.
Benner P (1984) From novice to expert: uncovering the
knowledge embedded in clinical practice. AddisonWesley, Menlo Park CA.
Benner P and Wrubel J (1989) The Primacy Of
Caring: Stress And Coping In Health And Illness
Addison-Wesley, Menlo Park CA.
Benton D (1999) Assertiveness, power and
influence. Nursing Standard, 13(52): 4852.
Cardillo D (2003) Become more assertive, one
step at a time. Nursing Spectrum 4(8): 17.
Chenoweth L and Kilstoff K (1998) Facilitating
CN
positive changes in community dementia
management through participatory action
research. International Journal of Nursing Practice
4: 175188.
Class P (2001) Assertiveness for dummies. Nursing
Spectrum 14(10): 3.
Clegg S (2000) Knowing through reflective
practice in higher education. Education Action
Research 8(3): 451469
Crouch D (2003) Careers. How to be assertive,
Nursing Times 99(40): 7071.
Cruickshank D (1996) The art of reflection:
using drawing to uncover knowledge
development in student nurses. Nurse Education
Today 16(2): 12730.
Dick RA (1995) A beginners guide to action
research. ARCS Newsletter 1(1): 59.
Floyd K (1999) Career fitness: Assertiveness made
simple. Nursing Spectrum 12(3): 15.
Floyd K (2001) Be assertive and true to
yourself. Nursing Spectrum 11(1): 34.
Freshwater D (1998) From acorn to oak tree: a
neoplatonic perspective of reflection and caring.
Australian Journal of Holistic Nursing 5(2): 1419.
Freshwater D (1999) Communicating with self
through caring:The student nurses experience
of reflective practice. International Journal of
Human Caring 3(3): 2833.
Freshwater D (ed) (2002) Therapeutic Nursing:
Improving Patient Care Through Reflection Sage,
London.
Gaddis S (2004) The power of positive nursing.
Pulse 41(4): 1314.
Gilbert T (2001) Reflective practice and supervision: meticulous rituals of the confessional.
Journal of Advanced Nursing 36(2): 199205.
Glaze J (1999) Reflection, clinical judgement and
staff development. British Journal of Theatre
Nursing 9(1): 3034.
Habel M (2004) Staying cool under fire: how well
do you communicate? NurseWeek, September.
Heath H (1998a) Keeping a reflective practice
diary: a practical guide, Nurse Education Today
18(7): 592598.
Heath H (1998b) Reflection and patterns of
Volume 20, Issue 2, December 2005
CN
245
Downloaded by [University of Otago] at 20:48 20 July 2015
CN
Beverley Taylor et al.
knowing in nursing. Journal of Advanced Nursing
27(5): 10541059.
Heath H and Freshwater D (2000) Clinical
supervision as an emancipatory process:
Avoiding inappropriate intent. Journal of
Advanced Nursing 32(5): 12981306.
Holmes C (1992) The drama of nursing. Journal of
Advanced Nursing (17): 954960.
Jaime S, Ortiz R and Vazquez P (1998)
Assertiveness in nursing: A characteristic of the
profession? Enfermeria Clinica 8(3): 98103.
Johns C (2000) Working with Alice: A reflection.
Complementary Therapies in Nursing and Midwifery
6: 199303.
Johns C (2003) Easing into the light. International
Journal for Human Caring 7(1): 4955.
Keatinge D, Scarfe C, Bellchambers H, McGee J,
Oakham R, Probert C, Stewart L and Stokes J
(2000) The manifestation and nursing management of agitation in institutionalised residents
with dementia. International Journal of Nursing
Practice 6: 1625.
Kemmis S and McTaggart R (eds) (1988) The
Action Research Planner Deakin University Press,
Geelong,Victoria.
Kim HS (1999) Critical reflective inquiry for
knowledge development in nursing practice.
Journal of Advanced Nursing (295): 12051212.
Koch T, Kralik D and Kelly S (2000) We just dont
talk about it: Men living with urinary
incontinence and multiple sclerosis. International Journal of Nursing Practice 6: 253260.
Kupperschmidt B (1994) Carefronting: caring
enough to confront. Oklahoma Nurse 39(4): 710.
Larson B (1997) Communication. Assertiveness,
Home Health Focus 4(4): 28.
Levesque J (2003) Nurses must be assertive. AACN
News 20(1): 2.
Lyttle V (2001) Why ED nurses have that attitude.
RN (reprinted by permission) Summer, 1618.
Madden P (1996) Onwards with new
assertiveness. World of Irish Nursing 4(3): 5.
McCabe C and Timmins F (2003) Teaching assertiveness to undergraduate nursing students.
Nurse Education in Practice 3(1): 3042.
246
CN
McCartan P and Hargie O (2004a) Assertiveness
and caring: Are they compatible? Issues in
Clinical Nursing 13: 707713.
McCartan P and Hargie O (2004b) Effects of
nurses sex-role orientation on positive and
negative assertion. Nursing and Health Sciences
6(1): 4549.
McNally S (2002) If nursings profile is to be
raised, it must be assertive. British Journal of
Nursing 11(17): 1114.
Milstead J (1996) Basic tools for the orthopaedic
staff nurse. Part 1: assertiveness. Orthopaedic
Nursing 15(1): 2330.
Morris R (2004) Speak up or shut up?
Accountability and the student nurse. Paediatric
Nursing 16(6): 2022.
Pacquiao D (2000) Impression management: an
alternative to assertiveness in intercultural
communication. Journal of Transcultural Nursing
11(1): 56.
Pauly-ONeill S (1997) Warning: being gutsy can
be habit-forming. Missouri Nurse 66(2): 16.
Pearce C (2004) Being assertive in the workplace.
Nursing Times 100(21): 4647.
Percival J (2000) Say what you want. Nursing
Standard 15(5): 25.
Percival J (2001) Dont be too nice. Nursing
Standard 15(19): 22.
Percival J (2005) Be clear and firm. Nursing
Standard 19(23): 26.
Platzer H, Blake D and Ashford D (2000a) Barriers
to learning from reflection:A study of the use of
groupwork with post-registration nurses. Journal
of Advanced Nursing 31(5): 10011008.
Platzer H, Blake D and Ashford D (2000b) An
evaluation of process and outcomes from
learning through reflective practice groups on a
post-registration nursing course. Journal of
Advanced Nursing 31(3): 689695.
Schn DA (1983) The reflective practitioner: how
practitioners think in action Basic Books, NY.
Schn DA (1987) Educating the reflective practitioner
Jossey-Bass, London.
Smith L (1997) Collaboration: the key to assertive
Volume 20, Issue 2, December 2005
Downloaded by [University of Otago] at 20:48 20 July 2015
Assertiveness in nursing practice
communications. MEDSURG Nursing 6(6):
373377.
Stein-Parbury J (2005) Patient and Person:
Interpersonal Skills in Nursing Elsevier, Sydney.
Stickley T and Freshwater D (2002) The art of
loving and the therapeutic relationship. Nursing
Inquiry 9(4): 250256.
Stringer ET (1996) Action research:A Handbook for
Practitioners Sage,Thousand Oaks CA.
Taylor B (1997) Big battles for small gains:A cautionary note for teaching reflective processes in
nursing and midwifery. Nursing Inquiry 4: 1926.
Taylor B (2000) Reflective practice for nurses and
midwives:A practical guide Allen & Unwin, Sydney.
Taylor B (2001a) Overcoming obstacles in
becoming a reflective nurse and person.
Contemporary Nurse 11(23): 187194.
Taylor B (2001b) Identifying and transforming
dysfunctional nursenurse relationships through
reflective practice and action research. International Journal of Nursing Practice 7(6): 406413.
Taylor B (2002a) Technical reflection for
improving nursing and midwifery procedures
using critical thinking in evidence based
practice. Contemporary Nurse 13(23): 281287.
Taylor B (2002b) Becoming a reflective nurse or
midwife: using complementary therapies while
CN
practising holistically. Complementary Therapies
in Nursing and Midwifery 8(4): 6268.
Taylor B (2003) Emancipatory reflective practice
for overcoming complexities and constraints in
holistic health care. Sacred Space 4(2): 4045.
Taylor B (2004) Technical, practical and emancipatory reflection for practising holistically. Journal
of Holistic Nursing 22(1): 7384.
Taylor B, Bulmer B, Hill L, Luxford C, McFarlane
J and Stirling K (2002) Exploring idealism in
palliative nursing care through reflective
practice and action research. International
Journal of Palliative Nursing 8(7): 324330.
Thorpe K and Barsky J (2001) Healing through
self-reflection. Journal of Advanced Nursing
35(5): 760768.
Timmins F and McCabe C (2005) How assertive
are nurses in the workplace? A preliminary pilot
study. Journal of Nursing Management 13(1): 6167.
Todd G and Freshwater D (1999) Reflective practice and guided discovery: Clinical supervision.
British Journal of Nursing 8(20): 13831389.
Wilkin K (2002) Exploring expert practice
through reflection. Nursing in Critical Care 7(2):
8893.
Woods R (2003) Healthy boundaries=healthy
nurse:The foundation of assertive living and
working. Nursing matters 14(12): 16, 1819.
ANNOUNCING
HEALTH SOCIOLOGY REVIEW
S OCIAL E QUITY
AND
H EALTH
Edited by Olle Lundberg, CHESS, Karolinska Institute, Sweden
ISBN 0-9757422-8-0; iv + 124 pages; softcover
Details at: http://hsre-contentmanagement.com/15.2/social-equity-and-health.htm
Course Coordinators are invited to contact the Publisher:
subscriptions@e-contentmanagement.com for an adoption evaluation copy.
Volume 20, Issue 2, December 2005
CN
247
Você também pode gostar
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5795)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Curriculum de Hong-Kong - Ed. B - Sica-MatematicaDocumento292 páginasCurriculum de Hong-Kong - Ed. B - Sica-MatematicaGregório Silva NetoAinda não há avaliações
- Ilp FullertonDocumento3 páginasIlp Fullertonapi-467608657Ainda não há avaliações
- Muluken Alemayehu FINAL PDFDocumento47 páginasMuluken Alemayehu FINAL PDFKefi BelayAinda não há avaliações
- Plmun Thesis Mike MahorDocumento36 páginasPlmun Thesis Mike MahorPAUL DANIEL MAHORAinda não há avaliações
- Annals of Medicine and Surgery: Bliss J. ChangDocumento2 páginasAnnals of Medicine and Surgery: Bliss J. ChangroromutiaraAinda não há avaliações
- Rti 2Documento10 páginasRti 2REG.B/0620103018/LUQMAN AHMADAinda não há avaliações
- Perceived Benefits Received and Behavioral Intentions of Kabankalan Sinulog Festival TouristsDocumento14 páginasPerceived Benefits Received and Behavioral Intentions of Kabankalan Sinulog Festival TouristsMark GermanAinda não há avaliações
- Blood Drive ProposalDocumento4 páginasBlood Drive Proposalapi-250853393100% (2)
- HDFC Bank Project Saving AccountDocumento58 páginasHDFC Bank Project Saving Accountkunal srivastava100% (6)
- Step by Step Approach For Qualitative Data Analysis: Babatunde Femi AkinyodeDocumento12 páginasStep by Step Approach For Qualitative Data Analysis: Babatunde Femi AkinyodeSarras InfoAinda não há avaliações
- Adminstrative LawDocumento27 páginasAdminstrative LawGuru PrashannaAinda não há avaliações
- ACTION RESEARCH PRoposalDocumento2 páginasACTION RESEARCH PRoposalFritzAinda não há avaliações
- IELTS Vocabulary (1) JDocumento7 páginasIELTS Vocabulary (1) JBolorAinda não há avaliações
- ResumeDocumento1 páginaResumeapi-289204640Ainda não há avaliações
- O 1 Request PacketDocumento18 páginasO 1 Request PacketcdolekAinda não há avaliações
- UNICEF Childhood Disability in MalaysiaDocumento140 páginasUNICEF Childhood Disability in Malaysiaying reenAinda não há avaliações
- Unit 2: Data Collection and Sampling Techniques: Activating Prior KnowledgeDocumento12 páginasUnit 2: Data Collection and Sampling Techniques: Activating Prior KnowledgeMaricel ViloriaAinda não há avaliações
- (Cernea, 1995) Social Integration and Population DisplacementDocumento32 páginas(Cernea, 1995) Social Integration and Population DisplacementChica con cara de gatoAinda não há avaliações
- Module 2Documento6 páginasModule 2Christian DelfinAinda não há avaliações
- Shanthini InternDocumento25 páginasShanthini InternJayalakshmi RavichandranAinda não há avaliações
- Household Emergency Preparedness A Literature Review2012Journal of Community HealthDocumento9 páginasHousehold Emergency Preparedness A Literature Review2012Journal of Community HealthAyuAinda não há avaliações
- 1 Running Head: Nursing Theory AnalysisDocumento16 páginas1 Running Head: Nursing Theory AnalysisMa.Therese GarganianAinda não há avaliações
- NCM 116 SyllabusDocumento42 páginasNCM 116 SyllabusMiller Acompañado100% (8)
- Chanakya National Law University: Public International Law On The TopicDocumento4 páginasChanakya National Law University: Public International Law On The TopicKaran Singh RautelaAinda não há avaliações
- RRL DocumentDocumento16 páginasRRL DocumentTito CadeliñaAinda não há avaliações
- 提高创意写作的秘诀Documento13 páginas提高创意写作的秘诀afoddokhvhtldv100% (1)
- Summer Internship Project: ON Performance Appraisal Effectiveness IN Hindalco Flat Rolled Product, HirakudDocumento92 páginasSummer Internship Project: ON Performance Appraisal Effectiveness IN Hindalco Flat Rolled Product, HirakudUmrah NaushadAinda não há avaliações
- Mis CRMDocumento2 páginasMis CRMsolaiman93Ainda não há avaliações
- How To Write A Learning Contract PDFDocumento6 páginasHow To Write A Learning Contract PDFCustom Writing ServicesAinda não há avaliações
- 2014 15 GraduateDocumento306 páginas2014 15 GraduateyukmAinda não há avaliações